Abstract
Objective—The objective of this study was to systematically assess meta-analyses to determine the lacunae in the literature for PCF following laryngectomy. Methods—Bibliometric analysis were carried out on meta-analyses on PCF after total laryngectomy for laryngeal cancer in the PubMed database. Results—Twenty-four meta-analyses were considered eligible and chosen for analysis. Six meta-analyses (25%) focused on the risk factors for PCF in TL. Four meta-analyses (16.6%) focused on the role of the onlay flap. Four meta-analyses (16.6%) focused on the timing of feed initiation. Three meta-analyses (12.5%) focused on using a stapler for pharyngeal closure. Two meta-analyses focused on types of pharyngeal reconstruction. Other meta-analyses analyzed the use of salivary bypass tubes, the method of pharyngeal closure, organ preservation protocols on PCF, primary and secondary TEP, and the effect of non-surgical treatment on PCF. Conclusion—Despite plenty of published meta-analyses, there is a lack of scrutiny on certain critical aspects of PCF.
1. Introduction
Pharyngocutaneous fistula (PCF) is a common complication that occurs after total laryngectomy (TL), and it can lead to increased morbidity. PCF can cause a more extended hospital stay, the need for nasogastric feeding, and delays in adjuvant therapy. It may also require additional surgery to reconstruct the pharyngeal defects [1]. As technology continues to evolve, new solutions are emerging that may provide alternative treatment methods. Surgeons aim for a complication-free postoperative period to ensure timely adjuvant therapy and improved outcomes [2]. Recently, there has been an increased focus on publications regarding pharyngocutaneous fistula, particularly in meta-analyses. Therefore, we intend to thoroughly analyze the bibliometrics of PCF meta-analyses to identify the study objectives and outcomes of published meta-analyses on PCF following TL. We also intend to identify gaps in the published data to better guide our planning of future studies on PCF.
2. Methods
2.1. Search Strategy
We have included only the PubMed/MEDLINE database to obtain the published meta-analyses on PCF. Published literature in English from inception to 2023 was considered.
2.2. Search Syntax
The search terms “pharyngocutaneous” [All Fields] AND (“fistula” [MeSH Terms] OR “fistula” [All Fields] OR “fistulas” [All Fields] OR “fistulas” [All Fields] OR “fistulae” [All Fields] OR “fistulaes” [All Fields]) AND (“laryngectomy” [MeSH Terms] OR “laryngectomy” [All Fields] OR “laryngectomies” [All Fields]) AND (“meta analysis” [Publication Type] OR “meta analysis as topic” [MeSH Terms] OR “meta analysis” [All Fields]) were used to obtain the results. The data were last retrieved on 26 April 2023.
2.3. Data Screening and Selection
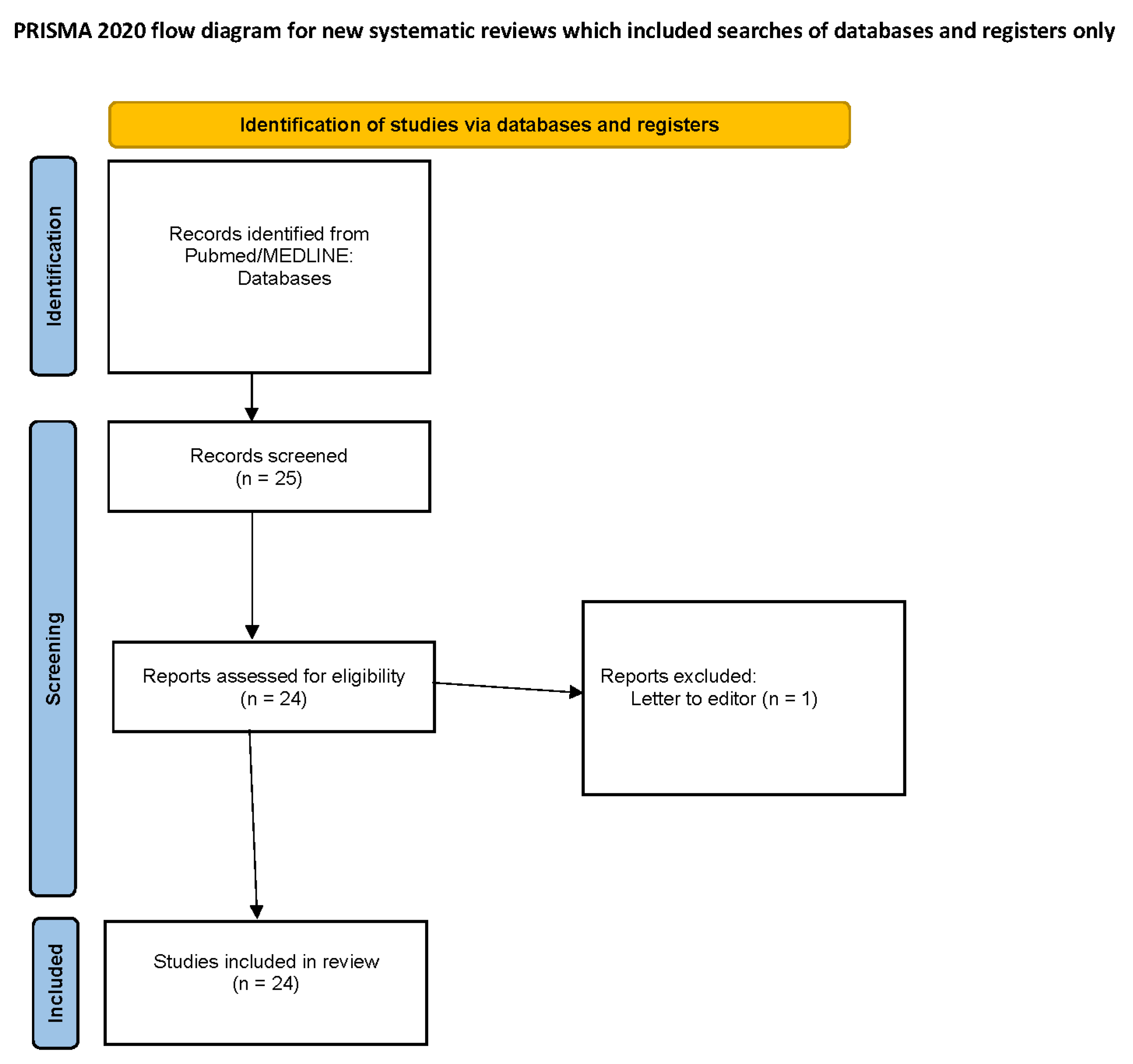
The retrieved articles were initially screened independently by KNR based on the type of article, title, and abstract. The eligible meta-analyses were pooled, and a thorough full-text analysis was conducted (Figure 1). The articles were selected based on concurrence with the predefined inclusion and exclusion criteria.
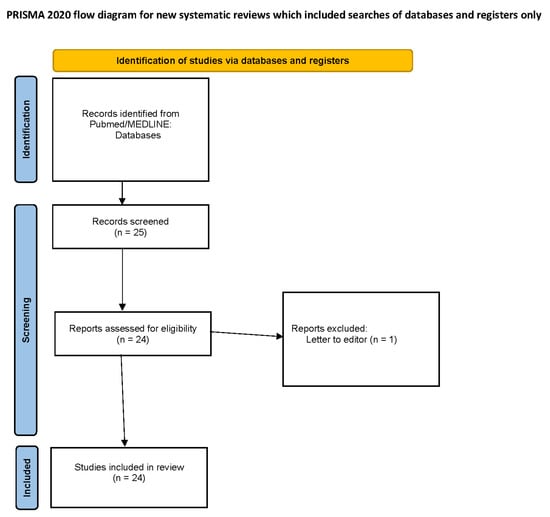
Figure 1.
PRISMA flowchart.
2.4. Inclusion Criteria
- Total laryngectomy/laryngopharyngectomy for laryngeal and hypopharyngeal cancer;
- Laryngeal or hypopharyngeal cancers with total laryngectomy/laryngopharyngectomy (with or without neck dissection) as primary or salvage therapy;
- A meta-analysis published in peer-reviewed journals;
- Meta-analysis must report on pharyngocutaneous fistula following total laryngectomy/laryngopharyngectomy.
2.5. Exclusion Criteria
- Non-human studies;
- Laryngectomy/laryngopharyngectomy for non-oncological reason;
- Not reported—regarding operative outcomes;
- Review articles, meeting abstracts, case reports, editorial letters, as well as other forms of publication;
- Incomplete data or insufficient information.
2.6. Data Extraction
All included articles were screened by KNR. The following study characteristics were recorded: first author, country, year of publication, journal, type of laryngectomy, research question, and study outcomes were analyzed (Table 1).

Table 1.
Summary of included meta-analyses.
2.7. Statistical Analysis
Descriptive statistical analysis was performed on the retrieved articles using Microsoft Excel version 2309.
3. Results
3.1. Literature Retrieval and Data Extraction
The initial literature search using the predefined search syntax identified 25 manuscripts. Upon title and abstract screening, only one article was excluded as it was a letter to the editor. Finally, 24 meta-analyses were considered eligible and chosen for analysis.
3.2. Year of Publication
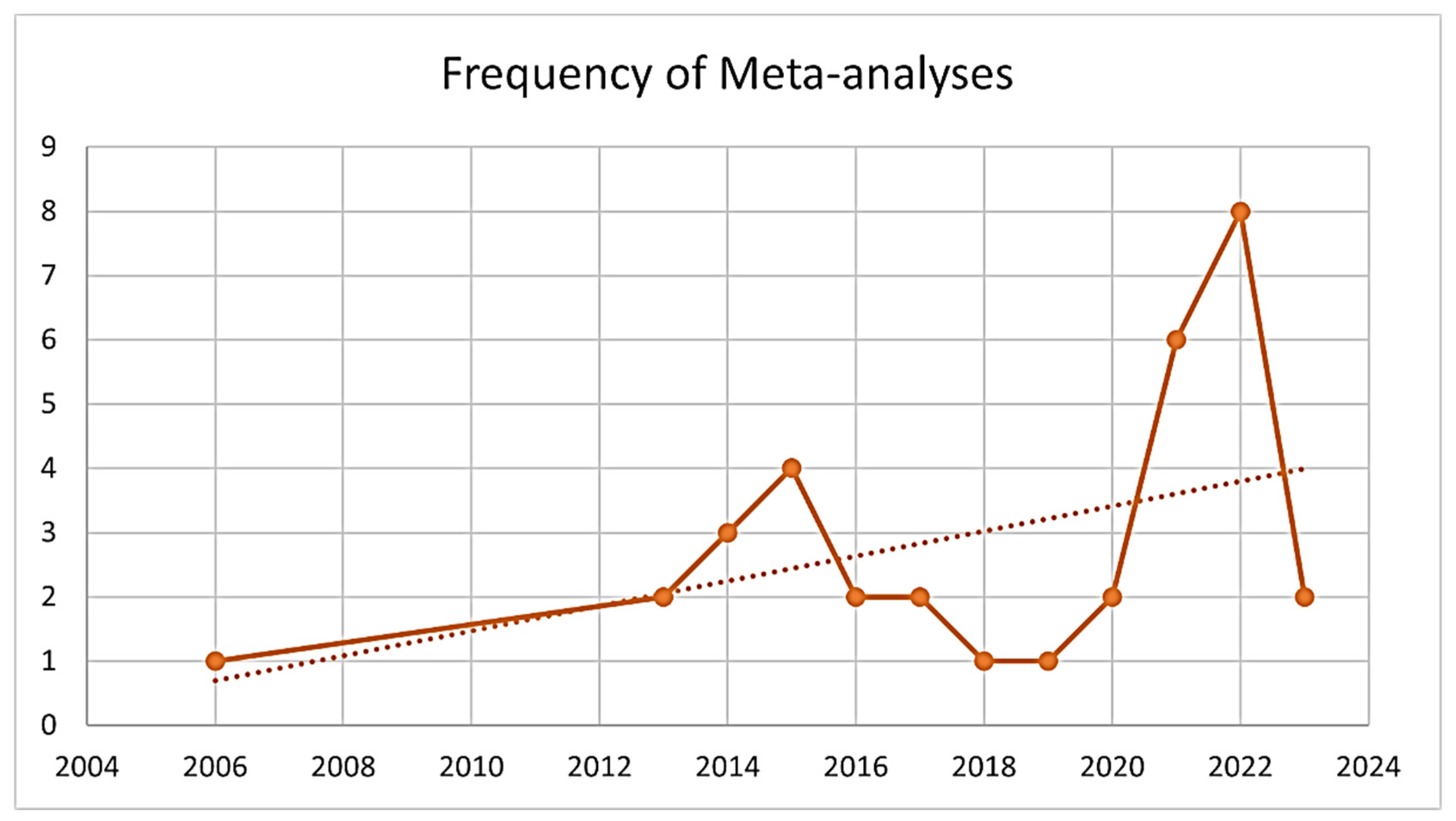
The first meta-analysis was published in the year 2006 [24]. Surprisingly, over 50% of the meta-analyses (n = 13) were published since 2021 (Figure 2).
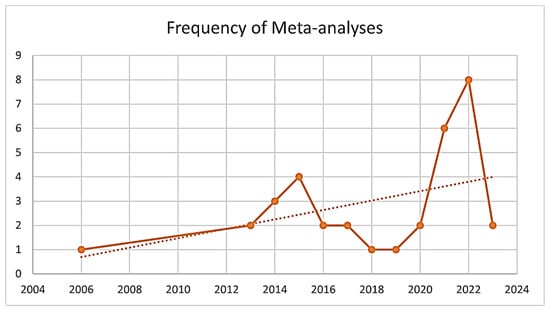
Figure 2.
Frequency of meta-analyses per year. (Solid line shows the number of published meta-analysis on PCF for that year; Dashed line shows the increasing trend of publications on PCF).
3.3. Country of Origin
The majority of the published meta-analyses (n = 5, 20.8%) originated from Italy [1,2,4,8,11], Brazil (n = 4, 16.6%) [17,18,19,21], the United Kingdom (n = 4, 16.6%) [13,15,22,23], China (n = 3, 12.5%) [10,14,20], and Australia (n = 2, 8.3%) [9,16], and one each from India [7], Thailand [6], South Korea [3], Taiwan [12], Spain [5], and the USA [24].
3.4. Type of Laryngectomy
Only one meta-analysis (4%) described exclusively PCF in primary TL [7]. Four meta-analyses (16.6%) described PCF exclusively on salvage TL [8,16,17,23]. The remaining fourteen meta-analyses (58.3%) described PCF in primary and salvage TL [1,2,3,4,5,6,9,10,11,12,13,14,15,19,20,21,22,24].
3.5. Journal
Six meta-analyses (25%) have been published in the Head Neck journal (affiliated with the International Federation of Head and Neck Oncologic Societies) [4,13,17,18,19,21]. Three were published in The Laryngoscope (affiliated with the American Triological Society) [3,22,23]. Two were published in the European archives of otorhinolaryngology (affiliated with the Confederation of European Otorhinolaryngologists) [8,14].
3.6. Research Question
Six meta-analyses (25%) focused on determining the risk factors for PCF in TL [3,7,14,19,20,24]. Four meta-analyses (16.6%) focused on the role of an onlay vascular flap over the pharyngeal closure in PCF [8,17,22,23]. Four meta-analyses (16.6%) focused on the timing of oral feed initiation in PCF [9,10,13,18]. Three meta-analyses (12.5%) focused on using a stapler for pharyngeal closure in PCF [5,12,21]. Two meta-analyses determined the risk of PCF following various types of pharyngeal reconstruction [1,2]. One meta-analysis analyzed the use of salivary bypass tubes in PCF [4]. One meta-analysis analyzed the method of pharyngeal closure in PCF [6]. One meta-analysis each described the role of organ preservation protocols in PCF [16], the rates of PCF following primary and secondary TEP [15], and the effect of non-surgical treatment on PCF [11].
3.7. Outcomes
- Risk factors for PCF was found to be age [3,14], smoking [14], low hemoglobin [3,7,14,19,20,24], low albumin [7,14], comorbidities [3,7,14,19], diabetes [3,7], chronic obstructive pulmonary disease [14,19], coronary artery disease [14], tumor site [3,14,19,20], hypopharyngeal involvement [7,19], previous radiation therapy [3,14,19,20,24], margins [7,19,20], type of pharyngeal closure [7,14], TEP [3], neck dissection [19,24], and blood transfusion [19];
- An onlay vascular flap over the pharyngeal closure led to lower rates of PCF [8,17,22,23].
- Timing of feed initiation—early feed initiation was found to have slightly higher PCF rates [9]; no significant difference was found between early and late feeds [10,13,18];
- The use of stapler for pharyngeal closure equivocally led to lower rates of PCF with stapler usage [5,12,21];
- Type of pharyngeal reconstruction—augmentation pharyngoplasty with a free radial forearm flap led to lower PCF rates [1], and a free jejunal flap for circumferential pharyngeal defects had lower rates of PCF [2];
- Salivary bypass tube usage following TL led to lower rates of PCF [4];
- The horizontal method of pharyngeal closure following TL led to lower rates of PCF [6].
- Organ preservation protocols led to higher rates of PCF [16];
- Primary and secondary TEP—no difference was found in the rates of PCF between primary and secondary TEP insertion [15];
- Non-surgical treatment had promising outcomes in PCF, but the sample size was too small [11] (Table 1).
3.8. Citation Network
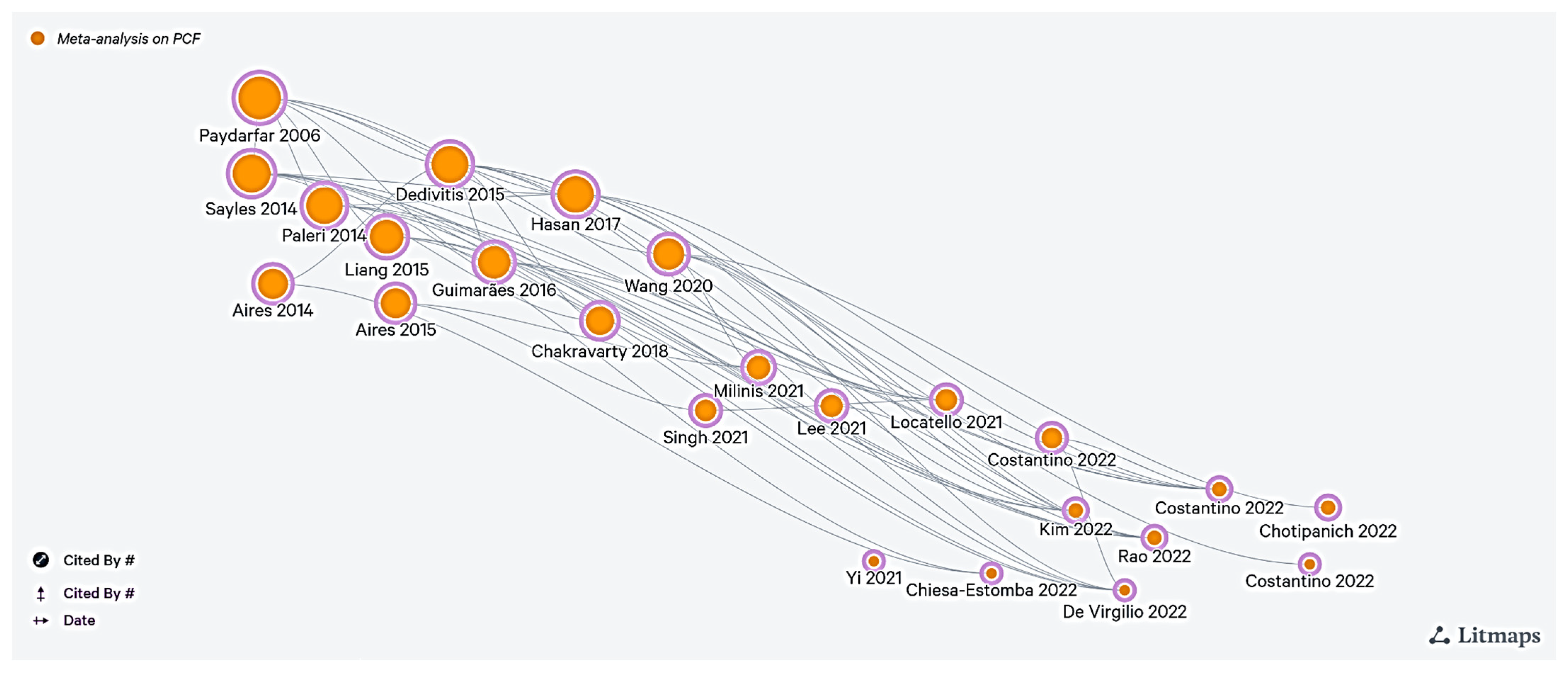
The citation network of the included articles was generated using the Litmaps tool [25]. The independent axes on the literature citation maps are the logarithmic scale of citations and distributed over the publication date. The size of the individual article bubble corresponds to the logarithmic scale of the article citation (Figure 3).
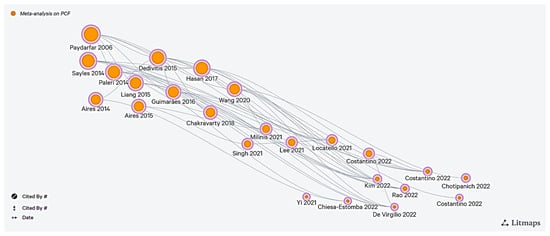
Figure 3.
Citation network [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24].
4. Discussion
There have been numerous meta-analyses conducted on pharyngocutaneous fistula (PCF) following total laryngectomy (TL), with the majority (over 50%) being published in the last 18 months. Although the topic is intriguing, there is considerable overlap in the research questions of many meta-analyses. Therefore, a bibliometric analysis was performed on PCF meta-analyses to identify the study objectives and outcomes to determine gaps in the literature and provide a guide map for further research. Here, we discuss the lacunae in the meta-analysis and the literature on PCF following TL.
Of the published meta-analyses (n = 24), six (25%) aimed to determine the risk factors for PCF in TL, but only one described the risk factors specifically for primary TL. None of the studies have determined the risk factors for salvage TL exclusively, with the remaining five analyses concentrating on TL. With the increasing use of organ preservation protocols as the initial therapy for laryngeal cancer, the rates of salvage TL are increasing, making it imperative to close this gap.
Many of the risk factors assessed in the meta-analyses had significant overlap. For example, the timing of salvage surgery after completing the organ preservation protocol needs to be considered, with at least an 8 to 12 week gap following radiation therapy to imaging, to determine if the suspected recurrence is due to post-radiotherapy change or truly due to residual disease [26]. Local tissue hypoxia following irradiation due to an increase in hypoxia-inducible factor 1-alpha (HIF-1α) can lead to impaired wound healing and ultimately to PCF [27]. The condition of the overlying skin is also a crucial factor, especially during salvage surgery, as there is an increase in wound dehiscence rates in STL, mainly due to tissue hypoxia, endarteritis, and endothelial dysfunction [28]. The use of electrocautery and cold instruments for ablating the pharyngeal mucosal margins may play a role, as there is the possibility of lateral thermal damage to the surrounding mucosa (up to 2–3 mm) with electrocautery and no injury with cold instruments (blade or scissors) [29]. Various techniques of pharyngeal mucosal closure have been described, simple continuous interlocking sutures interrupted by sutures with extraluminal or intraluminal knots, as described by Connell [30], Lembert [31], and Gambee [32], but these methods have not been compared mainly due to a lack of studies. The depth of cricopharyngeal myotomy is to be noted, as the deep myotomy may lead to thin pharyngeal mucosa at the point of myotomy, which may lead to higher chances of PCF.
Other factors that may contribute to the development of PCF include the extent of laryngectomy (total vs. partial), type of antibiotic used, the duration of surgery, tissue handling methods, the number of layers of closure, the surgeon’s experience, the type of suture used, the duration of the closed suction drain, and the use of compression dressing. However, there is a paucity of literature analyzing these factors, with only a few isolated case series reported. Thus, a high-quality study examining these factors individually is needed. The confounding variables make it difficult to perform a randomized trial for every scenario. To reach a good statistical power of the study, the sample size of the study must be relatively large. A good sample size can be achieved with multi-institutional and multinational collaborations [33]. The collaborations will also help us to identify these factors across various populations.
The published meta-analyses have severe heterogeneity, a lack of randomized trials, and confounding factors. Many meta-analyses are repetitions of similar research questions, which can be avoided by preregistering the meta-analyses and performing a thorough literature search to avoid duplication. Bias in surgical research must also be noted, particularly in articles describing a surgical technique [34]. Congruences in the results of multiple studies will strengthen the hypothesis and lead to a better understanding of the risk factors for PCF in TL.
The summary of lacunae and the methods to circumvent them has been provided in Table 2.

Table 2.
Summary of lacunae.
5. Conclusions
In conclusion, the literature on pharyngocutaneous fistula (PCF) following total laryngectomy (TL) has many meta-analyses with overlapping research questions. Despite the abundance of published analysis, there is a lack of scrutiny on certain critical aspects of PCF in TL. These aspects include the risk factors for PCF in salvage TL, the optimal timing of salvage surgery following radiation, and various surgical techniques for pharyngeal mucosal closure. It is essential to perform high-quality studies with good statistical power to close these gaps in the literature and generate new evidence that can guide clinical practice in preventing PCF in TL.
Author Contributions
Conceptualization—K.N.R., R.A. and N.M.N.; data collection—K.N.R., A.S., P.D. and R.A.; data synthesis—K.N.R., A.S. and P.D.; data analysis and interpretation—K.N.R., A.S. and P.D.; drafting the article—all authors; critical revision of the article—all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable, as this is a bibliometric study of published meta-analyses.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Costantino, A.; Festa, B.M.; Kim, S.H.; Baik, F.M.; Wang, C.C.; Pirola, F.; Malvezzi, L.; Spriano, G.; Mercante, G.; De Virgilio, A. Complications of pectoralis major myo-cutaneous flap, anterolateral thigh flap and radial forearm free flap after total laryngectomy with partial pharyngectomy: A systematic review and network meta-analysis. Microsurgery 2023, 43, 286–296. [Google Scholar] [CrossRef] [PubMed]
- Costantino, A.; Festa, B.M.; Ferreli, F.; Russo, E.; Malvezzi, L.; Giannitto, C.; Spriano, G.; Mercante, G.; De Virgilio, A. Circumferential pharyngeal reconstruction after total laryngopharyngectomy: A systematic review and network meta-analysis. Oral Oncol. 2022, 127, 105809. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Kim, S.W.; Hwang, S.H. Predictive Value of Risk Factors for Pharyngocutaneous Fistula After Total Laryngectomy. Laryngoscope 2023, 133, 742–754. [Google Scholar] [CrossRef] [PubMed]
- Costantino, A.; Pace, G.M.; Festa, B.M.; Ferreli, F.; Malvezzi, L.; Spriano, G.; Mercante, G.; De Virgilio, A. Salivary bypass tube in total laryngectomy: Systematic review and meta-analysis. Head Neck 2022, 44, 2608–2620. [Google Scholar] [CrossRef]
- Chiesa-Estomba, C.M.; Mayo-Yanez, M.; Palacios-García, J.M.; Lechien, J.R.; Viljoen, G.; Karkos, P.D.; Barillari, M.R.; González-García, J.A.; Sistiaga-Suarez, J.A.; González-Botas, J.H.; et al. Stapler-Assisted Pharyngeal Closure After Total Laryngectomy: A Systematic Review and Meta-Analysis. Oncol. Ther. 2022, 10, 241–252. [Google Scholar] [CrossRef]
- Chotipanich, A.; Wongmanee, S. Incidence of Pharyngocutaneous Fistula After Total Laryngectomy and Its Relationship With the Shapes of Mucosa Closure: A Meta-Analysis. Cureus 2022, 14, e28822. [Google Scholar] [CrossRef]
- Rao, K.N.; Arora, R.D.; Singh, A.; Nagarkar, N.M.; Aggarwal, A. Pharyngocutaneous Fistula Following Primary Total Laryngectomy: A Meta-analysis. Indian J. Surg. Oncol. 2022, 13, 797–808. [Google Scholar] [CrossRef]
- De Virgilio, A.; Costantino, A.; Festa, B.M.; Russo, E.; Malvezzi, L.; Pellini, R.; Colombo, G.; Spriano, G.; Mercante, G.; Ferreli, F. Surgical prevention of pharyngocutaneous fistula in salvage total laryngectomy: A systematic review and network meta-analysis. Eur. Arch. Oto-Rhino-Laryngol. 2022, 279, 5839–5849. [Google Scholar] [CrossRef]
- Singh, R.; Karantanis, W.; Fadhil, M.; Dow, C.; Fuzi, J.; Robinson, R.; Jacobson, I. Meta-analysis on the rate of pharyngocutaneous fistula in early oral feeding in laryngectomy patients. Am. J. Otolaryngol. 2021, 42, 102748. [Google Scholar] [CrossRef]
- Yi, X.; Hu, C.; Peng, Y.; Wen, Z.; Li, X.; Ye, L.; Huang, Q. Meta-analysis on the safety and efficacy of early oral feeding after total laryngectomy. J. BUON Off. J. Balk. Union. Oncol. 2021, 26, 2019–2025. [Google Scholar]
- Locatello, L.G.; Licci, G.; Maggiore, G.; Gallo, O. Non-Surgical Strategies for Assisting Closure of Pharyngocutaneous Fistula after Total Laryngectomy: A Systematic Review of the Literature. J. Clin. Med. 2021, 11, 100. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.C.; Fang, T.J.; Kuo, I.C.; Tsai, Y.T.; Hsin, L.J. Stapler closure versus manual closure in total laryngectomy for laryngeal cancer: A systematic review and meta-analysis. Clin. Otolaryngol. 2021, 46, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Milinis, K.; Gaskell, P.; Lau, A.; Lancaster, J.; Jones, T. Early versus late oral feeding following total (pharyngo)laryngectomy: Systematic review and meta-analysis. Head Neck 2021, 43, 1359–1368. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Xun, Y.; Wang, K.; Lu, L.; Yu, A.; Guan, B.; Yu, C. Risk factors of pharyngocutaneous fistula after total laryngectomy: A systematic review and meta-analysis. Eur. Arch. Oto-Rhino-Laryngol. 2020, 277, 585–599. [Google Scholar] [CrossRef] [PubMed]
- Chakravarty, P.D.; McMurran, A.E.L.; Banigo, A.; Shakeel, M.; Ah-See, K.W. Primary versus secondary tracheoesophageal puncture: Systematic review and meta-analysis. J. Laryngol. Otol. 2018, 132, 14–21. [Google Scholar] [CrossRef]
- Hasan, Z.; Dwivedi, R.C.; Gunaratne, D.A.; Virk, S.A.; Palme, C.E.; Riffat, F. Systematic review and meta-analysis of the complications of salvage total laryngectomy. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2017, 43, 42–51. [Google Scholar] [CrossRef]
- Guimarães, A.V.; Aires, F.T.; Dedivitis, R.A.; Kulcsar, M.A.V.; Ramos, D.M.; Cernea, C.R.; Brandão, L.G. Efficacy of pectoralis major muscle flap for pharyngocutaneous fistula prevention in salvage total laryngectomy: A systematic review. Head Neck 2016, 38 (Suppl. S1), E2317–E2321. [Google Scholar] [CrossRef]
- Aires, F.T.; Dedivitis, R.A.; Petrarolha, S.M.P.; Bernardo, W.M.; Cernea, C.R.; Brandão, L.G. Early oral feeding after total laryngectomy: A systematic review. Head Neck 2015, 37, 1532–1535. [Google Scholar] [CrossRef]
- Dedivitis, R.A.; Aires, F.T.; Cernea, C.R.; Brandão, L.G. Pharyngocutaneous fistula after total laryngectomy: Systematic review of risk factors. Head Neck 2015, 37, 1691–1697. [Google Scholar] [CrossRef]
- Liang, J.W.; Li, Z.D.; Li, S.C.; Fang, F.Q.; Zhao, Y.J.; Li, Y.G. Pharyngocutaneous fistula after total laryngectomy: A systematic review and meta-analysis of risk factors. Auris Nasus Larynx 2015, 42, 353–359. [Google Scholar] [CrossRef]
- Aires, F.T.; Dedivitis, R.A.; Castro, M.A.F.; Bernardo, W.M.; Cernea, C.R.; Brandão, L.G. Efficacy of stapler pharyngeal closure after total laryngectomy: A systematic review. Head Neck 2014, 36, 739–742. [Google Scholar] [CrossRef] [PubMed]
- Sayles, M.; Grant, D.G. Preventing pharyngo-cutaneous fistula in total laryngectomy: A systematic review and meta-analysis. Laryngoscope 2014, 124, 1150–1163. [Google Scholar] [CrossRef] [PubMed]
- Paleri, V.; Drinnan, M.; van den Brekel, M.W.M.; Hinni, M.L.; Bradley, P.J.; Wolf, G.T.; De Bree, R.; Fagan, J.J.; Hamoir, M.; Strojan, P.; et al. Vascularized tissue to reduce fistula following salvage total laryngectomy: A systematic review. Laryngoscope 2014, 124, 1848–1853. [Google Scholar] [CrossRef]
- Paydarfar, J.A.; Birkmeyer, N.J. Complications in head and neck surgery: A meta-analysis of postlaryngectomy pharyngocutaneous fistula. Arch. Otolaryngol. Head Neck Surg. 2006, 132, 67–72. [Google Scholar] [CrossRef]
- Litmaps [Internet]. Litmaps. Available online: https://app.litmaps.com (accessed on 7 May 2023).
- Ljumanovic, R.; Langendijk, J.A.; Hoekstra, O.S.; Knol, D.L.; Leemans, C.R.; Castelijns, J.A. Pre- and post-radiotherapy MRI results as a predictive model for response in laryngeal carcinoma. Eur. Radiol. 2008, 18, 2231–2240. [Google Scholar] [CrossRef][Green Version]
- Nauta, T.D.; van Hinsbergh, V.W.M.; Koolwijk, P. Hypoxic Signaling During Tissue Repair and Regenerative Medicine. Int. J. Mol. Sci. 2014, 15, 19791–19815. [Google Scholar] [CrossRef] [PubMed]
- Sheaff, M.; Baithun, S. Pathological effects of ionizing radiation. Curr. Diagn. Pathol. 1997, 4, 106–115. [Google Scholar] [CrossRef]
- Hefermehl, L.J.; Largo, R.A.; Hermanns, T.; Poyet, C.; Sulser, T.; Eberli, D. Lateral temperature spread of monopolar, bipolar and ultrasonic instruments for robot-assisted laparoscopic surgery. BJU Int. 2014, 114, 245–252. [Google Scholar] [CrossRef]
- Haksever, M.; Akduman, D.; Aslan, S.; Solmaz, F.; Ozmen, S. Modified Continuous Mucosal Connell Suture for the Pharyngeal Closure After Total Laryngectomy: Zipper Suture. Clin. Exp. Otorhinolaryngol. 2015, 8, 281–288. [Google Scholar] [CrossRef]
- Feng, F.; Sun, L.; Xu, G.; Hong, L.; Yang, J.; Cai, L.; Li, G.; Guo, M.; Lian, X.; Zhang, H. Albert-Lembert versus hybrid-layered suture in hand sewn end-to-end cervical esophagogastric anastomosis after esophageal squamous cell carcinoma resection. J. Thorac. Dis. 2015, 7, 1917–1926. [Google Scholar]
- Lafreniere, R.; Ketcham, A.S. A single layer open anastomosis for all intestinal structures. Am. J. Surg. 1985, 149, 797–798. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (US) Council on Health Care Technology; Sox, H.; Stern, S.; Owens, D.; Abrams, H.L. Problems of Multi-Institutional Studies. In Assessment of Diagnostic Technology in Health Care: Rationale, Methods, Problems, and Directions: Monograph of the Council on Health Care Technology [Internet]; National Academies Press (US): Washington, DC, USA, 1989. Available online: https://www.ncbi.nlm.nih.gov/books/NBK235189/ (accessed on 1 May 2023).
- Paradis, C. Bias in surgical research. Ann. Surg. 2008, 248, 180–188. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).