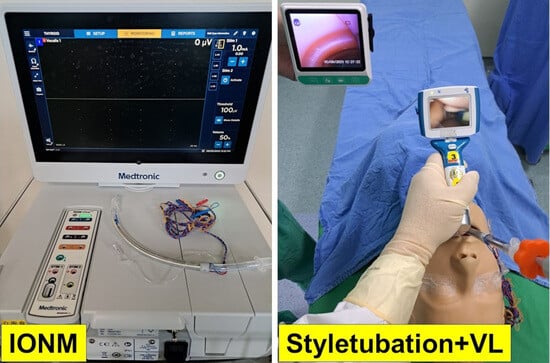
Combined Styletubation with Videolaryngoscopy for Tracheal Intubation in Patients Undergoing Thyroidectomy with Intraoperative Neuromonitoring
Abstract
:1. Introduction
2. Discussion
3. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chiang, F.Y.; Lee, K.W.; Chen, H.C.; Chen, H.Y.; Lu, I.C.; Kuo, W.R.; Hsieh, M.C.; Wu, C.W. Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. World J. Surg. 2010, 34, 223–229. [Google Scholar] [CrossRef]
- Randolph, G.W.; Dralle, H.; International Intraoperative Monitoring Study Group; Abdullah, H.; Barczynski, M.; Bellantone, R.; Brauckhoff, M.; Carnaille, B.; Cherenko, S.; Chiang, F.Y.; et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: International standards guideline statement. Laryngoscope 2011, 121 (Suppl. S1), S1–S16. [Google Scholar] [CrossRef]
- Vasileiadis, I.; Karatzas, T.; Charitoudis, G.; Karakostas, E.; Tseleni-Balafouta, S.; Kouraklis, G. Association of intraoperative neuromonitoring with reduced recurrent laryngeal nerve injury in patients undergoing total thyroidectomy. JAMA Otolaryngol. Head Neck Surg. 2016, 142, 994–1001. [Google Scholar] [CrossRef]
- Cirocchi, R.; Arezzo, A.; D’Andrea, V.; Abraha, I.; Popivanov, G.I.; Avenia, N.; Gerardi, C.; Henry, B.M.; Randolph, J.; Barczyñski, M. Intraoperative neuromonitoring versus visual nerve identification for prevention of recurrent laryngeal nerve injury in adults undergoing thyroid surgery. Cochrane Database Syst. Rev. 2019, 1, CD012483. [Google Scholar] [CrossRef]
- Pei, M.; Zhu, S.; Zhang, C.; Wang, G.; Hu, M. The value of intraoperative nerve monitoring against recurrent laryngeal nerve injury in thyroid reoperations. Medicine 2021, 100, e28233. [Google Scholar] [CrossRef]
- Al-Qurayshi, Z.; Randolph, G.W.; Alshehri, M.; Kandil, E. Analysis of variations in the use of intraoperative nerve monitoring in thyroid surgery. JAMA Otolaryngol. Head Neck Surg. 2016, 142, 584–589. [Google Scholar] [CrossRef]
- Pisanu, A.; Porceddu, G.; Podda, M.; Cois, A.; Uccheddu, A. Systematic review with meta-analysis of studies comparing intraoperative neuromonitoring of recurrent laryngeal nerves versus visualization alone during thyroidectomy. J. Surg. Res. 2014, 188, 152–161. [Google Scholar] [CrossRef]
- Joffe, A.M.; Aziz, M.F.; Posner, K.L.; Duggan, L.V.; Mincer, S.L.; Domino, K.B. Management of difficult tracheal intubation: A closed claims analysis. Anesthesiology 2019, 131, 818–829. [Google Scholar] [CrossRef]
- Rose, D.K.; Cohen, M.M. The incidence of airway problems depends on the definition used. Can. J. Anaesth. 1996, 43, 30–34. [Google Scholar] [CrossRef]
- Adnet, F.; Racine, S.X.; Borron, S.W.; Clemessy, J.L.; Fournier, J.L.; Lapostolle, F.; Cupa, M. A survey of tracheal intubation difficulty in the operating room: A prospective observational study. Acta Anaesthesiol. Scand. 2001, 45, 327–332. [Google Scholar] [CrossRef]
- Shiga, T.; Wajima, Z.; Inoue, T.; Sakamoto, A. Predicting difficult intubation in apparently normal patients: A meta-analysis of bedside screening test performance. Anesthesiology 2005, 103, 429–437. [Google Scholar] [CrossRef]
- Nørskov, A.K.; Wetterslev, J.; Rosenstock, C.V.; Afshari, A.; Astrup, G.; Jakobsen, J.C.; Thomsen, J.L.; Bøttger, M.; Ellekvist, M.; Schousboe, B.M.; et al. Effects of using the simplified airway risk index vs usual airway assessment on unanticipated difficult tracheal intubation—A cluster randomized trial with 64,273 participants. Br. J. Anaesth. 2016, 116, 680–689. [Google Scholar] [CrossRef]
- Schroeder, R.A.; Pollard, R.; Dhakal, I.; Cooter, M.; Aronson, S.; Grichnik, K.; Buhrman, W.; Kertai, M.D.; Mathew, J.P.; Stafford-Smith, M. Temporal trends in difficult and failed tracheal intubation in a regional community anesthetic practice. Anesthesiology 2018, 128, 502–510. [Google Scholar] [CrossRef]
- Bouaggad, A.; Nejmi, S.E.; Bouderka, M.A.; Abbassi, O. Prediction of difficult tracheal intubation in thyroid surgery. Anesth. Analg. 2004, 99, 603–606. [Google Scholar] [CrossRef]
- Kalezić, N.; Milosavljević, R.; Paunović, I.; Zivaljević, V.; Diklić, A.; Matić, D.; Ivanović, B.; Nesković, V. The incidence of difficult intubation in 2000 patients undergoing thyroid surgery—A single center expirience. Vojnosanit. Pregl. 2009, 66, 377–382. [Google Scholar] [CrossRef]
- Tutuncu, A.C.; Erbabacan, E.; Teksoz, S.; Ekici, B.; Koksal, G.; Altintas, F.; Kaya, G.; Ozcan, M. The assessment of risk factors for difficult intubation in thyroid patients. World J. Surg. 2018, 42, 1748–1753. [Google Scholar] [CrossRef]
- Voyagis, G.S.; Kyriakos, K.P. The effect of goiter on endotracheal intubation. Anesth. Analg. 1997, 84, 611–612. [Google Scholar] [CrossRef]
- De Cassai, A.; Papaccio, F.; Betteto, G.; Schiavolin, C.; Iacobone, M.; Carron, M. Prediction of difficult tracheal intubations in thyroid surgery. Predictive value of neck circumference to thyromental distance ratio. PLoS ONE 2019, 14, e0212976. [Google Scholar] [CrossRef]
- Amathieu, R.; Smail, N.; Catineau, J.; Poloujadoff, M.P.; Samii, K.; Adnet, F. Difficult intubation in thyroid surgery: Myth or reality? Anesth. Analg. 2006, 103, 965–968. [Google Scholar] [CrossRef]
- Liu, L.; Yue, H.; Li, J. Comparison of three tracheal intubation techniques in thyroid tumor patients with a difficult airway: A randomized controlled trial. Med. Princ. Pract. 2014, 23, 448–452. [Google Scholar] [CrossRef]
- Dempsey, G.A.; Snell, J.A.; Coathup, R.; Jones, T.M. Anaesthesia for massive retrosternal thyroidectomy in a tertiary referral centre. Br. J. Anaesth. 2013, 111, 594–599. [Google Scholar] [CrossRef]
- Gilfillan, N.; Ball, C.M.; Myles, P.S.; Serpell, J.; Johnson, W.R.; Paul, E. A cohort and database study of airway management in patients undergoing thyroidectomy for retrosternal goitre. Anaesth. Intensive Care 2014, 42, 700–708. [Google Scholar] [CrossRef]
- Pan, Y.; Chen, C.; Yu, L.; Zhu, S.; Zheng, Y. Airway management of retrosternal goiters in 22 cases in a tertiary referral center. Ther. Clin. Risk Manag. 2020, 16, 1267–1273. [Google Scholar] [CrossRef]
- Heinz, E.; Quan, T.; Nguyen, H.; Pla, R. Intubation of a patient with a large goiter: The advantageous role of videolaryngoscopy. Case Rep. Anesthesiol. 2019, 2019, 1327482. [Google Scholar] [CrossRef]
- Watt, S.; Kalpan, J.; Kolli, V. Case report of the use of videolaryngoscopy in thyroid goiter masses: An airway challenge. Int. J. Surg. Case Rep. 2016, 27, 119–121. [Google Scholar] [CrossRef]
- Tan, P.C.; Esa, N. Anesthesia for massive retrosternal goiter with severe intrathoracic tracheal narrowing: The challenges imposed—A case report. Korean J. Anesthesiol. 2012, 62, 474–478. [Google Scholar] [CrossRef]
- Ran, G.; Ning, M.; Zhang, X. Awake fiberoptic intubation in a patient with a large thyroid tumor invading the trachea: A case report. Am. J. Transl. Res. 2022, 14, 2497–2500. [Google Scholar]
- Tan, D.; Zhang, X. Awake fiberoptic nasotracheal intubation and anesthetic management of a patient with a compressed and deviated airway from a massive thyroid goiter: A case report. Cureus 2023, 15, e35278. [Google Scholar] [CrossRef]
- Kim, S.M.; Kim, H.J. Successful advancement of endotracheal tube with combined fiberoptic bronchoscopy and videolaryngoscopy in a patient with a huge goiter. SAGE Open Med. Case Rep. 2020, 8, 2050313X20923232. [Google Scholar] [CrossRef]
- Sun, X.; Chen, C.; Zhou, R.; Chen, G.; Jiang, C.; Zhu, T. Anesthesia and airway management in a patient with acromegaly and tracheal compression caused by a giant retrosternal goiter: A case report. J. Int. Med. Res. 2021, 49, 300060521999541. [Google Scholar] [CrossRef]
- Hohn, A.; Kauliņš, T.; Hinkelbein, J.; Kauliņa, K.; Kopp, A.; Russo, S.G.; Kohlen, S.; Schröder, S. Awake tracheotomy in a patient with stridor and dyspnoea caused by a sizeable malignant thyroid tumor: A case report and short review of the literature. Clin. Case Rep. 2017, 5, 1891–1895. [Google Scholar] [CrossRef]
- Liou, J.Y.; Chow, L.H.; Chan, K.H.; Tsou, M.Y. Successful anesthetic management of a patient with thyroid carcinoma invading the trachea with tracheal obstruction, scheduled for total thyroidectomy. J. Chin. Med. Assoc. 2014, 77, 496–499. [Google Scholar] [CrossRef]
- Jeong, Y.I.; Jun, I.G.; Ha, S.S.; Kwon, H.J.; Lee, Y.M. Extracorporeal membrane oxygenation for the anesthetic management of a patient with a massive intrathoracic goiter causing severe tracheal obstruction with positional symptoms: A case report. Medicine 2019, 98, e17650. [Google Scholar] [CrossRef]
- Xi, F.C.; Song, Y.Q.; Li, W.Q.; Yu, W.K. Extracorporeal membrane oxygenation would provide a new approach to anesthesia for giant thyroid tumor resection: A case report. Asian J. Surg. 2020, 43, 1123–1125. [Google Scholar] [CrossRef]
- Ikeda, Y.; Saito, Y.; Kadomura, T.; Yamada, R.; Shibuya, S.; Itoh, H.; Ishiwa, D.; Tsuji, K.; Nagashima, Z.; Segawa, S. Extracorporeal membrane oxygenation for the anesthetic management of a patient with severe airway stenosis caused by thyroid carcinoma invasion. Surg. Today 2021, 51, 2000–2005. [Google Scholar] [CrossRef]
- Lu, I.C.; Chu, K.S.; Tsai, C.J.; Wu, C.W.; Kuo, W.R.; Chen, H.Y.; Lee, K.W.; Chiang, F.Y. Optimal depth of NIM EMG endotracheal tube for intraoperative neuromonitoring of the recurrent laryngeal nerve during thyroidectomy. World J. Surg. 2008, 32, 1935–1939. [Google Scholar] [CrossRef]
- Tsai, C.J.; Tseng, K.Y.; Wang, F.Y.; Lu, I.C.; Wang, H.M.; Wu, C.W.; Chiang, H.C.; Chiang, F.Y. Electromyographic endotracheal tube placement during thyroid surgery in neuromonitoring of recurrent laryngeal nerve. Kaohsiung J. Med. Sci. 2011, 27, 96–101. [Google Scholar] [CrossRef]
- Atlas, G.; Lee, M. The neural integrity monitor electromyogram tracheal tube: Anesthetic considerations. J. Anaesthesiol. Clin. Pharmacol. 2013, 29, 403–404. [Google Scholar] [CrossRef]
- Mohammad Iskandar, F.F.; Nik Lah, N.A.S.; Ismail, A.J.; Yeap, T.B. Challenges in electromyographic endotracheal tube (EMG ETT) placement via awake fibreoptic intubation during emergency thyroidectomy. BMJ Case Rep. 2021, 14, e242286. [Google Scholar] [CrossRef]
- Berkow, L.; Dackiw, A.P.; Tufano, R.P. Use of the GlideScope for placement of a recurrent laryngeal nerve monitoring endotracheal tube. J. Clin. Anesth. 2011, 23, 81–83. [Google Scholar] [CrossRef]
- Huang, J.M.; Hsu, C.D.; Wu, S.H.; Kuo, Y.W.; Huang, T.Y.; Wu, C.W.; Lu, I.C. Optimization of electromyographic endotracheal tube electrode position by UEScope for monitored thyroidectomy. Laryngoscope Investig. Otolaryngol. 2021, 6, 1214–1219. [Google Scholar] [CrossRef]
- Casano, K.; Cannon, C.R.; Didlake, R.; Replogle, W.R.; Cannon, R. Use of GlideScope in patients undergoing NIM thyroidectomy. Ear Nose Throat J. 2022, 101, 650–653. [Google Scholar] [CrossRef]
- Kriege, M.; Hilt, J.A.; Dette, F.; Wittenmeier, E.; Meuser, R.; Staubitz, J.I.; Musholt, T.J. Impact of direct laryngoscopy vs. videolaryngoscopy on signal quality of recurrent laryngeal nerve monitoring in thyroid surgery: A randomised parallel group trial. Anaesthesia 2023, 78, 55–63. [Google Scholar] [CrossRef]
- Chang, P.Y.; Hu, P.Y.; Lin, Y.C.; Chen, H.Y.; Chiang, F.Y.; Wu, C.W.; Dionigi, G.; Lu, I.C. Trachway video intubating stylet allows for optimization of electromyographic endotracheal tube placement for monitored thyroidectomy. Gland Surg. 2017, 6, 464–468. [Google Scholar] [CrossRef]
- Hsieh, C.Y.; Tan, H.; Huang, H.F.; Huang, T.Y.; Wu, C.W.; Chang, P.Y.; Lu, D.V.; Lu, I.C. Optimization of intraoperative neural monitoring of the recurrent laryngeal nerve in thyroid surgery. Medicina 2022, 58, 495. [Google Scholar] [CrossRef]
- Luk, H.N.; Qu, J.Z.; Shikani, A. Styletubation: The paradigmatic role of video-assisted intubating stylet technique for routine tracheal intubation. Asian J. Anesthesiol. 2023; preprint. [Google Scholar] [CrossRef]
- Luk, H.N.; Luk, H.N.; Qu, J.Z.; Shikani, A. A paradigm shift of airway management: The role of video-assisted intubating stylet technique. In Advances in Tracheal Intubation; Lovich-Sapola, J., Ed.; IntechOpen: London, UK, 2022. [Google Scholar] [CrossRef]
- Luk, H.N.; Qu, J.Z.; Shikani, A. Styletubation for routine tracheal intubation for ear-nose-throat surgical procedures. Ann. Otol. Head Neck Surg. 2023, 2, 1–13. [Google Scholar]
- Kanotra, S.P.; Kuriloff, D.B.; Lesser, J.; Rest-Flarer, F. GlideScope-assisted nerve integrity monitoring tube placement for intra-operative recurrent laryngeal nerve monitoring. J. Laryngol. Otol. 2012, 126, 1271–1273. [Google Scholar] [CrossRef]
- Chen, I.W.; Chen, J.Y.; Lan, K.M.; Hung, K.C. The use of Trachway for electromyographic (EMG) tube placement. Gland Surg. 2018, 7, 244–245. [Google Scholar] [CrossRef]
- Lu, I.C.; Wu, S.H.; Wu, C.W. Neuromuscular blockade management for intraoperative neural monitoring. Kaohsiung J. Med. Sci. 2020, 36, 230–235. [Google Scholar] [CrossRef]
- Lu, I.C.; Hsu, C.D.; Chang, P.Y.; Wu, S.H.; Huang, T.Y.; Lin, Y.C.; Ko, H.Y.; Dionigi, G.; Chai, Y.J.; Chiang, F.Y.; et al. A surgeon-centered neuromuscular block protocol improving intraoperative neuromonitoring outcome of thyroid surgery. Front. Endocrinol. 2022, 13, 817476. [Google Scholar] [CrossRef]
- Lu, I.C.; Wu, C.W.; Chang, P.Y.; Chen, H.Y.; Tseng, K.Y.; Randolph, G.W.; Cheng, K.I.; Chiang, F.Y. Reversal of rocuronium-induced neuromuscular blockade by sugammadex allows for optimization of neural monitoring of the recurrent laryngeal nerve. Laryngoscope 2016, 126, 1014–1019. [Google Scholar] [CrossRef]
- Empis de Vendin, O.; Schmartz, D.; Brunaud, L.; Fuchs-Buder, T. Recurrent laryngeal nerve monitoring and rocuronium: A selective sugammadex reversal protocol. World J. Surg. 2017, 41, 2298–2303. [Google Scholar] [CrossRef]
- Chai, Y.J.; Lee, J.M.; Won, D.; Lee, J.; Hwang, J.Y.; Kim, T.K.; Chang, J.E.; Kim, H.; Yang, H.J.; Min, S.W. Comparison of sugammadex dose for intraoperative neuromonitoring in thyroid surgery: A randomized controlled trial. Laryngoscope 2021, 131, 2154–2159. [Google Scholar] [CrossRef]
- Lu, I.C.; Tan, H.; Wu, S.H.; Huang, T.Y.; Tseng, H.Y.; Wang, J.J.; Dionigi, G.; Chai, Y.J.; Chiang, F.Y.; Chang, P.Y.; et al. A comparison between cisatracurium and rocuronium-induced neuromuscular block on laryngeal electromyography recovery after neostigmine reversal in a porcine model. Front. Endocrinol. 2022, 13, 875597. [Google Scholar] [CrossRef]
- Oh, M.Y.; Chai, Y.J.; Huang, T.Y.; Wu, C.W.; Dionigi, G.; Kim, H.Y.; Kim, C.; Won, D.; Lee, J.M. Administration of neostigmine after tracheal intubation shortens time to successful intraoperative neuromonitoring during thyroid surgery: A randomized controlled trial. Sci. Rep. 2022, 12, 16797. [Google Scholar] [CrossRef]
- Mehanna, R.; Hennessy, A.; Mannion, S.; O’Leary, G.; Sheahan, P. Effect of endotracheal tube size on vocal outcomes after thyroidectomy: A randomized clinical trial. JAMA Otolaryngol. Head Neck Surg. 2015, 141, 690–695. [Google Scholar] [CrossRef]
- Aziz, M.F.; Berkow, L. Pro-con debate: Videolaryngoscopy should be standard of care for tracheal intubation. Anesth. Analg. 2023, 136, 683–688. [Google Scholar] [CrossRef]
- Gungorer, B.; Findik, M.; Kayipmaz, A.E. USB-endoscope laryngoscope is as effective as video laryngoscope in difficult intubation. Disaster Emerg. Med. J. 2021, 6, 75–79. [Google Scholar] [CrossRef]
- Evrin, T.; Szarpak, L.; Katipoglu, B.; Mishyna, N.; Kockan, B.S.; Ruetzler, K.; Schläpfer, M. Video-assisted versus macintosh direct laryngoscopy for intubation of obese patients: A meta-analysis of randomized controlled trials. Disaster Emerg. Med. J. 2022, 7, 30–40. [Google Scholar] [CrossRef]
- Palaczynski, P.; Misiolek, H.; Bialka, S.; Owczarek, A.J.; Gola, W.; Szarpak, L.; Smereka, J. A randomized comparison between the VivaSight double-lumen tube and standard double-lumen tube intubation in thoracic surgery patients. J. Thorac. Dis. 2022, 14, 3903–3914. [Google Scholar] [CrossRef] [PubMed]
- Wieczorek, P.; Szarpak, L.; Dabrowska, A.; Pruc, M.; Navolokina, A.; Raczynski, A.; Smereka, J. A comparison of the bébé VieScope™ and direct laryngoscope for use while wearing PPE-AGP: A randomized crossover simulation trial. Children 2022, 9, 1774. [Google Scholar] [CrossRef] [PubMed]
- Ludwin, K.; Bialka, S.; Czyzewski, L.; Smereka, J.; Marek Dabrowski, M.; Dabrowska, A.; Ladny, J.R.; Ruetzler, K.; Szarpak, L. Video laryngoscopy for endotracheal intubation of adult patients with suspected/ confirmed COVID-19. A systematic review and meta-analysis of randomized controlled trials. Disaster Emerg. Med. J. 2020, 5, 85–97. [Google Scholar] [CrossRef]
- Tsai, P.B.; Luk, H.-N. Sheet barrier and intubating stylet. Encyclopedia 2021, 1, 1058–1075. [Google Scholar] [CrossRef]








| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age/Gender | 64/F | 71/F | 45/F | 33/F | 54/F | 70/F | 41/F | 80/F | 54/F | 54/F |
| Height (cm)/weight (kg) | 153/64 | 154/52 | 156/60 | 148/62 | 153/53 | 147/47 | 151/55 | 152/55 | 161/72 | 145/56 |
| BMI (kg/m2) | 27.3 | 21.9 | 24.6 | 28.3 | 22.6 | 21.7 | 24.1 | 23.8 | 27.7 | 26.6 |
| ASA physical status | II | II | I | I | I | II | I | III | III | II |
| Comorbidity | Myocardial ischemia (T-wave inversion) | Hypertension | Nil | Nil | Hashimoto’s thyroiditis, multinodular goiter with tracheal compression and deviation | Hypertension | Nil | Hypertension, chronic kidney disease | Hypertension, cerebral aneurysm | Diabetes |
| Diagnosis | Bilateral mutinodular goiter | Parkinson’s disease | Thyroid cyst, left | Thyroid papillary carcinoma, left | Papillary microcarcinoma of thyroid | Bilateral multinodular goiter with tracheal deviation | Left thyroid goiter | Bilateral multiple nodular goiter, 3 cm lesion of left thyroid lower pole, T | Thyroid nodular goiter | Bilateral multinodular goiter |
| Major surgery | Bilateral total thyroidectomy; left upper parathyroid gland autotransplantation | Total thyroidectomy | Excision of thyroid cyst, left | Total thyroidectomy | Total thyroidectomy | Total thyroidectomy | Left total thyroidectomy | Total thyroidectomy | Lobectomy (right), partial thyroidectomy (left) | Total thyroidectomy |
| Size of resected thyroid mass | 0.8 to 2.7 cm | 70 to 94 gm | 2.8 × 1.3 (cm) | 1.4 × 0.9 (cm) | (Right lobe): 7.0 × 5.0 × 3.8, (left lobe): 4.8 × 4.2 × 2.3 (cm); (tumor size: 0.2 cm). | (Right lobe) 6.2 × 5.5 × 4.0; (left lobe) 5.5 × 4.0 × 2.0 (cm) | 3.5 × 3.0 × 1.8 (cm) nodular goiter with hemorrhagic cyst | (Right lobe) 5.5 × 3.0 × 2.2 cm; (left lobe) 6.0 × 4.5 × 3.6 (cm); (tumor) (right 1 cm) and (left 0.4 cm) | 0.74 × 0.8 (cm) | 6.8 × 5.0 × 3.6 (cm) |
| Induction | MDZ, FEN, PPF, ROC (0.3 mg/kg), SCh (1.4 mg/kg) | MDZ, FEN, PPF, ROC (1.0 mg/kg) | MDZ, FEN, PPF, ROC (0.3 mg/kg), SCh (1.4 mg/kg) | MDZ, FEN, PPF, ROC (0.6 mg/kg), SCh (1.3 mg/kg) | MDZ, FEN, PPF, ROC (1 mg/kg) | MDZ, FEN, PPF, ROC (0.4 mg/kg), SCh (2 mg/kg) | MDZ, FEN, PPF, ROC (0.2 mg/kg), SCh (2 mg/kg) | MDZ, FEN, PPF, ROC (0.8 mg/kg) | MDZ, FEN, PPF, ROC (0.7 mg/kg) | MDZ, FEN, PPF, ROC (0.9 mg/kg) |
| Maintenance | Sevoflurane | Desflurane | Sevoflurane | Sevoflurane | Sevoflurane | Sevoflurane | Sevoflurane | Sevoflurane | Sevoflurane | Sevoflurane |
| MMT | III | II | III | II | III | II | II | III | II | III |
| ULBT | 1 | Class 1 | Class 2 | Class 1 | Class 1 | Class 1 | Class 1 | Class 2 | Class 1 | Class 2 |
| Inter-incisor distance | 4 cm | 4 cm | 3.5 cm | 4 cm | 4 cm | 4 cm | 4 cm | 5 cm | 4 cm | 4.5 cm |
| Sternomental distance | 15 cm | 13 cm | 17 cm | 16 cm | 16 cm | 16 cm | 16 cm | 15 cm | 15 cm | 17 cm |
| Neck circumference | 34 cm | 39 cm | 31 cm | 34 cm | 34 cm | 35 cm | 38 cm | 39 cm | 36 cm | 34 cm |
| C-L grading | 2b | 2a | 2b | 2a | 2a | 2a | 2b | 2b | 1 | 3 |
| LQS grading | Grade 1 | Grade 1 | Grade 1 | Grade 1 | Grade 2 | Grade 1 | Grade 1 | Grade 2 | Grade 1 | Grade 2 |
| View of glottis (POGO grading) | 100% | 100% | 100% | 100% | 90% | 80% | 90% | 100% | 100 % | 60% |
| Success on first attempt | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Intubation time (VS) | 9 s | 4 s | 33 s | 15 s | 14 s | 8 s | 9 s | 7 s | 5 s | 10 s |
| V1 verification | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Complications | Nil | Nil | Nil | Nil | Nil | Nil | Nil | Nil | Nil | Nil |
| Subjective satisfaction | Easy and excellent | Easy and excellent | Awkward | Easy and excellent | Easy and excellent | Easy and excellent | East and excellent | Easy and excellent | Easy and excellent | Easy and excellent |
| Supplementary materials | Video S1 | Video S2 | Video S3 | Video S4 | Video S5 | Video S6 | Video S7 | Video S8 | Video S9 | Video S10 |
| Case 11 | Case 12 | Case 13 | Case 14 | Case 15 | ||||||
| Age/gender | 71/F | 55/F | 21F | 25/F | 51/F | |||||
| Height (cm)/weight (kg) | 159/53 | 157/72 | 157/63 | 164/64 | 152/73 | |||||
| BMI (kg/m2) | 20.9 | 29.2 | 25.5 | 25.5 | 31.5 | |||||
| ASA physical status | II | I | I | I | I | |||||
| Comorbidity | Hypertension | Nil | Nil | Nil | Nil | |||||
| Diagnosis | Multinodular goiter (left) | Thyroid nodule (right) | Papillary carcinoma, right thyroid; multiple nodular goiter, left | Papillary thyroid carcinoma, right | Bilateral thyroid cysts | |||||
| Major surgery | Hemithyroidectomy (left) | Right hemithyroidectomy, left lobectomy | Total tyroidectomy, neck lymph node dissection | Total thyroidectomy | Bilateral subtotal thyroidectomy | |||||
| Size of resected thyroid mass | 0.8 to 2.7 cm | 1.4 × 1.2 × 1.2 (cm) | 1.78 × 1.3 (cm) | 1.8 cm in length | (Right lobe): 3.0 × 3.2; (left lobe): 2.5 × 3.0 (cm) | |||||
| Induction | MDZ, FEN, PPF, ROC (0.6 mg/kg), SCh (1.5 mg/kg) | MDZ, FEN, PPF, ROC (0.6 mg/kg) | MDZ, FEN, PPF, ROC (0.8 mg/kg) | MDZ, FEN, PPF, ROC (0.6 mg/kg) | MDZ, FEN, PPF, ROC (0.7 mg/kg) | |||||
| Maintenance | Sevoflurane | Sevoflurane | Sevoflurane | Sevoflurane | Sevoflurane | |||||
| MMT | III | II | II | II | II | |||||
| ULBT | Class 3 | Class 1 | Class 1 | Class 1 | Class 1 | |||||
| Inter-incisor distance | 3.5 cm | 3.5 cm | 5.5 cm | 4 cm | 3.5 cm | |||||
| Sternomental distance | 15 cm | 14 | 15 cm | 15 cm | 19 cm | |||||
| Neck circumference | 31 cm | 38 | 35 cm | 34 cm | 40 cm | |||||
| C-L grading | 1 | 3 | 2a | 1 | 2a | |||||
| LQS grading | Grade 1 | Grade 2 | Grade 1 | Grade 1 | Grade 1 | |||||
| View of glottis (POGO grading) | 90% | 100% | 100% | 100% | 100% | |||||
| Success on first attempt | Yes | Yes | Yes | Yes | Yes | |||||
| Intubation time (VS) | 6 s | 10 s | 11 s | 10 s | 6 s | |||||
| V1 verification | Yes | Yes | Yes | Yes | Yes | |||||
| Complications | Nil | Nil | Nil | Nil | Nil | |||||
| Subjective satisfaction | Easy and excellent | Easy and excellent | Easy and excellent | Easy and excellent | Easy and excellent | |||||
| Supplementary materials | Video S11 | Video S12 | Video S13 | Video S14 | Video S15 | |||||
| DL | VL | FOB | Styletubation | |
|---|---|---|---|---|
| Availability and affordability | +++ | ++ | + | ++ |
| Difficult intubation with IONM tube | 6.5% [44] | - | - | 2.7% [44] 0% (this article) |
| First-pass success rate | 75% [20] 96.4% [44] | 97.5% [20] | - | 90% [20] 99% [44] 100% (this article) |
| Time to intubate | 68.8 s [20] | 29.8 s [20] | - | 42.4 s [20] 4–15 s (this article) |
| Initial successful placement without tube depth adjustment | 94.3% [36] 96.4% and 87.3% [37] 33.5% [42] | 67% [40] 97.5% [41] 100% [49] 44% [42] | 100% [38] | 100% [50] 100% (this article) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pan, H.-S.; Corey, T.; Luk, H.-N.; Qu, J.Z.; Shikani, A. Combined Styletubation with Videolaryngoscopy for Tracheal Intubation in Patients Undergoing Thyroidectomy with Intraoperative Neuromonitoring. Anesth. Res. 2024, 1, 8-23. https://doi.org/10.3390/anesthres1010003
Pan H-S, Corey T, Luk H-N, Qu JZ, Shikani A. Combined Styletubation with Videolaryngoscopy for Tracheal Intubation in Patients Undergoing Thyroidectomy with Intraoperative Neuromonitoring. Anesthesia Research. 2024; 1(1):8-23. https://doi.org/10.3390/anesthres1010003
Chicago/Turabian StylePan, Hui-Shan, Tiffany Corey, Hsiang-Ning Luk, Jason Zhensheng Qu, and Alan Shikani. 2024. "Combined Styletubation with Videolaryngoscopy for Tracheal Intubation in Patients Undergoing Thyroidectomy with Intraoperative Neuromonitoring" Anesthesia Research 1, no. 1: 8-23. https://doi.org/10.3390/anesthres1010003