1. Introduction
Retroperitoneal hemorrhage is a life-threatening clinical entity. The causes of abdominal pain are numerous, such as abdominal aortic aneurysm rupture, renal tumor bleeding, and coagulation disorders. The presented symptoms, including unspecific abdominal pain, radiation pain, and microscopy hematuria, are similar to acute pyelonephritis, renal colic and renal infarction. The differential diagnosis is very important for physicians. The typical symptoms of renal colic are flank pain and hematuria and the acute pyelonephritis is involved with flank pain and fever. The clinical presentation of acute renal infarction is acute onset of flank pain accompanied by nausea and vomiting. A history of atrial fibrillation is an important indication of renal infarction. However, the three conditions usually closely mimic the clinical presentation of retroperitoneal hemorrhage.
Spontaneous severe retroperitoneal hemorrhage, known as Wunderlich’s syndrome presented with Lenk’s triad, includes acute flank pain, flank mass, and hypovolemic shock. Giant adrenal myelolipoma causing Wunderlich’s syndrome is rare. Here, we present a case of a 59-year-old female who presented with left flank pain and vomiting with a markedly elevated D-dimer. After management, she was diagnosed with adrenal myelolipoma-induced spontaneous retroperitoneal hemorrhage based on computed tomography (CT) image studies. This paper also describes the clinical and CT features of a hemorrhagic myelolipoma and highlights the Wunderlich’s syndrome and Lenk’s triad for timely intervention in hypovolemic shock.
2. Case Report
A 59-year-old woman presented with acute onset persistent left flank pain, radiating to the lower left limb with vomiting and nausea. There was no history of trauma. She had not experienced any recent abdominal discomfort or pain. The frequency, urgency, and dysuria did not occur. Her temperature was 36.9 °C, blood pressure was 117/86 mmHg and heart rate was 76/min. On physical examination, left abdominal tenderness with hypoactive bowel sound was noted. The left knocking pain was not significant. The kidney, ureter, and bladder (KUB) study revealed left renal stones. One limitation of the KUB study is obesity which makes it difficult to distinguish many soft tissues in the abdomen. The laboratory evaluation included the following: white cell count of 8750/µL (neutrophils 72.5%, lymphocytes 18.6%, eosinophils 0.6%, and monocytes 8.2%); hemoglobin 13.0 g/dL; platelet counts 188,000/mL; sodium 138 mmole/L; potassium 3.7 mmol/L; creatinine 1.0 mg/dL; alanine aminotransferase 18 U/L; lipase 136 IU/L; CK 102 IU/L; CK-MB 12 IU/L, and FDP-D-dimer 9211.04 ng/mL. The urinalysis results showed red cell count 2–5/HPF and white cell count 0–2/HPF. The clinical presentations of acute onset persistent left flank pain with microscopic hematuria and renal stones initially favor renal calculus.
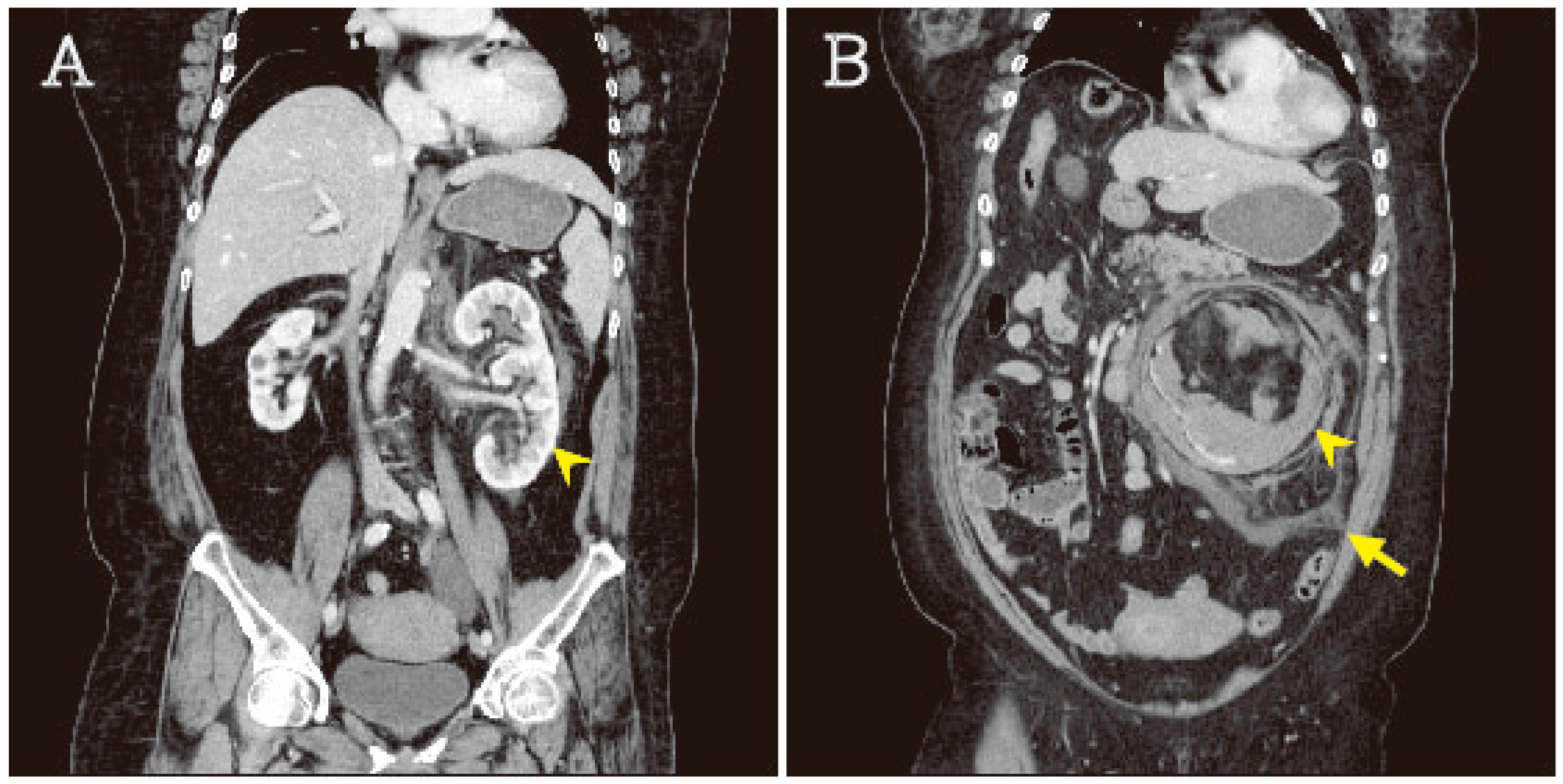
After pain-controlled treatment, the symptoms were progressive. Due to the abnormal D-dimer data accompanied with progressive abdominal pain, internal bleeding was also suspected. Contrast-enhanced abdominal aorta-computed tomography was performed and revealed that a mass lesion (13.6 × 13.1 cm) in the retroperitoneum was comprised of fat and soft tissue densities and abutting on the left kidney. Duplex kidney with duplication of the renal pelvis and ureter was noted with suspected hypertrophy. The contralateral kidney is shrinking. A hematoma was found in left peri- and pararenal spaces (
Figure 1A,B). It was suspected that left retroperitoneal hematoma was caused by renal angiomyolipoma or adrenal myelolipoma and she was admitted to SICU for intensive care.
After controlled internal bleeding, a computed tomography-guided biopsy showed adipose tissue without malignancy cells. After thoroughly explaining the re-bleeding risk of a large benign tumor, she refused the conservative surgery. This patient received an exploratory laparotomy with left nephrectomy due to the tumor being carcerated over the left renal vein. The lower abdominal aorta was repaired after removing the tumor and partial renal artery. During surgery, massive blood loss leading to hypovolemic shock was noted. The follow-up laboratory data revealed hemoglobin 9.9 g/dL. She received cardiopulmonary resuscitation (CPR) for 40 min. After resuscitation, she was returned to spontaneous circulation and transferred to intensive care. After surgery and CPR, the serum creatinine was mildly elevated to 1.7 mg/dL. Acute renal injury was suspected. In addition, the hypertrophy duplex kidney compensating the contralateral kidney is another hypothesis for impaired renal function. The long-term follow-up for residual renal function is necessary. Finally, the pathology report revealed a left adrenal gland tumor (13.0 × 12.5 × 9.5 cm) and left kidney (12.5 × 5.0 × 4.5 cm) with a combined weight of 1.12 kg. The tumor was yellow, dark red, solid, and soft with extensive necrosis and cystic degeneration. Adrenal myelolipoma with extensive hemorrhage and necrosis was diagnosed. Due to her stable condition, she was regularly received for follow-up at the outpatient department.
3. Discussion
Myelolipoma is an uncommon benign tumor, composed of hematopoietic elements and mature fat, with an incidence of 0.08–0.2% [
1,
2,
3]. Adrenal myelolipomas usually occur in patients with a mean age of 40–70 without gender predilection [
4]. The tumor is usually unilateral but there are about 10% patients with bilateral lesions [
5]. Most adrenal myelolipomas are non-functional and asymptomatic but some lesions associated with endocrine dysfunction have been reported [
6]. They are often discovered incidentally but some giant myelolipomas may be found to cause abdominal and back pain due to internal hemorrhage and tumor necrosis [
7]. In 2017, Michael J. Campbell, et al. [
8] reported that only 12 tumors of 150 adrenal myelolipomas were more than 6 cm in size and the giant tumor was 11.8 cm. Previous studies reported that myelolipoma-associated retroperitoneal hemorrhage usually occurred in tumors >7 cm in size [
8,
9]. In our case, the giant adrenal gland tumor (13.0 × 12.5 × 9.5 cm) has a higher retroperitoneal hemorrhage rate. Although the current concept of a treated benign tumor was conservative, some reported data suggest surgical resection in certain cases, including symptomatic, rapidly growing, or giant tumors, to prevent the development of abdominal pain, tumor rupture and intra-abdominal hemorrhage. In addition, previous data reported that the recurrence-free survival outcome of adrenal myelolipomas is up to 12 years [
10,
11].
Severe myelolipoma-induced spontaneous retroperitoneal hemorrhage may cause Wunderlich’s syndrome, which is commonly associated with Lenk’s triad: acute flank pain, flank mass and sign of hypovolemic shock [
12,
13,
14]. The unspecific symptoms are very similar to acute pyelonephritis, renal colic and renal infarction. In emergency departments, the differential diagnosis is very important for further intervention. In nephrolithiasis, the typical symptoms are usually unilateral flank pain or tenderness radiating to the ipsilateral testicle or labium. The laboratory data may reveal gross or microscopic hematuria in about 95% patients on Day 1 [
15]. A family history or previous history of renal stones and gout are risks of renal colic. Acute pyelonephritis is frequently associated with flank pain and fever. Severe acute pyelonephritis would meet the Systemic Inflammatory Response Syndrome (SIRS) criteria and induced sepsis. The laboratory data may reveal leukocytosis and pyuria. The typical clinical presentation of acute renal infarction is usually acute onset of flank pain accompanied by nausea and vomiting. A history of atrial fibrillation is an important indication of renal infarction. However, in the early period, the clinical sign and symptoms of the three conditions were unspecific, closely mimicking the clinical presentation of retroperitoneal hemorrhage, thus potentially leading to physicians missing the diagnosis.
Myelolipoma is commonly diagnosed by incidental image studies due to its characteristic appearance in an image. The computed tomography is a useful tool for myelolipoma. The typical adrenal myelolipoma appears as a fat-containing mass with a well surrounded capsule. The fat component may make it difficult to separate from retroperitoneal fat. In addition, the fatty component may comprise 10–50% soft tissue density. Different components can be distinguished by Hounsfield unit (HU) values. The HU values of myelolipoma are usually higher than those of retroperitoneal fat, which are reported to be <−20, because myelolipoma consists of fat and hematopoietic tissue. The hematopoietic tissue can also be enhanced by a contrast medium, causing a heterogeneous appearance. On magnetic resonance imaging (MRI), fat and hematopoietic tissue is typically hyperintense on the T1-weighted images due to abundant adipose tissue. In T2-weighted images, it is generally intermediate to hyperintense. In the imaging, the origin of the tumor can be defined and distinguished between the kidney and adrenal gland. Angiomyolipoma is one of the renal origin tumors that consists of three major components: smooth muscle; adipose tissue; dilated, thick walled blood vessels. Angiomyolipoma is associated with the tuberous sclerosis complex (TSC) in approximately 10% patients. In computed tomography, it is difficult to distinguish between angiomyolipoma and adrenal myelolipoma due to similar soft tissue density. In stable patients, MRI will provide more information to physicians for more effective management. Although MRI is an effective way of distinguishing between the water and fat component and provides more information to diagnose adrenal myelolipomas, it was not utilized in our case because in clinical practice, MRI is no more useful than a CT image for detecting and characterizing intra-abdominal hemorrhage and bleeding site.
Although Wunderlich’s syndrome is rarely caused by adrenal myolipoma, it is one of the most feared complications of renal neoplasms. The mortality and morbidity may be increased if not treated timely and aggressively. Lenk’s triad is a useful initial management method for differential diagnosis. The CT image is helpful to achieve an accurate diagnosis and determine lesions, based on characteristic appearance. In this article, we highlight that myelolipoma-induced spontaneous retroperitoneal hemorrhage may cause Wunderlich’s syndrome and lead to hypovolemic shock. It is important for emergency physicians to intervene timely. Early diagnosis and management lead to a better outcome.