Multiple Species Comparison of Cardiac Troponin T and Dystrophin: Unravelling the DNA behind Dilated Cardiomyopathy
Abstract
:1. Introduction to Cardiomyopathies
1.1. Dilated Cardiomyopathy in Humans
1.2. Dilated Cardiomyopathy in Animals
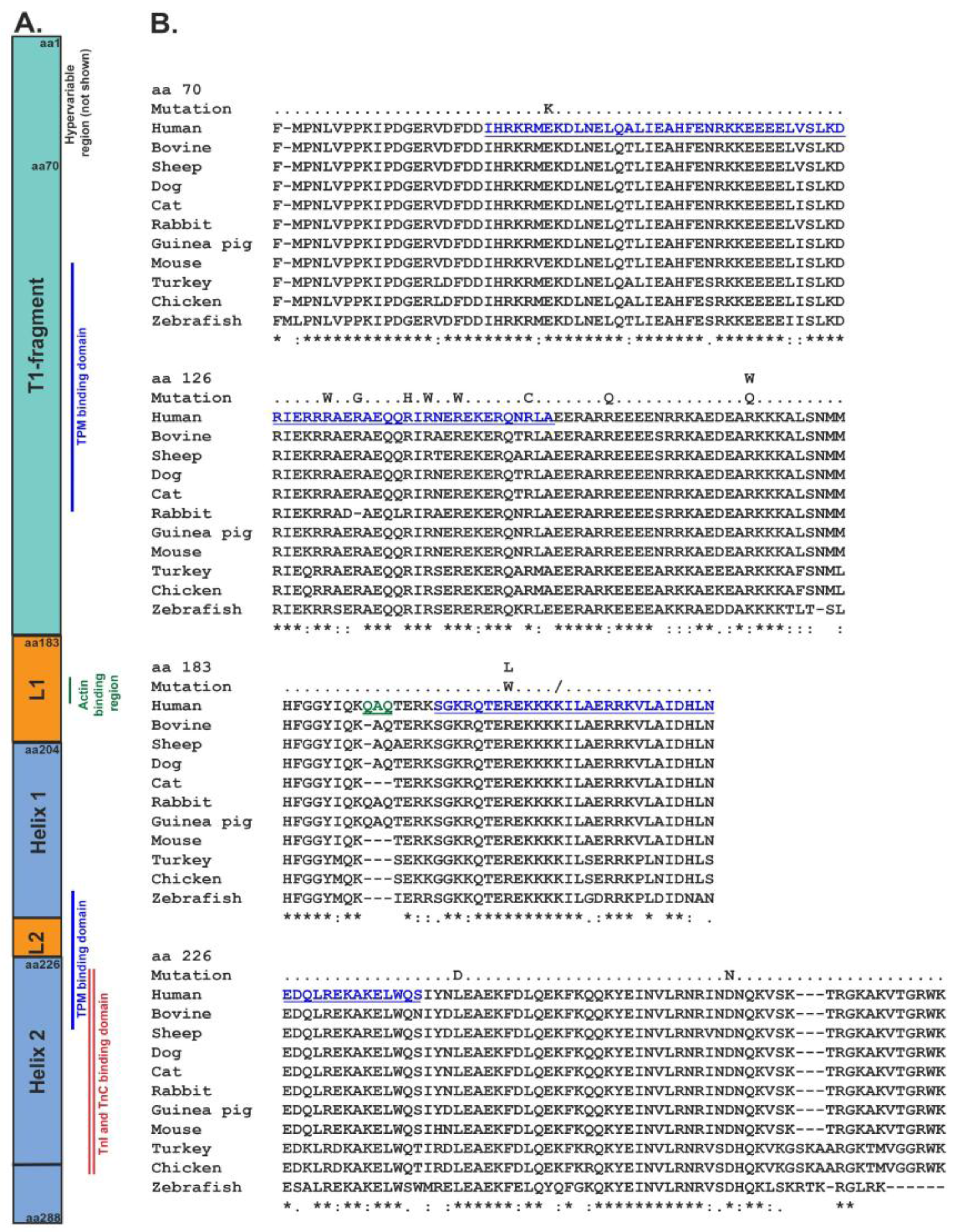
1.3. Expression, Structure, and Function of Cardiac Troponin T
1.4. Cardiac Troponin T Mutations Relating to Cardiomyopathy in Humans
1.5. Cardiac Troponin T Mutations Relating to Cardiomyopathy in Non-Humans
1.6. Expression, Structure, and Function of Dystrophin
1.7. Dystrophin Mutations Relating to Cardiomyopathy in Humans
1.8. Dystrophin Mutations Relating to Cardiomyopathy in Non-Humans
2. Discussion
3. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Wexler, R.K.; Elton, T.; Pleister, A.; Feldman, D. Cardiomyopathy: An overview. Am. Fam. Physician 2009, 79, 778–784. [Google Scholar] [PubMed]
- Maron, B.J.; Towbin, J.A.; Thiene, G.; Antzelevitch, C.; Corrado, D.; Arnett, D.; Moss, A.J.; Seidman, C.E.; Young, J.B. Contemporary definitions and classification of the cardiomyopathies: An american heart association scientific statement from the council on clinical cardiology, heart failure and transplantation committee; quality of care and outcomes research and functional genomics and translational biology interdisciplinary working groups; and council on epidemiology and prevention. Circulation 2006, 113, 1807–1816. [Google Scholar]
- Wieczorek, D.F.; Jagatheesan, G.; Rajan, S. The role of tropomyosin in heart disease. In Tropomyosin; Gunning, P., Ed.; Springer: New York, NY, USA, 2008; Volume 644, pp. 132–142. [Google Scholar]
- Kushwaha, S.S.; Fallon, J.T.; Fuster, V. Restrictive cardiomyopathy. N. Engl. J. Med. 1997, 336, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Basso, C.; Corrado, D.; Marcus, F.I.; Nava, A.; Thiene, G. Arrhythmogenic right ventricular cardiomyopathy. Lancet 2009, 373, 1289–1300. [Google Scholar] [CrossRef]
- Towbin, J.A. Left ventricular noncompaction: A new form of heart failure. Heart Fail. Clin. 2010, 6, 453–469. [Google Scholar] [CrossRef] [PubMed]
- Towbin, J.A.; Bowles, N.E. The failing heart. Nature 2002, 415, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Braunwald, E. Heart Disease: A Textbook of Cardiovascular Medicine, 8th ed.; Saunders: Phiadelphia, PA, USA, 2008. [Google Scholar]
- Fatkin, D. Guidelines for the diagnosis and management of familial dilated cardiomyopathy. Heart Lung Circ. 2011, 20, 691–693. [Google Scholar] [CrossRef] [PubMed]
- Cahill, T.J.; Ashrafian, H.; Watkins, H. Genetic cardiomyopathies causing heart failure. Circ. Res. 2013, 113, 660–675. [Google Scholar] [CrossRef] [PubMed]
- Fleming, J.M.; Creevy, K.E.; Promislow, D.E. Mortality in north american dogs from 1984 to 2004: An investigation into age-, size-, and breed-related causes of death. J. Vet. Intern. Med. 2011, 25, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Egenvall, A.; Bonnett, B.N.; Haggstrom, J. Heart disease as a cause of death in insured Swedish dogs younger than 10 years of age. J. Vet. Intern. Med. 2006, 20, 894–903. [Google Scholar] [CrossRef] [PubMed]
- Brownlie, S.E.; Cobb, M.A. Observations on the development of congestive heart failure in Irish wolfhounds with dilated cardiomyopathy. J. Small Anim. Pract. 1999, 40, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Simpson, S.; Edwards, J.; Ferguson-Mignan, T.F.; Cobb, M.; Mongan, N.P.; Rutland, C.S. Genetics of Human and Canine Dilated Cardiomyopathy. Int. J. Genom. 2015, 2015, 204823. [Google Scholar] [CrossRef] [PubMed]
- Schatzberg, S.J.; Olby, N.J.; Breen, M.; Anderson, L.V.B.; Langford, C.F.; Dickens, H.F.; Wilton, S.D.; Zeiss, C.J.; Binns, M.M.; Kornegay, J.N.; et al. Molecular analysis of a spontaneous dystrophin ‘knockout’ dog. Neuromuscul. Disord. 1999, 9, 289–295. [Google Scholar] [CrossRef]
- Meurs, K.M.; Lahmers, S.; Keene, B.W.; White, S.N.; Oyama, M.A.; Mauceli, E.; Lindblad-Toh, K. A splice site mutation in a gene encoding for PDK4, a mitochondrial protein, is associated with the development of dilated cardiomyopathy in the Doberman pinscher. Hum. Genet. 2012, 131, 1319–1325. [Google Scholar] [CrossRef] [PubMed]
- Meurs, K.M.; Stern, J.A.; Sisson, D.D.; Kittleson, M.D.; Cunningham, S.M.; Ames, M.K.; Atkins, C.E.; DeFrancesco, T.; Hodge, T.E.; Keene, B.W.; et al. Association of Dilated Cardiomyopathy with the Striatin Mutation Genotype in Boxer Dogs. J. Vet. Intern. Med. 2013, 27, 1437–1440. [Google Scholar] [CrossRef] [PubMed]
- Philipp, U.; Vollmar, A.; Haggstrom, J.; Thomas, A.; Distl, O. Multiple Loci Are Associated with Dilated Cardiomyopathy in Irish Wolfhounds. PLoS ONE 2012, 7, e36691. [Google Scholar] [CrossRef] [PubMed]
- Simpson, S.; Edwards, J.; Emes, R.D.; Cobb, M.A.; Mongan, N.P.; Rutland, C.S. A predictive model for canine dilated cardiomyopathy—A meta-analysis of Doberman Pinscher data. PeerJ 2015, 3, e842. [Google Scholar] [CrossRef] [PubMed]
- Simpson, S.; Dunning, M.D.; Brownlie, S.; Patel, J.; Godden, M.; Cobb, M.; Mongan, N.P.; Rutland, C.S. Multiple Genetic Associations with Irish Wolfhound Dilated Cardiomyopathy. Biomed. Res. Int. 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- Frame, D.D.; Kelly, E.J.; Van Wettere, A. Dilated Cardiomyopathy in a Rio Grande Wild Turkey (Meleagris gallopavo intermedia) in Southern Utah, USA, 2013. J. Wildl. Dis. 2015, 51, 790–792. [Google Scholar] [CrossRef] [PubMed]
- Biesiadecki, B.J.; Schneider, K.L.; Yu, Z.B.; Chong, S.M.; Jin, J.P. An R111C polymorphism in wild turkey cardiac troponin I accompanying the dilated cardiomyopathy-related abnormal splicing variant of cardiac troponin T with potentially compensatory effects. J. Biol. Chem. 2004, 279, 13825–13832. [Google Scholar] [CrossRef] [PubMed]
- Biesiadecki, B.J.; Jin, J.P. Exon skipping in cardiac troponin T of turkeys with inherited dilated cardiomyopathy. J. Biol. Chem. 2002, 277, 18459–18468. [Google Scholar] [CrossRef] [PubMed]
- Powers, M.D.; Good, A.L.; Czarnecki, C.M.; Evanson, O.A. Monoamine oxidase inhibition and furazolidone-induced cardiomyopathy in turkey poults. Poult. Sci. 1983, 62, 1850–1855. [Google Scholar] [CrossRef] [PubMed]
- Julian, R.J.; Mirsalimi, S.M.; Bagley, L.G.; Squires, E.J. Effect of hypoxia and diet on spontaneous turkey cardiomyopathy (round-heart disease). Avian Dis. 1992, 36, 1043–1047. [Google Scholar] [CrossRef] [PubMed]
- Gwathmey, J.K.; Hajjar, R.J. Calcium-activated force in a turkey model of spontaneous dilated cardiomyopathy: Adaptive changes in thin myofilament Ca2+ regulation with resultant implications on contractile performance. J. Mol. Cell. Cardiol. 1992, 24, 1459–1470. [Google Scholar] [CrossRef]
- Lin, K.C.; Xu, J.; Kamara, D.; Geng, T.; Gyenai, K.; Reed, K.M.; Smith, E.J. DNA sequence and haplotype variation in two candidate genes for dilated cardiomyopathy in the turkey Meleagris gallopavo. Genome 2007, 50, 463–469. [Google Scholar] [PubMed]
- Breeding, S.W.; McRee, W.A.; Ficken, M.D.; Ferket, P.R. Effect of protein restriction during brooding on spontaneous turkey cardiomyopathy. Avian Dis. 1994, 38, 366–370. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.C.; Gyenai, K.; Pyle, R.L.; Geng, T.; Xu, J.; Smith, E.J. Candidate gene expression analysis of toxin-induced dilated cardiomyopathy in the turkey (Meleagris gallopavo). Poult. Sci. 2006, 85, 2216–2221. [Google Scholar] [CrossRef] [PubMed]
- Kolb, E. Latest Findings on the Significance and Metabolism of Taurine and on Dysfunctions Caused by Taurine Deficiency (Retinal Degeneration, Cardiomyopathy Etc) in the Cat. Prakt. Tierarzt 1990, 71, 21–24. [Google Scholar]
- Pion, P.D.; Kittleson, M.D.; Rogers, Q.R.; Morris, J.G. Myocardial Failure in Cats Associated with Low Plasma Taurine—A Reversible Cardiomyopathy. Science 1987, 237, 764–768. [Google Scholar] [CrossRef] [PubMed]
- Pion, P.D.; Kittleson, M.D.; Skiles, M.L.; Rogers, Q.R.; Morris, J.G. Dilated Cardiomyopathy Associated with Taurine Deficiency in the Domestic Cat—Relationship to Diet and Myocardial Taurine Content. Taurine 1992, 315, 63–73. [Google Scholar]
- Pion, P.D.; Kittleson, M.D.; Thomas, W.P.; Delellis, L.A.; Rogers, Q.R. Response of Cats with Dilated Cardiomyopathy to Taurine Supplementation. J. Am. Vet. Med. Assoc. 1992, 201, 275–284. [Google Scholar] [PubMed]
- Lawler, D.F.; Templeton, A.J.; Monti, K.L. Evidence for Genetic Involvement in Feline Dilated Cardiomyopathy. J. Vet. Intern. Med. 1993, 7, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Wilson, F.D.; Magee, D.L.; Jones, K.H.; Baravik-Munsell, E.; Cummings, T.S.; Wills, R.W.; Pace, L.W. Morphometric Documentation of a High Prevalence of Left Ventricular Dilated Cardiomyopathy in Both Clinically Normal and Cyanotic Mature Commercial Broiler Breeder Roosters with Comparisons to Market-Age Broilers. Avian Dis. 2016, 60, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Weekes, J.; Wheeler, C.H.; Yan, J.X.; Weil, J.; Eschenhagen, T.; Scholtysik, G.; Dunn, M.J. Bovine dilated cardiomyopathy: Proteomic analysis of an animal model of human dilated cardiomyopathy. Electrophoresis 1999, 20, 898–906. [Google Scholar] [CrossRef]
- Nart, P.; Thompson, H.; Barrett, D.C.; Armstrong, S.C.; McPhaden, A.R. Clinical and pathological features of dilated cardiomyopathy in Holstein-Friesian cattle. Vet. Rec. 2004, 155, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Simpson, S.; Rutland, P.; Rutland, C.S. Genomic Insights into Cardiomyopathies: A Comparative Cross-Species Review. Vet. Sci. 2017, 1, 19. [Google Scholar] [CrossRef]
- Greaser, M.L.; Gergely, J. Reconstitution of troponin activity from three protein components. J. Biol. Chem. 1971, 246, 4226–4233. [Google Scholar] [PubMed]
- England, J.; Loughna, S. Heavy and light roles: Myosin in the morphogenesis of the heart. Cell. Mol. Life Sci. 2013, 70, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Sehnert, A.J.; Huq, A.; Weinstein, B.M.; Walker, C.; Fishman, M.; Stainier, D.Y.R. Cardiac troponin T is essential in sarcomere assembly and cardiac contractility. Nat. Genet. 2002, 31, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Gomes, A.V.; Potter, J.D. Molecular and cellular aspects of troponin cardiomyopathies. Ann. N. Y. Acad. Sci. 2004, 1015, 214–224. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.-P.; Zhang, Z.; Bautista, J.A. Isoform Diversity, Regulation, and Functional Adaptation of Troponin and Calponin. Crit. Rev. Eukaryot. Gene Expr. 2008, 18, 93–124. [Google Scholar] [CrossRef] [PubMed]
- Perry, S.V. Troponin T: Genetics, properties and function. J. Muscle Res. Cell Motil. 1998, 19, 575–602. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.P.; Chong, S.M. Localization of the two tropomyosin-binding sites of troponin T. Arch. Biochem. Biophys. 2010, 500, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Pearlstone, J.R.; Smillie, L.B. Binding of troponin-T fragments to several types of tropomyosin. Sensitivity to Ca2+ in the presence of troponin-C. J. Biol. Chem. 1982, 257, 10587–10592. [Google Scholar] [PubMed]
- Takeda, S.; Yamashita, A.; Maeda, K.; Maeda, Y. Structure of the core domain of human cardiac troponin in the Ca(2+)-saturated form. Nature 2003, 424, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Stefancsik, R.; Jha, P.K.; Sarkar, S. Identification and mutagenesis of a highly conserved domain in troponin T responsible for troponin I binding: Potential role for coiled coil interaction. Proc. Natl. Acad. Sci. USA 1998, 95, 957–962. [Google Scholar] [CrossRef] [PubMed]
- Pearlstone, J.R.; Smillie, L.B. Effects of troponin-I plus-C on the binding of troponin T and its fragments to alpha-tropomyosin. Ca2+ sensitivity and cooperativity. J. Biol. Chem. 1983, 258, 2534–2542. [Google Scholar] [PubMed]
- Morris, E.P.; Lehrer, S.S. Troponin-tropomyosin interactions. Fluorescence studies of the binding of troponin, troponin T, and chymotryptic troponin T fragments to specifically labeled tropomyosin. Biochemistry 1984, 23, 2214–2220. [Google Scholar] [CrossRef] [PubMed]
- Franklin, A.J.; Baxley, T.; Kobayashi, T.; Chalovich, J.M. The C-terminus of troponin T is essential for maintaining the inactive state of regulated actin. Biophys. J. 2012, 102, 2536–2544. [Google Scholar] [CrossRef] [PubMed]
- Hershberger, R.E.; Pinto, J.R.; Parks, S.B.; Kushner, J.D.; Li, D.; Ludwigsen, S.; Cowan, J.; Morales, A.; Parvatiyar, M.S.; Potter, J.D. Clinical and functional characterization of TNNT2 mutations identified in patients with dilated cardiomyopathy. Circ. Cardiovasc. Genet. 2009, 2, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Murakami, C.; Nakamura, S.; Kobayashi, M.; Maeda, K.; Irie, W.; Wada, B.; Hayashi, M.; Sasaki, C.; Nakamaru, N.; Furukawa, M.; et al. Analysis of the sarcomere protein gene mutation on cardiomyopathy—Mutations in the cardiac troponin I gene. Legal Med. 2010, 12, 280–283. [Google Scholar] [CrossRef] [PubMed]
- Parvatiyar, M.S.; Landstrom, A.P.; Figueiredo-Freitas, C.; Potter, J.D.; Ackerman, M.J.; Pinto, J.R. A Mutation in TNNC1-encoded Cardiac Troponin C, TNNC1-A31S, Predisposes to Hypertrophic Cardiomyopathy and Ventricular Fibrillation. J. Biol. Chem. 2012, 287, 31845–31855. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.N.; Parvatiyar, M.S.; Potter, J.D. Troponin and cardiomyopathy. Biochem. Biophys. Res. Commun. 2008, 369, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Mirza, M.; Marston, S.; Willott, R.; Ashley, C.; Mogensen, J.; McKenna, W.; Robinson, P.; Redwood, C.; Watkins, H. Dilated Cardiomyopathy Mutations in Three Thin Filament Regulatory Proteins Result in a Common Functional Phenotype. J. Biol. Chem. 2005, 280, 28498–28506. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.W.; Morimoto, S.; Harada, K.; Du, C.K.; Takahashi-Yanaga, F.; Miwa, Y.; Sasaguri, T.; Ohtsuki, I. Cardiac troponin T mutation R141W found in dilated cardiomyopathy stabilizes the troponin T-tropomyosin interaction and causes a Ca2+ desensitization. J. Mol. Cell. Cardiol. 2003, 35, 1421–1427. [Google Scholar] [CrossRef] [PubMed]
- Rampersaud, E.; Siegfried, J.D.; Norton, N.; Li, D.; Martin, E.; Hershberger, R.E. Rare variant mutations identified in pediatric patients with dilated cardiomyopathy. Prog. Pediatr. Cardiol. 2011, 31, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Zeller, R.; Ivandic, B.T.; Ehlermann, P.; Mucke, O.; Zugck, C.; Remppis, A.; Giannitsis, E.; Katus, H.A.; Weichenhan, D. Large-scale mutation screening in patients with dilated or hypertrophic cardiomyopathy: A pilot study using DGGE. J. Mol. Med. (Berl.) 2006, 84, 682–691. [Google Scholar] [CrossRef] [PubMed]
- Hershberger, R.E.; Parks, S.B.; Kushner, J.D.; Li, D.; Ludwigsen, S.; Jakobs, P.; Nauman, D.; Burgess, D.; Partain, J.; Litt, M. Coding sequence mutations identified in MYH7, TNNT2, SCN5A, CSRP3, LBD3, and TCAP from 313 patients with familial or idiopathic dilated cardiomyopathy. Clin. Trans. Sci. 2008, 1, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Mogensen, J.; Murphy, R.T.; Shaw, T.; Bahl, A.; Redwood, C.; Watkins, H.; Burke, M.; Elliott, P.M.; McKenna, W.J. Severe disease expression of cardiac troponin C and T mutations in patients with idiopathic dilated cardiomyopathy. J. Am. Coll. Cardiol. 2004, 44, 2033–2040. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.W.; Wu, X.Y.; Morimoto, S. Inherited cardiomyopathies caused by troponin mutations. J. Geriatr. Cardiol. 2013, 10, 91–101. [Google Scholar] [PubMed]
- Morales, A.; Pinto, J.R.; Siegfried, J.D.; Li, D.; Norton, N.; Hofmeyer, M.; Vallin, M.; Morales, A.R.; Potter, J.D.; Hershberger, R.E. Late onset sporadic dilated cardiomyopathy caused by a cardiac troponin T mutation. Clin. Transl. Sci. 2010, 3, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Czernuszewicz, G.Z.; Gonzalez, O.; Tapscott, T.; Karibe, A.; Durand, J.B.; Brugada, R.; Hill, R.; Gregoritch, J.M.; Anderson, J.L.; et al. Novel cardiac troponin T mutation as a cause of familial dilated cardiomyopathy. Circulation 2001, 104, 2188–2193. [Google Scholar] [CrossRef] [PubMed]
- Rani, D.S.; Dhandapany, P.S.; Nallari, P.; Narasimhan, C.; Thangaraj, K. A Novel Arginine to Tryptophan (R144W) Mutation in Troponin T (cTnT) Gene in an Indian Multigenerational Family with Dilated Cardiomyopathy (FDCM). PLoS ONE 2014, 9, e101451. [Google Scholar] [CrossRef] [PubMed]
- Stefanelli, C.B.; Rosenthal, A.; Borisov, A.B.; Ensing, G.J.; Russell, M.W. Novel troponin T mutation in familial dilated cardiomyopathy with gender-dependant severity. Mol. Genet. Metab. 2004, 83, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Jachymova, M.; Muravska, A.; Palecek, T.; Kuchynka, P.; Rehakova, H.; Magage, S.; Kral, A.; Zima, T.; Horky, K.; Linhart, A. Genetic variation screening of TNNT2 gene in a cohort of patients with hypertrophic and dilated cardiomyopathy. Physiol. Res. 2012, 61, 169–175. [Google Scholar] [PubMed]
- Van Acker, H.; De Sutter, J.; Vandekerckhove, K.; de Ravel, T.J.; Verhaaren, H.; De Backer, J. Dilated cardiomyopathy caused by a novel TNNT2 mutation-added value of genetic testing in the correct identification of affected subjects. Int. J. Cardiol. 2010, 144, 307–309. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.P.; Tikunova, S.B. Ca(2+) exchange with troponin C and cardiac muscle dynamics. Cardiovasc. Res. 2008, 77, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Sun, N.; Yazawa, M.; Liu, J.; Han, L.; Sanchez-Freire, V.; Abilez, O.J.; Navarrete, E.G.; Hu, S.; Wang, L.; Lee, A.; et al. Patient-specific induced pluripotent stem cells as a model for familial dilated cardiomyopathy. Sci. Transl. Med. 2012, 4, 130ra47. [Google Scholar] [CrossRef] [PubMed]
- Venkatraman, G.; Harada, K.; Gomes, A.V.; Kerrick, W.G.; Potter, J.D. Different functional properties of troponin T mutants that cause dilated cardiomyopathy. J. Biol. Chem. 2003, 278, 41670–41676. [Google Scholar] [CrossRef] [PubMed]
- Daehmlow, S.; Erdmann, J.; Knueppel, T.; Gille, C.; Froemmel, C.; Hummel, M.; Hetzer, R.; Regitz-Zagrosek, V. Novel mutations in sarcomeric protein genes in dilated cardiomyopathy. Biochem. Biophys. Res. Commun. 2002, 298, 116–120. [Google Scholar] [CrossRef]
- Kamisago, M.; Sharma, S.D.; DePalma, S.R.; Solomon, S.; Sharma, P.; McDonough, B.; Smoot, L.; Mullen, M.P.; Woolf, P.K.; Wigle, E.D.; et al. Mutations in Sarcomere Protein Genes as a Cause of Dilated Cardiomyopathy. N. Engl. J. Med. 2000, 343, 1688–1696. [Google Scholar] [CrossRef] [PubMed]
- Inoue, T.; Kobirumaki-Shimozawa, F.; Kagemoto, T.; Fujii, T.; Terui, T.; Kusakari, Y.; Hongo, K.; Morimoto, S.; Ohtsuki, I.; Hashimoto, K.; et al. Depressed Frank-Starling mechanism in the left ventricular muscle of the knock-in mouse model of dilated cardiomyopathy with troponin T deletion mutation DeltaK210. J. Mol. Cell. Cardiol. 2013, 63, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Watkins, H.; McKenna, W.J.; Thierfelder, L.; Suk, H.J.; Anan, R.; O’Donoghue, A.; Spirito, P.; Matsumori, A.; Moravec, C.S.; Seidman, J.G.; et al. Mutations in the Genes for Cardiac Troponin T and α-Tropomyosin in Hypertrophic Cardiomyopathy. N. Engl. J. Med. 1995, 332, 1058–1065. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.; Griffiths, P.J.; Watkins, H.; Redwood, C.S. Dilated and hypertrophic cardiomyopathy mutations in troponin and alpha-tropomyosin have opposing effects on the calcium affinity of cardiac thin filaments. Circ. Res. 2007, 101, 1266–1273. [Google Scholar] [CrossRef] [PubMed]
- McConnell, B.K.; Jones, K.A.; Fatkin, D.; Arroyo, L.H.; Lee, R.T.; Aristizabal, O.; Turnbull, D.H.; Georgakopoulos, D.; Kass, D.; Bond, M.; et al. Dilated cardiomyopathy in homozygous myosin-binding protein C mutant mice. J. Clin. Investig. 1999, 104, 1235–1244. [Google Scholar] [CrossRef] [PubMed]
- Murphy, R.T.; Mogensen, J.; Shaw, A.; Kubo, T.; Hughes, S.; McKenna, W.J. Novel mutation in cardiac troponin I in recessive idiopathic dilated cardiomyopathy. Lancet 2004, 363, 371–372. [Google Scholar] [CrossRef]
- Mogensen, J.; Kubo, T.; Duque, M.; Uribe, W.; Shaw, A.; Murphy, R.; Gimeno, J.R.; Elliott, P.; McKenna, W.J. Idiopathic restrictive cardiomyopathy is part of the clinical expression of cardiac troponin I mutations. J. Clin. Investig. 2003, 111, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, F.; Banerjee, S.K.; Lage, M.L.; Huang, X.N.; Smith, S.H.; Saba, S.; Rager, J.; Conner, D.A.; Janczewski, A.M.; Tobita, K.; et al. The Role of Cardiac Troponin T Quantity and Function in Cardiac Development and Dilated Cardiomyopathy. PLoS ONE 2008, 3, e2642. [Google Scholar] [CrossRef] [PubMed]
- Ramratnam, M.; Salama, G.; Sharma, R.K.; Wang, D.W.; Smith, S.H.; Banerjee, S.K.; Huang, X.N.; Gifford, L.M.; Pruce, M.L.; Gabris, B.E.; et al. Gene-Targeted Mice with the Human Troponin T R141W Mutation Develop Dilated Cardiomyopathy with Calcium Desensitization. PLoS ONE 2016, 11, e0167681. [Google Scholar] [CrossRef] [PubMed]
- Burke, M.A.; Chang, S.; Wakimoto, H.; Gorham, J.M.; Conner, D.A.; Christodoulou, D.C.; Parfenov, M.G.; DePalma, S.R.; Eminaga, S.; Konno, T.; et al. Molecular profiling of dilated cardiomyopathy that progresses to heart failure. JCI Insight 2016, 1. [Google Scholar] [CrossRef] [PubMed]
- Hamada, T.; Kubo, T.; Kitaoka, H.; Hirota, T.; Hoshikawa, E.; Hayato, K.; Shimizu, Y.; Okawa, M.; Yamasaki, N.; Matsumura, Y.; et al. Clinical features of the dilated phase of hypertrophic cardiomyopathy in comparison with those of dilated cardiomyopathy. Clin. Cardiol. 2010, 33, E24–E28. [Google Scholar] [CrossRef] [PubMed]
- Fujino, N.; Shimizu, M.; Ino, H.; Okeie, K.; Yamaguchi, M.; Yasuda, T.; Kokado, H.; Mabuchi, H. Cardiac troponin T Arg92 Trp mutation and progression from hypertrophic to dilated cardiomyopathy. Clin. Cardiol. 2001, 24, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Fujino, N.; Shimizu, M.; Ino, H.; Yamaguchi, M.; Yasuda, T.; Nagata, M.; Konno, T.; Mabuchi, H. A novel mutation Lys273Glu in the cardiac troponin T gene shows high degree of penetrance and transition from hypertrophic to dilated cardiomyopathy. Am. J. Cardiol. 2002, 89, 29–33. [Google Scholar] [CrossRef]
- Thierfelder, L.; Watkins, H.; MacRae, C.; Lamas, R.; McKenna, W.; Vosberg, H.P.; Seidman, J.G.; Seidman, C.E. Alpha-tropomyosin and cardiac troponin T mutations cause familial hypertrophic cardiomyopathy: A disease of the sarcomere. Cell 1994, 77, 701–712. [Google Scholar] [CrossRef]
- Menon, S.C.; Michels, V.V.; Pellikka, P.A.; Ballew, J.D.; Karst, M.L.; Herron, K.J.; Nelson, S.M.; Rodeheffer, R.J.; Olson, T.M. Cardiac troponin T mutation in familial cardiomyopathy with variable remodeling and restrictive physiology. Clin. Genet. 2008, 74, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Ripoll-Vera, T.; Gamez, J.M.; Govea, N.; Gomez, Y.; Nunez, J.; Socias, L.; Escandell, A.; Rosell, J. Clinical and Prognostic Profiles of Cardiomyopathies Caused by Mutations in the Troponin T Gene. Rev. Esp. Cardiol. (Engl. Ed.) 2016, 69, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.; Mirza, M.; Knott, A.; Abdulrazzak, H.; Willott, R.; Marston, S.; Watkins, H.; Redwood, C. Alterations in thin filament regulation induced by a human cardiac troponin T mutant that causes dilated cardiomyopathy are distinct from those induced by troponin T mutants that cause hypertrophic cardiomyopathy. J. Biol. Chem. 2002, 277, 40710–40716. [Google Scholar] [CrossRef] [PubMed]
- Jaquet, K.; Mugge, A. Consequences of Mutations in Genes Encoding Cardiac Troponin C, T and I-Molecular Insights and Cardiomyopathies; Veselka, J., Ed.; Basic Research to Clincal Management; InTech: Rijeka, Croatia, 2012. [Google Scholar]
- Na, I.; Kong, M.J.; Straight, S.; Pinto, J.R.; Uversky, V.N. Troponins, intrinsic disorder, and cardiomyopathy. Biol. Chem. 2016, 397, 731–751. [Google Scholar] [CrossRef] [PubMed]
- Biesiadecki, B.J.; Elder, B.D.; Yu, Z.-B.; Jin, J.-P. Cardiac Troponin T Variants Produced by Aberrant Splicing of Multiple Exons in Animals with High Instances of Dilated Cardiomyopathy. J. Biol. Chem. 2002, 277, 50275–50285. [Google Scholar] [CrossRef] [PubMed]
- Kunkel, L.M.; Beggs, A.H.; Hoffman, E.P. Molecular genetics of Duchenne and Becker muscular dystrophy: Emphasis on improved diagnosis. Clin. Chem. 1989, 35 (Suppl. 7), B21–B24. [Google Scholar] [PubMed]
- Mandel, J.L. Dystrophin. The gene and its product. Nature 1989, 339, 584–586. [Google Scholar] [PubMed]
- Manole, E. The dystrophin gene and its product—A view. Rom. J. Neurol. Psychiatry 1995, 33, 109–119. [Google Scholar] [PubMed]
- Surono, A.; Barnea, E.; Levy, Z.; Neuman, S.; Yaffe, D.; Nudel, U. Circular dystrophin RNAs consisting of exons that were skipped by alternative splicing. Hum. Mol. Genet. 1999, 8, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Muntoni, F.; Torelli, S.; Ferlini, A. Transcription of the dystrophin gene in normal tissues and in skeletal muscle of a family with X-linked dilated cardiomyopathy. Am. J. Hum. Genet. 1995, 56, 151–157. [Google Scholar] [PubMed]
- Bar, S.; Takeshima, Y.; Wibawa, T.; Ikezawa, M.; Nonaka, I.; Matsuo, M. A novel product of the Duchenne muscular dystrophy gene which greatly differs from the known isoforms in its structure and tissue distribution. Biochem. J. 1990, 272, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Muntoni, F.; Torelli, S.; Ferlini, A. Dystrophin and mutations: One gene, several proteins, multiple phenotypes. Lancet Neurol. 2003, 2, 731–740. [Google Scholar] [CrossRef]
- Wang, Y.X.; Marino-Enriquez, A.; Bennett, R.R.; Zhu, M.J.; Shen, Y.P.; Eilers, G.; Lee, J.C.; Henze, J.; Fletcher, B.S.; Gu, Z.Z.; et al. Dystrophin is a tumor suppressor in human cancers with myogenic programs. Nat. Genet. 2014, 46, 601–606. [Google Scholar] [CrossRef] [PubMed]
- Korner, H.; Epanchintsev, A.; Berking, C.; Schuler-Thurner, B.; Speicher, M.R.; Menssen, A.; Hermeking, H. Digital karyotyping reveals frequent inactivation of the Dystrophin/DMD gene in malignant melanoma. Cell Cycle 2007, 6, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Monaco, A.P.; Neve, R.L.; Collettifeener, C.; Bertelson, C.J.; Kurnit, D.M.; Kunkel, L.M. Isolation of Candidate Cdnas for Portions of the Duchenne Muscular-Dystrophy Gene. Nature 1986, 323, 646–650. [Google Scholar] [CrossRef] [PubMed]
- Aartsma-Rus, A.; Van Deutekom, J.C.T.; Fokkema, I.F.; Van Ommen, G.J.B.; Den Dunnen, J.T. Entries in the Leiden Duchenne muscular dystrophy mutation database: An overview of mutation types and paradoxical cases that confirm the reading-frame rule. Muscle Nerve 2006, 34, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Fokkema, I.F.A.C.; den Dunnen, J.T.; Taschner, P.E.M. LOVD: Easy creation of a locus-specific sequence variation database using an “LSDB-in-a-Box” approach. Hum. Mutat. 2005, 26, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Laing, N.G. Molecular Genetics and Genetic Couselling for Duchenne/Becker Muscular Dystrophy, in Molecular and Cell Biology of Muscular Dystrophy; Partridge, T., Ed.; Chapman & Hall: London, UK, 1993; pp. 37–84. [Google Scholar]
- Love, D.R.; Flint, T.J.; Genet, S.A.; Middletonprice, H.R.; Davies, K.E. Becker Muscular-Dystrophy Patient with a Large Intragenic Dystrophin Deletion—Implications for Functional Minigenes and Gene-Therapy. J. Med. Genet. 1991, 28, 860–864. [Google Scholar] [CrossRef] [PubMed]
- England, S.B.; Nicholson, L.V.B.; Johnson, M.A.; Forrest, S.M.; Love, D.R.; Zubrzyckagaarn, E.E.; Bulman, D.E.; Harris, J.B.; Davies, K.E. Very Mild Muscular-Dystrophy Associated with the Deletion of 46-Percent of Dystrophin. Nature 1990, 343, 180–182. [Google Scholar] [CrossRef] [PubMed]
- Love, D.R.; Flint, T.J.; Marsden, R.F.; Bloomfield, J.F.; Daniels, R.J.; Forrest, S.M.; Gabrielli, O.; Giorgi, P.; Novelli, G.; Davies, K.E. Characterization of Deletions in the Dystrophin Gene Giving Mild Phenotypes. Am. J. Med. Genet. 1990, 37, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Monaco, A.P.; ertelson, C.J.; Liechti-Gallati, S.; Moser, H.; Kunkel, L.M. An Explanation for the Phenotypic Differences between Patients Bearing Partial Deletions of the DMD Locus. Genomics 1988, 2, 90–95. [Google Scholar] [CrossRef]
- Kerr, T.P.; Sewry, C.A.; Robb, S.A.; Roberts, R.G. Long mutant dystrophins and variable phenotypes: Evasion of nonsense-mediated decay? Hum. Genet. 2001, 109, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Ferlini, A.; Sewry, C.; Melis, M.A.; Mateddu, A.; Muntoni, F. X-linked dilated cardiomyopathy and the dystrophin gene. Neuromuscul. Disord. 1999, 9, 339–346. [Google Scholar] [CrossRef]
- Feng, J.; Yan, J.Y.; Buzin, C.H.; Sommer, S.S.; Towbin, J.A. Comprehensive mutation scanning of the dystrophin gene in patients with nonsyndromic X-linked dilated cardiomyopathy. J. Am. Coll. Cardiol. 2002, 40, 1120–1124. [Google Scholar] [CrossRef]
- Milasin, J.; Muntoni, F.; Severini, G.M.; Bartoloni, L.; Vatta, M.; Krajinovic, M.; Mateddu, A.; Angelini, C.; Camerini, F.; Falaschi, A.; et al. A point mutation in the 5′ splice site of the dystrophin gene first intron responsible for X-linked dilated cardiomyopathy. Hum. Mol. Genet. 1996, 5, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, A.; Ikeda, S.; Yazaki, M.; Yoshida, K.; Kobayashi, O.; Yanagisawa, N.; Takeda, S. Up-regulation of the brain and Purkinje-cell forms of dystrophin transcripts, in Becker muscular dystrophy. Am. J. Hum. Genet. 1997, 60, 1555–1558. [Google Scholar] [CrossRef]
- Bies, R.D.; Maeda, M.; Roberds, S.L.; Holder, E.; Bohlmeyer, T.; Young, J.B.; Campbell, K.P. A 5′ dystrophin duplication mutation causes membrane deficiency of alpha-dystroglycan in a family with X-linked cardiomyopathy. J. Mol. Cell. Cardiol. 1997, 29, 3175–3188. [Google Scholar] [CrossRef] [PubMed]
- Franz, W.M.; Cremer, M.; Herrmann, R.; Grunig, E.; Fogel, W.; Scheffold, T.; Goebel, H.H.; Kircheisen, R.; Kubler, W.; Voit, T.; et al. X-linked dilated cardiomyopathy. Novel mutation of the dystrophin gene. Ann. N. Y. Acad. Sci. 1995, 752, 470–491. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Lopez, R.; Li, H.; Su, J.; Goytia, V.; Towbin, J.A. Evidence for a dystrophin missense mutation as a cause of X-linked dilated cardiomyopathy. Circulation 1997, 95, 2434–2440. [Google Scholar] [CrossRef] [PubMed]
- Winder, S.J.; Gibson, T.J.; Kendrick-Jones, J. Dystrophin and utrophin: The missing links! FEBS Lett. 1995, 369, 27–33. [Google Scholar] [CrossRef]
- Cullen, M.J.; Jaros, E. Ultrastructure of the Skeletal-Muscle in the X-Chromosome-Linked Dystrophic (Mdx) Mous—Comparison with Duchenne Muscular-Dystrophy. Acta Neuropathol. 1988, 77, 69–81. [Google Scholar] [CrossRef] [PubMed]
- Bulfield, G.; Siller, W.G.; Wight, P.A.L.; Moore, K.J. X-Chromosome-Linked Muscular-Dystrophy (Mdx) in the Mouse. Proc. Natl. Acad. Sci. USA 1984, 81, 1189–1192. [Google Scholar] [CrossRef]
- Chapman, V.M.; Miller, D.R.; Armstrong, D.; Caskey, C.T. Recovery of Induced Mutations for X-Chromosome-Linked Muscular-Dystrophy in Mice. Proc. Natl. Acad. Sci. USA 1989, 86, 1292–1296. [Google Scholar] [CrossRef] [PubMed]
- Li, D.J.; Long, C.; Yue, Y.P.; Duan, D.S. Sub-physiological sarcoglycan expression contributes to compensatory muscle protection in mdx mice. Hum. Mol. Genet. 2009, 18, 1209–1220. [Google Scholar] [CrossRef] [PubMed]
- Deconinck, A.E.; Rafael, J.A.; Skinner, J.A.; Brown, S.C.; Potter, A.C.; Metzinger, L.; Watt, D.J.; Dickson, J.G.; Tinsley, J.M.; Davies, K.E. Utrophin-dystrophin-deficient mice as a model for Duchenne muscular dystrophy. Cell 1997, 90, 717–727. [Google Scholar] [CrossRef]
- Rooney, J.E.; Welser, J.V.; Dechert, M.A.; Flintoff-Dye, N.L.; Kaufman, S.J.; Burkin, D.J. Severe muscular dystrophy in mice that lack dystrophin and alpha 7 integrin. J. Cell Sci. 2006, 119, 2185–2195. [Google Scholar] [CrossRef] [PubMed]
- Chun, J.L.; O’Brien, R.; Berry, S.E. Cardiac dysfunction and pathology in the dystrophin and utrophin-deficient mouse during development of dilated cardiomyopathy. Neuromuscul. Disord. 2012, 22, 368–379. [Google Scholar] [CrossRef] [PubMed]
- McGreevy, J.W.; Hakim, C.H.; McIntosh, M.A.; Duan, D.S. Animal models of Duchenne muscular dystrophy: From basic mechanisms to gene therapy. Dis. Model. Mech. 2015, 8, 195–213. [Google Scholar] [CrossRef] [PubMed]
- Taghli-Lamallem, O.; Akasaka, T.; Hogg, G.; Nudel, U.; Yaffe, D.; Chamberlain, J.S.; Ocorr, K.; Bodmer, R. Dystrophin deficiency in Drosophila reduces lifespan and causes a dilated cardiomyopathy phenotype. Aging Cell 2008, 7, 237–249. [Google Scholar] [CrossRef] [PubMed]
- Innes, J.R. Myopathies in animals; a record of some cases including progressive muscular dystrophy (pseudo-hypertrophic) (dog), “weisses Fleisch” (lamb), neuropathic muscular atrophy (sheep) and lymphocytic/histiocytic myositis, neuritis, radiculitis (dog). Br. Vet. J. 1951, 107, 131–143. [Google Scholar] [PubMed]
- Schatzberg, S.; Olby, N.; Steingold, S.; Keene, B.; Atkins, C.; Meurs, K.; Solomon, G.; Goedegebuure, S.A.; Wilton, S.; Sharp, N. A polymerase chain reaction screening strategy for the promoter of the canine dystrophin gene. Am. J. Vet. Res. 1999, 60, 1040–1046. [Google Scholar] [PubMed]
- Sewry, C.A.; Wilson, L.A.; Dux, L.; Dubowitz, V.; Cooper, B.J. Experimental regeneration in canine muscular dystrophy—1. Immunocytochemical evaluation of dystrophin and beta-spectrin expression. Neuromuscul. Disord. 1992, 2, 331–342. [Google Scholar] [CrossRef]
- Cooper, B.J.; Gallagher, E.A.; Smith, C.A.; Valentine, B.A.; Winand, N.J. Mosaic expression of dystrophin in carriers of canine X-linked muscular dystrophy. Lab. Investig. 1990, 62, 171–178. [Google Scholar] [PubMed]
- Howell, J.M.; Fletcher, S.; Kakulas, B.A.; OHara, M.; Lochmuller, H.; Karpati, G. Use of the dog model for Duchenne muscular dystrophy in gene therapy trials. Neuromuscul. Disord. 1997, 7, 325–328. [Google Scholar] [CrossRef]
- Valentine, B.A.; Chandler, S.K.; Cummings, J.F.; Cooper, B.J. In vitro characteristics of normal and dystrophic skeletal muscle from dogs. Am. J. Vet. Res. 1991, 52, 104–107. [Google Scholar] [PubMed]
- Cooper, B.J. The Xmd Dog—Molecular and Phenotypic Characteristics. In Duchenne Muscular Dystrophy; Animal Models and Genetic Manipulations; Raven Press: New York, NY, USA, 1992; pp. 109–111. [Google Scholar]
- Wang, Z.; Storb, R.; Halbert, C.L.; Banks, G.B.; Butts, T.M.; Finn, E.E.; Allen, J.M.; Miller, A.D.; Chamberlain, J.S.; Tapscott, S.J. Successful regional delivery and long-term expression of a dystrophin gene in canine muscular dystrophy: A preclinical model for human therapies. Mol. Ther. 2012, 20, 1501–1507. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.J.; Chamberlain, J.S.; Tapscott, S.J.; Storb, R. Gene Therapy in Large Animal Models of Muscular Dystrophy. Ilar J. 2009, 50, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Gregorevic, P.; Blankinship, M.J.; Allen, J.M.; Crawford, R.W.; Meuse, L.; Miller, D.G.; Russell, D.W.; Chamberlain, J.S. Systemic delivery of genes to striated muscles using adeno-associated viral vectors. Nat. Med. 2004, 10, 828–834. [Google Scholar] [CrossRef] [PubMed]
- Yue, Y.P.; Ghosh, A.; Long, C.; Bostick, B.; Smith, B.F.; Kornegay, J.N.; Duan, D.S. A Single Intravenous Injection of Adeno-associated Virus Serotype-9 Leads to Whole Body Skeletal Muscle Transduction in Dogs. Mol. Ther. 2008, 16, 1944–1952. [Google Scholar] [CrossRef] [PubMed]
- Cobb, M.A.; Brownlie, S.E.; Pidduck, H.G.; Batt, R.M. Evidence for genetic involvement in dilated cardiomyopathy in the Irish Wolfhound. In Proceedings of the Annual Congress of BSAVA, Birmingham, UK, 15–18 September 1996. [Google Scholar]
- Dukes McEwan, J. Dilated cardiomyopathy in Newfoundlands. In Proceedings of the Veterinary Cardiovascular Society Meeting, Birmingham, UK; 1997. [Google Scholar]
- Tidholm, A.; Haggstrom, J.; Borgarelli, M.; Tarducci, A. Canine idiopathic dilated cardiomyopathy. Part I: Aetiology, clinical characteristics, epidemiology and pathology. Vet. J. 2001, 162, 92–107. [Google Scholar] [PubMed]
- Meurs, K.R. Insights into the hereditability of canine cardiomyopathy. Vet. Clin. N. Am.-Small Anim. Pract. 1998, 28, 1449–1457. [Google Scholar] [CrossRef]
- Dambach, D.M.; Lannon, A.; Sleeper, M.M.; Buchanan, J. Familial dilated cardiomyopathy of young Portuguese Water Dogs. J. Vet. Intern. Med. 1999, 13, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Meurs, K.M.; Miller, M.W.; Wright, N.A. Clinical features of dilated cardiomyopathy in Great Danes and results of a pedigree analysis: 17 cases (1990–2000). J. Am. Vet. Med. Assoc. 2001, 218, 729–732. [Google Scholar] [CrossRef] [PubMed]
- Cohen, N.; Muntoni, F. Multiple pathogenetic mechanisms in X linked dilated cardiomyopathy. Heart 2004, 90, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Counsell, J.R.; Asgarian, Z.; Meng, J.; Ferrer, V.; Vink, C.A.; Howe, S.J.; Waddington, S.N.; Thrasher, A.J.; Muntoni, F.; Morgan, J.E.; et al. Lentiviral vectors can be used for full-length dystrophin gene therapy. Sci. Rep. 2017, 7, 44775. [Google Scholar] [CrossRef] [PubMed]
- Farruggio, A.P.; Bhakta, M.S.; du Bois, H.; Ma, J.; Calos, M.P. Genomic integration of the full-length dystrophin coding sequence in Duchenne muscular dystrophy induced pluripotent stem cells. Biotechnol. J. 2017, 12. [Google Scholar] [CrossRef] [PubMed]
- Lu-Nguyen, N.; Malerba, A.; Popplewell, L.; Schnell, F.; Hanson, G.; Dickson, G. Systemic Antisense Therapeutics for Dystrophin and Myostatin Exon Splice Modulation Improve Muscle Pathology of Adult mdx Mice. Mol. Ther. Nucleic Acids 2017, 6, 15–28. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, M.; Ino, H.; Yasuda, T.; Fujino, N.; Uchiyama, K.; Mabuchi, T.; Konno, T.; Kaneda, T.; Fujita, T.; Masuta, E.; et al. Gene mutations in adult Japanese patients with dilated cardiomyopathy. Circ. J. 2005, 69, 150–153. [Google Scholar] [CrossRef] [PubMed]
- Arbustini, E.; Diegoli, M.; Morbini, P.; Dal Bello, B.; Banchieri, N.; Pilotto, A.; Magani, F.; Grasso, M.; Narula, J.; Gavazzi, A.; et al. Prevalence and characteristics of dystrophin defects in adult male patients with dilated cardiomyopathy. J. Am. Coll. Cardiol. 2000, 35, 1760–1768. [Google Scholar] [CrossRef]
- Deftereos, S.; Papoutsidakis, N.; Giannopoulos, G.; Angelidis, C.; Raisakis, K.; Bouras, G.; Davlouros, P.; Panagopoulou, V.; Goudevenos, J.; Cleman, M.W.; et al. Calcium Ions in Inherited Cardiomyopathies. Med. Chem. 2016, 12, 139–150. [Google Scholar] [CrossRef] [PubMed]
| Mutation/rs ID | Exon | Clinical Presentation/Frequency | Molecular/Cellular Effects | Reference |
|---|---|---|---|---|
| E96K/LOVD#0030558 | 10 | Familial DCM (age 5 months) | - | [58,59] |
| R131W/rs 483352833 | 11 | DCM diagnosed (age 23); SCD (age 16); heart failure death (age 34) | Enhanced cTnC-cTnI interaction while decreasing cTnC-cTnT interactions; decreased Ca2+ sensitivity; decreased ATPase activity | [56,60,61] |
| R134G/45525839 | 11 | Familial DCM (age 6) and heart transplant (by age 7) | increased maximal force development; no change in Ca2+ sensitivity | [52,58,60,62] |
| R139H | 11 | Late onset DCM (age 70) | Decreased Ca2+ sensitivity and maximal force development | [63] |
| R141W/rs 7315379 and rs 74315380 | 11 | Idiopathic DCM and Familial DCM; does not cause SCD | Increased affinity of cTnT to TPM; decreased Ca2+ sensitivity; decreased ATPase activity | [56,62,64] |
| R144W/rs 483352832 | 11 | Familial DCM with history of SCD; variability in severity within the family | Decreased ATPase activity | [65] |
| R151C/rs 45608937 | 11 | Idiopathic DCM | Decreased Ca2+ sensitivity | [52,60] |
| R159Q/rs 45501500 | 12 | Idiopathic DCM | Decreased Ca2+ sensitivity | [52,60] |
| A171S | 12 | Familial DCM and SCD (>age 20) | - | [66,67] |
| R173G | 12 | Familial DCM. Diagnosed at birth with dilated left ventricles (n = 2). Asymptomatic maternal uncle (age 45) and his cousin with mildly dilated left ventricle. | - | [68] |
| R173W | 12 | Familial DCM with dilated left ventricle, decreased ejection fraction and heart transplant (age 14) | Altered Ca2+ regulation; decreased contractility; sarcomere disorganization | [69,70] |
| R173Q | 12 | Dilated left ventricle at birth; SCD due to arrhythmia; asymptomatic dilated left ventricle | - | [68] |
| R205W/rs 45586240 | 14 | Idiopathic DCM (6 months) | Decreased Ca2+ sensitivity | [52,60] |
| R205L/rs 121964860 | 14 | Familial DCM | Impaired cTnI-cTnC and cTnC-cTnT interactions; decreased ATPase activity | [56,61] |
| ΔK210/rs 121964859 | 14 | Familial DCM; high incidence of SCD | Decreased Ca2+ sensitivity, maximal force and ATPase activity; impaired cTnC-cTnI and cTnC-cTnT interactions | [61,71,72,73,74] |
| E244D/rs 45466197 | 15 | Familial DCM, previously associated with HCM; idiopathic DCM (age 7), heart transplant required; mutation seen with A277V mutation in TPM1. Identified in one family. | - | [52,58,75] |
| D270N/rs 121964861 | 16 | Familial DCM (early death in n = 2 family members age 44 and 21) | Impaired cTnC-cTnI and cTnC-cTnT interactions; decreased Ca2+ sensitivity and ATPase activity | [61,76] |
| Mutation | Exon | Clinical Presentation | Molecular/Cellular Effects | Reference |
|---|---|---|---|---|
| I79N | 8 | Previously diagnosed in HCM with high incidence of SCD. Idiopathic DCM (age 68 and 64) | Disrupts the TPM binding domain of cTnT | [86,87] |
| R92W | 10 | Progression from HCM to DCM | - | [71,84] |
| R92Q | 10 | Mixed phenotype such as mild HCM, DCM with ventricular dysfunction and noncompaction; severe left ventricular dysfunction, dyspnea, chest pain and SCD (and SCD without clinical manifestation) | - | [88,89] |
| R113W | 10 | HCM, DCM and RCM | - | [62,90,91] |
| K273E | 16 | Transition from FHC to DCM during disease progression; initially asymmetrical septal hypertrophy with disease progression to DCM; high incidence of SCD | Decreased ATPase activity and Ca2+ sensitivity, impaired force production | [85] |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
England, J.; Loughna, S.; Rutland, C.S. Multiple Species Comparison of Cardiac Troponin T and Dystrophin: Unravelling the DNA behind Dilated Cardiomyopathy. J. Cardiovasc. Dev. Dis. 2017, 4, 8. https://doi.org/10.3390/jcdd4030008
England J, Loughna S, Rutland CS. Multiple Species Comparison of Cardiac Troponin T and Dystrophin: Unravelling the DNA behind Dilated Cardiomyopathy. Journal of Cardiovascular Development and Disease. 2017; 4(3):8. https://doi.org/10.3390/jcdd4030008
Chicago/Turabian StyleEngland, Jennifer, Siobhan Loughna, and Catrin Sian Rutland. 2017. "Multiple Species Comparison of Cardiac Troponin T and Dystrophin: Unravelling the DNA behind Dilated Cardiomyopathy" Journal of Cardiovascular Development and Disease 4, no. 3: 8. https://doi.org/10.3390/jcdd4030008





