Using a Statistical Model to Estimate the Effect of Wildland Fire Smoke on Ground Level PM2.5 and Asthma in California, USA
Abstract
:1. Introduction
2. Methods
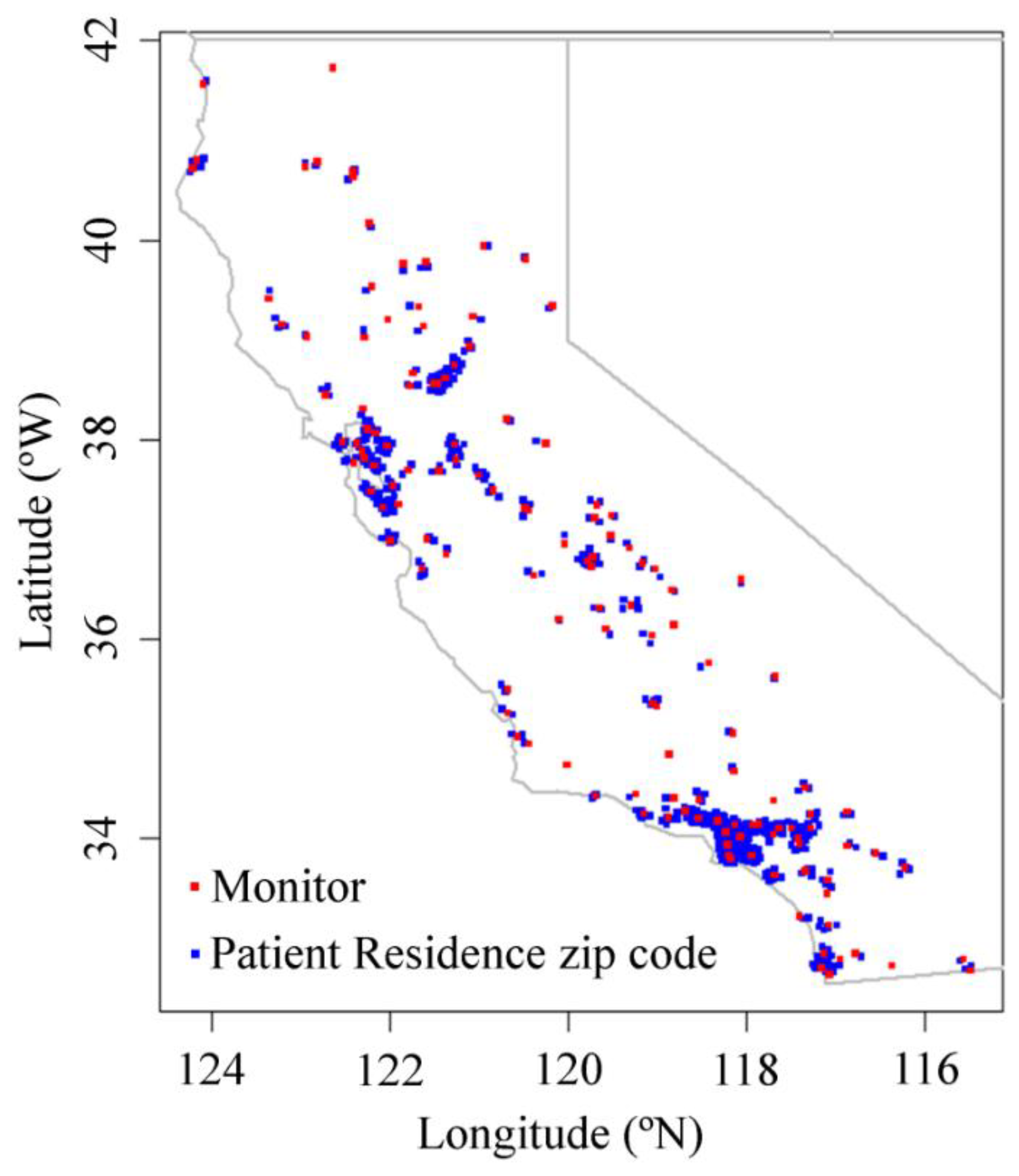
2.1. Data and Participants
2.2. PM2.5 and Smoke Data
2.3. Statistical Models
2.3.1. Odds of Asthma Emergency Room Visit
2.3.2. Odds of Elevated PM2.5 Values
3. Results
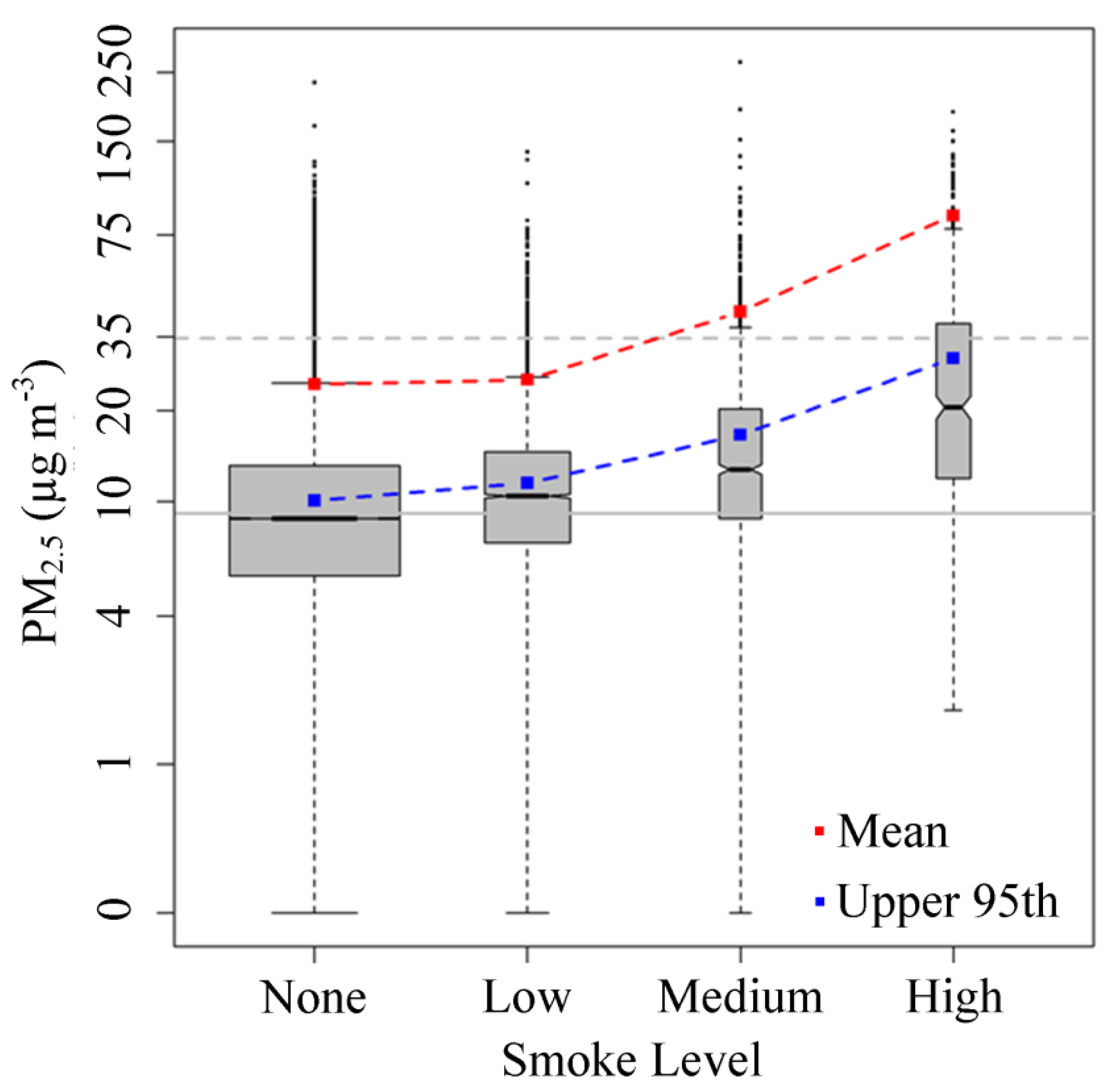
3.1. Effect of Smoke from Fires on Daily PM2.5 Levels
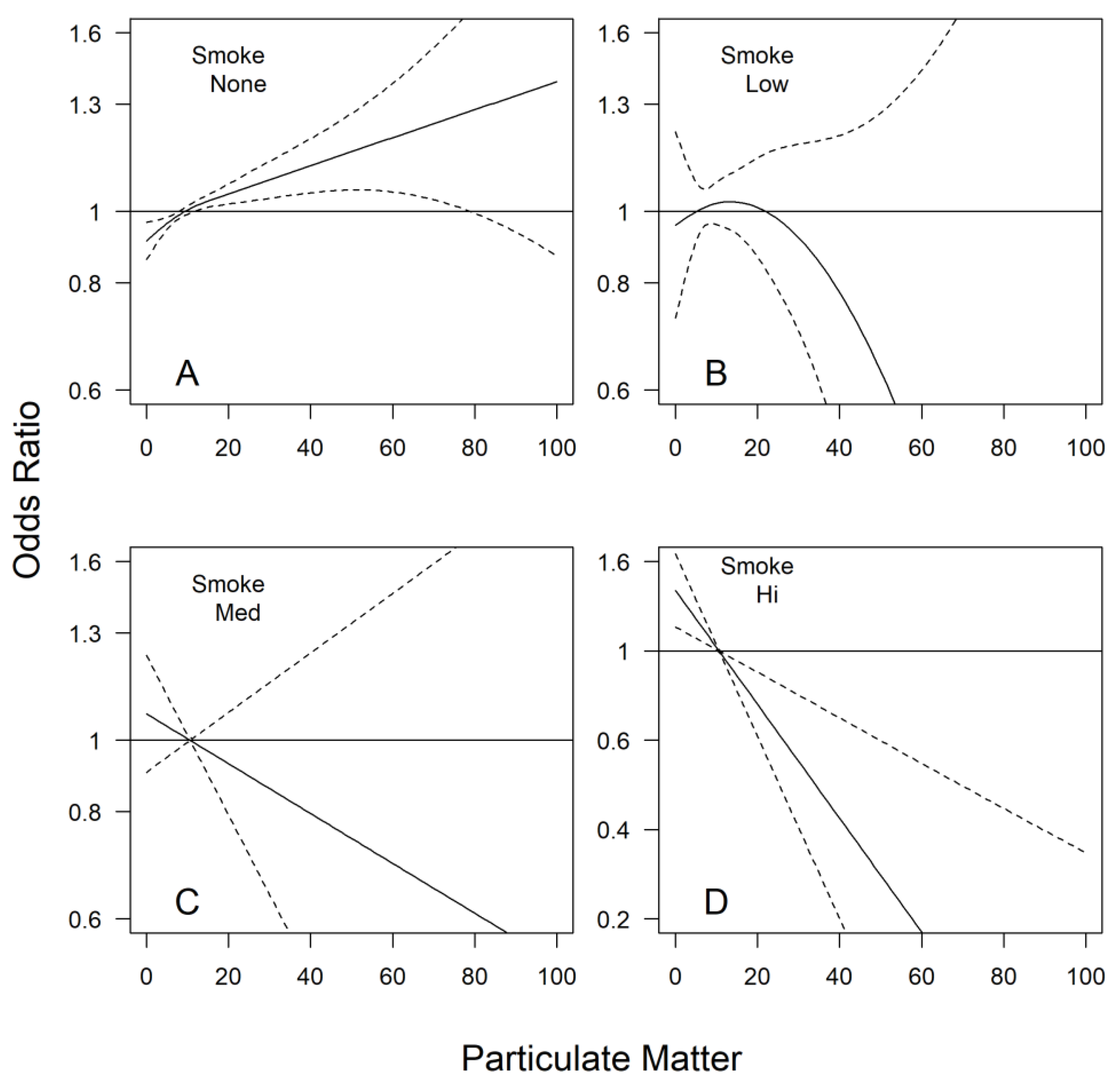
3.2. Effect of PM2.5 on Asthma Emergency Room Visit Cases
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Calkin, D.E.; Gebert, K.M.; Jones, J.G.; Neilson, R.P. Forest Service Large Fire Area Burned and Suppression Expenditure Trends, 1970–2002. J. For. 2005, 103, 179–183. [Google Scholar] [CrossRef]
- Duclos, P.; Sanderson, L.M.; Lipsett, M. The 1987 Forest Fire Disaster in California: Assessment of Emergency Room Visits. Arch. Environ. Health Int. J. 1990, 45, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.D.; Safford, H. Trends in Wildfire Severity: 1984 to 2010 in the Sierra Nevada, Modoc Plateau, and Southern Cascades, California, USA. Fire Ecol. 2012, 8, 41–57. [Google Scholar] [CrossRef]
- Navarro, K.M.; Cisneros, R.; O’Neill, S.M.; Schweizer, D.; Larkin, N.K.; Balmes, J.R. Air-Quality Impacts and Intake Fraction of PM 2.5 during the 2013 Rim Megafire. Environ. Sci. Technol. 2016, 50, 11965–11973. [Google Scholar] [CrossRef] [PubMed]
- Westerling, A.L.; Hidalgo, H.G.; Cayan, D.R.; Swetnam, T.W. Warming and earlier spring increase western U.S. forest wildfire activity. Science 2006, 313, 940–943. [Google Scholar] [CrossRef]
- Flannigan, M.; Stocks, B.; Wotton, B. Climate change and forest fires. Sci. Total Environ. 2000, 262, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Heyerdahl, E.K.; Brubaker, L.B.; Agee, J.K. Annual and decadal climate forcing of historical fire regimes in the interior Pacific Northwest, USA. Holocene 2002, 12, 597–604. [Google Scholar] [CrossRef]
- Liu, Y.; Goodrick, S.L.; Stanturf, J.A. Future U.S. wildfire potential trends projected using a dynamically downscaled climate change scenario. For. Ecol. Manag. 2013, 294, 120–135. [Google Scholar] [CrossRef]
- Stockdale, C.A.; McLoughlin, N.; Flannigan, M.; Macdonald, S.E. Could restoration of a landscape to a pre-European historical vegetation condition reduce burn probability? Ecosphere 2019, 10, e02584. [Google Scholar] [CrossRef]
- Schweizer, D.; Cisneros, R. Wildland fire management and air quality in the southern Sierra Nevada: Using the Lion Fire as a case study with a multi-year perspective on PM2.5 impacts and fire policy. J. Environ. Manag. 2014, 144, 265–278. [Google Scholar] [CrossRef] [PubMed]
- Schweizer, D.; Preisler, H.K.; Cisneros, R. Assessing relative differences in smoke exposure from prescribed, managed, and full suppression wildland fire. Air Qual. Atmos. Health 2019, 12, 87–95. [Google Scholar] [CrossRef]
- Graw, R.L.; Anderson, B.A. Strategies to reduce wildfire smoke in frequently impacted communities in south-western Oregon. Int. J. Wildl. Fire 2022, 31, 1155–1166. [Google Scholar] [CrossRef]
- Dale, V.H.; Joyce, L.A.; McNulty, S.; Neilson, R.P.; Ayres, M.P.; Flannigan, M.D.; Hanson, P.J.; Irland, L.C.; Lugo, A.E.; Peterson, C.J.; et al. Climate change and forest disturbances. Bioscience 2001, 51, 723–734. [Google Scholar] [CrossRef]
- Kampa, M.; Castanas, E. Human health effects of air pollution. Environ. Pollut. 2008, 151, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Pénard-Morand, C.; Annesi-Maesano, I. Air pollution: From sources of emissions to health effects. Breathe 2004, 1, 108–119. [Google Scholar] [CrossRef]
- Perez-Padilla, R.; Schilmann, A.; Riojas-Rodriguez, H. Respiratory health effects of indoor air pollution. Int. J. Tuberc. Lung Dis. 2010, 14, 1079–1086. [Google Scholar]
- Fan, J.; Li, S.; Fan, C.; Bai, Z.; Yang, K. The impact of PM2.5 on asthma emergency department visits: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. 2016, 23, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-K.; Kim, S.-H.; Tak, Y.-J.; Jee, Y.-K.; Lee, B.-J.; Kim, S.-H.; Park, H.-W.; Jung, J.-W.; Bahn, J.-W.; Chang, Y.-S.; et al. High prevalence of current asthma and active smoking effect among the elderly. Clin. Exp. Allergy 2002, 32, 1706–1712. [Google Scholar] [CrossRef] [PubMed]
- Silverman, R.A.; Ito, K. Age-related association of fine particles and ozone with severe acute asthma in New York City. J. Allergy Clin. Immunol. 2010, 125, 367–373.e5. [Google Scholar] [CrossRef]
- Liu, J.C.; Pereira, G.; Uhl, S.A.; Bravo, M.A.; Bell, M.L. A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ. Res. 2015, 136, 120–132. [Google Scholar] [CrossRef]
- Kiser, D.; Metcalf, W.J.; Elhanan, G.; Schnieder, B.; Schlauch, K.; Joros, A.; Petersen, C.; Grzymski, J. Particulate matter and emergency visits for asthma: A time-series study of their association in the presence and absence of wildfire smoke in Reno, Nevada, 2013–2018. Environ. Health 2020, 19, 92. [Google Scholar] [CrossRef] [PubMed]
- Gan, R.W.; Liu, J.; Ford, B.; O’Dell, K.; Vaidyanathan, A.; Wilson, A.; Volckens, J.; Pfister, G.; Fischer, E.V.; Pierce, J.R.; et al. The association between wildfire smoke exposure and asthma-specific medical care utilization in Oregon during the 2013 wildfire season. J. Expo. Sci. Environ. Epidemiol. 2020, 30, 618–628. [Google Scholar] [CrossRef]
- Liu, J.C.; Wilson, A.; Mickley, L.J.; Dominici, F.; Ebisu, K.; Wang, Y.; Sulprizio, M.P.; Peng, R.D.; Yue, X.; Son, J.-Y.; et al. Wildfire-specific Fine Particulate Matter and Risk of Hospital Admissions in Urban and Rural Counties. Epidemiology 2017, 28, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, L.d.S.V.; Hacon, S.d.S.; de Castro, H.A.; Ignotti, E.; Artaxo, P.; Ponce de Leon, A.C.M. Association between fine particulate matter and the peak expiratory flow of schoolchildren in the Brazilian subequatorial Amazon: A panel study. Environ. Res. 2012, 117, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Jalaludin, B.; Smith, M.; O’Toole, B.; Leeder, S. Acute effects of bushfires on peak expiratory flow rates in children with wheeze: A time series analysis. Aust. N. Z. J. Public Health 2000, 24, 174–177. [Google Scholar] [CrossRef]
- Vora, C.; Renvall, M.J.; Chao, P.; Ferguson, P.; Ramsdell, J.W. 2007 San Diego Wildfires and Asthmatics. J. Asthma 2011, 48, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Wiwatanadate, P.; Liwsrisakun, C. Acute effects of air pollution on peak expiratory flow rates and symptoms among asthmatic patients in Chiang Mai, Thailand. Int. J. Hyg. Environ. Health 2011, 214, 251–257. [Google Scholar] [CrossRef]
- Tavallali, P.; Gharibi, H.; Singhal, M.; Schweizer, D.; Cisneros, R. A multi-pollutant model: A method suitable for studying complex relationships in environmental epidemiology. Air Qual. Atmos. Health 2020, 13, 645–657. [Google Scholar] [CrossRef]
- Harrison, R.M.; Jones, A.M.; Lawrence, R.G. Major component composition of PM10 and PM2.5 from roadside and urban background sites. Atmos. Environ. 2004, 38, 4531–4538. [Google Scholar] [CrossRef]
- Tsapakis, M.; Lagoudaki, E.; Stephanou, E.G.; Kavouras, I.G.; Koutrakis, P.; Oyola, P.; von Baer, D. The composition and sources of PM2.5 organic aerosol in two urban areas of Chile. Atmos. Environ. 2002, 36, 3851–3863. [Google Scholar] [CrossRef]
- Watson, J.G.; Chow, J.C.; Houck, J.E. PM2.5 chemical source profiles for vehicle exhaust, vegetative burning, geological material, and coal burning in Northwestern Colorado during 1995. Chemosphere 2001, 43, 1141–1151. [Google Scholar] [CrossRef]
- Jung, C.; Young, L.; Hsu, H.; Lin, M.; Chen, Y.; Hwang, B.; Tsai, P. PM2.5 components and outpatient visits for asthma: A time-stratified case-crossover study in a suburban area. Environ. Pollut. 2017, 231, 1085–1092. [Google Scholar] [CrossRef] [PubMed]
- Chuang, H.-C.; Sun, J.; Ni, H.; Tian, J.; Lui, K.H.; Han, Y.; Cao, J.; Huang, R.-J.; Shen, Z.; Ho, K.-F. Characterization of the chemical components and bioreactivity of fine particulate matter produced during crop-residue burning in China. Environ. Pollut. 2019, 245, 226–234. [Google Scholar] [CrossRef]
- Ruminski, M.; Simko, J.; Kibler, J.; Kondragunta, S.; Draxler, R.; Davidson, P.; Li, P. Use of multiple satellite sensors in NOAA’s operational near real-time fire and smoke detection and characterization program. Proc. SPIE 2008, 7089, 76–86. [Google Scholar] [CrossRef]
- Preisler, H.; Schweizer, D.; Cisneros, R.; Procter, T.; Ruminski, M.; Tarnay, L. A statistical model for determining impact of wildland fires on Particulate Matter (PM 2.5) in Central California aided by satellite imagery of smoke. Environ. Pollut. 2015, 205, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Gharibi, H.; Entwistle, M.R.; Ha, S.; Gonzalez, M.; Brown, P.; Schweizer, D.; Cisneros, R. Ozone pollution and asthma emergency department visits in the Central Valley, California, USA, during June to September of 2015: A time-stratified case-crossover analysis. J. Asthma 2019, 56, 1037–1048. [Google Scholar] [CrossRef]
- Entwistle, M.R.; Gharibi, H.; Tavallali, P.; Cisneros, R.; Schweizer, D.; Brown, P.; Ha, S. Ozone pollution and asthma emergency department visits in Fresno, CA, USA, during the warm season (June–September) of the years 2005 to 2015: A time-stratified case-crossover analysis. Air Qual. Atmos. Health 2019, 12, 661–672. [Google Scholar] [CrossRef]
- Stowell, J.D.; Geng, G.; Saikawa, E.; Chang, H.H.; Fu, J.; Yang, C.-E.; Zhu, Q.; Liu, Y.; Strickland, M.J. Associations of wildfire smoke PM2.5 exposure with cardiorespiratory events in Colorado 2011–2014. Environ. Int. 2019, 133, 105151. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Schweizer, D.; Cisneros, R.; Traina, S.; Ghezzehei, T.A.; Shaw, G. Using National Ambient Air Quality Standards for fine particulate matter to assess regional wildland fire smoke and air quality management. J. Environ. Manag. 2017, 201, 345–356. [Google Scholar] [CrossRef]
- Cisneros, R.; Schweizer, D.; Preisler, H.; Bennett, D.H.; Shaw, G.; Bytnerowicz, A. Spatial and seasonal patterns of particulate matter less than 2.5 microns in the Sierra Nevada Mountains, California. Atmos. Pollut. Res. 2014, 5, 581–590. [Google Scholar] [CrossRef]
- Pope, C.A.; Dockery, D.W. Health Effects of Fine Particulate Air Pollution: Lines that Connect. J. Air Waste Manag. Assoc. 2006, 56, 709–742. [Google Scholar] [CrossRef]
- Wettstein, Z.S.; Hoshiko, S.; Fahimi, J.; Harrison, R.J.; Cascio, W.E.; Rappold, A.G. Cardiovascular and Cerebrovascular Emergency Department Visits Associated With Wildfire Smoke Exposure in California in 2015. J. Am. Heart Assoc. 2018, 7, e007492. [Google Scholar] [CrossRef]
- Cox, T.; Popken, D.; Ricci, P.F. Temperature, not Fine Particulate Matter (PM2.5), is Causally Associated with Short-Term Acute Daily Mortality Rates: Results from One Hundred United States Cities. Dose-Response 2013, 11, 319–343. [Google Scholar] [CrossRef]
- Roberts, S. Interactions between particulate air pollution and temperature in air pollution mortality time series studies. Environ. Res. 2004, 96, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Cisneros, R.; Schweizer, D.; Gharibi, H.; Tavallali, P.; Veloz, D.; Navarro, K. Air Quality Impacts during the 2015 Rough Fire in Areas Surrounding the Sierra Nevada, California. Fire 2021, 4, 31. [Google Scholar] [CrossRef]
- Borchers Arriagada, N.; Horsley, J.A.; Palmer, A.J.; Morgan, G.G.; Tham, R.; Johnston, F.H. Association between fire smoke fine particulate matter and asthma-related outcomes: Systematic review and meta-analysis. Environ. Res. 2019, 179, 108777. [Google Scholar] [CrossRef]
- Cisneros, R.; Brown, P.; Cameron, L.; Gaab, E.; Gonzalez, M.; Ramondt, S.; Veloz, D.; Song, A.; Schweizer, D. Understanding Public Views about Air Quality and Air Pollution Sources in the San Joaquin Valley, California. J. Environ. Public Health 2017, 2017, 4535142. [Google Scholar] [CrossRef]
- Cisneros, R.; Alcala, E.; Schweizer, D.; Burke, N. Smoke complaints caused by wildland fire in the southern Sierra Nevada region, California. Int. J. Wildl. Fire 2018, 27, 677. [Google Scholar] [CrossRef]
- Rappold, A.G.; Fann, N.L.; Crooks, J.; Huang, J.; Cascio, W.E.; Devlin, R.B.; Diaz-Sanchez, D. Forecast-Based Interventions Can Reduce the Health and Economic Burden of Wildfires. Environ. Sci. Technol. 2014, 48, 10571–10579. [Google Scholar] [CrossRef]
- Ng, C.F.S.; Hashizume, M.; Obase, Y.; Doi, M.; Tamura, K.; Tomari, S.; Kawano, T.; Fukushima, C.; Matsuse, H.; Chung, Y.; et al. Associations of chemical composition and sources of PM2.5 with lung function of severe asthmatic adults in a low air pollution environment of urban Nagasaki, Japan. Environ. Pollut. 2019, 252, 599–606. [Google Scholar] [CrossRef] [PubMed]
| Odds Ratio for PM2.5 (µg m−3) Exceeding: | Smoke Level | ||
|---|---|---|---|
| Low | Medium | High | |
| 35 | 3.29 (2.6–4.2) | 26.81 (20.8–34.5) | 114 (87–150) |
| 20 | 2.74 (2.5–3.0) | 10.94 (9.5–12.6) | 34.73 (28.5–42.3) |
| 10 | 2.06 (1.9–2.2) | 4.27 (3.8–4.8) | 9.03 (7.2–11.3) |
| Days with PM2.5 > 35 µg m−3 | One Day | Two Days | Three Days |
|---|---|---|---|
| Odds ratio | 1.23 * | 1.36 * | 1.38 * |
| (95% Confidence Bounds) | (1.12–1.35) * | (1.19–1.55) * | (1.21–1.57) * |
| Days with High Smoke | 1 Day | 2 Days | 3 Days | 4+ Days |
|---|---|---|---|---|
| Odds Ratio | 1.00 | 0.83 | 0.31 * | 0.28 * |
| (95% Confidence Bounds) | (0.83–1.21) | (0.51–1.34) | (0.11–0.89) * | (0.14–0.58) * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schweizer, D.; Preisler, H.; Entwistle, M.; Gharibi, H.; Cisneros, R. Using a Statistical Model to Estimate the Effect of Wildland Fire Smoke on Ground Level PM2.5 and Asthma in California, USA. Fire 2023, 6, 159. https://doi.org/10.3390/fire6040159
Schweizer D, Preisler H, Entwistle M, Gharibi H, Cisneros R. Using a Statistical Model to Estimate the Effect of Wildland Fire Smoke on Ground Level PM2.5 and Asthma in California, USA. Fire. 2023; 6(4):159. https://doi.org/10.3390/fire6040159
Chicago/Turabian StyleSchweizer, Donald, Haiganoush Preisler, Marcela Entwistle, Hamed Gharibi, and Ricardo Cisneros. 2023. "Using a Statistical Model to Estimate the Effect of Wildland Fire Smoke on Ground Level PM2.5 and Asthma in California, USA" Fire 6, no. 4: 159. https://doi.org/10.3390/fire6040159





