Development of Small-Footprint Thermal Sensor Detecting Airflow at Mouth in Baby †
Abstract
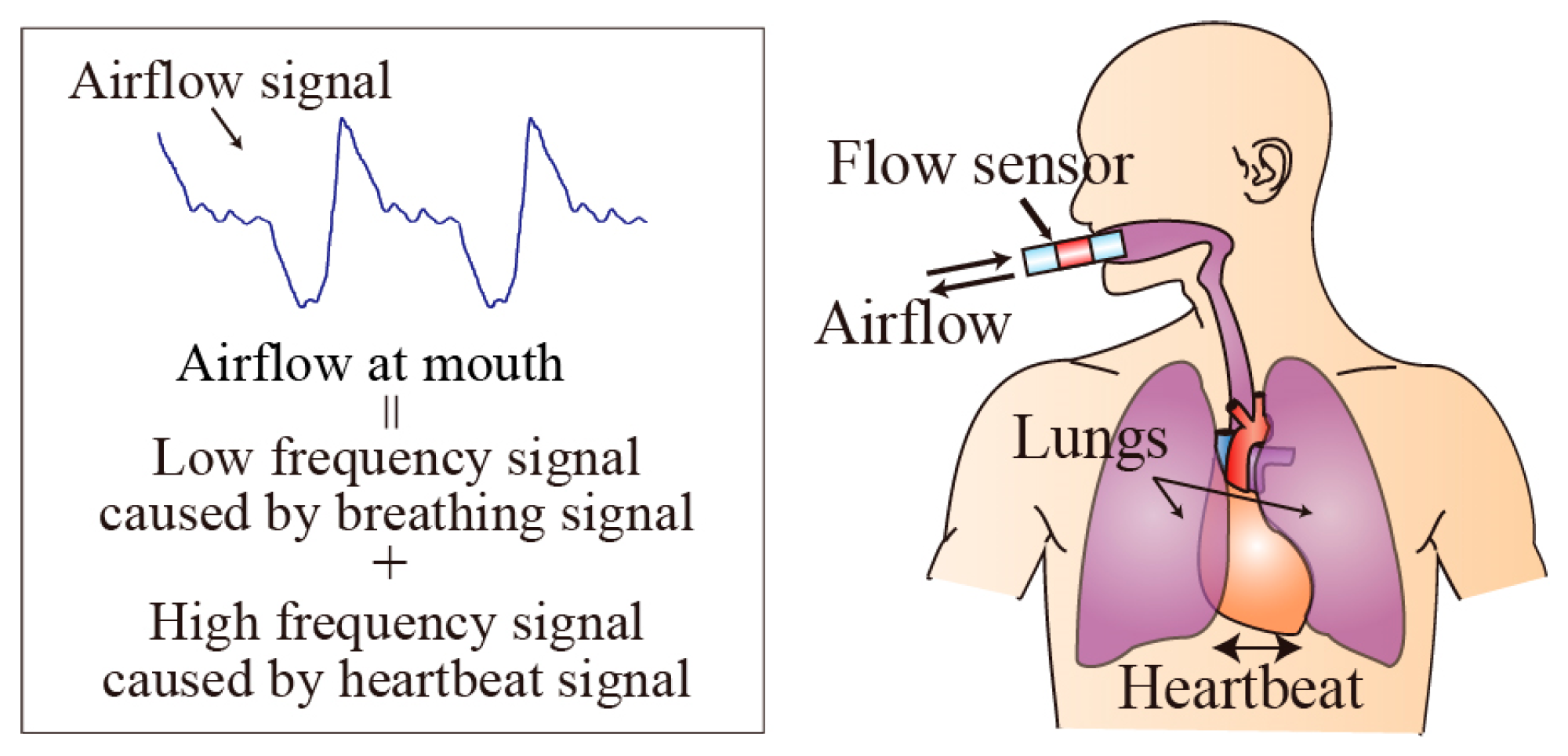
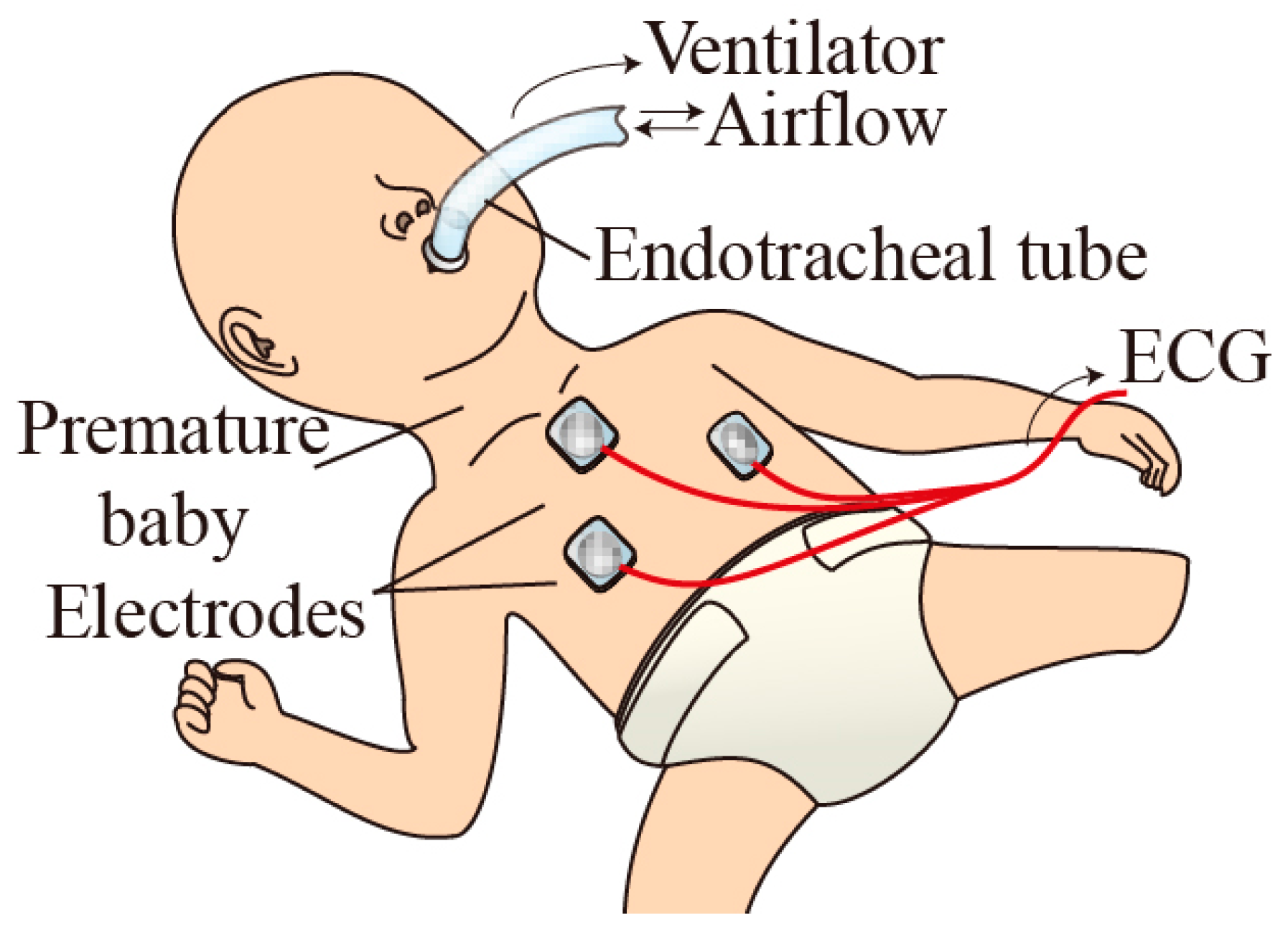
:1. Introduction
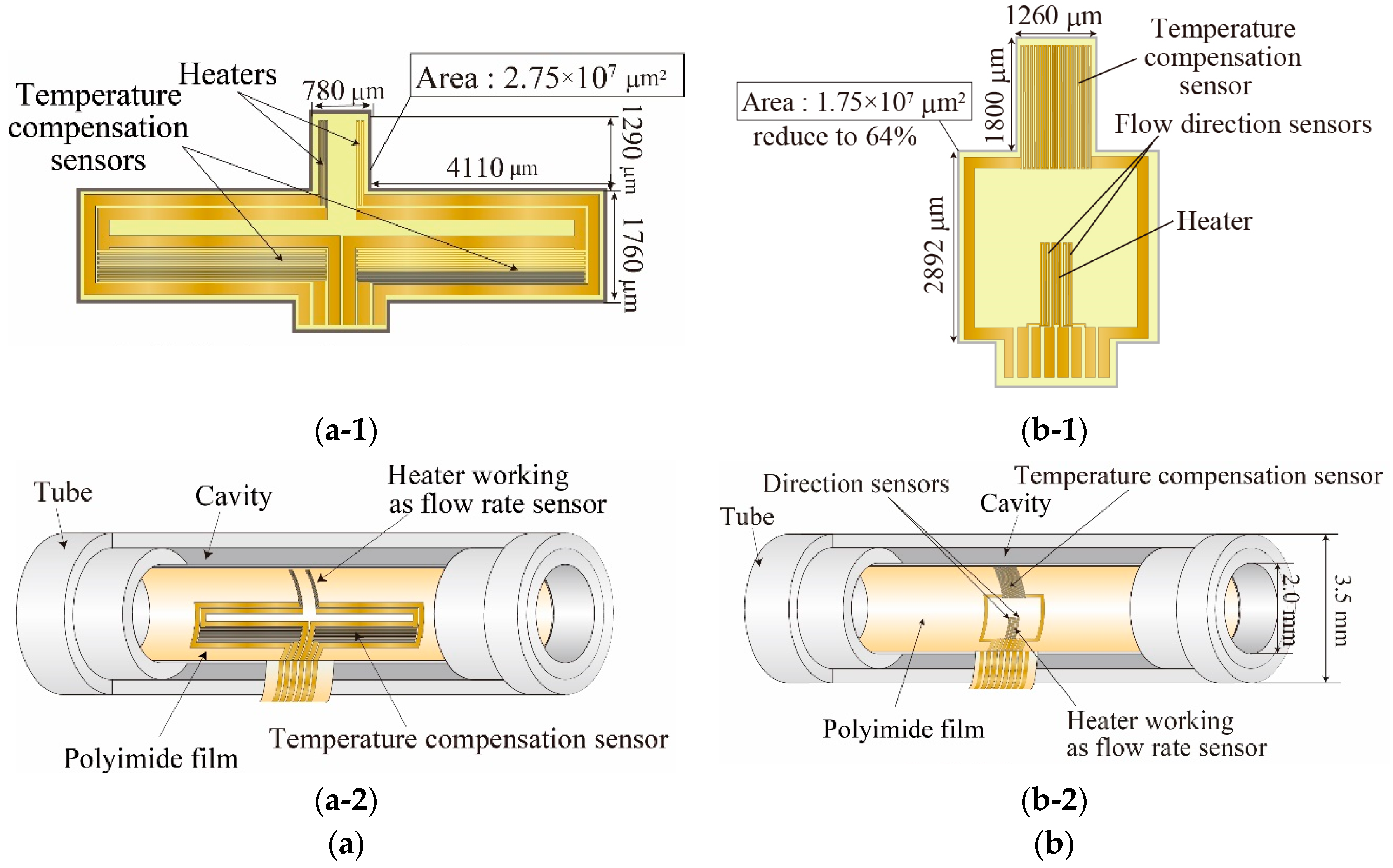
2. Tube Flow Sensor
2.1. Sensor Design
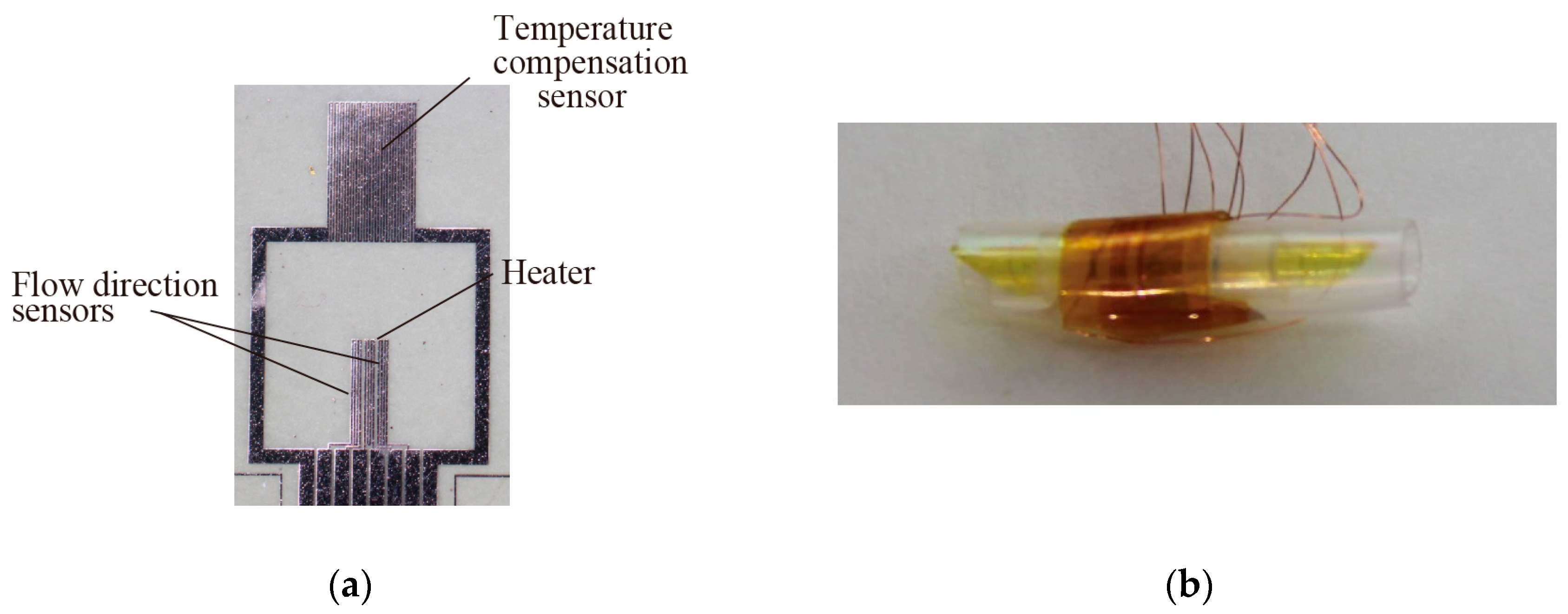
2.2. Sensor Fabrication
3. Experiments and Results
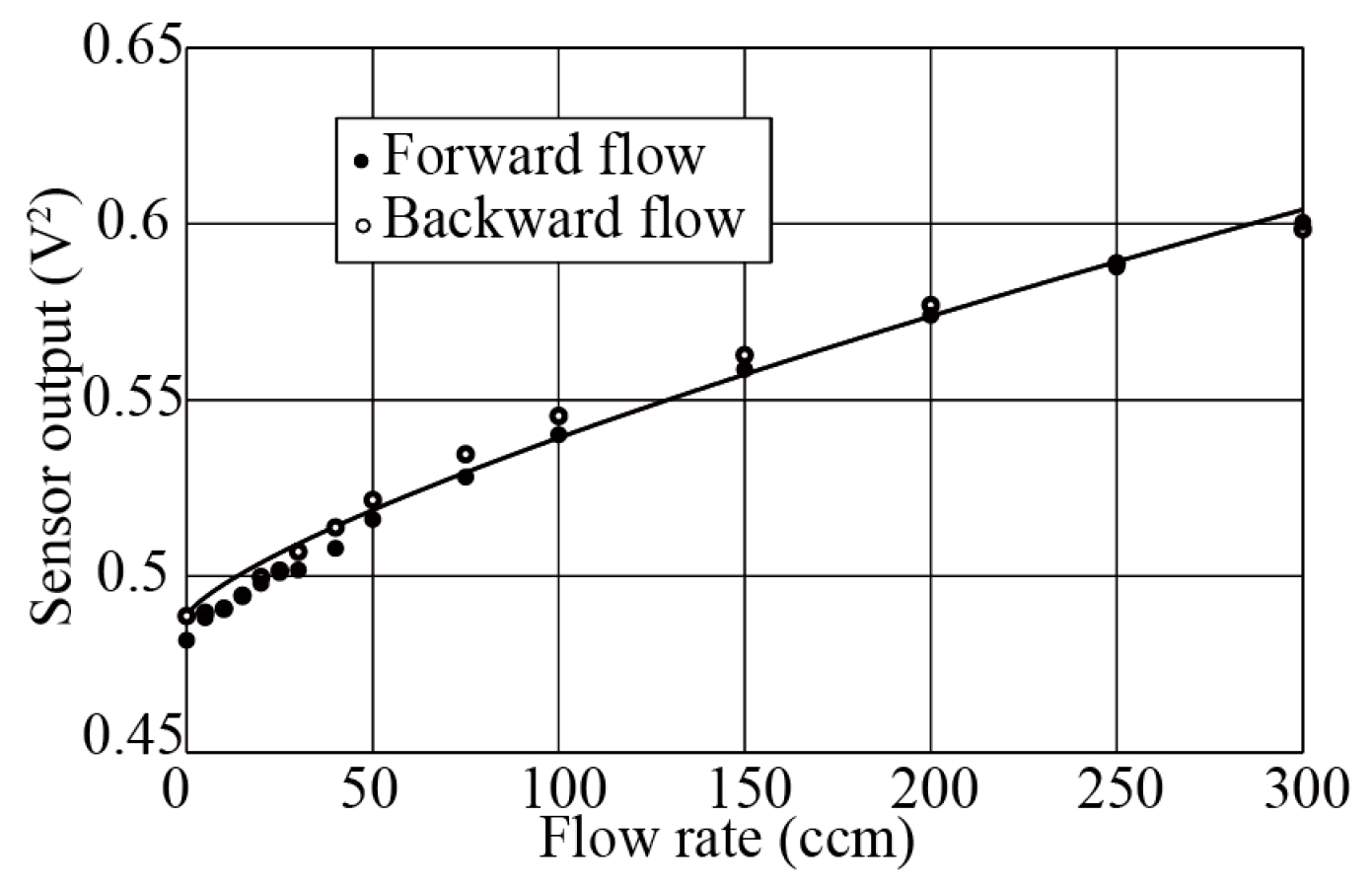
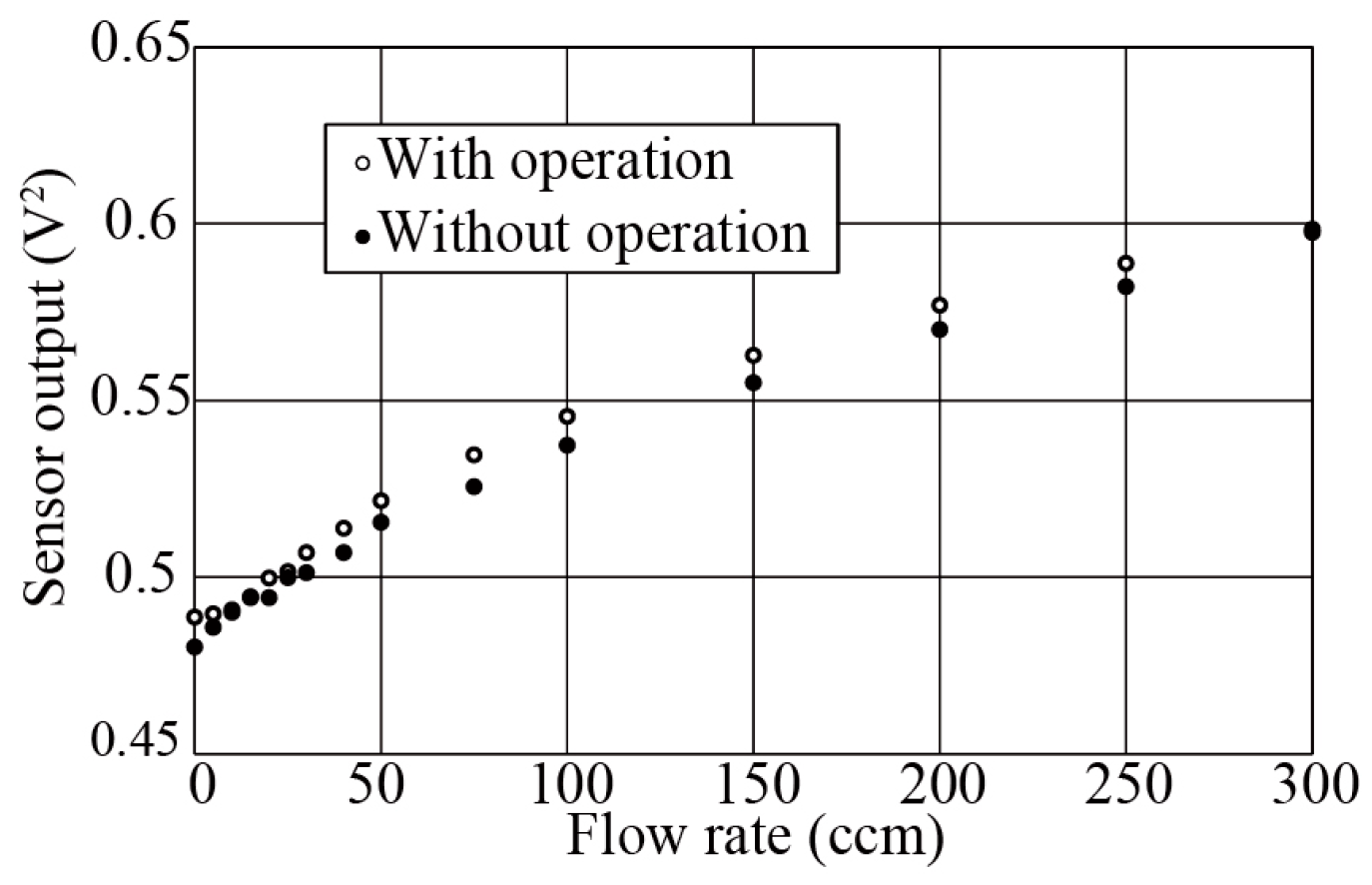
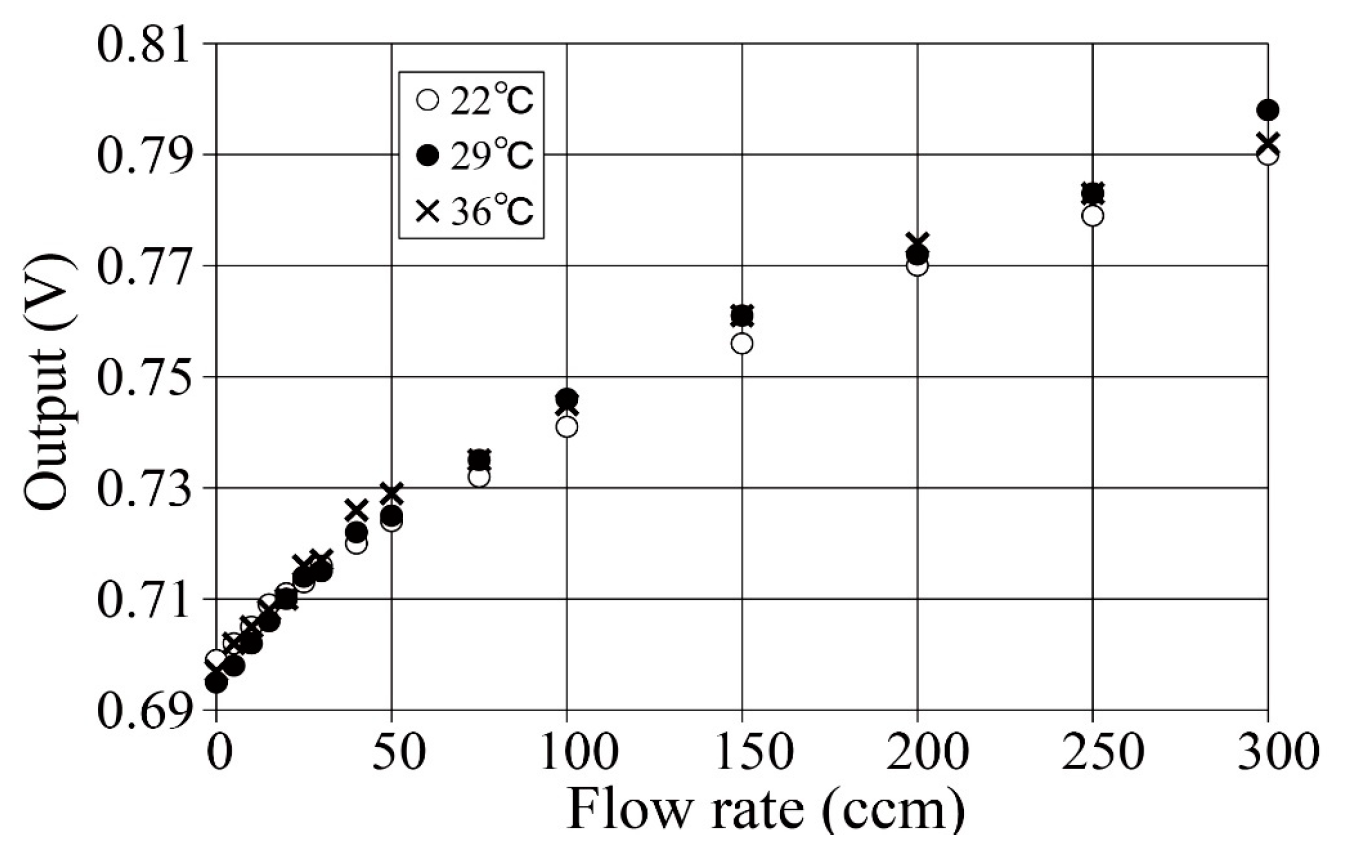
3.1. Flow Rate Measurement
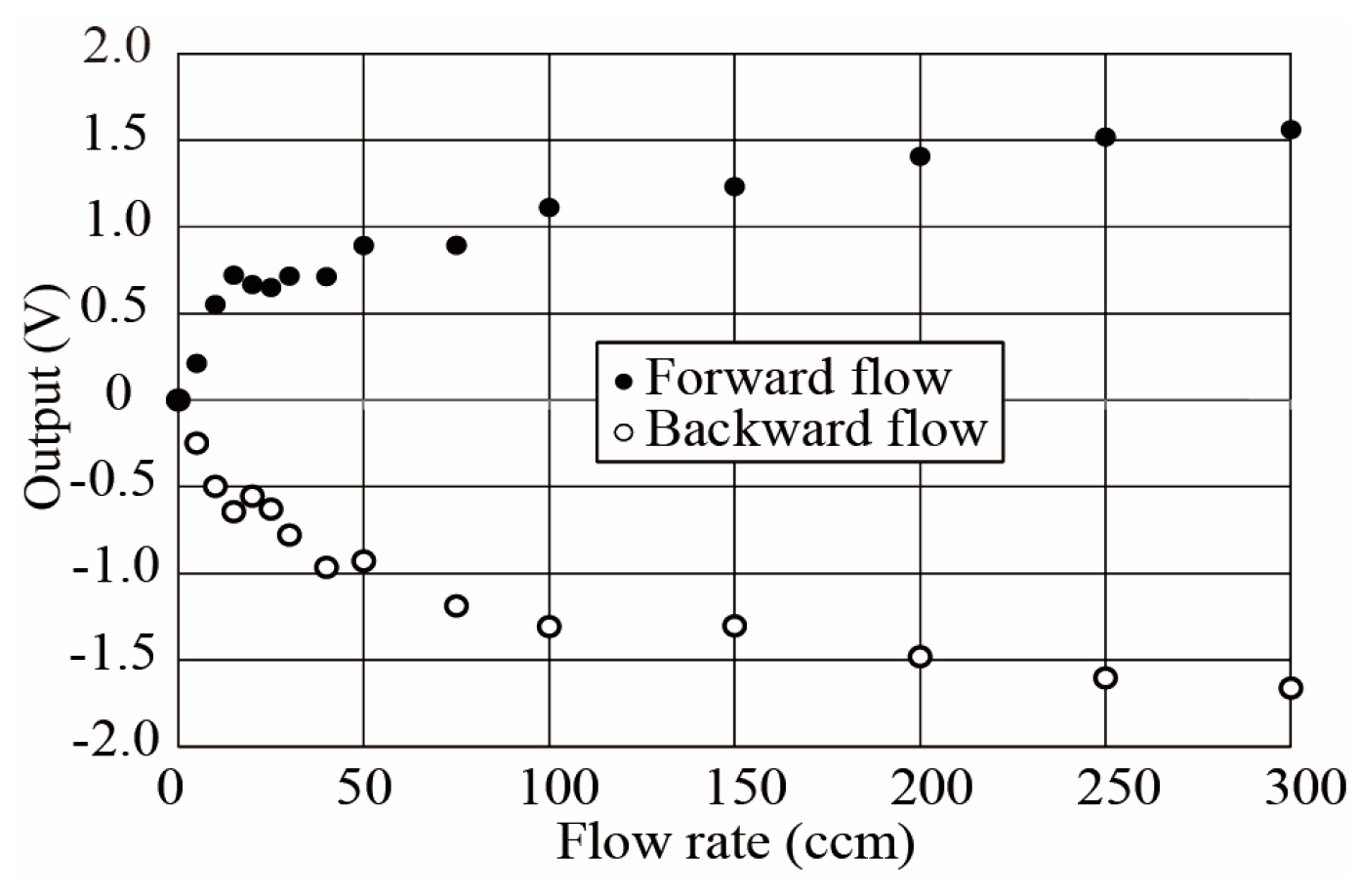
3.2. Flow Direction Measurement
4. Conclusions
Acknowledgments
Conflicts of Interest
References
- Kawaoka, H.; Yamada, T.; Matsushima, M.; Kawabe, T.; Hasegawa, Y.; Shikida, M. Detection of kinetic heartbeat signals from airflow at mouth by catheter flow sensor with temperature compensation. In Proceedings of the Technical Digit of IEEE MEMS Conference, Shanghai, China, 24 January 2016; pp. 359–362. [Google Scholar]
- Watanabe, S. Response time shortening in thermal catheter flow sensor. In Proceedings of the Technical Digit of Asia-Pacific Conference of Transducers and Micro-Nano Technology 2016, Kanazawa, Japan, 26–29 June 2016; pp. 253–254. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitsunari, Y.; Hasegawa, Y.; Matsushima, M.; Kawabe, T.; Shikida, M. Development of Small-Footprint Thermal Sensor Detecting Airflow at Mouth in Baby. Proceedings 2017, 1, 359. https://doi.org/10.3390/proceedings1040359
Mitsunari Y, Hasegawa Y, Matsushima M, Kawabe T, Shikida M. Development of Small-Footprint Thermal Sensor Detecting Airflow at Mouth in Baby. Proceedings. 2017; 1(4):359. https://doi.org/10.3390/proceedings1040359
Chicago/Turabian StyleMitsunari, Yuki, Yoshihiro Hasegawa, Miyoko Matsushima, Tsutomu Kawabe, and Mitsuhiro Shikida. 2017. "Development of Small-Footprint Thermal Sensor Detecting Airflow at Mouth in Baby" Proceedings 1, no. 4: 359. https://doi.org/10.3390/proceedings1040359




