Gastroenterological Aspects of COVID-19 Infection
Share This Topical Collection
Editors
 Dr. Radislav Nakov
Dr. Radislav Nakov
 Dr. Radislav Nakov
Dr. Radislav Nakov
*
E-Mail
Website
Guest Editor
Clinic of Gastroenterology, Tsaritsa Joanna University Hospital, Medical University of Sofia, 1527 Sofia, Bulgaria
Interests: IBD; neurogatroenterology; endoscopy; IBS; colonoscopy; microbiome; FMT; transthyretin amyloidosis; xenobiotics
* We dedicate the memory of the editor, Dr. Radislav Nakov, who passed away during this special issue period.
 Dr. Monika Peshevska-Sekulovska
Dr. Monika Peshevska-Sekulovska
 Dr. Monika Peshevska-Sekulovska
Dr. Monika Peshevska-Sekulovska
E-Mail
Website
Guest Editor
Department of Gastroenterology, University Hospital Lozenetz, Sofia University St. Kliment Ohridski, 1407 Sofia, Bulgaria
Interests: endoscopy; gastrointestinal oncology; IBD; hepatology; microbiome
Topical Collection Information
Dear Colleagues,
The gastrointestinal tract is one of the most vulnerable to SARS-CoV-2 infection systems. As the first line for physical and immunological defense, the intestinal immune system is essential since the gastrointestinal tract can also be a crucial entrance or an interaction site during COVID-19. In addition, patients with gastrointestinal disorders have been associated with poorer clinical outcomes after infection. The liver can also be damaged by the virus or drugs used for treatment.
This Special Issue is devoted to recent and novel insights and perspectives regarding virus–immune cells interactions, immunological mechanisms and processes inside the intestinal mucosa throughout the illness, the involvement of the gastrointestinal tract in SARS-CoV-2 infection, symptoms, complications, therapeutic options, the role of the microbiome in the infection, vaccination for people with gastrointestinal diseases, etc.
Dr. Tsvetelina Velikova
Dr. Radislav Nakov
Dr. Monika Peshevska-Sekulovska
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Gastroenterology Insights is an international peer-reviewed open access quarterly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript.
The Article Processing Charge (APC) for publication in this open access journal is 1600 CHF (Swiss Francs).
Submitted papers should be well formatted and use good English. Authors may use MDPI's
English editing service prior to publication or during author revisions.
Keywords
- SARS-CoV-2
- COVID-19
- mucosa
- gut mucosa
- ACE II
- mucosa-associated lymphoid tissue
- secretory immunoglobulin A
- gut microbiota
- gastrointestinal disorders
- gastrointestinal symptoms
- treatment
- COVID-19 vaccine
- liver failure
- drug-induced live injury
Published Papers (10 papers)
Open AccessReview
Microbiome and Genetic Factors in the Pathogenesis of Liver Diseases
by
Dimitrina Miteva, Monika Peshevska-Sekulovska, Violeta Snegarova, Milena Peruhova, Georgi H. Vasilev, Georgi V. Vasilev, Metodija Sekulovski, Snezhina Lazova, Milena Gulinac, Latchezar Tomov, Antoaneta Mihova and Tsvetelina Velikova
Cited by 1 | Viewed by 1922
Abstract
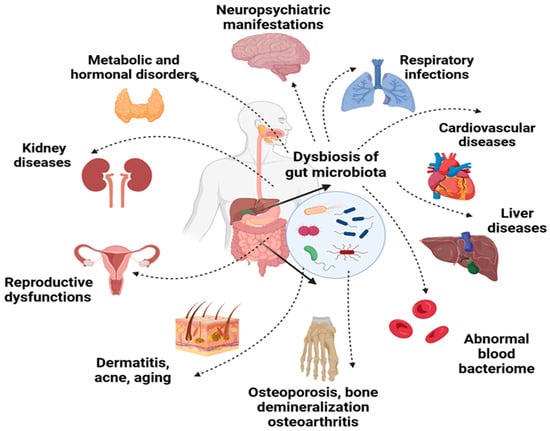
Our genetic background has not changed over the past century, but chronic diseases are on the rise globally. In addition to the genetic component, among the critical factors for many diseases are inhabitants of our intestines (gut microbiota) as a crucial environmental factor.
[...] Read more.
Our genetic background has not changed over the past century, but chronic diseases are on the rise globally. In addition to the genetic component, among the critical factors for many diseases are inhabitants of our intestines (gut microbiota) as a crucial environmental factor. Dysbiosis has been described in liver diseases with different etiologies like non-alcoholic fatty liver disease (NAFLD), alcohol-related liver disease (ALD), viral hepatitis, autoimmune hepatitis (AIH), primary sclerosing cholangitis (PSC), primary biliary cholangitis (PBC), cirrhosis, hepatocellular carcinoma (HCC). On the other hand, new technologies have increased our understanding of liver disease genetics and treatment options. Genome-wide association studies (GWAS) identify unknown genetic risk factors, positional cloning of unknown genes associated with different diseases, gene tests for single nucleotide variations (SNVs), and next-generation sequencing (NGS) of selected genes or the complete genome. NGS also allowed studying the microbiome and its role in various liver diseases has begun. These genes have proven their effect on microbiome composition in host genome–microbiome association studies. We focus on altering the intestinal microbiota, and supplementing some bacterial metabolites could be considered a potential therapeutic strategy. The literature data promote probiotics/synbiotics role in reducing proinflammatory cytokines such as TNF-α and the interleukins (IL-1, IL-6, IL-8), therefore improving transaminase levels, hepatic steatosis, and NAFLD activity score. However, even though microbial therapy appears to be risk-free, evaluating side effects related to probiotics or synbiotics is imperative. In addition, safety profiles for long-term usage should be researched. Thus, this review focuses on the human microbiome and liver diseases, recent GWASs on liver disease, the gut-liver axis, and the associations with the microbiome and microbiome during/after liver disease therapy.
Full article
►▼
Show Figures
Open AccessArticle
COVID-19 and Acute Pancreatitis: Not Increased Risk but Reduced Care
by
Michele Cevolani, Marco Ferronato, Chiara Elide Lizzio, Eleonora Elia, Desy Marini, Elena Mazzotta, Claudio Ricci, Riccardo Casadei and Marina Migliori
Viewed by 982
Abstract
Background and aim: Over the last few years, SARS-CoV-2 has been reported as a possible cause of acute pancreatitis (AP), but whether it is a relevant clinical–epidemiological entity is still a matter of debate. We aim to evaluate the epidemiological characteristics of AP
[...] Read more.
Background and aim: Over the last few years, SARS-CoV-2 has been reported as a possible cause of acute pancreatitis (AP), but whether it is a relevant clinical–epidemiological entity is still a matter of debate. We aim to evaluate the epidemiological characteristics of AP during the first year of the COVID pandemic (2020) and compare them with the pre-COVID period (2008–2019) to identify any differences and clarify a potential causative role of SARS-CoV-2. Methods: We used a monocentric retrospective study of 132 AP patients during 2020 and 1987 AP patients during 2008–2019. Diagnosis and severity were classified according to the revised Atlanta criteria. Propensity score matching was performed according to clinical–epidemiological features, and outcome analysis was performed on two subgroups of 109 patients. Results: The total number of AP cases in 2020 is one of the lowest in the last 13 years (132 cases, median 161, IQR 146-183). No major epidemiological differences were noted. During 2020, we observed a significant modification of the distribution of etiologies (
p < 0.001), mainly based on a decrease in biliary forms (59.6% vs. 43.2%) and an increase in alcoholic forms (6.9% vs. 12.9%). Idiopathic forms remain unchanged (20.5% vs. 21.9%). The proportion of AP of idiopathic etiology and SARS-CoV-2 infection was 0.008%. There were no differences in terms of severity distribution (
p = 0.127), length of stay (
p = 0.916), need for ICU (
p = 0.139), or mortality (
p = 0.462). Even among statistically matched groups, there were no differences between the length of stay (9 vs. 10 days,
p = 0.890), need for ICU admission (1.8% vs. 3.7%,
p = 0.683), or in-hospital mortality (0 vs. 1.8%,
p = 0.342). Conclusions: The lower AP diagnoses indicate delayed and likely missed diagnoses, probably because of both hesitancy and organizational problems during the pandemic. The unchanged proportion of idiopathic forms supports the hypothesis that SARS-CoV-2 is not an AP trigger.
Full article
►▼
Show Figures
Open AccessArticle
Clinical and Laboratory Manifestation of Gastrointestinal Involvement in MIS-C: A Single-Center Observational Study
by
Snezhina Lazova, Latchezar Tomov, Dimitrina Miteva, Iren Tzotcheva, Stamatios Priftis and Tsvetelina Velikova
Cited by 2 | Viewed by 1784
Abstract
Background: Digestive symptoms and gastrointestinal issues in children with coronavirus 2019 disease (COVID-19) and Multisystem Inflammatory Syndrome in Children (MIS-C) are commonly reported in pediatric studies from different countries. Our retrospective observational study aimed to summarize the main digestive symptoms and objective data
[...] Read more.
Background: Digestive symptoms and gastrointestinal issues in children with coronavirus 2019 disease (COVID-19) and Multisystem Inflammatory Syndrome in Children (MIS-C) are commonly reported in pediatric studies from different countries. Our retrospective observational study aimed to summarize the main digestive symptoms and objective data on gastrointestinal involvement in children with MIS-C. Methods: We present the clinical, laboratory, and imaging data of 51 children with MIS-C hospitalized in a single center from 25 November 2020 to 24 April 2021, focusing on gastrointestinal involvement. Results: A total of 46/51 children (90.2%) reported at least one abdominal symptom (abdominal pain (86%, N = 44), vomiting, nausea, diarrhea), predominantly at presentation. Most children were older than 5 years (N = 40, 78%), predominated by the male sex (N = 37, 72.5%), and with a mean age of 8.82 ± 4.16 years. We found a tendency for lymphopenia, neutrophilia, and higher levels of CRP, d-dimer, and ferritin in MIS-C patients with abdominal pain (R-squared 0.188, F-statistic vs. constant model: 11.9,
p-value = 0.00122, 20% explanation of variation with
p = 0.001). We found a statistically significant linear relationship (regression) between neutrophile percentage (NEU%) and hospital stay and a tendency for elevated transaminases to be more frequent in older children (27.3% under 5 years and 65% over 5 years;
p = 0.0583). We found no significant associations between digestive symptoms and age or the predominant SARS-CoV-2 variant. Conclusions: Most of our MIS-C patients presented with abdominal pain, usually along with other GI symptoms, which could be applied in clinical practice to MIS-C in children visiting the emergency room with abdominal pain and evidence of recent COVID-19 contact or infection. Further information from larger cohorts of MIS-C patients is needed to better understand the epidemiology of gastrointestinal involvement in these patients.
Full article
Open AccessReview
Features of Liver Injury in COVID-19 Pathophysiological, Biological and Clinical Particularities
by
Cristina Maria Marginean, Eliza Cinteza, Corina Maria Vasile, Mihaela Popescu, Viorel Biciusca, Anca Oana Docea, Radu Mitrut, Marian Sorin Popescu and Paul Mitrut
Cited by 1 | Viewed by 2576
Abstract
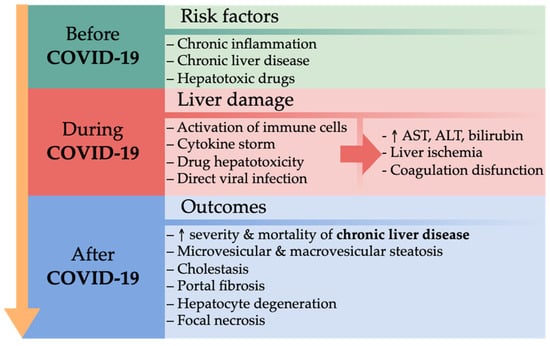
The outbreak of the coronavirus pandemic in March 2020 has caused unprecedented pressure on public health and healthcare. The spectrum of COVID-19 onset is large, from mild cases with minor symptoms to severe forms with multi-organ dysfunction and death. In COVID-19, multiple organ
[...] Read more.
The outbreak of the coronavirus pandemic in March 2020 has caused unprecedented pressure on public health and healthcare. The spectrum of COVID-19 onset is large, from mild cases with minor symptoms to severe forms with multi-organ dysfunction and death. In COVID-19, multiple organ damage has been described, including lung damage, acute kidney injury, liver damage, stroke, cardiovascular and digestive tract disorders. The aspects of liver injury are different, sometimes presenting with only a slight increase in liver enzymes, but sometimes with severe liver injury, leading to acute liver failure requiring liver transplantation. In patients with chronic liver disease, especially liver cirrhosis, immune dysfunction can increase the risk of infection. Immune dysfunction has a multifactorial physiopathological mechanism, implying a complement system and macrophage activation, lymphocyte and neutrophil activity dysfunction, and intestinal dysbiosis. This review aims to evaluate the most relevant studies published in the last years related to the etiopathogenetic, biochemical, and histological aspects of liver injury in patients diagnosed with COVID-19. Liver damage is more evident in patients with underlying chronic liver disease, with a significantly higher risk of developing severe outcomes of COVID-19 and death. Systemic inflammation, coagulation disorders, endothelial damage, and immune dysfunction explain the pathogenic mechanisms involved in impaired liver function. Although various mechanisms of action of SARS-CoV-2 on the liver cell have been studied, the impact of the direct viral effect on hepatocytes is not yet established.
Full article
►▼
Show Figures
Open AccessArticle
Abdominal and Thoracic Imaging Features in Children with MIS-C
by
Elena Ilieva, Vilyana Kostadinova, Iren Tzotcheva, Nadezhda Rimpova, Yordanka Paskaleva and Snezhina Lazova
Cited by 4 | Viewed by 2647
Abstract
(1) Background: Currently, multisystem inflammatory syndrome in children (MIS-C) is diagnosed based on clinical symptoms and laboratory findings of inflammation in the body. Once MIS-C is diagnosed, children will need to be followed over time. The imaging modalities most commonly used in the
[...] Read more.
(1) Background: Currently, multisystem inflammatory syndrome in children (MIS-C) is diagnosed based on clinical symptoms and laboratory findings of inflammation in the body. Once MIS-C is diagnosed, children will need to be followed over time. The imaging modalities most commonly used in the evaluation of patients with MIS-C include radiographs, ultrasound (US), and computed tomography (CT). Our study aims to summarise the literature data for the main gastrointestinal and pulmonary imaging features in children diagnosed with MIS-C and to share a single-centre experience. (2) Methods: We present the imaging findings in a cohort of 51 children diagnosed with MIS-C, admitted between December 2020 and February 2022. Imaging studies include chest and abdominal radiographs, thoracic, abdominal, and neck US and echocardiography (ECHO), and CT of the chest, abdomen, and pelvis. (3) Results: In accordance with the results in other studies, our observations show predominantly gastrointestinal involvement (GI) with ascites (33/51, 65%) and lymphadenopathy (19/51, 37%), ileitis or colitis (18/51, 35%), some cases of splenomegaly (9/51, 18%), hepatomegaly (8/51, 16%), and a few cases of renal enlargement (3/51, 6%) and gallbladder fossa oedema/wall thickening (2/51, 4%). Most common among the thoracic findings are posterior–basal consolidations (16/51, 31%), pleural effusion (14/51, 27%), and ground-glass opacities (12/51, 24%). We also register the significant involvement of the cardiovascular system with pericarditis (30/51, 58%), pericardial effusion (16/51, 31%), and myocarditis (6/51, 12%). (4) Conclusions: Radiologists should be aware of those imaging findings in order to take an important and active role not only in applying an accurate diagnosis, but also in the subsequent management of children with MIS-C. Radiological findings are not the primary diagnostic tool, but can assist in the evaluation of the affected systems and guide treatment.
Full article
►▼
Show Figures
Open AccessReview
Gastrointestinal Ischemia—Stumbling Stone in COVID-19 Patients
by
Monika Peshevska-Sekulovska, Irina Boeva, Metodija Sekulovski, Miroslav Zashev and Milena Peruhova
Cited by 4 | Viewed by 2957
Abstract
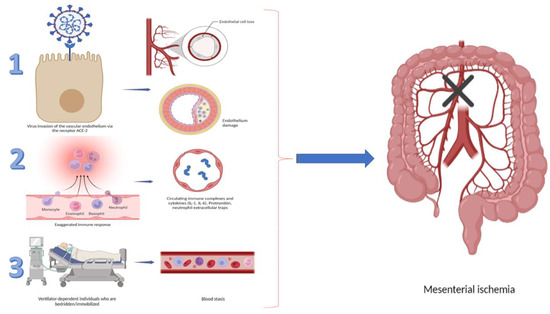
The emergence of the novel SARS-CoV2 virus, proclaimed by the World Health Organization (WHO) as a culpable agent for the pandemic situation, caught the scientific and medical communities off guard. One of the most common complications following pulmonary disease is represented by gastrointestinal
[...] Read more.
The emergence of the novel SARS-CoV2 virus, proclaimed by the World Health Organization (WHO) as a culpable agent for the pandemic situation, caught the scientific and medical communities off guard. One of the most common complications following pulmonary disease is represented by gastrointestinal (GI) disorders, especially ischemic damage. Inflammation, vasculopathy, immobility, endothelial dysfunction, and a hypercoagulable condition have all been proposed as pathophysiological factors for GI ischemia in these patients. Owing to the COVID-19 effect on a variety of GI conditions, especially ischemic changes, and the high mortality rate, physicians should always keep in mind this complication. They should take a deeper look at clinical and imaging modalities in this cohort of patients so that a proper and time-saving treatment strategy can be applied. Our study aimed to elucidate the thrombogenic mechanism in different GI disorders. Moreover, we analyzed the factors related to necrotic GI changes, by summarizing the already reported data of GI ischemia in COVID-19. To the best of our knowledge, this review is the first to incorporate all GI ischemia cases reported in the literature so far.
Full article
►▼
Show Figures
Open AccessArticle
Telemedicine Is an Effective Tool to Monitor Disease Activity in IBD Patients in the COVID-19 Era: A Single Centre Experience Based on Objective Data
by
Emanuele Sinagra, Anita Busacca, Laura Guida, Lucio Carrozza, Daniele Brinch, Federica Crispino, Marcello Maida, Salvatore Battaglia, Ciro Celsa, Calogero Cammà and Maria Cappello
Cited by 4 | Viewed by 3643
Abstract
Background: The COVID-19 outbreak has led IBD clinics to adopt a remote monitoring approach in order to guarantee an adequate follow-up of patients with inflammatory bowel disease (IBD) and ensure the rules of social distancing. Aim: The aim of the study was to
[...] Read more.
Background: The COVID-19 outbreak has led IBD clinics to adopt a remote monitoring approach in order to guarantee an adequate follow-up of patients with inflammatory bowel disease (IBD) and ensure the rules of social distancing. Aim: The aim of the study was to perform a survey on IBD patients who underwent remote monitoring in our tertiary referral center, to assess adherence, patients’ perceptions and satisfaction, and finally their opinions for future monitoring. Furthermore, we evaluated changes in disease activity and Quality of Life (QoL) using validated questionnaires. Methods: Consecutive patients with IBD scheduled for follow-up visits were switched to remote monitoring through e-mail from March 2020 to February 2021. Patients were asked to complete a questionnaire focusing on the following elements of the intervention: (1) self-assessment questions, (2) action plans, and (3) educational messages. Results: Four hundred and twenty four Caucasian patients completed the survey. 233 (55.1%) were male, 220 (52.0%) had Crohn’s Disease (CD). Median baseline Mayo Score and Harvey Bradshaw Index were 3 and 4, respectively. 9 (2.1%) patients were referred to the emergency department because of disease flares. 410 (96.9%) patients were satisfied with telemedicine, and 320 (76.5%) patients reported that they would maintain this approach also after COVID-19 pandemic. Overall, on univariate logistic regression analysis, none of the variables were related to patients’ satisfaction or to an improved QoL. The presence of ulcerative colitis was associated with the need for treatment change. Conclusions: Our results suggest that a telemedicine approach is well accepted by patients with IBD and could represent an effective tool in monitoring disease activity. Further controlled studies are warranted to properly assess if telemedicine can replace face-to-face consultations in IBD.
Full article
Open AccessArticle
COVID-19 Pandemic and Its Impact on Training Programs of Medical Residency in Romania
by
Gabriel Constantinescu, Gina Gheorghe, Vlad Alexandru Ionescu, Oana-Mihaela Plotogea, Vasile Sandru, Camelia Cristina Diaconu, Valentin Nicolae Varlas, Nicolae Bacalbasa, Carmen Cristina Diaconu and Madalina Stan-Ilie
Cited by 2 | Viewed by 3426
Abstract
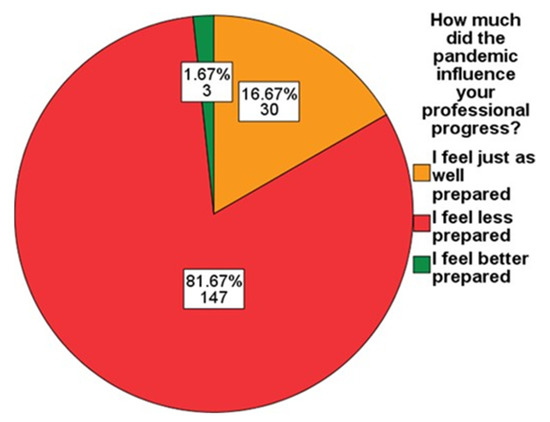
Background: The COVID-19 pandemic has had a negative impact on the training process for resident physicians. The objective of this study was to evaluate the impact of the COVID-19 pandemic on professional training, and also the subjective perception of the levels of stress,
[...] Read more.
Background: The COVID-19 pandemic has had a negative impact on the training process for resident physicians. The objective of this study was to evaluate the impact of the COVID-19 pandemic on professional training, and also the subjective perception of the levels of stress, anxiety, and depression among resident doctors specializing in gastroenterology in Romania. Methods: We conducted an observational cross-sectional study, for a period of two months, among 180 resident doctors specializing in gastroenterology, working in university hospitals in Romania. A questionnaire consisting of 29 questions distributed through social media platforms was completed in Google Forms. Statistical analyses were performed using IBM SPSS software v.20. Results: A linear relationship was identified between the number of daily hospitalizations in the gastroenterology department and the rate of SARS-CoV-2 infection among resident physicians. In total, 80% of the participants reported an increase in the levels of stress, anxiety, and depression during the COVID-19 pandemic, and 88.3% stated that they were unsatisfied by online courses. Conclusions: The COVID-19 pandemic has had negative effects on both professional training and levesl of stress, anxiety and depression of resident doctors specializing in gastroenterology. In the specialty of gastroenterology there may be certain peculiarities, due to the interventional aspects that this medical specialty involves, for example, endoscopic procedures. Thus, the necessity to acquire practical skills in addition to theoretical knowledge increases the negative impact on gastroenterology internship.
Full article
►▼
Show Figures
Open AccessReview
Gastrointestinal Microbiota Dysbiosis Associated with SARS-CoV-2 Infection in Colorectal Cancer: The Implication of Probiotics
by
Frederick Odun-Ayo and Lalini Reddy
Cited by 12 | Viewed by 3912
Abstract
The complexity of coronavirus disease 2019 (COVID-19)’s pathophysiology is such that microbial dysbiosis in the lung and gastrointestinal (GI) microbiota may be involved in its pathogenic process. GI microbiota dysbiosis has been associated with respiratory disorders, including COVID-19, as well as sporadic colorectal
[...] Read more.
The complexity of coronavirus disease 2019 (COVID-19)’s pathophysiology is such that microbial dysbiosis in the lung and gastrointestinal (GI) microbiota may be involved in its pathogenic process. GI microbiota dysbiosis has been associated with respiratory disorders, including COVID-19, as well as sporadic colorectal cancer (CRC) through imbalanced microbiota and compromised immune response. It is pertinent to understand the possible role of probiotics in stabilizing the microbial environment and maintaining the integrity of the respiratory and GI tracts in SARS-CoV-2 induced dysbiosis and colorectal carcinogenesis. The long-term implication of SARS-CoV-2 in GI dysbiosis via microbiota-gut-lung cross-talk could increase the risk of new CRC diagnosis or worsen the condition of previously diagnosed individuals. Recent knowledge shows that the immune-modulatory response to probiotics is shifting the beneficial use of probiotics towards the treatment of various diseases. In this review, we highlight the potential impact of probiotics on SARS-CoV-2 infection associated with CRC through microbiota imbalance in COVID-19 patients.
Full article
►▼
Show Figures
Open AccessReview
COVID-19 and the Gastrointestinal Tract
by
María-Jimena Mucino-Bermejo
Cited by 6 | Viewed by 3555
Abstract
Since it was discovered at the end of 2019; the pandemic of coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has made a serious public health threat worldwide, with over 175 million confirmed cases reported globally. Even
[...] Read more.
Since it was discovered at the end of 2019; the pandemic of coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has made a serious public health threat worldwide, with over 175 million confirmed cases reported globally. Even when COVID-19 was initially considered a respiratory disease, it was actually known to be multisystemic, with gastrointestinal involvement a common clinical finding. Furthermore, COVID-19 may affect patients with gastrointestinal comorbidities, being the clinical intersectionality of utmost interest for gastroenterologists; critical care physicians and all the healthcare team taking care of COVID-19 patients. The present article presents a brief review of the reported gastrointestinal manifestations of COVID-19 disease in both previously healthy individuals and in patients with gastrointestinal comorbidities.
Full article
►▼
Show Figures