Recent Advances in the Development of Biomimetic Materials
Abstract
:1. Introduction
2. Rationale for Biomimetic Materials Design
2.1. The Role of Mechanical Properties
2.2. Extracellular Matrix Mimicry
3. Hydrogels
Self-Assembling Peptides

4. Collagen-Based Materials
5. Surface Modification
5.1. Physical Surface Modifications
5.2. Chemical Surface Modifications
6. 2D and 3D Fabrication Techniques
Advances and Limitations in 3D Bioprinting
7. Artificial Intelligence (AI) Implications and Future Perspective
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Naik, R.R.; Singamaneni, S. Introduction: Bioinspired and Biomimetic Materials. Chem. Rev. 2017, 117, 12581–12583. [Google Scholar] [CrossRef] [PubMed]
- Rowley, T. Science imitates life. Lab Anim. 2013, 42, 271–272. [Google Scholar] [CrossRef] [PubMed]
- Glaser, D.E.; Viney, C. Biomimetic Materials. In Biomaterials Science; Elsevier: Amsterdam, The Netherlands, 2013; pp. 349–360. [Google Scholar]
- Atala, A.; Kasper, F.K.; Mikos, A.G. Engineering Complex Tissues. Sci. Transl. Med. 2012, 4, 160rv12. [Google Scholar] [CrossRef] [PubMed]
- Lavik, E.B.; Zheng, G. (Eds.) Biomimetic Materials. Bioconjug. Chem. 2018, 29, 825. [Google Scholar] [CrossRef]
- Liebschner, M.; Bucklen, B.; Wettergreen, M. Mechanical Aspects of Tissue Engineering. Semin. Plast. Surg. 2005, 19, 217–228. [Google Scholar] [CrossRef]
- Mantha, S.; Pillai, S.; Khayambashi, P.; Upadhyay, A.; Zhang, Y.; Tao, O.; Pham, H.M.; Tran, S.D. Smart Hydrogels in Tissue Engineering and Regenerative Medicine. Materials 2019, 12, 3323. [Google Scholar] [CrossRef]
- Koutsopoulos, S. Self-assembling peptide nanofiber hydrogels in tissue engineering and regenerative medicine: Progress, design guidelines, and applications. J. Biomed. Mater. Res. Part A 2016, 104, 1002–1016. [Google Scholar] [CrossRef]
- Thomson, J.A. On Growth and Form, 2nd ed.; Cambridge University Press: Cambridge, UK, 1968. [Google Scholar]
- Currey, J.D. Bones: Structure and Mechanics; Princeton University Press: Princeton, NJ, USA, 2002; ISBN 9780691128047. [Google Scholar]
- Vincent, J.F.V. Structural Biomaterials; Princeton University Press: Princeton, NJ, USA; Available online: https://press.princeton.edu/books/paperback/9780691154008/structural-biomaterials (accessed on 29 July 2012).
- Muiznieks, L.D.; Keeley, F.W. Molecular assembly and mechanical properties of the extracellular matrix: A fibrous protein perspective. Biochim. Biophys. Acta Mol. Basis Dis. 2013, 1832, 866–875. [Google Scholar] [CrossRef]
- Coenen, A.M.J.; Bernaerts, K.V.; Harings, J.A.W.; Jockenhoevel, S.; Ghazanfari, S. Elastic materials for tissue engineering applications: Natural, synthetic, and hybrid polymers. Acta Biomater. 2018, 79, 60–82. [Google Scholar] [CrossRef]
- Guz, N.; Dokukin, M.; Kalaparthi, V.; Sokolov, I. If Cell Mechanics Can Be Described by Elastic Modulus: Study of Different Models and Probes Used in Indentation Experiments. Biophys. J. 2014, 107, 564–575. [Google Scholar] [CrossRef]
- Radmacher, M.; Fritz, M.; Kacher, C.M.; Cleveland, J.P.; Hansma, P.K. Measuring the viscoelastic properties of human platelets with the atomic force microscope. Biophys. J. 1996, 70, 556–567. [Google Scholar] [CrossRef]
- Karimi, A.; Shojaei, A. Measurement of the Mechanical Properties of the Human Kidney. IRBM 2017, 38, 292–297. [Google Scholar] [CrossRef]
- Vogel, H. Influence of maturation and aging on mechanical and biochemical properties of connective tissue in rats. Mech. Ageing Dev. 1980, 14, 283–292. [Google Scholar] [CrossRef]
- Buchanan, C.I.; Marsh, R.L. Effects of long-term exercise on the biomechanical properties of the Achilles tendon of guinea fowl. J. Appl. Physiol. 2001, 90, 164–171. [Google Scholar] [CrossRef]
- Wren, T.A.; Yerby, S.A.; Beaupré, G.S.; Carter, D.R. Mechanical properties of the human achilles tendon. Clin. Biomech. 2001, 16, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Gosline, J.; Lillie, M.; Carrington, E.; Guerette, P.; Ortlepp, C.; Savage, K. Elastic proteins: Biological roles and mechanical properties. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2002, 357, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Varanko, A.K.; Su, J.C.; Chilkoti, A. Elastin-Like Polypeptides for Biomedical Applications. Annu. Rev. Biomed. Eng. 2020, 22, 343–369. [Google Scholar] [CrossRef]
- Wu, D.; Isaksson, P.; Ferguson, S.J.; Persson, C. Young’s modulus of trabecular bone at the tissue level: A review. Acta Biomater. 2018, 78, 1–12. [Google Scholar] [CrossRef]
- Taberlet, N.; Ferrand, J.; Camus, É.; Lachaud, L.; Plihon, N. How tall can gelatin towers be? An introduction to elasticity and buckling. Am. J. Phys. 2017, 85, 908–914. [Google Scholar] [CrossRef]
- Parmar, P.A.; Chow, L.W.; St-Pierre, J.-P.; Horejs, C.-M.; Peng, Y.Y.; Werkmeister, J.A.; Ramshaw, J.A.M.; Stevens, M.M. Collagen-mimetic peptide-modifiable hydrogels for articular cartilage regeneration. Biomaterials 2015, 54, 213–225. [Google Scholar] [CrossRef]
- Ciulla, M.G.; Pugliese, R.; Gelain, F. Boosted Cross-Linking and Characterization of High-Performing Self-Assembling Peptides. Nanomaterials 2022, 12, 320. [Google Scholar] [CrossRef] [PubMed]
- Kaya, G.; Oytun, F. Rheological Properties of İnjectable Hyaluronic Acid Hydrogels for Soft Tissue Engineering Applications. Biointerface Res. Appl. Chem. 2020, 11, 8424–8430. [Google Scholar] [CrossRef]
- Heris, H.K.; Rahmat, M.; Mongeau, L. Characterization of a Hierarchical Network of Hyaluronic Acid/Gelatin Composite for use as a Smart Injectable Biomaterial. Macromol. Biosci. 2012, 12, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Adler-Abramovich, L.; Gazit, E. The physical properties of supramolecular peptide assemblies: From building block association to technological applications. Chem. Soc. Rev. 2014, 43, 6881–6893. [Google Scholar] [CrossRef] [PubMed]
- Malektaj, H.; Drozdov, A.D.; deClaville Christiansen, J. Mechanical Properties of Alginate Hydrogels Cross-Linked with Multivalent Cations. Polymers 2023, 15, 3012. [Google Scholar] [CrossRef]
- Pugliese, R.; Marchini, A.; Saracino, G.A.A.; Zuckermann, R.N.; Gelain, F. Cross-linked self-assembling peptide scaffolds. Nano Res. 2018, 11, 586–602. [Google Scholar] [CrossRef]
- Le, H.R.; Qu, S.; Mackay, R.E.; Rothwell, R. Fabrication and mechanical properties of chitosan composite membrane containing hydroxyapatite particles. J. Adv. Ceram. 2012, 1, 66–71. [Google Scholar] [CrossRef]
- Velasquez, S.T.R.; Jang, D.; Jenkins, P.; Liu, P.; Yang, L.; Korley, L.T.J.; Bruns, N. Peptide-Reinforced Amphiphilic Polymer Conetworks. Adv. Funct. Mater. 2022, 32, 2207317. [Google Scholar] [CrossRef]
- Wu, Y.; Xiang, Y.; Fang, J.; Li, X.; Lin, Z.; Dai, G.; Yin, J.; Wei, P.; Zhang, D. The influence of the stiffness of GelMA substrate on the outgrowth of PC12 cells. Biosci. Rep. 2019, 39, BSR20181748. [Google Scholar] [CrossRef]
- Wenger, M.P.E.; Bozec, L.; Horton, M.A.; Mesquida, P. Mechanical Properties of Collagen Fibrils. Biophys. J. 2007, 93, 1255–1263. [Google Scholar] [CrossRef]
- Hoeve, C.A.J.; Flory, P.J. The elastic properties of elastin. Biopolymers 1974, 13, 677–686. [Google Scholar] [CrossRef]
- Trębacz, H.; Barzycka, A. Mechanical Properties and Functions of Elastin: An Overview. Biomolecules 2023, 13, 574. [Google Scholar] [CrossRef]
- Saitow, C.B.; Wise, S.G.; Weiss, A.S.; Castellot, J.J.; Kaplan, D.L. Elastin biology and tissue engineering with adult cells. Biomol. Concepts 2013, 4, 173–185. [Google Scholar] [CrossRef] [PubMed]
- Daamen, W.; Veerkamp, J.; Vanhest, J.; Vankuppevelt, T. Elastin as a biomaterial for tissue engineering. Biomaterials 2007, 28, 4378–4398. [Google Scholar] [CrossRef] [PubMed]
- Aaron, B.B.; Gosline, J.M. Elastin as a random-network elastomer: A mechanical and optical analysis of single elastin fibers. Biopolymers 1981, 20, 1247–1260. [Google Scholar] [CrossRef]
- Debelle, L.; Tamburro, A.M. Elastin: Molecular description and function. Int. J. Biochem. Cell Biol. 1999, 31, 261–272. [Google Scholar] [CrossRef]
- Li, B.; Alonso, D.O.V.; Bennion, B.J.; Daggett, V. Hydrophobic Hydration Is an Important Source of Elasticity in Elastin-Based Biopolymers. J. Am. Chem. Soc. 2001, 123, 11991–11998. [Google Scholar] [CrossRef]
- Luo, T.; Kiick, K.L. Collagen-like peptides and peptide–polymer conjugates in the design of assembled materials. Eur. Polym. J. 2013, 49, 2998–3009. [Google Scholar] [CrossRef]
- Ciulla, M.G.; Civera, M.; Sattin, S.; Kumar, K. Nature-inspired and medicinally relevant short peptides. Explor. Drug Sci. 2023, 1, 140–171. [Google Scholar] [CrossRef]
- Zhao, B.; Li, N.K.; Yingling, Y.G.; Hall, C.K. LCST Behavior is Manifested in a Single Molecule: Elastin-Like polypeptide (VPGVG) n. Biomacromolecules 2016, 17, 111–118. [Google Scholar] [CrossRef]
- Betre, H.; Ong, S.R.; Guilak, F.; Chilkoti, A.; Fermor, B.; Setton, L.A. Chondrocytic differentiation of human adipose-derived adult stem cells in elastin-like polypeptide. Biomaterials 2006, 27, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Trabbic-Carlson, K.; Setton, L.A.; Chilkoti, A. Swelling and Mechanical Behaviors of Chemically Cross-Linked Hydrogels of Elastin-like Polypeptides. Biomacromolecules 2003, 4, 572–580. [Google Scholar] [CrossRef] [PubMed]
- Lim, D.W.; Nettles, D.L.; Setton, L.A.; Chilkoti, A. Rapid Cross-Linking of Elastin-like Polypeptides with (Hydroxymethyl)phosphines in Aqueous Solution. Biomacromolecules 2007, 8, 1463–1470. [Google Scholar] [CrossRef]
- Hrabchak, C.; Rouleau, J.; Moss, I.; Woodhouse, K.; Akens, M.; Bellingham, C.; Keeley, F.; Dennis, M.; Yee, A. Assessment of biocompatibility and initial evaluation of genipin cross-linked elastin-like polypeptides in the treatment of an osteochondral knee defect in rabbits. Acta Biomater. 2010, 6, 2108–2115. [Google Scholar] [CrossRef] [PubMed]
- Mozhdehi, D.; Luginbuhl, K.M.; Simon, J.R.; Dzuricky, M.; Berger, R.; Varol, H.S.; Huang, F.C.; Buehne, K.L.; Mayne, N.R.; Weitzhandler, I.; et al. Genetically encoded lipid–polypeptide hybrid biomaterials that exhibit temperature-triggered hierarchical self-assembly. Nat. Chem. 2018, 10, 496–505. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, R.; Maleki, M.; Zuckermann, R.N.; Gelain, F. Self-assembling peptides cross-linked with genipin: Resilient hydrogels and self-standing electrospun scaffolds for tissue engineering applications. Biomater. Sci. 2019, 7, 76–91. [Google Scholar] [CrossRef]
- Pugliese, R.; Fontana, F.; Marchini, A.; Gelain, F. Branched peptides integrate into self-assembled nanostructures and enhance biomechanics of peptidic hydrogels. Acta Biomater. 2018, 66, 258–271. [Google Scholar] [CrossRef]
- Pugliese, R.; Montuori, M.; Gelain, F. Bioinspired photo-crosslinkable self-assembling peptides with pH-switchable “on–off” luminescence. Nanoscale Adv. 2022, 4, 447–456. [Google Scholar] [CrossRef]
- Chronopoulou, L.; Margheritelli, S.; Toumia, Y.; Paradossi, G.; Bordi, F.; Sennato, S.; Palocci, C. Biosynthesis and Characterization of Cross-Linked Fmoc Peptide-Based Hydrogels for Drug Delivery Applications. Gels 2015, 1, 179–193. [Google Scholar] [CrossRef]
- Chronopoulou, L.; Toumia, Y.; Cerroni, B.; Pandolfi, D.; Paradossi, G.; Palocci, C. Biofabrication of genipin-crosslinked peptide hydrogels and their use in the controlled delivery of naproxen. New Biotechnol. 2017, 37, 138–143. [Google Scholar] [CrossRef]
- Pugliese, R. Supramolecular-Covalent Peptides Self-Assembly: From Design to Regenerative Medicine and Beyond. Biophysica 2022, 2, 324–339. [Google Scholar] [CrossRef]
- Gaar, J.; Naffa, R.; Brimble, M. Enzymatic and non-enzymatic crosslinks found in collagen and elastin and their chemical synthesis. Org. Chem. Front. 2020, 7, 2789–2814. [Google Scholar] [CrossRef]
- Ciulla, M.G.; Marchini, A.; Gazzola, J.; Sambrotta, M.; Gelain, F. Low-Power Microwaves: A Cell-Compatible Physical Treatment to Enhance Self-Assembling Peptides Mechanical Propertie. Nanoscale 2023, 15, 15840–15854. [Google Scholar] [CrossRef] [PubMed]
- Ma, P.X. Biomimetic materials for tissue engineering. Adv. Drug Deliv. Rev. 2008, 60, 184–198. [Google Scholar] [CrossRef]
- Ma, P.X. Scaffolds for tissue fabrication. Mater. Today 2004, 7, 30–40. [Google Scholar] [CrossRef]
- Chan, B.P.; Leong, K.W. Scaffolding in tissue engineering: General approaches and tissue-specific considerations. Eur. Spine J. 2008, 17, 467–479. [Google Scholar] [CrossRef]
- Montaseri, Z.; Abolmaali, S.S.; Tamaddon, A.M.; Farvadi, F. Composite silk fibroin hydrogel scaffolds for cartilage tissue regeneration. J. Drug Deliv. Sci. Technol. 2023, 79, 104018. [Google Scholar] [CrossRef]
- Wess, T.J. Collagen Fibril Form and Function. Adv. Protein Chem. 2005, 70, 341–374. [Google Scholar] [PubMed]
- Hodge, A.J.; Petruska, J.A. Recent studies with the electron microscope on ordered aggregates of the tropocollagen molecules. In Aspects of Protein Structure; Ramachandran, G.N., Ed.; Academic Press: New York, NY, USA, 1963; pp. 289–300. [Google Scholar]
- Ottani, V.; Raspanti, M.; Ruggeri, A. Collagen structure and functional implications. Micron 2001, 32, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Abune, L.; Lee, K.; Wang, Y. Development of a Biomimetic Extracellular Matrix with Functions of Protein Sequestration and Cell Attachment Using Dual Aptamer-Functionalized Hydrogels. ACS Biomater. Sci. Eng. 2022, 8, 1279–1289. [Google Scholar] [CrossRef]
- Hoare, T.R.; Kohane, D.S. Hydrogels in drug delivery: Progress and challenges. Polymer 2008, 49, 1993–2007. [Google Scholar] [CrossRef]
- Richter, A.; Paschew, G.; Klatt, S.; Lienig, J.; Arndt, K.; Adler, H.P. Review on Hydrogel-based pH Sensors and Microsensors. Sensors 2008, 8, 561–581. [Google Scholar] [CrossRef]
- Tan, H.; Marra, K.G. Injectable, Biodegradable Hydrogels for Tissue Engineering Applications. Materials 2010, 3, 1746–1767. [Google Scholar] [CrossRef]
- Nicolson, P.C. Soft contact lens polymers: An evolution. Biomacromolecules 2001, 22, 3273–3283. [Google Scholar] [CrossRef]
- Films, G.H.; Xu, Y.; Lin, Z.; Huang, X.; Liu, Y.; Huang, Y.; Duan, X. Flexible Solid-State Supercapacitors Based on Three-Dimensional. ACS Nano 2013, 7, 4042–4049. [Google Scholar] [CrossRef]
- Caló, E.; Khutoryanskiy, V.V. Biomedical applications of hydrogels: A review of patents and commercial products. Eur. Polym. J. 2015, 65, 252–267. [Google Scholar] [CrossRef]
- Burdick, J.A.; Prestwich, G.D. Hyaluronic acid hydrogels for biomedical applications. Adv. Mater. 2011, 23, 41–56. [Google Scholar] [CrossRef]
- Hoffman, A.S. Hydrogels for biomedical applications. Adv. Drug Deliv. Rev. 2012, 64, 18–23. [Google Scholar] [CrossRef]
- Suresh Kumar, N.; Padma Suvarna, R.; Chandra Babu Naidu, K.; Banerjee, P.; Ratnamala, A.; Manjunatha, H. A review on biological and biomimetic materials and their applications. Appl. Phys. A Mater. Sci. Process. 2020, 126, 445. [Google Scholar] [CrossRef]
- Cecen, B.; Bal-Ozturk, A.; Yasayan, G.; Alarcin, E.; Kocak, P.; Tutar, R.; Kozaci, L.D.; Shin, S.R.; Miri, A.K. Selection of natural biomaterials for micro-tissue and organ-on-chip models. J. Biomed. Mater. Res. Part A 2022, 110, 1147–1165. [Google Scholar] [CrossRef]
- Li, Y.; Tian, H.; Chen, X. Hyaluronic acid based injectable hydrogels for localized and sustained gene delivery. J. Control. Release 2015, 213, e140–e141. [Google Scholar] [CrossRef]
- Muşat, V.; Anghel, E.M.; Zaharia, A.; Atkinson, I.; Mocioiu, O.C.; Buşilă, M.; Alexandru, P. A chitosan–agarose polysaccharide-based hydrogel for biomimetic remineralization of dental enamel. Biomolecules 2021, 11, 1137. [Google Scholar] [CrossRef]
- Tran, T.T.; Hamid, Z.A.; Cheong, K.Y. A Review of Mechanical Properties of Scaffold in Tissue Engineering: Aloe Vera Composites. In Journal of Physics: Conference Series; IOP Publishing: Bristol, UK, 2018; Volume 1082. [Google Scholar]
- Khan, Y.; Bashir, S.; Hina, M.; Ramesh, S.; Ramesh, K.; Lahiri, I. Effect of Salt Concentration on Poly (Acrylic Acid) Hydrogel Electrolytes and their Applications in Supercapacitor. J. Electrochem. Soc. 2020, 167, 100524. [Google Scholar] [CrossRef]
- Wang, H.; Chen, Z.; Cheng, S.; Li, R.; Pan, X.; Zhang, C.; Gu, H.; Xie, A.; Dong, W. Synthesis of cationic hydrogels with tunable physicochemical properties for antibacterial applications. Eur. Polym. J. 2022, 173, 111228. [Google Scholar] [CrossRef]
- Wang, T.; Jones, J.D.; Niyonshuti, I.I.; Agrawal, S.; Gundampati, R.K.; Kumar, T.K.S.; Quinn, K.P.; Chen, J. Biocompatible, Injectable Anionic Hydrogels Based on Poly(Oligo Ethylene Glycol Monoacrylate- co -Acrylic Acid) for Protein Delivery. Adv. Ther. 2019, 2, 1900092. [Google Scholar] [CrossRef]
- Chang, R.Y.K.; Okamoto, Y.; Morales, S.; Kutter, E.; Chan, H.-K. Hydrogel formulations containing non-ionic polymers for topical delivery of bacteriophages. Int. J. Pharm. 2021, 605, 120850. [Google Scholar] [CrossRef] [PubMed]
- He, H.; Xiao, Z.; Zhou, Y.; Chen, A.; Xuan, X.; Li, Y.; Guo, X.; Zheng, J.; Xiao, J.; Wu, J. Zwitterionic poly(sulfobetaine methacrylate) hydrogels with optimal mechanical properties for improving wound healing in vivo. J. Mater. Chem. B 2019, 7, 1697–1707. [Google Scholar] [CrossRef] [PubMed]
- Iizawa, T.; Ninomiya, T.; Gotoh, T.; Sakohara, S. Synthesis of Porous Poly(N-isopropylacrylamide) Gel Beads by Sedimentation Polymerization. Polym. J. 2004, 36, 356–360. [Google Scholar] [CrossRef]
- Singh, M.R.; Patel, S.; Singh, D. Natural polymer-based hydrogels as scaffolds for tissue engineering. In Nanobiomaterials in Soft Tissue Engineering; Elsevier: Amsterdam, The Netherlands, 2016; pp. 231–260. [Google Scholar]
- Krstic, M.; Rogic Miladinovic, Z.; Barudzija, T.; Mladenovic, A.; Suljovrujic, E. Stimuli-responsive copolymeric hydrogels based on oligo(ethylene glycol) dimethacrylate for biomedical applications: An optimisation study of pH and thermoresponsive behaviour. React. Funct. Polym. 2022, 170, 105140. [Google Scholar] [CrossRef]
- Yan, C.; Altunbas, A.; Yucel, T.; Nagarkar, R.P.; Schneider, J.P.; Pochan, D.J. Injectable solid hydrogel: Mechanism of shear-thinning and immediate recovery of injectable β-hairpin peptide hydrogels. Soft Matter 2010, 6, 5143. [Google Scholar] [CrossRef]
- Ghorbanizamani, F.; Moulahoum, H.; Guler Celik, E.; Timur, S. Ionic liquids enhancement of hydrogels and impact on biosensing applications. J. Mol. Liq. 2022, 357, 119075. [Google Scholar] [CrossRef]
- Baus, R.A.; Zahir-Jouzdani, F.; Dünnhaupt, S.; Atyabi, F.; Bernkop-Schnürch, A. Mucoadhesive hydrogels for buccal drug delivery: In vitro-in vivo correlation study. Eur. J. Pharm. Biopharm. 2019, 142, 498–505. [Google Scholar] [CrossRef]
- Janes, K.A.; Fresneau, M.P.; Marazuela, A.; Fabra, A.; Alonso, M.J. Chitosan nanoparticles as delivery systems for doxorubicin. J. Control. Release 2001, 73, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Ono, K.; Saito, Y.; Yura, H.; Ishikawa, K.; Kurita, A.; Akaike, T.; Ishihara, M. Photocrosslinkable chitosan as a biological adhesive. J. Biomed. Mater. Res. 2000, 49, 289–295. [Google Scholar] [CrossRef]
- ITO, T.; YEO, Y.; HIGHLEY, C.; BELLAS, E.; KOHANE, D. Dextran-based in situ cross-linked injectable hydrogels to prevent peritoneal adhesions. Biomaterials 2007, 28, 3418–3426. [Google Scholar] [CrossRef]
- Riacci, L.; Sorriento, A.; Ricotti, L. Genipin-based crosslinking of jellyfish collagen 3D hydrogels. Gels 2021, 7, 238. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Yu, L.; Wang, S.; Zhang, L.; Chen, L.; Xu, X.; Song, Z.; Liu, H.; Chen, C. Strong, tough, ionic conductive, and freezing-tolerant all-natural hydrogel enabled by cellulose-bentonite coordination interactions. Nat. Commun. 2022, 13, 3408. [Google Scholar] [CrossRef] [PubMed]
- Nasution, H.; Harahap, H.; Dalimunthe, N.F.; Ginting, M.H.S.; Jaafar, M.; Tan, O.O.H.; Aruan, H.K.; Herfananda, A.L. Hydrogel and Effects of Crosslinking Agent on Cellulose-Based Hydrogels: A Review. Gels 2022, 8, 568. [Google Scholar] [CrossRef]
- Huang, C.; Ye, Q.; Dong, J.; Li, L.; Wang, M.; Zhang, Y.; Zhang, Y.; Wang, X.; Wang, P.; Jiang, Q. Biofabrication of natural Au/bacterial cellulose hydrogel for bone tissue regeneration via in-situ fermentation. Smart Mater. Med. 2023, 4, 1–14. [Google Scholar] [CrossRef]
- Massironi, A.; Franco, A.R.; Babo, P.S.; Puppi, D.; Chiellini, F.; Reis, R.L.; Gomes, M.E. Development and Characterization of Highly Stable Silver NanoParticles as Novel Potential Antimicrobial Agents for Wound Healing Hydrogels. Int. J. Mol. Sci. 2022, 23, 2161. [Google Scholar] [CrossRef]
- Trappmann, B.; Chen, C.S. How cells sense extracellular matrix stiffness: A material’s perspective. Curr. Opin. Biotechnol. 2013, 24, 948–953. [Google Scholar] [CrossRef]
- Leng, Y.; Abdullah, A.; Wendt, M.K.; Calve, S. Hyaluronic acid, CD44 and RHAMM regulate myoblast behavior during embryogenesis. Matrix Biol. 2019, 78–79, 236–254. [Google Scholar] [CrossRef] [PubMed]
- Nakod, P.S.; Kim, Y.; Rao, S.S. Three-dimensional biomimetic hyaluronic acid hydrogels to investigate glioblastoma stem cell behaviors. Biotechnol. Bioeng. 2020, 117, 511–522. [Google Scholar] [CrossRef] [PubMed]
- Antich, C.; de Vicente, J.; Jiménez, G.; Chocarro, C.; Carrillo, E.; Montañez, E.; Gálvez-Martín, P.; Marchal, J.A. Bio-inspired hydrogel composed of hyaluronic acid and alginate as a potential bioink for 3D bioprinting of articular cartilage engineering constructs. Acta Biomater. 2020, 106, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Almeida, L.D.F.; Babo, P.S.; Silva, C.R.; Rodrigues, M.T.; Hebling, J.; Reis, R.L.; Gomes, M.E. Hyaluronic acid hydrogels incorporating platelet lysate enhance human pulp cell proliferation and differentiation. J. Mater. Sci. Mater. Med. 2018, 29, 88. [Google Scholar] [CrossRef]
- Levin, A.; Hakala, T.A.; Schnaider, L.; Bernardes, G.J.L.; Gazit, E.; Knowles, T.P.J. Biomimetic peptide self-assembly for functional materials. Nat. Rev. Chem. 2020, 4, 615–634. [Google Scholar] [CrossRef]
- Issaka, E.; Wariboko, M.A.; Agyekum, E.A. Synergy and Coordination between Biomimetic Nanoparticles and Biological Cells/Tissues/Organs/Systems: Applications in Nanomedicine and Prospect; Springer: New York, NY, USA, 2023; ISBN 0123456789. [Google Scholar]
- Hosoyama, K.; Lazurko, C.; Muñoz, M.; McTiernan, C.D.; Alarcon, E.I. Peptide-based functional biomaterials for soft-tissue repair. Front. Bioeng. Biotechnol. 2019, 7, 205. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, R.; Gelain, F. Peptidic Biomaterials: From Self-Assembling to Regenerative Medicine. Trends Biotechnol. 2017, 35, 145–158. [Google Scholar] [CrossRef]
- Aulisa, L.; Dong, H.; Hartgerink, J.D. Self-Assembly of Multidomain Peptides: Sequence Variation Allows Control over Cross-Linking and Viscoelasticity. Biomacromolecules 2009, 10, 2694–2698. [Google Scholar] [CrossRef]
- Zhang, S. Self-assembling peptides: From a discovery in a yeast protein to diverse uses and beyond. Protein Sci. 2020, 29, 2281–2303. [Google Scholar] [CrossRef]
- Zhang, S.; Altman, M. Peptide self-assembly in functional polymer science and engineering. React. Funct. Polym. 1999, 41, 91–102. [Google Scholar] [CrossRef]
- Gelain, F.; Luo, Z.; Zhang, S. Self-Assembling Peptide EAK16 and RADA16 Nanofiber Scaffold Hydrogel. Chem. Rev. 2020, 120, 13434–13460. [Google Scholar] [CrossRef] [PubMed]
- Kisiday, J.; Jin, M.; Kurz, B.; Hung, H.; Semino, C.; Zhang, S.; Grodzinsky, A.J. Self-assembling peptide hydrogel fosters chondrocyte extracellular matrix production and cell division: Implications for cartilage tissue repair. Proc. Natl. Acad. Sci. USA 2002, 99, 9996–10001. [Google Scholar] [CrossRef]
- Gelain, F.; Silva, D.; Caprini, A.; Taraballi, F.; Natalello, A.; Villa, O.; Nam, K.T.; Zuckermann, R.N.; Doglia, S.M.; Vescovi, A. BMHP1-derived self-assembling peptides: Hierarchically assembled structures with self-healing propensity and potential for tissue engineering applications. ACS Nano 2011, 5, 1845–1859. [Google Scholar] [CrossRef] [PubMed]
- Ciulla, M.G.; Fontana, F.; Lorenzi, R.; Marchini, A.; Campone, L.; Sadeghi, E.; Paleari, A.; Sattin, S.; Gelain, F. Novel self-assembling cyclic peptides with reversible supramolecular nanostructures. Mater. Chem. Front. 2023. [Google Scholar] [CrossRef]
- Yang, M.; Xing, R.; Shen, G.; Yuan, C.; Yan, X. A versatile cyclic dipeptide hydrogelator: Self-assembly and rheology in various physiological conditions. Colloids Surfaces A Physicochem. Eng. Asp. 2019, 572, 259–265. [Google Scholar] [CrossRef]
- Insua, I.; Montenegro, J. 1D to 2D Self Assembly of Cyclic Peptides. J. Am. Chem. Soc. 2020, 142, 300–307. [Google Scholar] [CrossRef]
- Dehsorkhi, A.; Castelletto, V.; Hamley, I.W. Self-assembling amphiphilic peptides. J. Pept. Sci. 2014, 20, 453–467. [Google Scholar] [CrossRef] [PubMed]
- Hendricks, M.P.; Sato, K.; Palmer, L.C.; Stupp, S.I. Supramolecular Assembly of Peptide Amphiphiles. Acc. Chem. Res. 2017, 50, 2440–2448. [Google Scholar] [CrossRef]
- Lopez-Silva, T.L.; Leach, D.G.; Li, I.-C.; Wang, X.; Hartgerink, J.D. Self-Assembling Multidomain Peptides: Design and Characterization of Neutral Peptide-Based Materials with pH and Ionic Strength Independent Self-Assembly. ACS Biomater. Sci. Eng. 2019, 5, 977–985. [Google Scholar] [CrossRef] [PubMed]
- Marchini, A.; Raspa, A.; Pugliese, R.; Abd El Malek, M.; Pastori, V.; Lecchi, M.; Vescovi, A.L.; Gelain, F. Multifunctionalized hydrogels foster hNSC maturation in 3D cultures and neural regeneration in spinal cord injuries. Proc. Natl. Acad. Sci. USA 2019, 116, 7483–7492. [Google Scholar] [CrossRef] [PubMed]
- Marchini, A.; Ciulla, M.G.; Antonioli, B.; Agnoli, A.; Bovio, U.; Visnoviz, V.; Bertuzzi, F.; Gelain, F. Long-term cultures of human pancreatic islets in self-assembling peptides hydrogels. Front. Bioeng. Biotechnol. 2023, 11, 1105157. [Google Scholar] [CrossRef] [PubMed]
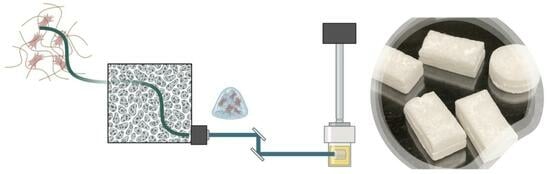
- Forouharshad, M.; Raspa, A.; Marchini, A.; Ciulla, M.G.; Magnoni, A.; Gelain, F. Biomimetic Electrospun Self-Assembling Peptide Scaffolds for Neural Stem Cell Transplantation in Neural Tissue Engineering. Pharmaceutics 2023, 15, 2261. [Google Scholar] [CrossRef] [PubMed]
- Standley, S.M.; Toft, D.J.; Cheng, H.; Soukasene, S.; Chen, J.; Raja, S.M.; Band, V.; Band, H.; Cryns, V.L.; Stupp, S.I. Induction of Cancer Cell Death by Self-assembling Nanostructures Incorporating a Cytotoxic Peptide. Cancer Res. 2010, 70, 3020–3026. [Google Scholar] [CrossRef]
- Kumar, V.B.; Ozguney, B.; Vlachou, A.; Chen, Y.; Gazit, E.; Tamamis, P. Peptide Self-Assembled Nanocarriers for Cancer Drug Delivery. J. Phys. Chem. B 2023, 127, 1857–1871. [Google Scholar] [CrossRef]
- Hernandez, A.; Hartgerink, J.D.; Young, S. Self-assembling peptides as immunomodulatory biomaterials. Front. Bioeng. Biotechnol. 2023, 11, 1139782. [Google Scholar] [CrossRef]
- Ciulla, M.G.; Gelain, F. Structure-Activity Relationships of Antibacterial Peptides. Microb. Biotechnol. 2023, 16, 757–777. [Google Scholar] [CrossRef]
- Yang, J.; An, H.-W.; Wang, H. Self-Assembled Peptide Drug Delivery Systems. ACS Appl. Bio Mater. 2021, 4, 24–46. [Google Scholar] [CrossRef]
- Tikhonova, T.N.; Cohen-Gerassi, D.; Arnon, Z.A.; Efremov, Y.; Timashev, P.; Adler-Abramovich, L.; Shirshin, E.A. Tunable Self-Assembled Peptide Hydrogel Sensor for Pharma Cold Supply Chain. ACS Appl. Mater. Interfaces 2022, 14, 55392–55401. [Google Scholar] [CrossRef]
- Deng, D.; Chang, Y.; Liu, W.; Ren, M.; Xia, N.; Hao, Y. Advancements in Biosensors Based on the Assembles of Small Organic Molecules and Peptides. Biosensors 2023, 13, 773. [Google Scholar] [CrossRef]
- Farsheed, A.C.; Thomas, A.J.; Pogostin, B.H.; Hartgerink, J.D. 3D Printing of Self-Assembling Nanofibrous Multidomain Peptide Hydrogels. Adv. Mater. 2023, 35, 2210378. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.-J.; Cheng, J.; Zhang, L.-Y.; Zhang, J.-G. Self-assembling peptides-based nano-cargos for targeted chemotherapy and immunotherapy of tumors: Recent developments, challenges, and future perspectives. Drug Deliv. 2022, 29, 1184–1200. [Google Scholar] [CrossRef]
- Peng, F.; Zhang, W.; Qiu, F. Self-assembling Peptides in Current Nanomedicine: Versatile Nanomaterials for Drug Delivery. Curr. Med. Chem. 2020, 27, 4855–4881. [Google Scholar] [CrossRef] [PubMed]
- Das, A.K.; Gavel, P.K. Low molecular weight self-assembling peptide-based materials for cell culture, antimicrobial, anti-inflammatory, wound healing, anticancer, drug delivery, bioimaging and 3D bioprinting applications. Soft Matter 2020, 16, 10065–10095. [Google Scholar] [CrossRef] [PubMed]
- Bong, D.T.; Clark, T.D.; Granja, J.R.; Ghadiri, M.R. Self-Assembling Organic Nanotubes. Angew. Chemie Int. Ed. 2001, 40, 988–1011. [Google Scholar] [CrossRef]
- Ma, M.; Stoyanova, M.; Rademacher, G.; Dutcher, S.K.; Brown, A.; Zhang, R. Structure of the Decorated Ciliary Doublet Microtubule. Cell 2019, 179, 909–922.e12. [Google Scholar] [CrossRef]
- Li, H.; DeRosier, D.J.; Nicholson, W.V.; Nogales, E.; Downing, K.H. Microtubule Structure at 8 Å Resolution. Structure 2002, 10, 1317–1328. [Google Scholar] [CrossRef]
- He, Y.-X.; Zhang, N.-N.; Li, W.-F.; Jia, N.; Chen, B.-Y.; Zhou, K.; Zhang, J.; Chen, Y.; Zhou, C.-Z. N-Terminal Domain of Bombyx mori Fibroin Mediates the Assembly of Silk in Response to pH Decrease. J. Mol. Biol. 2012, 418, 197–207. [Google Scholar] [CrossRef]
- Rubenstein, M.; Cornejo, A.; Nagpal, R. Programmable self-assembly in a thousand-robot swarm. Science 2014, 345, 795–799. [Google Scholar] [CrossRef]
- Goldstein, S.C.; Campbell, J.D.; Mowry, T.C. Programmable matter. Computer 2005, 38, 99–101. [Google Scholar] [CrossRef]
- Tolley, M.T.; Kalontarov, M.; Neubert, J.; Erickson, D.; Lipson, H. Stochastic Modular Robotic Systems: A Study of Fluidic Assembly Strategies. IEEE Trans. Robot. 2010, 26, 518–530. [Google Scholar] [CrossRef]
- Salleh, F.; Amid, A.; Nordin, N.F.H. In Vitro Study on Collagen Application in Wound Healing: A Systematic Review. IIUM Med. J. Malaysia 2022, 21, 13–22. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, Z.; Dong, Y. Collagen-Based Biomaterials for Tissue Engineering. ACS Biomater. Sci. Eng. 2023, 9, 1132–1150. [Google Scholar] [CrossRef]
- Speakman, J.B. Fibrous Proteins. Design, Synthesis, and Assembly; Ling, S., Ed.; Humana Press: Totowa, NJ, USA, 2021; Volume 158, ISBN 9781071615737. [Google Scholar]
- Chattopadhyay, S.; Raines, R.T. Review collagen-based biomaterials for wound healing. Biopolymers 2014, 101, 821–833. [Google Scholar] [CrossRef]
- Ghodbane, S.A.; Dunn, M.G. Physical and mechanical properties of cross-linked type I collagen scaffolds derived from bovine, porcine, and ovine tendons. J. Biomed. Mater. Res. Part A 2016, 104, 2685–2692. [Google Scholar] [CrossRef] [PubMed]
- Nayak, V.V.; Tovar, N.; Khan, D.; Pereira, A.C.; Mijares, D.Q.; Weck, M.; Durand, A.; Smay, J.E.; Torroni, A.; Coelho, P.G.; et al. 3D Printing Type 1 Bovine Collagen Scaffolds for Tissue and In Vitro Evaluation. Gels 2023, 9, 637. [Google Scholar] [CrossRef]
- Davison-Kotler, E.; Marshall, W.S.; García-Gareta, E. Sources of collagen for biomaterials in skin wound healing. Bioengineering 2019, 6, 56. [Google Scholar] [CrossRef] [PubMed]
- Silva, T.H.; Moreira-Silva, J.; Marques, A.L.P.; Domingues, A.; Bayon, Y.; Reis, R.L. Marine origin collagens and its potential applications. Mar. Drugs 2014, 12, 5881–5901. [Google Scholar] [CrossRef]
- Rigogliuso, S.; Campora, S.; Notarbartolo, M.; Ghersi, G. Recovery of Bioactive Compounds from Marine Organisms: Focus on the Future Perspectives for Pharmacological, Biomedical and Regenerative Medicine Applications of Marine Collagen. Molecules 2023, 28, 1152. [Google Scholar] [CrossRef]
- Diamantides, N.; Wang, L.; Pruiksma, T.; Siemiatkoski, J.; Dugopolski, C.; Shortkroff, S.; Kennedy, S.; Bonassar, L.J. Correlating rheological properties and printability of collagen bioinks: The effects of riboflavin photocrosslinking and pH. Biofabrication 2017, 9, 034102. [Google Scholar] [CrossRef]
- Gaudet, I.D.; Shreiber, D.I. Characterization of methacrylated Type-I collagen as a dynamic, photoactive hydrogel. Biointerphases 2012, 7, 25. [Google Scholar] [CrossRef] [PubMed]
- Zeugolis, D.I.; Paul, R.G.; Attenburrow, G. Factors influencing the properties of reconstituted collagen fibers prior to self-assembly: Animal species and collagen extraction method. J. Biomed. Mater. Res. Part A 2008, 86, 892–904. [Google Scholar] [CrossRef]
- Ferrario, C.; Rusconi, F.; Pulaj, A.; Macchi, R.; Landini, P.; Paroni, M.; Colombo, G.; Martinello, T.; Melotti, L.; Gomiero, C.; et al. From food waste to innovative biomaterial: Sea urchin-derived collagen for applications in skin regenerative medicine. Mar. Drugs 2020, 18, 414. [Google Scholar] [CrossRef]
- Carolo, A.; Melotti, L.; Zivelonghi, G.; Sacchetto, R.; Akyürek, E.E.; Martinello, T.; Venerando, A.; Iacopetti, I.; Sugni, M.; Martinelli, G.; et al. Mutable Collagenous Tissue Isolated from Echinoderms Leads to the Production of a Dermal Template That Is Biocompatible and Effective for Wound Healing in Rats. Mar. Drugs 2023, 21, 506. [Google Scholar] [CrossRef]
- Xu, Q.; Torres, J.E.; Hakim, M.; Babiak, P.M.; Pal, P.; Battistoni, C.M.; Nguyen, M.; Panitch, A.; Solorio, L.; Liu, J.C. Collagen- and hyaluronic acid-based hydrogels and their biomedical applications. Mater. Sci. Eng. R Rep. 2021, 146, 100641. [Google Scholar] [CrossRef] [PubMed]
- Doyle, M.E.; Dalgarno, K.; Masoero, E.; Ferreira, A.M. Advances in biomimetic collagen mineralisation and future approaches to bone tissue engineering. Biopolymers 2023, 114, e23527. [Google Scholar] [CrossRef] [PubMed]
- Campodoni, E.; Montanari, M.; Artusi, C.; Bassi, G.; Furlani, F.; Montesi, M.; Panseri, S.; Sandri, M.; Tampieri, A. Calcium-Based Biomineralization: A Smart Approach for the Design of Novel Multifunctional Hybrid Materials. J. Compos. Sci. 2021, 5, 278. [Google Scholar] [CrossRef]
- Focarete, M.L.; Tampieri, A. Core-Shell Nanostructures for Drug Delivery and Theranostics Challenges, Strategies and Prospects for Novel Carrier Systems; Elsevier: Amsterdam, The Netherlands, 2018; ISBN 9780081021989. [Google Scholar]
- Rastian, Z.; Pütz, S.; Wang, Y.J.; Kumar, S.; Fleissner, F.; Weidner, T.; Parekh, S.H. Type I Collagen from Jellyfish Catostylus mosaicus for Biomaterial Applications. ACS Biomater. Sci. Eng. 2018, 4, 2115–2125. [Google Scholar] [CrossRef]
- Wichuda, J.; Sunthorn, C.; Busarakum, P. Comparison of the properties of collagen extracted from dried jellyfish and dried squid. Afr. J. Biotechnol. 2016, 15, 642–648. [Google Scholar] [CrossRef]
- Cheng, X.; Shao, Z.; Li, C.; Yu, L.; Raja, M.A.; Liu, C. Isolation, Characterization and Evaluation of Collagen from Jellyfish Rhopilema esculentum Kishinouye for Use in Hemostatic Applications. PLoS ONE 2017, 12, e0169731. [Google Scholar] [CrossRef]
- Veeruraj, A.; Arumugam, M.; Ajithkumar, T.; Balasubramanian, T. Isolation and characterization of collagen from the outer skin of squid (Doryteuthis singhalensis). Food Hydrocoll. 2015, 43, 708–716. [Google Scholar] [CrossRef]
- Dellaquila, A.; Campodoni, E.; Tampieri, A.; Sandri, M. Overcoming the Design Challenge in 3D Biomimetic Hybrid Scaffolds for Bone and Osteochondral Regeneration by Factorial Design. Front. Bioeng. Biotechnol. 2020, 8, 550524. [Google Scholar] [CrossRef] [PubMed]
- Fernandes Patrício, T.M.; Panseri, S.; Sandri, M.; Tampieri, A.; Sprio, S. New bioactive bone-like microspheres with intrinsic magnetic properties obtained by bio-inspired mineralisation process. Mater. Sci. Eng. C 2017, 77, 613–623. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Rowe, D.W.; Perera, I.P.; Zhang, J.; Suib, S.L.; Xin, X.; Wei, M. Intrafibrillar Mineralized Collagen-Hydroxyapatite-Based Scaffolds for Bone Regeneration. ACS Appl. Mater. Interfaces 2020, 12, 18235–18249. [Google Scholar] [CrossRef]
- Xing, F.; Chi, Z.; Yang, R.; Xu, D.; Cui, J.; Huang, Y.; Zhou, C.; Liu, C. Chitin-hydroxyapatite-collagen composite scaffolds for bone regeneration. Int. J. Biol. Macromol. 2021, 184, 170–180. [Google Scholar] [CrossRef]
- Song, Y.; Wu, H.; Gao, Y.; Li, J.; Lin, K.; Liu, B.; Lei, X.; Cheng, P.; Zhang, S.; Wang, Y.; et al. Zinc Silicate/Nano-Hydroxyapatite/Collagen Scaffolds Promote Angiogenesis and Bone Regeneration via the p38 MAPK Pathway in Activated Monocytes. ACS Appl. Mater. Interfaces 2020, 12, 16058–16075. [Google Scholar] [CrossRef]
- Richardson, T.P.; Murphy, W.L.; Mooney, D.J. Polymeric delivery of proteins and plasmid DNA for tissue engineering and gene therapy. Crit. Rev. Eukaryot. Gene Expr. 2001, 11, 47–58. [Google Scholar] [CrossRef]
- A Biomimetic and Bioactive Scaffold with Intelligently Pulsatile Teriparatide Delivery for Local and Systemic Osteoporosis Regeneration—ScienceDirect. Available online: https://www.sciencedirect.com/science/article/pii/S2452199X22001402 (accessed on 25 August 2023).
- Zielińska, A.; Karczewski, J.; Eder, P.; Kolanowski, T.; Szalata, M.; Wielgus, K.; Szalata, M.; Kim, D.; Shin, S.R.; Słomski, R.; et al. Scaffolds for drug delivery and tissue engineering: The role of genetics. J. Control. Release 2023, 359, 207–223. [Google Scholar] [CrossRef]
- Flemming, R.G.; Murphy, C.J.; Abrams, G.A.; Goodman, S.L.; Nealey, P.F. Effects of synthetic micro- and nano-structured surfaces on cell behavior. Biomaterials 1999, 20, 573–588. [Google Scholar] [CrossRef]
- Matsuzaka, K.; Walboomers, X.F.; De Ruijter, J.E.; Jansen, J.A. The effect of poly-L-lactic acid with parallel surface micro on groove on osteoblast-like cells in vitro. Biomaterials 1999, 20, 1293–1301. [Google Scholar] [CrossRef]
- Di Pompo, G.; Liguori, A.; Carlini, M.; Avnet, S.; Boi, M.; Baldini, N.; Focarete, M.L.; Bianchi, M.; Gualandi, C.; Graziani, G. Electrospun fibers coated with nanostructured biomimetic hydroxyapatite: A new platform for regeneration at the bone interfaces. Biomater. Adv. 2023, 144, 213231. [Google Scholar] [CrossRef]
- Mohammadalipour, M.; Asadolahi, M.; Mohammadalipour, Z.; Behzad, T.; Karbasi, S. Plasma surface modification of electrospun polyhydroxybutyrate (PHB) nanofibers to investigate their performance in bone tissue engineering. Int. J. Biol. Macromol. 2023, 230, 123167. [Google Scholar] [CrossRef] [PubMed]
- Akbari, N.; Khorshidi, S.; Karkhaneh, A. Effect of piezoelectricity of nanocomposite electrospun scaffold on cell behavior in bone tissue engineering. Iran. Polym. J. 2022, 31, 919–930. [Google Scholar] [CrossRef]
- Chakraborty, R.; Anoop, A.G.; Thakur, A.; Mohanta, G.C.; Kumar, P. Strategies To Modify the Surface and Bulk Properties of 3D-Printed Solid Scaffolds for Tissue Engineering Applications. ACS Omega 2023, 8, 5139–5156. [Google Scholar] [CrossRef] [PubMed]
- Shopova, D.; Yaneva, A.; Bakova, D.; Mihaylova, A.; Kasnakova, P.; Hristozova, M.; Sbirkov, Y.; Sarafian, V.; Semerdzhieva, M. (Bio)printing in Personalized Medicine—Opportunities and Potential Benefits. Bioengineering 2023, 10, 287. [Google Scholar] [CrossRef]
- Shi, Y.; Deng, T.; Peng, Y.; Qin, Z.; Ramalingam, M.; Pan, Y.; Chen, C.; Zhao, F.; Cheng, L.; Liu, J. Effect of Surface Modification of PEEK Artificial Phalanx by 3D Printing on its Biological Activity. Coatings 2023, 13, 400. [Google Scholar] [CrossRef]
- Chandra, S. Natural and Synthetic Polymers. In Polymers in Concrete; CRC Press: Boca Raton, FL, USA, 2020; pp. 5–25. [Google Scholar] [CrossRef]
- Grigora, M.-E.; Terzopoulou, Z.; Baciu, D.; Steriotis, T.; Charalambopoulou, G.; Gounari, E.; Bikiaris, D.N.; Tzetzis, D. 3D printed poly(lactic acid)-based nanocomposite scaffolds with bioactive coatings for tissue engineering applications. J. Mater. Sci. 2023, 58, 2740–2763. [Google Scholar] [CrossRef]
- Mou, X.; Shah, J.; Bhattacharya, R.; Kalejaiye, T.D.; Sun, B.; Hsu, P.-C.; Musah, S. A Biomimetic Electrospun Membrane Supports the Differentiation and Maturation of Kidney Epithelium from Human Stem Cells. Bioengineering 2022, 9, 188. [Google Scholar] [CrossRef]
- Yao, T.; Chen, H.; Wang, R.; Rivero, R.; Wang, F.; Kessels, L.; Agten, S.M.; Hackeng, T.M.; Wolfs, T.G.A.M.; Fan, D.; et al. Thiol-ene conjugation of a VEGF peptide to electrospun scaffolds for potential applications in angiogenesis. Bioact. Mater. 2023, 20, 306–317. [Google Scholar] [CrossRef]
- Teimouri, R.; Abnous, K.; Taghdisi, S.M.; Ramezani, M.; Alibolandi, M. Surface modifications of scaffolds for bone regeneration. J. Mater. Res. Technol. 2023, 24, 7938–7973. [Google Scholar] [CrossRef]
- Laput, O.A.; Vasenina, I.V.; Korzhova, A.G.; Bryuzgina, A.A.; Khomutova, U.V.; Tuyakova, S.G.; Akhmadeev, Y.H.; Shugurov, V.V.; Bolbasov, E.N.; Tverdokhlebov, S.I.; et al. Effect of Nitrogen Arc Discharge Plasma Treatment on Physicochemical Properties and Biocompatibility of PLA-Based Scaffolds. Polymers 2023, 15, 3381. [Google Scholar] [CrossRef] [PubMed]
- Namhongsa, M.; Daranarong, D.; Molloy, R.; Ross, S.; Ross, G.M.; Tuantranont, A.; Boonyawan, D.; Tocharus, J.; Sivasinprasasn, S.; Topham, P.D.; et al. Plasma surface modification of two-component composite scaffolds consisting of 3D-printed and electrospun fiber components from biodegradable PLGA and PLCL. Eur. Polym. J. 2023, 194, 112135. [Google Scholar] [CrossRef]
- Nakanishi, K.; Sakiyama, T.; Imamura, K. On the adsorption of proteins on solid surfaces, a common but very complicated phenomenon. J. Biosci. Bioeng. 2001, 91, 233–244. [Google Scholar] [CrossRef] [PubMed]
- Stivaktakis, N.; Nikou, K.; Panagi, Z.; Beletsi, A.; Leondiadis, L.; Avgoustakis, K. Immune responses in mice of b-galactosidase adsorbed or encapsulated in poly(lactic acid) and poly(lactic-co-glycolic acid) microspheres. J. Biomed. Mater. Res. Part A 2005, 73A, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Thijssen, Q.; Parmentier, L.; Van Holsbeeck, K.; Ballet, S.; Van Vlierberghe, S. Nature-Inspired Dual Purpose Strategy toward Cell-Adhesive PCL Networks: C(-linker-)RGD Incorporation via Thiol-ene Crosslinking. Biomacromolecules 2023, 24, 1638–1647. [Google Scholar] [CrossRef]
- Chroni, A.; Kafetzi, M.; Pispas, S. Block copolymer-protein/peptide nanostructures for biomedical applications. In Functional Materials in Biomedical Applications; Taylor and Francis: Boca Raton, FL, USA, 2023; pp. 91–133. ISBN 9781003411468. [Google Scholar]
- Liu, Q.; Chiu, A.; Wang, L.; An, D.; Li, W.; Chen, E.Y.; Zhang, Y.; Pardo, Y.; McDonough, S.P.; Liu, L.; et al. Developing mechanically robust, triazole-zwitterionic hydrogels to mitigate foreign body response (FBR) for islet encapsulation. Biomaterials 2020, 230, 119640. [Google Scholar] [CrossRef]
- Kang, M.-S.; Lee, G.-H.; Kwon, I.H.; Yang, M.-J.; Heo, M.B.; Choi, J.-W.; Lee, T.G.; Yoon, C.-H.; Baek, B.; Sung, M.-C.; et al. Uptake and toxicity of cerium dioxide nanoparticles with different aspect ratio. Toxicol. Lett. 2023, 373, 196–209. [Google Scholar] [CrossRef]
- Fukuda, S.; Xu, Y. A biomimetic anti-biofouling coating in nanofluidic channels. J. Mater. Chem. B 2022, 10, 2481–2489. [Google Scholar] [CrossRef]
- Cao, Z.; Gan, T.; Xu, G.; Ma, C. Biomimetic Self-Renewal Polymer Brushes with Protein Resistance Inspired by Fish Skin. Langmuir 2019, 35, 14596–14602. [Google Scholar] [CrossRef]
- Jeong, J.-O.; Kim, S.; Park, J.; Lee, S.; Park, J.-S.; Lim, Y.-M.; Lee, J.Y. Biomimetic nonbiofouling polypyrrole electrodes grafted with zwitterionic polymer using gamma rays. J. Mater. Chem. B 2020, 8, 7225–7232. [Google Scholar] [CrossRef]
- Liu, S.; Zhi, J.; Chen, Y.; Song, Z.; Wang, L.; Tang, C.; Li, S.; Lai, X.; Xu, N.; Liu, T. Biomimetic modification on the microporous surface of cardiovascular materials to accelerate endothelialization and regulate intimal regeneration. Biomater. Adv. 2022, 135, 112666. [Google Scholar] [CrossRef]
- Yun, X.; Xiong, Z.; He, Y.; Wang, X. Superhydrophobic lotus-leaf-like surface made from reduced graphene oxide through soft-lithographic duplication. RSC Adv. 2020, 10, 5478–5486. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yuan, J.; Chen, J.; Zeng, Y.; Yu, T.; Guo, X.; Wang, S.; Yang, G.; Li, Y. A Single-Component Molecular Glass Resist Based on Tetraphenylsilane Derivatives for Electron Beam Lithography. ACS Omega 2023, 8, 12173–12182. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.D.T.; Aryal, S.; Pitchaimani, A.; Park, S.; Key, J.; Aryal, S. Biomimetic surface modification of discoidal polymeric particles. Nanomed. Nanotechnol. Biol. Med. 2019, 16, 79–87. [Google Scholar] [CrossRef]
- Gao, S.; Chen, S.; Lu, Q. Cell-imprinted biomimetic interface for intelligent recognition and efficient capture of CTCs. Biomater. Sci. 2019, 7, 4027–4035. [Google Scholar] [CrossRef] [PubMed]
- Christopherson, G.T.; Song, H.; Mao, H.-Q. The influence of fiber diameter of electrospun substrates on neural stem cell differentiation and proliferation. Biomaterials 2009, 30, 556–564. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Patra, P.K.; Lovett, M.L.; Kaplan, D.L.; Bhowmick, S. Role of electrospun fibre diameter and corresponding specific surface area (SSA) on cell attachment. J. Tissue Eng. Regen. Med. 2009, 3, 269–279. [Google Scholar] [CrossRef]
- Ozbolat, V.; Dey, M.; Ayan, B.; Povilianskas, A.; Demirel, M.C.; Ozbolat, I.T. 3D Printing of PDMS Improves Its Mechanical and Cell Adhesion Properties. ACS Biomater. Sci. Eng. 2018, 4, 682–693. [Google Scholar] [CrossRef]
- Wu, Z.; Li, Q.; Xie, S.; Shan, X.; Cai, Z. In vitro and in vivo biocompatibility evaluation of a 3D bioprinted gelatin-sodium alginate/rat Schwann-cell scaffold. Mater. Sci. Eng. C 2020, 109, 110530. [Google Scholar] [CrossRef]
- Wu, C.A.; Zhu, Y.; Woo, Y.J. Advances in 3D Bioprinting: Techniques, Applications, and Future Directions for Cardiac Tissue Engineering. Bioengineering 2023, 10, 842. [Google Scholar] [CrossRef]
- Gu, Z.; Fu, J.; Lin, H.; He, Y. Development of 3D bioprinting: From printing methods to biomedical applications. Asian J. Pharm. Sci. 2020, 15, 529–557. [Google Scholar] [CrossRef] [PubMed]
- Santoni, S.; Gugliandolo, S.G.; Sponchioni, M.; Moscatelli, D.; Colosimo, B.M. 3D bioprinting: Current status and trends—A guide to the literature and industrial practice. Bio-Design Manuf. 2022, 5, 14–42. [Google Scholar] [CrossRef]
- Nadernezhad, A.; Caliskan, O.S.; Topuz, F.; Afghah, F.; Erman, B.; Koc, B. Nanocomposite Bioinks Based on Agarose and 2D Nanosilicates with Tunable Flow Properties and Bioactivity for 3D Bioprinting. ACS Appl. Bio Mater. 2019, 2, 796–806. [Google Scholar] [CrossRef] [PubMed]
- Alarçin, E.; İzbudak, B.; Yüce Erarslan, E.; Domingo, S.; Tutar, R.; Titi, K.; Kocaaga, B.; Guner, F.S.; Bal-Öztürk, A. Optimization of methacrylated gelatin /layered double hydroxides nanocomposite cell-laden hydrogel bioinks with high printability for 3D extrusion bioprinting. J. Biomed. Mater. Res. Part A 2023, 111, 209–223. [Google Scholar] [CrossRef] [PubMed]
- Amukarimi, S.; Mozafari, M. 4D bioprinting of tissues and organs. Bioprinting 2021, 23, e00161. [Google Scholar] [CrossRef]
- Díaz-Payno, P.J.; Kalogeropoulou, M.; Muntz, I.; Kingma, E.; Kops, N.; D’Este, M.; Koenderink, G.H.; Fratila-Apachitei, L.E.; van Osch, G.J.V.M.; Zadpoor, A.A. Swelling-Dependent Shape-Based Transformation of a Human Mesenchymal Stromal Cells-Laden 4D Bioprinted Construct for Cartilage Tissue Engineering. Adv. Healthc. Mater. 2023, 12, 2201891. [Google Scholar] [CrossRef]
- Kitana, W.; Apsite, I.; Hazur, J.; Boccaccini, A.R.; Ionov, L. 4D Biofabrication of T-Shaped Vascular Bifurcation. Adv. Mater. Technol. 2023, 8, 2200429. [Google Scholar] [CrossRef]
- Mea, H.; Wan, J. Microfluidics-enabled functional 3D printing. Biomicrofluidics 2022, 16, 021501. [Google Scholar] [CrossRef]
- Li, Y.B.; Sodja, C.; Rukhlova, M.; Nhan, J.; Poole, J.J.A.; Allen, H.; Yimer, S.; Baumann, E.; Bedford, E.; Prazak, H.; et al. Microfluidic-Based 3D Bioprinting of Vascular Endothelial Networks Using Alginate-Collagen Based Biomaterials. SSRN Electron. J. 2022. [Google Scholar] [CrossRef]
- Wang, D.; Maharjan, S.; Kuang, X.; Wang, Z.; Mille, L.S.; Tao, M.; Yu, P.; Cao, X.; Lian, L.; Lv, L.; et al. Microfluidic bioprinting of tough hydrogel-based vascular conduits for functional blood vessels. Sci. Adv. 2022, 8, eabq6900. [Google Scholar] [CrossRef]
- Yin, Y.; Vázquez-Rosado, E.J.; Wu, D.; Viswananthan, V.; Farach, A.; Farach-Carson, M.C.; Harrington, D.A. Microfluidic coaxial 3D bioprinting of cell-laden microfibers and microtubes for salivary gland tissue engineering. Biomater. Adv. 2023, 154, 213588. [Google Scholar] [CrossRef] [PubMed]
- You, S.; Xiang, Y.; Hwang, H.H.; Berry, D.B.; Kiratitanaporn, W.; Guan, J.; Yao, E.; Tang, M.; Zhong, Z.; Ma, X.; et al. High cell density and high-resolution 3D bioprinting for fabricating vascularized tissues. Sci. Adv. 2023, 9, eade7923. [Google Scholar] [CrossRef]
- Rajput, M.; Mondal, P.; Yadav, P.; Chatterjee, K. Light-based 3D bioprinting of bone tissue scaffolds with tunable mechanical properties and architecture from photocurable silk fibroin. Int. J. Biol. Macromol. 2022, 202, 644–656. [Google Scholar] [CrossRef] [PubMed]
- Kumari, S.; Mondal, P.; Chatterjee, K. Digital light processing-based 3D bioprinting of κ-carrageenan hydrogels for engineering cell-loaded tissue scaffolds. Carbohydr. Polym. 2022, 290, 119508. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Chen, W.; Xiao, X.; Xu, Y.; Li, C.; Jia, X.; Meng, M.Q.-H. A survey of the development of biomimetic intelligence and robotics. Biomim. Intell. Robot. 2021, 1, 100001. [Google Scholar] [CrossRef]
- Whitley, D. A genetic algorithm tutorial. Stat. Comput. 1994, 4, 65–85. [Google Scholar] [CrossRef]
- Dorigo, M.; Di Caro, G. Ant colony optimization: A new meta-heuristic. In Proceedings of the 1999 Congress on Evolutionary Computation-CEC99 (Cat. No. 99TH8406), Washington, DC, USA, 6–9 July 1999; IEEE: Piscataway, NJ, USA, 1999; pp. 1470–1477. [Google Scholar]
- Freitas, A.A. Data Mining and Knowledge Discovery with Evolutionary Algorithms; Natural Computing Series; Springer: Berlin/Heidelberg, Germany, 2002; ISBN 978-3-642-07763-0. [Google Scholar]
- Lam, B.; Ciesielski, V. Discovery of Human-Competitive Image Texture Feature Extraction Programs Using Genetic Programming. In Genetic and Evolutionary Computation Conference; Springer: Berlin/Heidelberg, Germany, 2004; pp. 1114–1125. [Google Scholar]
- Ahnert, S.E.; Marsh, J.A.; Hernández, H.; Robinson, C.V.; Teichmann, S.A. Principles of assembly reveal a periodic table of protein complexes. Science 2015, 350, aaa2245. [Google Scholar] [CrossRef]
- Dasgupta, D.; Michalewicz, Z. (Eds.) Evolutionary Algorithms in Engineering Applications; Springer Science & Business Media: Berlin, Germany, 2013. [Google Scholar]
- Badini, S.; Regondi, S.; Pugliese, R. Unleashing the Power of Artificial Intelligence in Materials Design. Materials 2023, 16, 5927. [Google Scholar] [CrossRef]
- Ball, P. Using artificial intelligence to accelerate materials development. MRS Bull. 2019, 44, 335–344. [Google Scholar] [CrossRef]
- Raabe, D.; Mianroodi, J.R.; Neugebauer, J. Accelerating the design of compositionally complex materials via physics-informed artificial intelligence. Nat. Comput. Sci. 2023, 3, 198–209. [Google Scholar] [CrossRef]
- Rao, Z.; Tung, P.-Y.; Xie, R.; Wei, Y.; Zhang, H.; Ferrari, A.; Klaver, T.P.C.; Körmann, F.; Sukumar, P.T.; Kwiatkowski da Silva, A.; et al. Machine learning–enabled high-entropy alloy discovery. Science 2022, 378, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, K.; Maryanovsky, D.; Mellor, W.M.; Zhu, C.; Rosengarten, A.S.; Harrington, T.J.; Oses, C.; Toher, C.; Curtarolo, S.; Vecchio, K.S. Discovery of high-entropy ceramics via machine learning. npj Comput. Mater. 2020, 6, 42. [Google Scholar] [CrossRef]
- Badini, S.; Regondi, S.; Frontoni, E.; Pugliese, R. Assessing the capabilities of ChatGPT to improve additive manufacturing troubleshooting. Adv. Ind. Eng. Polym. Res. 2023, 6, 278–287. [Google Scholar] [CrossRef]
- Agathokleous, E.; Saitanis, C.J.; Fang, C.; Yu, Z. Use of ChatGPT: What does it mean for biology and environmental science? Sci. Total Environ. 2023, 888, 164154. [Google Scholar] [CrossRef] [PubMed]
- Cheng, K.; Guo, Q.; He, Y.; Lu, Y.; Gu, S.; Wu, H. Exploring the Potential of GPT-4 in Biomedical Engineering: The Dawn of a New Era. Ann. Biomed. Eng. 2023, 51, 1645–1653. [Google Scholar] [CrossRef] [PubMed]
- Purkait, M.K.; Sinha, M.K.; Mondal, P.; Singh, R. Biologically Responsive Membranes. In Interface Science and Technology; Elsevier: Amsterdam, The Netherlands, 2018; pp. 145–171. [Google Scholar]
- Kim, J.H.; Lee, S.J. A Biomimetic Strategy to Design Biomaterials for In Situ Tissue Regeneration. In In Situ Tissue Regeneration; Elsevier: Amsterdam, The Netherlands, 2016; pp. 185–201. [Google Scholar]
- Lee, J.Y.; Bashur, C.A.; Milroy, C.A.; Forciniti, L.; Goldstein, A.S.; Schmidt, C.E. Nerve Growth Factor-Immobilized Electrically Conducting Fibrous Scaffolds for Potential Use in Neural Engineering Applications. IEEE Trans. Nanobiosci. 2012, 11, 15–21. [Google Scholar] [CrossRef]
- Rashid, M.; Roni, M.A.; Rahman, M. Clinical status of bioinspired and biomimetic materials. In Bioinspired and Biomimetic Materials for Drug Delivery; Elsevier: Amsterdam, The Netherlands, 2021; pp. 277–294. [Google Scholar]
- Liu, S.; Yu, J.-M.; Gan, Y.-C.; Qiu, X.-Z.; Gao, Z.-C.; Wang, H.; Chen, S.-X.; Xiong, Y.; Liu, G.-H.; Lin, S.-E.; et al. Biomimetic natural biomaterials for tissue engineering and regenerative medicine: New biosynthesis methods, recent advances, and emerging applications. Mil. Med. Res. 2023, 10, 16. [Google Scholar] [CrossRef]
- Qiu, Z.-Y.; Cui, Y.; Tao, C.-S.; Zhang, Z.-Q.; Tang, P.-F.; Mao, K.-Y.; Wang, X.-M.; Cui, F.-Z. Mineralized Collagen: Rationale, Current Status, and Clinical Applications. Materials 2015, 8, 4733–4750. [Google Scholar] [CrossRef]
- Song, T.-X.; Hu, Y.-L.; He, Z.-M.; Cui, Y.; Ding, Q.; Qiu, Z.-Y. Clinical Applications of the Mineralized Collagen. In Mineralized Collagen Bone Graft Substitutes; Elsevier: Amsterdam, The Netherlands, 2019; pp. 167–232. [Google Scholar]
- Kantak, M.N.; Bharate, S.S. Analysis of clinical trials on biomaterial and therapeutic applications of chitosan: A review. Carbohydr. Polym. 2022, 278, 118999. [Google Scholar] [CrossRef]







| Tissue | Young’s Elastic Modulus | Reference |
|---|---|---|
| Human epithelial cells (normal) | 1.60 kPa | [14] |
| Human epithelial cells (cancer) | 1.40 kPa | [14] |
| Human platelets | 1–50 kPa | [15] |
| Kidney | 180 kPa | [16] |
| Skin (different species) | 20–40 Mpa | [17] |
| Muscle | 480 Mpa | [18] |
| Tendon | 43–1660 Mpa | [19] |
| Elastin-free tendon | 1.2 Gpa | [20] |
| Cartilage | 100–500 kPa | [21] |
| Human proximal tibia | 11–14 Gpa | [22] |
| Biomaterial | Young’s Elastic Modulus | Ref. |
| Gelatin (Ge) 1 | 0 Pa < E < 75 kPa | [23] |
| Collagen mimetic peptide | ~8 kPa | [24] |
| SAPs | 0.1 kPa < E < 10 kPa | [25] |
| Hyaluronic acid (HA) hydrogel 2 | 1 kPa | [26] |
| HA-Ge | 22 kPa | [27] |
| Fmoc-Phe-Phe-OH | 200 kPa | [28] |
| Alginate hydrogel 3 | 117 kPa | [29] |
| Cross-SAPs | 200 kPa < E < 850 kPa | [25,30] |
| Chitosan | ~ 7 Mpa | [31] |
| Amphiphile polymer conetworks | 5 Mpa < E < 200 Mpa | [32] |
| H-Phe-Phe-OH nanotubes | 20 Gpa | [28] |
| Gelatin methacryloyl (GelMA) | 3 kPa < E < 184 kPa | [33] |
| Collagen type I (in rat) | 5–11.5 Gpa | [34] |
| Collagen (mammalian tendon) | 1.2 Gpa | [12] |
| Class | Subclass | Examples | Reference |
|---|---|---|---|
| Source | Natural | hyaluronic acid chitosan alginate | [76] [77] [78] |
| Synthetic | poly (vinyl alcohol) (PVA) poly (ethylene glycol) (PEG) poly (acrylic acid) (PAA) | [78] [78] [79] | |
| Charge | |||
| Ionic | |||
| Cationic | ε-poly-l-lysine (EPL) with poly(ethylene glycol) diglycidyl ether) (PEGDGE) | [80] | |
| Anionic | poly(oligo ethylene glycol monoacrylate-co-acrylic acid) | [81] | |
| Non-ionic | hydroxyethyl cellulose | [82] | |
| Zwitterionic | poly(sulfobetaine methacrylate) | [83] | |
| Composition | |||
| Homopolymeric | poly(N-isopropylacrylamide) | [84] | |
| Heteropolymeric (co-polymeric/multi-polymeric) | oligo(ethylene glycol) with di(meth)acrylate | [85,86] | |
| Physical properties | |||
| Solid | β-hairpin peptide-based | [87] | |
| Liquid | gelators with ion liquids | [88] | |
| Mucoadhesive | polymer with intestinal mucus | [89] | |
| Crosslinking mechanism | |||
| Physical | polyelectrolyte hydrogels ionizing radiation MW irradiation | [90] [52,91] [57] | |
| Chemical | with small molecules | [54,92,93] |
| Collagen Source | Blending Procedure | Scaffold Production Technique | Stabilization Treatment | Application | Authors | References |
|---|---|---|---|---|---|---|
| Bovine, porcine, and ovine tendons | Pure collagen | Lyophilization | Crosslinking in a 10 mM EDC and 5 mM NHS | Tissue engineering application | Ghodbane et al. | [144] |
| Type I bovine collagen | Pure collagen | 3D printing | Fiber formation buffer solution + crosslinking in EDC in 90% acetone | Tissue engineering application | Nayak et al. | [145] |
| Femoral condyles old bovids | Pure collagen | 3D printing | Riboflavin crosslinking | Natural-mimicking hydrogels | Diamantides et al. | [149] |
| Type I bovine collagen | Pure collagen | Lyophilization | Collagen methacrylamide + crosslinking in EDC/NHS | Tissue engineering application as dynamic, photoactive hydrogel | Gaudet et al. | [150] |
| JellaGel™ solution, jellyfish collagen | Pure collagen | Gel formation | Genipin crosslinking | Cartilage regeneration | Riacci et al. | [93] |
| Sea urchin waste | Pure collagen | Lyophilization | UV crosslinking | Wound healing | Ferrario et al. | [151,152] |
| Catostylus mosaicus jellyfish | Collagen/agarose | Gel formation | None | Tissue regeneration | Rastian et al. | [158] |
| Dried squid and dried jellyfish | Pure collagen | Lyophilization | None | Tissue regeneration | Jankangram et al. | [159] |
| R. esculentum jellyfish | Pure collagen | Lyophilization | Crosslinking in EDC/NHS | Hemostatic applications | Xiaochen et al. | [160] |
| Doryteuthis singhalensis squid waste | Pure collagen | Gel formation | None | Tissue regeneration | Veeruraj et al. | [161] |
| Type I collagen from equine tendon | Hydroxyapatite/collagen | Gel formation, biomineralization | Ribose crosslinking | Bone and osteochondral regeneration | Dellaquila et al. | [162] |
| Commercial Type I collagen-based recombinant peptide | Fe-doped Hydroxyapatite/collagen | Water-in-oil emulsification process | None | Bone-like microspheres with intrinsic magnetic properties | Fernandes Patrício et al. | [163] |
| Type I collagen from rat tails | Fe and Mn-doped Hydroxyapatite/Collagen | Lyophilization | None | Bone regeneration | Yu et al. | [164] |
| Bovine tendon collagen | Chitin–hydroxyapatite–collagen | Lyophilization | Epichlorohydrin crosslinking | Bone regeneration | Xing et al. | [165] |
| Bovine tendon collagen | Zinc silicate/nano-Hydroxyapatite/collagen | 3D printing | None | Angiogenesis and bone regeneration | Yue et al. | [166] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciulla, M.G.; Massironi, A.; Sugni, M.; Ensign, M.A.; Marzorati, S.; Forouharshad, M. Recent Advances in the Development of Biomimetic Materials. Gels 2023, 9, 833. https://doi.org/10.3390/gels9100833
Ciulla MG, Massironi A, Sugni M, Ensign MA, Marzorati S, Forouharshad M. Recent Advances in the Development of Biomimetic Materials. Gels. 2023; 9(10):833. https://doi.org/10.3390/gels9100833
Chicago/Turabian StyleCiulla, Maria G., Alessio Massironi, Michela Sugni, Matthew A. Ensign, Stefania Marzorati, and Mahdi Forouharshad. 2023. "Recent Advances in the Development of Biomimetic Materials" Gels 9, no. 10: 833. https://doi.org/10.3390/gels9100833