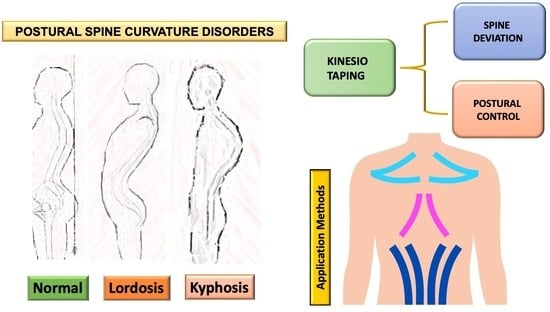
A Short Overview of the Effects of Kinesio Taping for Postural Spine Curvature Disorders
Abstract
:1. Introduction
2. Kinesio Taping and Spine
3. Possible Explanation for the Effects of KT
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Raciborski, F.; Gasik, R.; Klak, A. Disorders of the spine. A major health and social problem. Reumatology 2016, 54, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Coenen, P.; Smith, A.; Paananen, M.; O’Sullivan, P.; Beales, D.; Straker, L. Trajectories of Low Back Pain from Adolescence to Young Adulthood. Arthritis Care Res. 2017, 69, 403–412. [Google Scholar] [CrossRef] [PubMed]
- Alshami, A.M. Prevalence of spinal disorders and their relationships with age and gender. Saudi Med. J. 2015, 36, 725–730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Czaprowski, D.S.Ł.; Stoliński, Ł.; Tyrakowski, M.; Kozinoga, M.; Kotwicki, T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018, 13, 6. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; De Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT Guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growt. Scoliosis 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Braccialli, L.M.P.; Vilarta, R. Aspectos a serem considerados na elaboração de programas de prevenção e orientação de problemas posturais. Rev. Paul. Educ. Fis. 2000, 14, 159–171. [Google Scholar]
- Detsch, C.; Candotti, C.T. A incidência de desvios posturais em meninas de 6 a 17 anos da cidade de Novo Hamburgo. Rev. Mov. 2000, 7, 43–56. [Google Scholar]
- Sedrez, J.A.; Da Rosa, M.I.; Noll, M.; Medeiro Fda, S.; Candotti, C.T. Risk factors associated with structural postural changes in the spinal column of children and adolescence. Rev. Paul Pediatr. 2015, 33, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Ferrándiz, M.E.; Castro-Sánchez, A.M.; Matarán-Peñarrocha, G.A.; García-Muro, F.; Serge, T.; Moreno-Lorenzo, C. Effects of kinesion taping on venous symptoms, bioelectrical activity of the gastrocnemius muscle, range of ankle motion, and quality of life in postmeno pausal women with chronic venous insufficieny: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2013, 94, 2315–2328. [Google Scholar]
- Kase, K.; Wallis, J.; Kase, T. Clinical Therapeutic Application of the Taping Method, 3rd ed.; KinesioTaping Association: Boston, MA, USA, 2003; pp. 39–42. [Google Scholar]
- Williams, S.; Whatman, C.; Hume, P.A.; Sheerin, K. Kinesio taping in treatment and preevention of sports injuries: A meta-analysis of the evidence for its effectiveness. Sports Med. 2012, 42, 153–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, M.; Julu, P.O.O.; Monro, J.A.; Coutinho, J.; Ijeh, C.; Puri, B.K. Neuromuscular taping reduces blood pressure in systemic arterial hypertension. Med. Hypotheses 2018, 116, 30–32. [Google Scholar] [CrossRef] [PubMed]
- Kase, K.; Tatsuyuki, H.; Tomoki, O. Development of Kinesiotape. Kinesiotaping Perfect Manual, 1st ed.; Kinesio Taping Association: Boston, MA, USA, 1996; pp. 5–11. [Google Scholar]
- Serrao, J.C.; Mezencio, B.; Claudino, J.C.; Soncin, R.; Miyashiro, S.P.L.; Sousa, P.E.; Borges, E.; Zanetti, V.; Phillip, I.; Mochizuki, L.; et al. Effect of 3 different applications of Kinesio Taping Denko on electromyographic activity: Inhinibion or facilitation of the quadriceps of males during squat exercise. J. Sport Sci. Med. 2016, 15, 403–409. [Google Scholar]
- Hagen, L.; Helbert, J.J.; Dekanich, J.; Koppenhaver, S. The effect of elastic therapeutic taping on back extensor muscle endurance in patients with low back pain: A randomized, controlled, crossover trial. J. Orthop. Sports Phys. Ther. 2015, 45, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Ekiz, T.; Aslan, M.D.; Özgirgin, N. Effects of kinesio tape application to quadriceps muscle on isokinetic muscle stegnth, gait and functional parameters in patients with stroke. J. Rehabil. Res. Dev. 2015, 52, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Aydoğdu, O.; Sari, Z.; Yurdalan, S.U.; Polat, M.G. Clinical outcome of kinesio taping applied in patients with knee osteoarthritis: A randomized controlled trial. J. Back Musculiskelet. Rehabil. 2017, 30, 1045–1051. [Google Scholar] [CrossRef] [PubMed]
- Castrogiovanni, P.; Di Giunta, A.; Guglielmino, C.; Roggio, F.; Romeo, D.; Fidone, F.; Imbesi, R.; Loreto, C.; Castorina, S.; Musumeci, G. The effects of exercise and kinesio tape on physical limitations in patients with knee osteoarthritis. J. Funct. Morphol. Kinesiol. 2016, 1, 355. [Google Scholar] [CrossRef]
- Musumeci, G. Sarcopenia and exercise “The State of the Art”. J. Funct. Morpholog. Kinesiolog. 2017, 2, 40. [Google Scholar] [CrossRef]
- Wageck, B.; Nunes, G.S.; Bohlen, N.B.; Santos, G.M.; De Noronha, M. Kinesio Taping does not improve the symptoms or function of older people with knee osteoarthritis: A randomised trial. J. Physiother. 2016, 62, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Boobphachart, D.; Manimmanakorn, N.; Manimmanakorn, A.; Thuwakum, W.; Hamlin, M.J. Effect of elastic taping, non-elastic taping and static stretching on recovery after intensive eccentric exercise. Res. Sports Med. 2017, 25, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, S.; Lee, J. Longer application of kinesio taping would be beneficial for exercise-induced muscle damage. J. Exerc. Rehabil. 2016, 12, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Bae, S.H.; Hwang, J.A.; Kim, K.Y. The effects of kinesio taping on architecture, strength and pain of muscles in delayed onset muscle soreness of biceps brachii. J. Phys. Sci. 2015, 27, 457–459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Öztürk, G.; Külcü, D.G.; Mesci, N.; Şilte, A.D.; Aydog, E. Efficacy of kinesio tape application on pain and muscle strength in patients with myofascial pain syndrome: A placebo-controlled trial. J. Phys. Sci. 2016, 28, 1074–1079. [Google Scholar] [CrossRef] [PubMed]
- Karabay, İ.; Doğan, A.; Ekiz, T.; Köseoğlu, B.F.; Ersöz, M. Training postural control and sitting in children with cerebral palsy: Kinesio taping vs. neuromuscular electrical stimulation. Complement. Clin. Pract. 2016, 24, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Voos, M.C.; Oliveira Tde, P.; Piemonte, M.E.; Barbosa, E.R. Case report: Physical therapy managment of axial dystonia. Physioter. Theory Pract. 2014, 30, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.H.; Lee, J.H. Effects of proprioceptive sense-based kinesio taping on walking imbalance. J. Phys. Ther. Sci. 2016, 28, 3060–3062. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.K.; Nam, C.W.; Lee, J.H.; Park, Y.H. The effect of taping prior to PNF treatment on lower etremity proprioception of hemiplegic pateints. J. Phys. Ther. Sci. 2013, 25, 1119–1122. [Google Scholar] [CrossRef] [PubMed]
- Capecci, M.; Serpicelli, C.; Fiorentini, L.; Censi, G.; Ferretti, M.; Orni, C.; Renzi, R.; Provinciali, L.; Ceravolo, M.G. Postural rehabilitation and kinesio taping for axial postural disorders in Parkinsons’s disease. Arch. Phys. Med. Rehabil. 2014, 95, 1067–1075. [Google Scholar] [CrossRef] [PubMed]
- Lambert, F.M.; Malinvaud, D.; Glaunès, J.; Bergot, C.; Straka, H.; Vidal, P.P. Vestibular asymmetry as the cause of idiopathic scoliosis: A possible answer from Xenopus. J. Neurosci. 2009, 29, 12477–12483. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Yoo, W.C. Application of posterior pelvic tilt taping for the treatment of chronic low back pain with sacroiliac joint dysfunction and increased horizontal angle. Phys. Ther. Sport 2012, 3, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Sneag, D.B.; Bendo, J.A. Pregnancy-related low back pain. Orthopedics 2007, 30, 839–845. [Google Scholar] [PubMed]
- Kaplan, S.; Alpayci, M.; Karaman, E.; Çetin, O.; Özkan, Y.; İlter, S.; Şah, V.; Şahin, H.G. Short-term effects of kinesio taping in women with pregnancy-related low back pain: A randomized controlled clinical trial. Med. Sci. Monit. 2016, 18, 1297–1301. [Google Scholar] [CrossRef]
- Kalinowski, P.; Krawulska, A. Kinesio taping vs. placebo taping in reducing pregnancy-related low back pain: A cross over study. Med. Sci. Monit. 2017, 26, 6114–6120. [Google Scholar] [CrossRef]
- Kamali, F.; Sinaei, E.; Taherkhani, E. Comparing spinal manipulation with and without kinesio taping in the treatment of chronic low back pain. J. Bodyw. Ovement Ther. 2018, 22, 540–545. [Google Scholar] [CrossRef] [PubMed]
- González-Iglesias, J.; Fernández-de-Las-Peñas, C.; Cleland, J.A.; Huijbregts, P.; Del Rosario Gutiérrez-Vega, M. Short-term effect of cervical kinesio taping on pain and cervical range of motion in patients with acute whiplash injury: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2009, 39, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Preece, H.; White, P. Does kinesiology tape increase trunk forward flexion? J. Bodywork Mov. Ther. 2017, 21, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Airaksinen, O.; Brox, J.I.; Cedraschi, C.; Hildebrandt, J.; Klaber-Moffett, J.; Kovacs, F.; Mannion, A.F.; Reis, S.; Staal, J.B.; Ursin, H.; et al. European guidelines for the managment of chronic on-specific low back pain. Eur. Spine J. 2006, 15, 192–300. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Álvarez, S.; José, F.G.; Rodríguez-Fernández, A.L.; Güeita-Rodríguez, J.; Waller, B.J. Effects of kinesio tape in low back muscle fatigue: Randomized, controlled doubled-blinded clinical trial on healthy subjects. J. Back Muscoskelet. Rehabil. 2014, 27, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Nelson, N.L. Kinesio taping for chronic low back pain: A systematic review. J. Bodyw. Mov. Ther. 2016, 20, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Castro-Sanchez, A.M.; Lara-Palomo, I.C.; Matarán-Peñarrocha, G.A.; Fernández-Sánchez, M.; Sánchez-Labraca, N.; Arroyo-Morales, M. Kinesio taping reduces disability and pain slighly in chronic non-specific low-back pain: A randomised trial. J. Phys. 2012, 58, 89–95. [Google Scholar]
- Velasco-Rodan, O.; Riquelme, I.; Ferragut-Garcías, A.; Heredia-Rizo, A.M.; Rodríguez-Blanco, C.; Oliva-Pascual-Vaca, Á. Effects of Kinesio Taping Tightness in Low Back Pain. PMR J. 2018, 10, 28–35. [Google Scholar]
- Parreira, S.P.C.; Costa Lda, C.; Takahashi, R.; Hespanhol Junior, L.C.; Luz Junior, M.A.; Silva, T.M.; Costa, L.O. Kinesio taping to generate skin convolutions is not better than sham taping for people with chronic non-specific low back pain: A randomised trial. J. Phys. 2014, 60, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Copurgensli, C.; Gur, G.; Tunay, V.B. A comparison of the effects of mulligan’s mobilization and kinesio taping on pain, range of motion, muscle strength and neck disability in patient with cervical spondylolysis: A randomized controlled study. J. Back Muscoskelet. Rehabil. 2017, 30, 51–62. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; Westrick, R.; Diebal, A.; Marks, C.; Gerber, J.P. Immediate effects of lumbopelvic manipulation and lateral gluteal taping on unilateral patellofemoral pain syndrome: A pilot study. Sport Phys. Ther. 2013, 5, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Saavedra-Hernández, M.; Castro-Sánchez, A.M.; Arroyo-Morales, M.; Cleland, J.A.; Lara-Palomo, I.C.; Fernández-de-Las-Peñas, C. Short-term effects of kinesio taping versus cervical thrust manipulation in patients with mechanical neck pain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2012, 42, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Rigo, M.; Weiss, H. The Chêneau concept of bracing—Biomechanical aspects. Stud. Health Technol. Inform. 2008, 135, 303–319. [Google Scholar] [PubMed]
- Paolucci, T.; Morone, G.; Di Cesare, A.; Grasso, M.R.; Fusco, A.; Paolucci, S.; Saraceni, V.M.; Iosa, M. Effect of chêneau brace on postural balance in adolescent idiopathic scoliosis: A pilot study. Eur. J. Phys. Rehabil. Med. 2013, 49, 649–657. [Google Scholar] [PubMed]
- Misterska, E.; Glowacki, M.; Harasymczuk, J. Brace and deformity-related stress level in females with adolescent ideopathic scoliosis based on the bad sobernheim stress questionnaire. Med. Sci. Monit. 2011, 17, CR83–CR90. [Google Scholar] [CrossRef] [PubMed]
- Gur, G.; Dilek, B.; Ayhan, C.; Simsek, E.; Aras, O.; Aksoy, S.; Yakut, Y. Effect of a spinal brace on postural control in different sensory conditions in adolescent idiopathic scoliosis: A preliminary analysis. Gait Posture 2015, 41, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Eshraghi, A.; Maroufi, N.; Sanjari, M.A.; Saeedi, H.; Keyhani, M.R.; Gholizadeh, H.; Osman, N.A. Effect of Milwaukee brace on static and dynamic balance of female hyperkyphotic adolescents. Prosthet. Orthot. Int. 2013, 37, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, H.; Allard, P.; Barbier, F.; Gatto, L.; Chavet, P.; Rivard, C.H.; Hinse, S.; Simoneau, M. Bracing has no effect on standing balance in females with adolescent idiopathic scoliosis. Med. Sci. Monit. 2008, 14, CR293–CR298. [Google Scholar] [PubMed]
- Bayar, B.; Uygur, F.; Bayar, K.; Bek, N.; Yakut, Y. The short-term effects of an exercise programme as an adjunct to an orthosis in neuromuscular scoliosis. Prosthet. Orthot. Int. 2004, 28, 273–277. [Google Scholar] [PubMed]
- Poon, K.Y.; Li, S.M.; Roper, M.G.; Wong, M.K.; Wong, O.; Cheung, R.T. Kinesiology type does not facilitate muscle performance: A deceptive controlled trial. Man. Ther. 2015, 20, 130–133. [Google Scholar] [CrossRef] [PubMed]
- Cai, C.; Au, I.P.; An, W.; Cheung, R.T.I. Facilitatory and inhibitory effects of Kinesio tape: Fact or fad? J. Sci. Med. Sport 2016, 19, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Lins, C.A.; Neto, F.L.; Amorim, A.B.; Macedo Lde, B.; Brasileiro, J.S. Kinesio taping does not alter neuromuscular performance of femoral quadriceps or lower limb function in healthy subjects: Randomized, blind, controlled, clinical trial. Man. Ther. 2013, 18, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Bienfait, M. Estudo e Tratamento do Esqueleto Fibroso-Fascias e Pompages, 5th ed.; Summus Editorial: Spain, 1999; pp. 89–95. [Google Scholar]
- Cimino, S.R.; Beaudette, S.M.; Brown, S.H.M. Kinesio tape influences the mechanical behaviour of the skin of the low back: A possible pathways for functionally relevant effects. J. Biomech. 2018, 23, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Lemos, T.V.; Albino, A.C.; Matheus, J.P.; Barbosa Ade, M. The Effect of Kinesio Taping in Forward Bending of the Lumbar Spine. J. Phys. Ther. Sci. 2014, 26, 1371–1375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, H.Y.; Chou, K.Y.; Lin, J.J.; Lin, C.F.; Wang, C.H. Immediate effect of forearm Kinesio taping on maximal grip strength and force sense in healthy collegiate athletes. Phys. Ther. Sport 2010, 11, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, L.; Babisch, C.; Babisch, J.; Layher, F.; Sander, K.; Matziolis, G.; Pietsch, S.; Röhner, E.; Bischoff, L.B. Effects on proprioception by kinesio taping of the knee after anterior cruciate ligament rupture. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 1157–1164. [Google Scholar] [CrossRef] [PubMed]
- Ridding, M.C.; Brouwer, B.; Miles, T.S.; Pitcher, J.B.; Thompson, P.D. Changes in muscle response to stimulation of the motor cortex induced by peripheral nerve stimulation in human subjects. Exp. Brain Res. 2000, 131, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Maratou, E.; Theophilidis, G. An axon pacemaker: Diversity in the mechanism of generation and conduction of action potentials in snail neurons. Neuroscience 2000, 96, 1–2. [Google Scholar] [CrossRef]
- De Ru, E. The possibilities of using elastic therapeutic (Kinesio) tape in patients with scoliosis. Scoliosis 2014, 9, P12. [Google Scholar] [CrossRef]
- Romano, M.; Negrini, A.; Parzini, S.; Tavernaro, M.; Zaina, F.; Donzelli, S.; Negrini, S. SEAS (Scientific Exercises Approach to Scoliosis): A modern and effective evidence based approach to physiotherapic specific scoliosis exercises. Scoliosis 2015, 10, 3. [Google Scholar] [CrossRef] [PubMed]
- Paoloni, M.; Bernetti, A.; Fratocchi, G.; Mangone, M.; Parrinello, L.; Cooper, M.D.P.; Sesto, L.; Di Sante, L.; Santilli, V. Kinesio Taping applied to lumbar muscles influences clinical and electromyographic characteristics in chronic low back pain patients. Eur. J. Phys. Rehabil. Med. 2011, 47, 237–244. [Google Scholar] [PubMed]
- Mostafavifar, M.; Wertz, J.; Borchers, J. A systematic review of the effectiveness of kinesio taping for musculoskeletal injury. Phys. Sportsmed. 2012, 40, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Hsieh, T.; Lu, S.; Su, F. Effect of kinesio tape to muscle activity and vertical jump performance in healthy active people. Biomed. Eng. Online 2011, 10, 70. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Fu, W.; Pan, J.; Wang, L.; Xia, R.; Liu, Y. Acute effects of Kinesio taping on muscle strength and fatigue in the forearm of tennis players. J. Sci. Med. Sport 2016, 19, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Choi, I.R.; Lee, J.H. Effect of kinesiology tape application direction on quadriceps strength. Medicine 2018, 97, e11038. [Google Scholar] [CrossRef] [PubMed]
- Macedo, L.B.; Richards, J.; Borges, D.T.; Melo, S.A.; Brasileiro, J.S. Kinesio Taping reduces pain and improves disability in low back pain patients: A randomized controlled trial. Physiotherapy 2018. [Google Scholar] [CrossRef] [PubMed]

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borzì, F.; Szychlinska, M.A.; Di Rosa, M.; Musumeci, G. A Short Overview of the Effects of Kinesio Taping for Postural Spine Curvature Disorders. J. Funct. Morphol. Kinesiol. 2018, 3, 59. https://doi.org/10.3390/jfmk3040059
Borzì F, Szychlinska MA, Di Rosa M, Musumeci G. A Short Overview of the Effects of Kinesio Taping for Postural Spine Curvature Disorders. Journal of Functional Morphology and Kinesiology. 2018; 3(4):59. https://doi.org/10.3390/jfmk3040059
Chicago/Turabian StyleBorzì, Francesca, Marta Anna Szychlinska, Michelino Di Rosa, and Giuseppe Musumeci. 2018. "A Short Overview of the Effects of Kinesio Taping for Postural Spine Curvature Disorders" Journal of Functional Morphology and Kinesiology 3, no. 4: 59. https://doi.org/10.3390/jfmk3040059