Risk Factors Contributing to Reinfection by SARS-CoV-2: A Systematic Review
Abstract
:Highlights
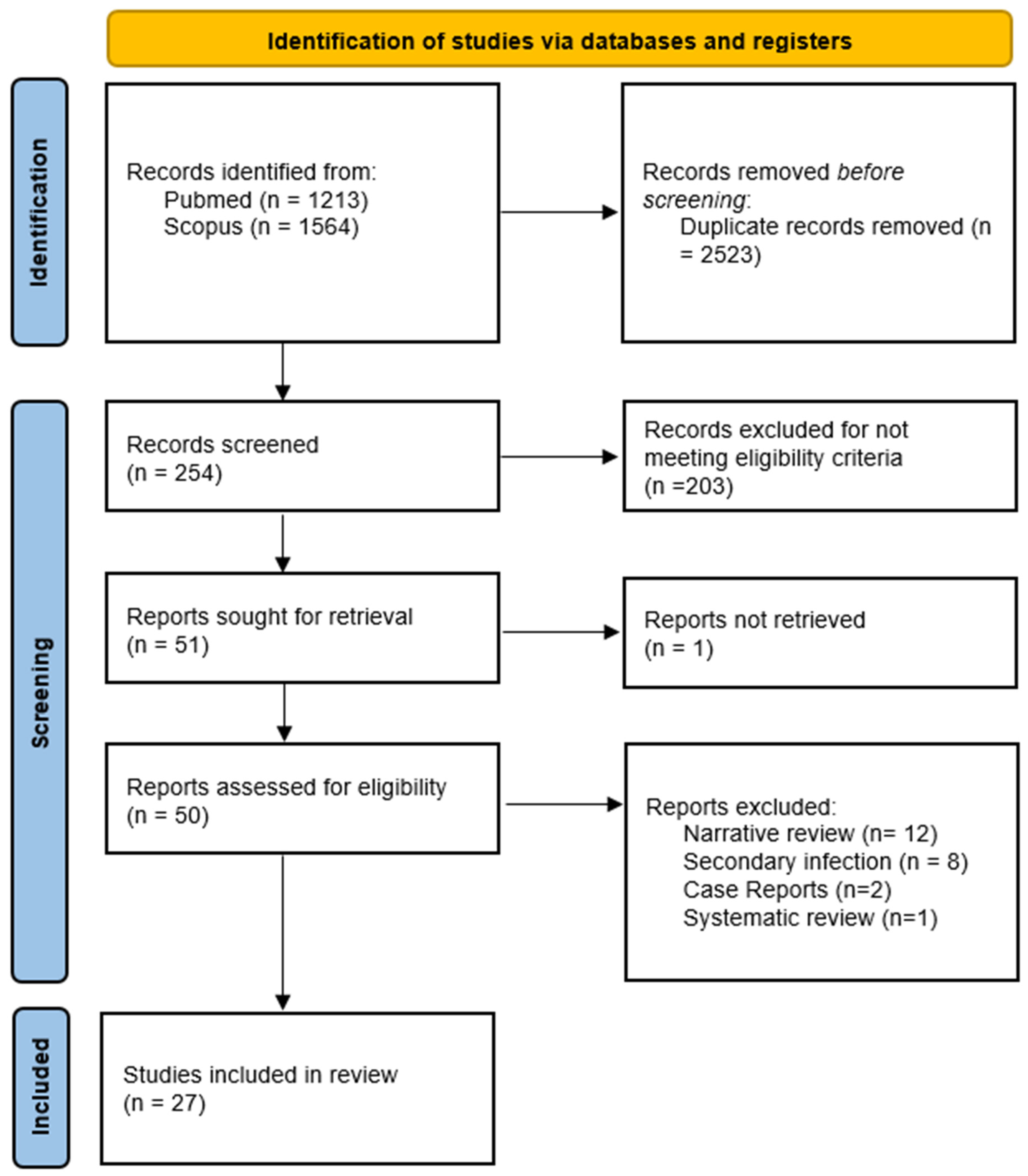
- This comprehensive analysis meticulously examined 51 studies, pinpointing 27 that rigorously adhered to stringent criteria. The incorporation of diverse studies afforded a panoramic perspective on COVID-19 reinfection.
- Emphasis was placed on the effectiveness of vaccination, showcasing a remarkable risk reduction of up to 66% with the administration of two vaccine doses.
- In spite of an overall low reinfection rate, the findings unveiled noteworthy patterns. Factors such as non-vaccination, advanced age, and the presence of comorbidities emerged as significant contributors to the likelihood of reinfection.
- While the review furnished valuable insights, it underscored the persistent necessity for more nuanced observational studies. Special attention was urged, particularly regarding emerging variants and the duration of immunity post-infection or post-vaccination.
Abstract
1. Background
2. Methodology
2.1. Bibliographic Search Strategy
2.2. Eligibility Criteria
2.3. Selection of Studies and Data Extraction
2.4. Summary of Results
2.5. Synthesis of Results
2.6. Study Quality Assessment
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gaudreault, N.N.; Carossino, M.; Morozov, I.; Trujillo, J.D.; Meekins, D.A.; Madden, D.W.; Cool, K.; Artiaga, B.L.; McDowell, C.; Bold, D.; et al. Experimental Re-Infected Cats Do Not Transmit SARS-CoV-2. Emerg. Microbes Infect. 2021, 10, 638–650. [Google Scholar] [CrossRef]
- Rahman, S.; Rahman, M.M.; Miah, M.; Begum, M.N.; Sarmin, M.; Mahfuz, M.; Hossain, M.E.; Rahman, M.Z.; Chisti, M.J.; Ahmed, T.; et al. COVID-19 Reinfections among Naturally Infected and Vaccinated Individuals. Sci. Rep. 2022, 12, 1438. [Google Scholar] [CrossRef]
- Almadhi, M.; Alsayyad, A.S.; Conroy, R.; Atkin, S.; Awadhi, A.A.; Al-Tawfiq, J.A.; AlQahtani, M. Epidemiological Assessment of SARS-CoV-2 Reinfection. Int. J. Infect. Dis. 2022, 123, 9–16. [Google Scholar] [CrossRef]
- Pecho-Silva, S.; Navarro-Solsol, A.C.; Panduro-Correa, V.; Rodriguez-Morales, A.J. COVID-19 Reinfection in a Bolivian Patient. Report of the First Possible Case. Microbes Infect. Chemother. 2021, 1, e1171. [Google Scholar] [CrossRef]
- Arteaga-Livias, K.; Panduro-Correa, V.; Pinzas-Acosta, K.; Perez-Abad, L.; Pecho-Silva, S.; Espinoza-Sánchez, F.; Dámaso-Mata, B.; Rodriguez-Morales, A.J. COVID-19 Reinfection? A Suspected Case in a Peruvian Patient. Travel. Med. Infect. Dis. 2021, 39, 101947. [Google Scholar] [CrossRef]
- West, J.; Everden, S.; Nikitas, N. A Case of COVID-19 Reinfection in the UK. Clin. Med. 2021, 21, e52–e53. [Google Scholar] [CrossRef]
- Pujadas, E.; Chaudhry, F.; McBride, R.; Richter, F.; Zhao, S.; Wajnberg, A.; Nadkarni, G.; Glicksberg, B.S.; Houldsworth, J.; Cordon-Cardo, C. SARS-CoV-2 Viral Load Predicts COVID-19 Mortality. Lancet Respir. Med. 2020, 8, e70. [Google Scholar] [CrossRef]
- Sotoodeh Ghorbani, S.; Taherpour, N.; Bayat, S.; Ghajari, H.; Mohseni, P.; Hashemi Nazari, S.S. Epidemiologic Characteristics of Cases with Reinfection, Recurrence, and Hospital Readmission Due to COVID-19: A Systematic Review and Meta-Analysis. J. Med. Virol. 2022, 94, 44–53. [Google Scholar] [CrossRef]
- To, K.K.-W.; Hung, I.F.-N.; Ip, J.D.; Chu, A.W.-H.; Chan, W.-M.; Tam, A.R.; Fong, C.H.-Y.; Yuan, S.; Tsoi, H.-W.; Ng, A.C.-K.; et al. Coronavirus Disease 2019 (COVID-19) Re-Infection by a Phylogenetically Distinct Severe Acute Respiratory Syndrome Coronavirus 2 Strain Confirmed by Whole Genome Sequencing. Clin. Infect. Dis. 2021, 73, e2946–e2951. [Google Scholar] [CrossRef]
- Santos, V.M.; dos Santos, L.A.M.; dos Modesto, L.C.; Modesto, J.C. Reinfection with SARS-CoV-2: A Challenging Event. Microbes Infect. Chemother. 2021, 1, e1189. [Google Scholar] [CrossRef]
- Ren, X.; Zhou, J.; Guo, J.; Hao, C.; Zheng, M.; Zhang, R.; Huang, Q.; Yao, X.; Li, R.; Jin, Y. Reinfection in Patients with COVID-19: A Systematic Review. Glob. Health Res. Policy 2022, 7, 12. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Reinfection with SARS-CoV: Considerations for Public Health Response; ECDC: Solna, Sweden, 2020. [Google Scholar]
- Lind, M.L.; Dorion, M.; Houde, A.J.; Lansing, M.; Lapidus, S.; Thomas, R.; Yildirim, I.; Omer, S.B.; Schulz, W.L.; Andrews, J.R.; et al. Evidence of Leaky Protection Following COVID-19 Vaccination and SARS-CoV-2 Infection in an Incarcerated Population. Nat. Commun. 2023, 14, 5055. [Google Scholar] [CrossRef] [PubMed]
- Roberts, T.; Keddie, S.H.; Rattanavong, S.; Gomez, S.R.; Bradley, J.; Keogh, R.H.; Bärenbold, O.; Falconer, J.; Mens, P.F.; Hopkins, H.; et al. Accuracy of the Direct Agglutination Test for Diagnosis of Visceral Leishmaniasis: A Systematic Review and Meta-Analysis. BMC Infect. Dis. 2023, 23, 782. [Google Scholar] [CrossRef] [PubMed]
- Arafkas, M.; Khosrawipour, T.; Kocbach, P.; Zielinski, K.; Schubert, J.; Mikolajczyk, A.; Celinska, M.; Khosrawipour, V. Current Meta-Analysis Does Not Support the Possibility of COVID-19 Reinfections. J. Med. Virol. 2021, 93, 1599–1604. [Google Scholar] [CrossRef]
- Tillett, R.L.; Sevinsky, J.R.; Hartley, P.D.; Kerwin, H.; Crawford, N.; Gorzalski, A.; Laverdure, C.; Verma, S.C.; Rossetto, C.C.; Jackson, D.; et al. Genomic Evidence for Reinfection with SARS-CoV-2: A Case Study. Lancet Infect. Dis. 2021, 21, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Cooper, L.A. COVID-19 and Health Equity-A New Kind of “Herd Immunity”. JAMA 2020, 323, 2478–2480. [Google Scholar] [CrossRef]
- Plans-Rubió, P. Percentages of Vaccination Coverage Required to Establish Herd Immunity against SARS-CoV-2. Vaccines 2022, 10, 736. [Google Scholar] [CrossRef]
- Al-Hatamleh, M.A.I.; Abusalah, M.A.; Hatmal, M.M.; Alshaer, W.; Ahmad, S.; Mohd-Zahid, M.H.; Rahman, E.N.S.E.A.; Yean, C.Y.; Alias, I.Z.; Uskoković, V.; et al. Understanding the Challenges to COVID-19 Vaccines and Treatment Options, Herd Immunity and Probability of Reinfection. J. Taibah Univ. Med. Sci. 2022, 18, 600–638. [Google Scholar] [CrossRef] [PubMed]
- SeyedAlinaghi, S.; Afsahi, A.M.; MohsseniPour, M.; Behnezhad, F.; Salehi, M.A.; Barzegary, A.; Mirzapour, P.; Mehraeen, E.; Dadras, O. Late Complications of COVID-19; a Systematic Review of Current Evidence. Arch. Acad. Emerg. Med. 2021, 9, e14. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Rev. Esp. Cardiol. 2021, 74, 790–799. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Qureshi, R.; Mattis, P.; Lisy, K.; et al. Chapter 7: Systematic Reviews of Etiology and Risk. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020; Available online: https://Synthesismanual.Jbi.Global (accessed on 3 December 2023).
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; NOS: Oxford, UK, 2000. [Google Scholar]
- Sacco, C.; Petrone, D.; Del Manso, M.; Mateo-Urdiales, A.; Fabiani, M.; Bressi, M.; Bella, A.; Pezzotti, P.; Rota, M.C.; Riccardo, F.; et al. Risk and Protective Factors for SARS-CoV-2 Reinfections, Surveillance Data, Italy, August 2021 to March 2022. Euro Surveill. 2022, 27, 2200372. [Google Scholar] [CrossRef]
- Flacco, M.E.; Soldato, G.; Acuti Martellucci, C.; Di Martino, G.; Carota, R.; Caponetti, A.; Manzoli, L. Risk of SARS-CoV-2 Reinfection 18 Months After Primary Infection: Population-Level Observational Study. Front. Public Health 2022, 10, 884121. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, N.A.; Sambas, R.; Alenezi, M.; Alharbi, N.K.; Aldibasi, O.; Bosaeed, M. COVID-19 Reinfection: A Multicenter Retrospective Study in Saudi Arabia. Ann. Thorac. Med. 2022, 17, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Nordström, P.; Ballin, M.; Nordström, A. Risk of SARS-CoV-2 Reinfection and COVID-19 Hospitalisation in Individuals with Natural and Hybrid Immunity: A Retrospective, Total Population Cohort Study in Sweden. Lancet Infect. Dis. 2022, 22, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Slezak, J.; Bruxvoort, K.; Fischer, H.; Broder, B.; Ackerson, B.; Tartof, S. Rate and Severity of Suspected SARS-CoV-2 Reinfection in a Cohort of PCR-Positive COVID-19 Patients. Clin. Microbiol. Infect. 2021, 27, 1860.e7–1860.e10. [Google Scholar] [CrossRef] [PubMed]
- Mensah, A.A.; Lacy, J.; Stowe, J.; Seghezzo, G.; Sachdeva, R.; Simmons, R.; Bukasa, A.; O’Boyle, S.; Andrews, N.; Ramsay, M.; et al. Disease Severity during SARS-CoV-2 Reinfection: A Nationwide Study. J. Infect. 2022, 84, 542–550. [Google Scholar] [CrossRef]
- Yao, M.-Q.; Zheng, Q.-X.; Xu, J.; Deng, J.-W.; Ge, T.-T.; Zhou, H.-B.; Wu, F.-T.; Gu, X.-Y.; Yang, Q.; Ren, Y.-L.; et al. Factors Associated with a SARS-CoV-2 Recurrence after Hospital Discharge among Patients with COVID-19: Systematic Review and Meta-Analysis. J. Zhejiang Univ. Sci. B 2020, 21, 940–947. [Google Scholar] [CrossRef]
- Pulliam, J.R.C.; van Schalkwyk, C.; Govender, N.; von Gottberg, A.; Cohen, C.; Groome, M.J.; Dushoff, J.; Mlisana, K.; Moultrie, H. Increased Risk of SARS-CoV-2 Reinfection Associated with Emergence of Omicron in South Africa. Science 2022, 376, eabn4947. [Google Scholar] [CrossRef] [PubMed]
- Al-Otaiby, M.; Krissaane, I.; Al Seraihi, A.; Alshenaifi, J.; Qahtani, M.H.; Aljeri, T.; Zaatari, E.; Hassanain, M.; Algwizani, A.; Albarrag, A.; et al. SARS-CoV-2 Reinfection Rate and Outcomes in Saudi Arabia: A National Retrospective Study. Int. J. Infect. Dis. 2022, 122, 758–766. [Google Scholar] [CrossRef]
- Murillo-Zamora, E.; Mendoza-Cano, O.; Delgado-Enciso, I.; Hernandez-Suarez, C.M. Predictors of Severe Symptomatic Laboratory-Confirmed SARS-CoV-2 Reinfection. Public Health 2021, 193, 113–115. [Google Scholar] [CrossRef]
- Garduño-Orbe, B.; Sánchez-Rebolledo, J.M.; Cortés-Rafael, M.; García-Jiménez, Y.; Perez-Ortiz, M.; Mendiola-Pastrana, I.R.; López-Ortiz, E.; López-Ortiz, G. SARS-CoV-2 Reinfection among Healthcare Workers in Mexico: Case Report and Literature Review. Medicina 2021, 57, 442. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Varela, N.; Cinza-Sanjurjo, S.; Portela-Romero, M. Reinfection by the Omicron variant in patients previously infected with the Delta variant of the SARS-CoV-2 coronavirus: An increasingly frequent reality in Primary Care. Semergen 2022, 48, e35–e36. [Google Scholar] [CrossRef]
- Hu, R.; Jiang, Z.; Gao, H.; Huang, D.; Jiang, D.; Chen, F.; Li, J. Recurrent Positive Reverse Transcriptase-Polymerase Chain Reaction Results for Coronavirus Disease 2019 in Patients Discharged from a Hospital in China. JAMA Netw. Open 2020, 3, e2010475. [Google Scholar] [CrossRef] [PubMed]
- Quattrocchi, A.; Tsioutis, C.; Demetriou, A.; Kyprianou, T.; Athanasiadou, M.; Silvestros, V.; Mamais, I.; Demetriou, C.A.; Theophanous, F.; Soteriou, S.; et al. Effect of Vaccination on SARS-CoV-2 Reinfection Risk: A Case-Control Study in the Republic of Cyprus. Public Health 2022, 204, 84–86. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, A.M.; Spicer, K.B.; Thoroughman, D.; Glick, C.; Winter, K. Reduced Risk of Reinfection with SARS-CoV-2 After COVID-19 Vaccination—Kentucky, May-June 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1081–1083. [Google Scholar] [CrossRef]
- Medić, S.; Anastassopoulou, C.; Lozanov-Crvenković, Z.; Vuković, V.; Dragnić, N.; Petrović, V.; Ristić, M.; Pustahija, T.; Gojković, Z.; Tsakris, A.; et al. Risk and Severity of SARS-CoV-2 Reinfections during 2020-2022 in Vojvodina, Serbia: A Population-Level Observational Study. Lancet Reg. Health Eur. 2022, 20, 100453. [Google Scholar] [CrossRef]
- Pilz, S.; Chakeri, A.; Ioannidis, J.P.; Richter, L.; Theiler-Schwetz, V.; Trummer, C.; Krause, R.; Allerberger, F. SARS-CoV-2 Re-Infection Risk in Austria. Eur. J. Clin. Investig. 2021, 51, e13520. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, L.A.; de Góis Filho, P.G.; Silva, A.M.F.; Santos, J.V.G.; Santos, D.S.; Aquino, M.M.; de Jesus, R.M.; Almeida, M.L.D.; da Silva, J.S.; Altmann, D.M.; et al. Recurrent COVID-19 Including Evidence of Reinfection and Enhanced Severity in Thirty Brazilian Healthcare Workers. J. Infect. 2021, 82, 399–406. [Google Scholar] [CrossRef]
- Havervall, S.; Ng, H.; Jernbom Falk, A.; Greilert-Norin, N.; Månberg, A.; Marking, U.; Laurén, I.; Gabrielsson, L.; Salomonsson, A.-C.; Aguilera, K.; et al. Robust Humoral and Cellular Immune Responses and Low Risk for Reinfection at Least 8 Months Following Asymptomatic to Mild COVID-19. J. Intern. Med. 2022, 291, 72–80. [Google Scholar] [CrossRef]
- Nisha, B.; Dakshinamoorthy, K.; Padmanaban, P.; Jain, T.; Neelavarnan, M. Infection, Reinfection, and Postvaccination Incidence of SARS-CoV-2 and Associated Risks in Healthcare Workers in Tamil Nadu: A Retrospective Cohort Study. J. Fam. Community Med. 2022, 29, 49–55. [Google Scholar] [CrossRef]
- Levin-Rector, A.; Firestein, L.; McGibbon, E.; Sell, J.; Lim, S.; Lee, E.H.; Weiss, D.; Geevarughese, A.; Zucker, J.R.; Greene, S.K. Reduced Odds of Severe Acute Respiratory Syndrome Coronavirus 2 Reinfection After Vaccination Among New York City Adults, July 2021-November 2021. Clin. Infect. Dis. 2023, 76, e469–e476. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.N.; Houhamdi, L.; Hoang, V.T.; Delerce, J.; Delorme, L.; Colson, P.; Brouqui, P.; Fournier, P.-E.; Raoult, D.; Gautret, P. SARS-CoV-2 Reinfection and COVID-19 Severity. Emerg. Microbes Infect. 2022, 11, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Mensah, A.A.; Campbell, H.; Stowe, J.; Seghezzo, G.; Simmons, R.; Lacy, J.; Bukasa, A.; O’Boyle, S.; Ramsay, M.E.; Brown, K.; et al. Risk of SARS-CoV-2 Reinfections in Children: A Prospective National Surveillance Study between January, 2020, and July, 2021, in England. Lancet Child Adolesc. Health 2022, 6, 384–392. [Google Scholar] [CrossRef] [PubMed]
- Ochoa-Hein, E.; Leal-Morán, P.E.; Nava-Guzmán, K.A.; Vargas-Fernández, A.T.; Vargas-Fernández, J.F.; Díaz-Rodríguez, F.; Rayas-Bernal, J.A.; González-González, R.; Vázquez-González, P.; Huertas-Jiménez, M.A.; et al. Significant Rise in SARS-CoV-2 Reinfection Rate in Vaccinated Hospital Workers during the Omicron Wave: A Prospective Cohort Study. Rev. Investig. Clin. 2022, 74, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Jang, E.J.; Choe, Y.J.; Yun, G.-W.; Wang, S.; Cho, U.J.; Yi, S.; Lee, S.; Park, Y.-J. Reinfection with SARS-CoV-2 in General Population, South Korea; Nationwide Retrospective Cohort Study. J. Med. Virol. 2022, 94, 5589–5592. [Google Scholar] [CrossRef] [PubMed]
| No. | Country | Publication Date | Author | Title | Findings |
|---|---|---|---|---|---|
| 1 | Italy | May 2022 | Sacco et al. [24] | Risk and protection factors for SARS-CoV-2 reinfections | Not being vaccinated emerges as the most significant risk factor. The risk of infection escalates 18 times more with the Omicron variant. Individuals who have experienced a severe initial infection and are over 60 years of age face heightened risks. |
| 2 | Italy | May 2022 | Flacco et al. [25] | Risk of SARS-CoV-2 reinfection 18 months after primary infection: a population-based observational study | Risk is significantly higher in women, young people, and people who have not been vaccinated. |
| 3 | Saudi Arabia | April 2022 | Shaheen et al. [26] | COVID-19 reinfection: a multicenter retrospective study in Saudi Arabia | Among the 35,288 analyzed patients, 0.37% experienced reinfection. The mean age of the participants was 40.95 ± 19.48 years, and 50.76% were female. |
| 4 | Sweden | April 2022 | Nordström et al. [27] | Risk of SARS-CoV-2 reinfection and hospitalization from COVID-19 in people with natural and hybrid immunity: a retrospective total population cohort study in Sweden | Two doses of the SARS-CoV-2 vaccine were associated with a 66% lower risk of reinfection. |
| 5 | USA | August 2021 | Slezak et al. [28] | Rate and severity of suspected reinfection by SARS-CoV-2 in a cohort of PCR-positive COVID-19 patients | Out of 75,149 cases, only 315 suspected reinfections were identified. Significant independent predictors of suspected reinfection included being a woman, an adult, being immunocompromised, and having previously been hospitalized for COVID-19. |
| 6 | England | April 2022 | Mensah et al. [29] | Illness severity during SARS-CoV-2 reinfection: a nationwide study | The female sex represented the highest proportion of reinfections (67%). Evidence suggested a rising increase in the risk of infection in individuals over 70 years of age. |
| 7 | China | December 2020 | Yao et al. [30] | Factors associated with a recurrence of SARS-CoV-2 after hospital discharge among patients with COVID-19: systematic review and meta-analysis | The primary factors associated with the recurrence of COVID-19 after hospital discharge included advanced age, severity of the previous infection, bilateral pulmonary infiltration, and decreases in leukocyte, platelet, and CD4+ T counts. |
| 8 | South Africa | March 2022 | Pulliam et al. [31] | Increased risk of reinfection by SARS-CoV-2 associated with the emergence of Omicron in South Africa | The relative risk of reinfection by COVID-19 increased with the third wave, marked by the emergence of the Omicron variant. |
| 9 | Bahrain (Middle East) | August 2022 | Almadhi et al. [3] | Epidemiological evaluation of reinfection by SARS-CoV-2 | The proportion of reinfected males was significantly higher at 60.3% (p < 0.0001), particularly within the 30–39 age group (29.7%). The lowest number of episodes occurred between 3 and 6 months after the first infection (20.6%), while the highest number of episodes occurred from the 9th month after the previous infection (46.4%). |
| 10 | Saudi Arabia | July 2022 | Al-Otaiby et al. [32] | SARS-CoV-2 reinfection rate and outcomes in Saudi Arabia: a national retrospective study | In the analysis of the risk factors, reinfection was highly associated with comorbidities, including HIV, obesity, and being healthcare personnel. |
| 11 | Mexico | April 2021 | Murillo-Zamora et al. [33] | Predictors of severe laboratory-confirmed symptomatic SARS-CoV-2 reinfection | Factors associated with an increased risk of severe symptomatic SARS-CoV-2 reinfection included a history of laboratory-confirmed severe coronavirus disease. |
| 12 | Mexico | May 2021 | Garduño-Orbe et al. [34] | SARS-CoV-2 reinfection in health workers in Mexico: Case report and review of the literature | Two out of the four cases of reinfection were severe, while in the remaining cases, the clinical manifestations resembled those of the previous infection. |
| 13 | Spain | January 2022 | Sánchez-Varela et al. [35] | Reinfection by the Omicron variant in patients previously performed with the Delta variant of the SARS-CoV-2 coronavirus: an increasingly frequent reality in primary care | Increased incidence due to the Omicron variant |
| 14 | China | May 2020 | Hu et al. [36] | Recurrent positive reverse transcriptase–polymerase chain reaction results for coronavirus disease 2019 in patients discharged from a hospital in China | There were no significant differences between the demographic and baseline clinical characteristics in the recurrence and non-recurrence groups. |
| 15 | Republic of Cyprus | March 2022 | Quattrocchi et al. [37] | Effect of vaccination on the risk of reinfection by SARS-CoV-2: a case-control study in the Republic of Cyprus | Their findings support the benefit of vaccination for individuals previously infected with SARS-CoV-2. |
| 16 | USA | August 2021 | Cavanaugh et al. [38] | Reduced risk of reinfection with SARS-CoV-2 after vaccination against COVID-19 in Kentucky, May–June 2021 | Those not vaccinated were from 2.3 to 4 times more likely to be reinfected compared to those who received all vaccinations (odds ratio (OR) = 2.34; 95% confidence interval (CI) = 1.58–3.47). In individuals with prior infection, full vaccination provided additional protection against reinfection. |
| 17 | Serbia | July 2022 | Medić et al. [39] | Risk and severity of SARS-CoV-2 reinfections during 2020–2022 in Vojvodina, Serbia: a population-level observational study | Those who were not vaccinated (OR = 1.23; 95% CI = 1.14–1.33), those with incomplete vaccination (OR = 1.33; 95% CI = 1.08–1.64), or fully vaccinated individuals (OR = 1.50; 95% CI = 1.37–1.63) were more likely to experience reinfection compared to patients who received the booster dose. |
| 18 | Austria | February 2021 | Pilz et al. [40] | Risk of SARS-CoV-2 reinfection in Austria | A relatively low risk of reinfection was documented. Patients with reinfections were of both sexes, spanning a wide age range, and were hospitalized during both infections. |
| 19 | Brazil | February 2021 | Adrielle Dos Santos et al. [41] | Recurrent COVID-19 including evidence of reinfection and increased severity in thirty Brazilian healthcare workers | Out of 33 patients with recurrent COVID-19, 26 were women, and 30 were healthcare workers. The median time to recurrence was 50.5 days. |
| 20 | Sweden | January 2020 | Havervall et al. [42] | Robust humoral and cellular immune responses and low risk of reinfection at least 8 months after asymptomatic or mild COVID-19 | The presence of IgG anti-spike antibodies is associated with a significantly reduced risk of reinfection for up to 9 months following asymptomatic or mild COVID-19. |
| 21 | India | January 2022 | Nisha et al. [43] | Incidence of SARS-CoV-2 infection, reinfection, and post-vaccination and associated risks in healthcare workers in Tamil Nadu: a retrospective cohort study | Men and primary care providers were at a higher risk of infection. Partial vaccination status was identified as one of the determinants of reinfection. |
| 22 | USA | May 2022 | Levin-Rector et al. [44] | Reduced odds of SARS-CoV-2 reinfection after vaccination among New York City adults, July–November 2021 | Vaccination decreased the likelihood of reinfections, particularly when the Delta variant predominated. |
| 23 | Several countries | August 2021 | Sotoodeh Ghorbani et al. [8] | Epidemiological characteristics of cases with reinfection, recurrence, and hospital readmission due to COVID-19: a systematic review and meta-analysis | The recurrence of reinfections was higher in women in comparison to men. Hospital readmission rates were similar for both sexes. There remains uncertainty regarding long-term immunity after SARS-CoV-2 infection. |
| 24 | France | March 2022 | Nguyen et al. [45] | SARS-CoV-2 reinfection and severity of COVID-19 | Reinfection represented 0.4% of the diagnosed positive cases. Among the 64 patients who underwent serological tests, 39 had antibodies when sampled early in their second infection. Only seven patients (3.4%) experienced infection twice with the same variant. |
| 25 | England | March 2022 | Mensah et al. [46] | Risk of SARS-CoV-2 reinfections in children: a prospective national surveillance study between January 2020 and July 2021 in England | Children were at a lower risk of reinfection compared to adults, and reinfections were not associated with more severe disease or fatal outcomes. |
| 26 | Mexico | June 2022 | Ochoa-Hein et al. [47] | Significant increase in SARS-CoV-2 reinfection rate in vaccinated hospital workers during the Omicron wave: a prospective cohort study | The SARS-CoV-2 reinfection rate increased significantly during the Omicron wave despite a high primary vaccination coverage rate. Nearly a third of reinfected individuals had received a booster vaccine at least 14 days before the last episode of COVID-19. |
| 27 | South Korea | August 2022 | Jang et al. [48] | SARS-CoV-2 reinfection in general population, South Korea: nationwide retrospective cohort study | Individuals with one dose of the vaccine had the highest reinfection rate at 642.2 per 100,000, followed by those not vaccinated (536.2/100,000) and individuals vaccinated with two doses (406.3/100,000). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Gonzales, W.; Chihuantito-Abal, L.A.; Gamarra-Bustillos, C.; Morón-Valenzuela, J.; Zavaleta-Oliver, J.; Gomez-Livias, M.; Vargas-Pancorbo, L.; Auqui-Canchari, M.E.; Mejía-Zambrano, H. Risk Factors Contributing to Reinfection by SARS-CoV-2: A Systematic Review. Adv. Respir. Med. 2023, 91, 560-570. https://doi.org/10.3390/arm91060041
Gómez-Gonzales W, Chihuantito-Abal LA, Gamarra-Bustillos C, Morón-Valenzuela J, Zavaleta-Oliver J, Gomez-Livias M, Vargas-Pancorbo L, Auqui-Canchari ME, Mejía-Zambrano H. Risk Factors Contributing to Reinfection by SARS-CoV-2: A Systematic Review. Advances in Respiratory Medicine. 2023; 91(6):560-570. https://doi.org/10.3390/arm91060041
Chicago/Turabian StyleGómez-Gonzales, Walter, Luis A. Chihuantito-Abal, Carlos Gamarra-Bustillos, Julia Morón-Valenzuela, Jenny Zavaleta-Oliver, Maria Gomez-Livias, Lidia Vargas-Pancorbo, María E. Auqui-Canchari, and Henry Mejía-Zambrano. 2023. "Risk Factors Contributing to Reinfection by SARS-CoV-2: A Systematic Review" Advances in Respiratory Medicine 91, no. 6: 560-570. https://doi.org/10.3390/arm91060041
APA StyleGómez-Gonzales, W., Chihuantito-Abal, L. A., Gamarra-Bustillos, C., Morón-Valenzuela, J., Zavaleta-Oliver, J., Gomez-Livias, M., Vargas-Pancorbo, L., Auqui-Canchari, M. E., & Mejía-Zambrano, H. (2023). Risk Factors Contributing to Reinfection by SARS-CoV-2: A Systematic Review. Advances in Respiratory Medicine, 91(6), 560-570. https://doi.org/10.3390/arm91060041






