Long-Term Benefits of Adapted Physical Activity on Upper Limb Performance and Quality of Life in Breast Cancer Survivors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Study Procedures
2.3. Statistical Analysis
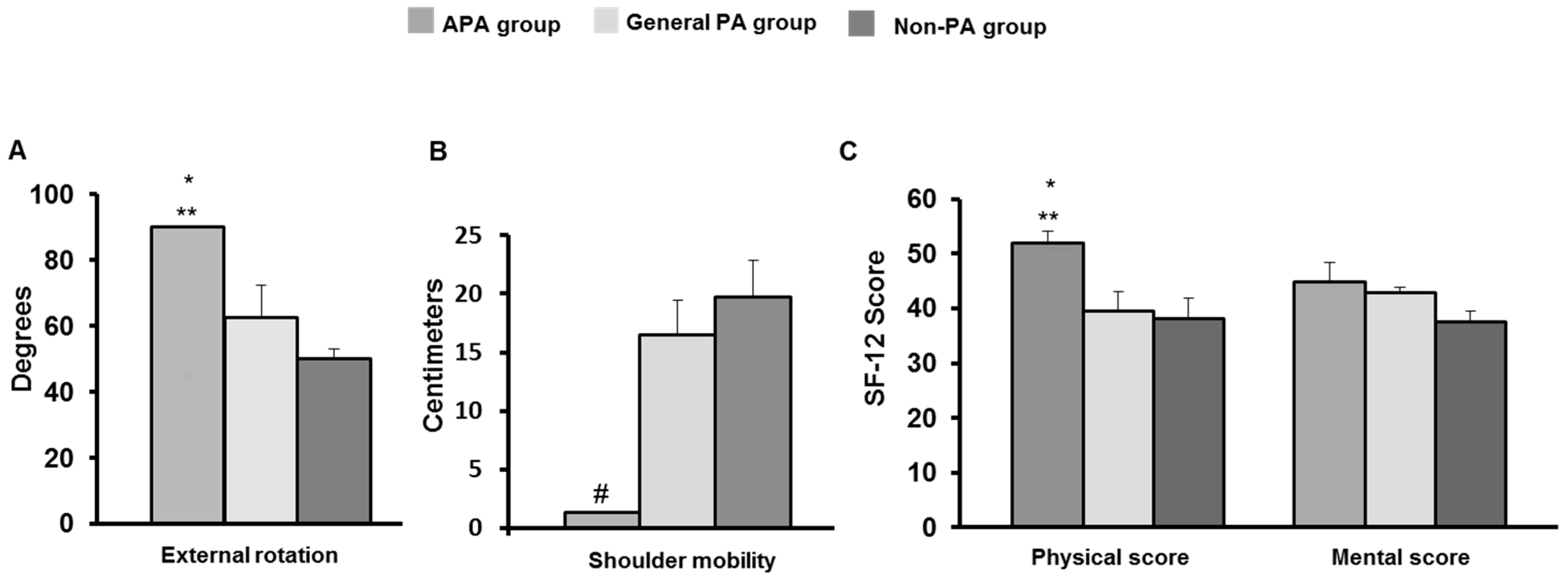
3. Results
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ghoncheh, M.; Mirzaei, M.; Salehiniya, H. Incidence and Mortality of Breast Cancer and their Relationship with the Human Development Index (HDI) in the World in 2012. Asian Pac. J. Cancer Prev. 2015, 16, 8439–8443. [Google Scholar] [CrossRef] [PubMed]
- Recchia, T.L.; Prim, A.C.; Luz, C.M. Upper Limb Functionality and Quality of Life in Women with Five-Year Survival after Breast Cancer Surgery. Rev. Bras. Ginecol. Obstet. 2017, 39, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Mirandola, D.; Miccinesi, G.; Muraca, M.G.; Sgambati, E.; Monaci, M.; Marini, M. Evidence for adapted physical activity as an effective intervention for upper limb mobility and quality of life in breast cancer survivors. J. Phys. Act. Health 2014, 1, 814–822. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.I.; Scherer, R.W.; Geigle, P.M.; Berlanstein, D.R.; Topaloglu, O.; Gotay, C.C.; Snyder, C. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst. Rev. 2012, 15. [Google Scholar] [CrossRef]
- Kampshoff, C.S.; Jansen, F.; van Mechelen, W.; May, A.M.; Brug, J.; Chinapaw, M.J.; Buffart, L.M. Determinants of exercise adherence and maintenance among cancer survivors: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 80. [Google Scholar] [CrossRef] [PubMed]
- Short, C.E.; James, E.L.; Plotnikoff, R.C. Theory-and evidence-based development and process evaluation of the Move More for Life program: A tailored-print intervention designed to promote physical activity among post-treatment breast cancer survivors. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 124. [Google Scholar] [CrossRef] [PubMed]
- Desnoyers, A.; Riesco, E.; Fülöp, T.; Pavic, M. Physical activity and cancer: Update and literature review. Rev. Med. Interne 2016, 37, 399–405. [Google Scholar] [CrossRef]
- Mirandola, D.; Monaci, M.; Muraca, M.G.; Catallo, R.; Gulisano, M.; Sgambati, E.; Marini, M. Role of dance as part of an adapted physical activity program in breast cancer survivors: A pilot study. Med. Sport 2015, 68, 591–599. [Google Scholar]
- Apolone, G.; Mosconi, P.; Quattrociocchi, L.; Gianicolo, E.A.L.; Groth, N.; Ware, J.E., Jr. Questionario Sullo Stato di Salute SF-12; Associati, G.E., Ed.; Versione Italiana; Istituto di Ricerche Farmacologiche Mario Negri.: Milano, Italy, 2001. [Google Scholar]
- Kendrick, D.B.; Strout, T.D. The minimum clinically significant difference in patient-assigned numeric scores for pain. Am. J. Emerg. Med. 2005, 23, 828–832. [Google Scholar] [CrossRef] [PubMed]
- Khadilkar, L.; MacDermid, J.C.; Sinden, K.E.; Jenkyn, T.R.; Birmingham, T.B.; Athwal, G.S. An analysis of functional shoulder movements during task performance using Dartfish movement analysis software. Int. J. Shoulder Surg. 2014, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, R.; Krauss, O.; Höckel, M.; Meyer, A.; Zenger, M.; Hinz, A. The course of anxiety and depression in patients with breast cancer and gynaecological cancer. Breast Care 2008, 3, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Phillips, S.M.; Lloyd, G.R.; Awick, E.A.; McAuley, E. Correlates of objectively measured sedentary behavior in breast cancer survivors. Cancer Causes Control. 2016, 27, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Han, C.J.; Korde, L.A.; Reding, S.; Allott, K.; Van Doren, M.; Schwarz, Y.; Vaughan, C.; Reding, K.W. Investigation of a Lifestyle Intervention in Women at High Risk of Breast Cancer. West. J. Nurs. Res. 2017. [Google Scholar] [CrossRef] [PubMed]
| Variables | Participants (n = 15) |
|---|---|
| Age, mean ± SD (range) | 60.3 ± 10.5 (47–80) |
| Body weight, mean kg ± SD | 66.9 ± 13.2 |
| Height, mean m ± SD | 1.6 ± 0.04 |
| BMI, mean kg/m2 ± SD (range) | 25.7 ± 4.3 |
| BMI category, n | |
| <25 (normal weight) | 7 |
| 25–29.9 (overweight) | 6 |
| ≥30 (obese) | 2 |
| Breast surgery, n | |
| Breast conservation surgery | 6 |
| Modified radical mastectomy | 5 |
| Radical mastectomy | 4 |
| Operated side, n | |
| Right | 12 |
| Left | 3 |
| Adjuvant treatments, n | |
| Chemotherapy | 12 |
| Radiotherapy | 8 |
| Endocrine treatment | 12 |
| Degree of lymphedema, n | |
| None | 6 |
| Mild | 9 |
| Variables | Baseline Mean (SEM) | Post-APA Mean (SEM) | Follow up Mean (SEM) | p-Value * |
|---|---|---|---|---|
| ROM surgical shoulder | ||||
| Extension | 44.16 (0.08) | 45 (0) | 45 (0) | 0.206 |
| Flexion | 148.75 (8.23) | 161.25 (5.22) | 165 (6.06) | 0.006 |
| External rotation | 63.75 (5.54) | 69.58 (6.35) | 67.5 (5.88) | 0.555 |
| Abduction | 141.66 (10.35) | 165.25 (6.5) | 171.66 (5.75) | <0.0001 |
| Surgical shoulder mobility | 18.33 (2.39) | 14.33 (1.98) | 12.08 (2.91) | 0.022 |
| Sit and reach | 9.54 (3.76) | 7.27 (2.73) | 5.36 (2.83) | 0.090 |
| Perception of pain (NRS) | ||||
| Surgical shoulder pain | 4.83 (0.56) | 4.41 (0.63) | 2.50 (0.60) | 0.004 |
| Cervical pain | 3.58 (0.55) | 2.66 (0.72) | 3 (0.62) | 0.398 |
| Dorsal pain | 2.41 (0.63) | 3.25 (0.70) | 2.41 (0.43) | 1.000 |
| Lumbar pain | 4 (0.80) | 3.41 (0.71) | 3.08 (0.62) | 0.170 |
| Quality of life (SF-12) | ||||
| Physical | 39.39 (2.03) | 44.27 (1.79) | 42.92 (2.67) | 0.216 |
| Mental | 38.13 (2.61) | 42.48 (2.06) | 41.48 (2.01) | 0.151 |
| APA Group | General PA Group | Non-PA Group | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Baseline Mean (SEM) | Post-APA Mean (SEM) | Follow up Mean (SEM) | Baseline Mean (SEM) | Post-APA Mean (SEM) | Follow up Mean (SEM) | Baseline Mean (SEM) | Post-APA Mean (SEM) | Follow up Mean (SEM) |
| ROM surgical shoulder | |||||||||
| Extension | 42.1 (2.5) | 45 (0) | 45 (0) | 45 (--) | 45 (--) | 45 (--) | 45 (--) | 45 (--) | 45 (--) |
| Flexion | 155 (18.92) | 160 (11.54) | 180 (0) | 148.75 (12.31) | 165 (9.57) | 166.25 (6.25) | 142.5 (14.50) | 158.75 (8.26) | 148.75 (14.19) |
| External rotation | 73.75 (10.68) | 67.5 (12.99) | 90 (0) | 58.75 (10.48) | 78.75 (11.25) | 62.50 (9.68) | 58.75 (8) | 62.5 (10.10) | 50 (2.88) |
| Abduction | 140 (17.79) | 154.5 (15.17) | 180 (0) | 150 (21.21) | 171 (8.75) | 170 (10) | 135 (19.36) | 170 (10) | 165 (15) |
| Surgical shoulder mobility | 18.5 (4.36) | 15.25 (2.13) | 0 (0) | 18.50 (1.32) | 13 (2.54) | 16.50 (2.98) | 18 (6.48) | 14.75 (5.58) | 19.75 (3.11) |
| Sit and reach | 12.5 (8.50) | 8.25 (5.66) | 0 (0) | 6 (6) | 4.5 (4.5) | 6 (6) | 10.33 (5.36) | 9.66 (4.91) | 11.66 (6) |
| APA Group | General PA Group | Non-PA Group | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Baseline Mean (SEM) | Post-APA Mean (SEM) | Follow up Mean (SEM) | Baseline Mean (SEM) | Post-APA Mean (SEM) | Follow up Mean (SEM) | Baseline Mean (SEM) | Post-APA Mean (SEM) | Follow up Mean (SEM) |
| Perception of pain (NRS) | |||||||||
| Surgical shoulder pain | 4.75 (0.47) | 3.5 (0.95) | 1.25 (0.75) | 5 (0.91) | 6 (1.22) | 2.25 (0.85) | 4.75 (1.54) | 3.75 (0.85) | 4 (1.22) |
| Cervical pain | 4.25 (0.47) | 2.25 (0.31) | 1.75 (0.47) | 4.75 (0.85) | 3.75 (1.75) | 4.75 (0.85) | 1.75 (0.85) | 2 (0.57) | 2.5 (1.32) |
| Dorsal pain | 2.5 (1.04) | 3 (1.22) | 1.5 (0.28) | 3.25 (1.43) | 4.75 (1.37) | 3 (1.08) | 1.5 (0.86) | 2 (0.91) | 2.75 (0.62) |
| Lumbar pain | 3.25 (1.88) | 3.25 (1.97) | 2.75 (0.25) | 6 (1.08) | 4 (0.81) | 5.5 (0.50) | 2.75 (0.62) | 3 (0.91) | 1 (0.70) |
| APA Group | General PA Group | Non-PA Group | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Baselin Mean (SEM) | Post-APA Mean (SEM) | Follow up Mean (SEM) | Baseline Mean (SEM) | Post-APA Mean (SEM) | Follow up Mean (SEM) | Baseline Mean (SEM) | Post-APA Mean (SEM) | Follow up Mean (SEM) |
| Quality of life (SF-12) | |||||||||
| Physical | 39.07 (3.74) | 41.85 (2.61) | 51.93 (2.29) | 38.81 (4.03) | 45.06 (4.81) | 39.61 (3.46) | 42.20 (3.11) | 45.28 (0.87) | 38.21 (3.76) |
| Mental | 36.87 (6.39) | 44.22 (6.39) | 44.95 (3.55) | 38.11 (3.39) | 42.37 (1.04) | 42.90 (4.21) | 39.10 (4.86) | 41.27 (4.02) | 37.47 (2.01) |
| Variables | Time | APA vs. Non-PA | General PA vs. Non-PA |
|---|---|---|---|
| ROM surgical shoulder | |||
| Extension | 0.41 (−0.22; 1.06) | −1.14 (−2.17; −0.11) | 0.19 (−0.79; 1.19) |
| Flexion | 8.12 (2.38; 13.87) | 11.81 (−1452; 38.15) | 7.92 (−17.38; 33.22) |
| External rotation | 1.87 (−4.34; 8.09) | 16.60 (1.42; 31.79) | 13.92 (−0.67; 28.52) |
| Abduction | 15.00 (7.28; 22.72) | −2.79 (−31.20; 25.61) | −.55 (−27.35; 27.24) |
| Surgical shoulder mobility | −3.12 (−5.80; 0.44) | −3.82 (−10.61; 2.96) | 0.83 (−5.69; 7.36) |
| Sit and reach | −2.09 (−1.97; 0.38) | −4.45 (−17.63; 8.73) | −4.85 (−17.58; 7.88) |
| Perception of pain (NRS) | |||
| Surgical shoulder pain | −1.17 (−1.97; −0.37) | −1.23 (−2.83; 0.37) | 0.14 (−1.39; 1.68) |
| Cervical pain | −0.29 (−0.97; 0.38) | 0.74 (−1.24; 2.71) | 2.29 (0.39; 4.19) |
| Dorsal pain | NE | .68 (−0.79; 2.15) | 1.66 (0.24; 3.07) |
| Lumbar pain | −0.46 (−1.11; 0.19) | 1.17 (−0.94; 3.29) | 2.59 (0.56; 4.63) |
| Quality of life (SF-12) | |||
| Physical | 1.77 (−1.03; 4.56) | −2.285 (−8.19; 3.63) | −2.40 (−7.25; 2.45) |
| Mental | 1.67 (0.61; 3.96) | 7.42 (−0.15; 15.00) | −0.14 (−6.37; 6.07) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mirandola, D.; Monaci, M.; Miccinesi, G.; Ventura, L.; Muraca, M.G.; Casini, E.; Sgambati, E.; Manetti, M.; Marini, M. Long-Term Benefits of Adapted Physical Activity on Upper Limb Performance and Quality of Life in Breast Cancer Survivors. J. Funct. Morphol. Kinesiol. 2017, 2, 38. https://doi.org/10.3390/jfmk2040038
Mirandola D, Monaci M, Miccinesi G, Ventura L, Muraca MG, Casini E, Sgambati E, Manetti M, Marini M. Long-Term Benefits of Adapted Physical Activity on Upper Limb Performance and Quality of Life in Breast Cancer Survivors. Journal of Functional Morphology and Kinesiology. 2017; 2(4):38. https://doi.org/10.3390/jfmk2040038
Chicago/Turabian StyleMirandola, Daniela, Marco Monaci, Guido Miccinesi, Leonardo Ventura, Maria Grazia Muraca, Elisa Casini, Eleonora Sgambati, Mirko Manetti, and Mirca Marini. 2017. "Long-Term Benefits of Adapted Physical Activity on Upper Limb Performance and Quality of Life in Breast Cancer Survivors" Journal of Functional Morphology and Kinesiology 2, no. 4: 38. https://doi.org/10.3390/jfmk2040038
APA StyleMirandola, D., Monaci, M., Miccinesi, G., Ventura, L., Muraca, M. G., Casini, E., Sgambati, E., Manetti, M., & Marini, M. (2017). Long-Term Benefits of Adapted Physical Activity on Upper Limb Performance and Quality of Life in Breast Cancer Survivors. Journal of Functional Morphology and Kinesiology, 2(4), 38. https://doi.org/10.3390/jfmk2040038







