Journal Description
Pediatric Reports
Pediatric Reports
is an international, scientific, peer-reviewed open access journal on all aspects of pediatrics, published bimonthly online by MDPI (from Volume 12 Issue 3 - 2020). The Italian Society of Pediatric Psychology (SIPPed) is affiliated with Pediatric Reports and the members receive discounts of the article processing charge.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, ESCI (Web of Science), PubMed, PMC, Embase, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 30.4 days after submission; acceptance to publication is undertaken in 4.9 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
1.4 (2024);
5-Year Impact Factor:
1.2 (2024)
Latest Articles
Language and Cognitive Features in a Girl with Bosch–Boonstra–Schaaf Optic Atrophy Syndrome
Pediatr. Rep. 2025, 17(6), 112; https://doi.org/10.3390/pediatric17060112 (registering DOI) - 24 Oct 2025
Abstract
►
Show Figures
Bosch–Boonstra–Schaaf optic atrophy syndrome (BBSOAS) is an extremely rare neurological condition caused by a disruption in the NR2F-1 gene. The most common clinical features are optic atrophy and intellectual and developmental delay. This case report aims to describe the cognitive and language profile
[...] Read more.
Bosch–Boonstra–Schaaf optic atrophy syndrome (BBSOAS) is an extremely rare neurological condition caused by a disruption in the NR2F-1 gene. The most common clinical features are optic atrophy and intellectual and developmental delay. This case report aims to describe the cognitive and language profile of a six-year-old girl diagnosed with BBSOAS, with a focus on the syndrome’s impact on her developmental outcomes. A detailed assessment of her cognitive and speech–language abilities is provided. Given the limited number of published case studies on BBSOAS, this report integrates relevant findings from the literature, including information on epidemiology, diagnostics, clinical manifestations, and developmental outcomes. It contributes to the expansion of the known mutational spectrum of BBSOAS, in addition to documenting its phenotypic presentation of cognitive and speech–language development. The case is analyzed within the context of current evidence, emphasizing the importance of early assessment, individualized intervention, ongoing developmental monitoring, and the potential for tailored support to promote optimal developmental outcomes.
Full article
Open AccessArticle
Urological, Digestive and Motor Function in Children After Prenatal or Postnatal Repair of Myelomeningocele
by
Marianna Łoskot and Tomasz Koszutski
Pediatr. Rep. 2025, 17(6), 111; https://doi.org/10.3390/pediatric17060111 - 22 Oct 2025
Abstract
►▼
Show Figures
Objectives: Myelomeningocele is one of the most common dysraphic defects. Does shortening the time of exposure to the toxic effects of amniotic fluid and mechanical trauma in utero on the herniated spinal cord and spinal nerves, thanks to prenatal surgery, reduce the
[...] Read more.
Objectives: Myelomeningocele is one of the most common dysraphic defects. Does shortening the time of exposure to the toxic effects of amniotic fluid and mechanical trauma in utero on the herniated spinal cord and spinal nerves, thanks to prenatal surgery, reduce the risk of hydrocephalus with improved musculoskeletal function and better function of the urinary and digestive systems? The aim of the study was to compare the clinical effects of prenatal and postnatal surgery for myelomeningocele in pediatric patients. Methods: Comparison of urological, digestive and motor function in children following prenatal versus postnatal repair of myelomeningocele. The study group consisted of 110 children- 46 operated prenatally and 64 patients postnatally. Information about the children’s assessment of shunt-dependent hydrocephalus, motor skills, bladder and bowel function was obtained from a validated survey questionnaire completed by the children’s parents. Results: In the prenatal group, there was a significantly (p = 0.011) lower percentage of hydrocephalus treated with a shunt (45.71%) compared to the postnatal group (78.26%). The prenatal group revealed a lower percentage of paresis (p = 0.0422) and contractures of the lower limbs (p = 0.0108) and varus deformity (p = 0.0272). Also, in the prenatal group, fewer children move with only the use of a wheelchair (p = 0.0280) and more move independently or with orthopedic equipment (p = 0.0280). In prenatal children, the overall grade of vesico-ureteral reflux was significantly lower (p = 0.0105) and there was also a higher percentage of children with self-controlled defecation (p = 0.0395) and fewer children using enemas (p = 0.0269) and oral pharmacological agents (p = 0.0026). Conclusions: In children with myelomeningocele operated prenatally, compared to the postnatal group, shunt-dependent hydrocephalus and bladder and bowel incontinence were observed with significantly less frequency, and there was better musculoskeletal function. More children operated prenatally moved independently or with orthopedic equipment, and fewer used an orthopedic wheelchair. Further studies, particularly in even larger patient groups, are required to assess clinical benefits of prenatal surgery for children with myelomeningocele.
Full article

Figure 1
Open AccessArticle
Effect of Breastfeeding on the Course of Respiratory Syncytial Virus Infection in Infants: A Single-Center Retrospective Study
by
Anna Maćkowska, Jakub Nowicki and Elżbieta Jakubowska-Pietkiewicz
Pediatr. Rep. 2025, 17(5), 110; https://doi.org/10.3390/pediatric17050110 - 21 Oct 2025
Abstract
Background/Objectives: Respiratory syncytial virus (RSV) is one of the main pathogens causing infections of the respiratory system. In our study, we investigated whether breastfeeding, compared to feeding with formula milk, has an effect on RSV infection in newborns and infants. Methods:
[...] Read more.
Background/Objectives: Respiratory syncytial virus (RSV) is one of the main pathogens causing infections of the respiratory system. In our study, we investigated whether breastfeeding, compared to feeding with formula milk, has an effect on RSV infection in newborns and infants. Methods: We analyzed 51 patients hospitalized at Department of Pediatrics, Newborn Pathology and Bone Metabolic Diseases, University of Lodz, with RSV infection. The infants were divided into two groups by the type of the feeding mode: breast milk or formula milk. Results: Breastfed infants were hospitalized for less time compared to those fed with milk formula (8 days vs. 11 days, p < 0.05). A multivariate linear regression model showed that babies fed with formula milk spent an average of 1.7 days longer in hospital than those fed with breast milk (95% Cl 0.247–3.209). Conclusions: Breastfeeding could reduce the risk, and in some cases, also the severity of RSV infection.
Full article
Open AccessArticle
Sociodemographic Factors, Intent-Uptake Disparities, and Nirsevimab Availability in Infant RSV Immunoprophylaxis
by
Brody J. Lipsett, Benjamin N. Fogel, Katherine E. Shedlock, Ian M. Paul, Eric W. Schaefer, Ruth E. Gardner, Leah D. Kaye and Steven D. Hicks
Pediatr. Rep. 2025, 17(5), 109; https://doi.org/10.3390/pediatric17050109 - 16 Oct 2025
Abstract
Background/Objectives: Respiratory syncytial virus (RSV) is the most common cause of bronchiolitis and infant hospitalization in the US. RSV prevention evolved in 2023 as nirsevimab and maternal RSV pre-fusion vaccine became available for healthy newborns and infants. This study investigates sociodemographic characteristics associated
[...] Read more.
Background/Objectives: Respiratory syncytial virus (RSV) is the most common cause of bronchiolitis and infant hospitalization in the US. RSV prevention evolved in 2023 as nirsevimab and maternal RSV pre-fusion vaccine became available for healthy newborns and infants. This study investigates sociodemographic characteristics associated with RSV immunoprophylaxis. Methods: A cross-sectional survey was conducted from November 2023 through March 2024 among a convenience sample of parents of infants aged <8 months who received newborn care or pediatric ambulatory care at a single academic institution in Central Pennsylvania, USA. Logistic regression examined sociodemographic factors associated with RSV immunoprophylaxis uptake. Given the nirsevimab shortage during the 2023–2024 RSV season, a sensitivity analysis was completed for intended immunoprophylaxis. Results: Among 118 participants, 66.9% received RSV immunoprophylaxis while 74.5% intended to receive nirsevimab. Higher income, private insurance, out-of-home childcare, and an adult/partner working in healthcare were associated with intended nirsevimab receipt. Participation in the Women, Infants and Children program was associated with lower rates of intended nirsevimab receipt. Out-of-home childcare was associated with both RSV immunoprophylaxis uptake and intended nirsevimab receipt. Conclusions: Sociodemographic factors significantly influence the intent to receive nirsevimab and RSV immunoprophylaxis uptake. Having an adult/partner in healthcare was the most significant predictor for intent, suggesting that greater health literacy drives immunization intention. Enrollment in out-of-home childcare was the sole predictor of RSV immunoprophylaxis uptake. These findings highlight the importance of policy initiatives that promote equitable access to RSV immunoprophylaxis, including strategies to address socioeconomic barriers, improve health literacy, and ensure consistent availability of preventive agents for all infants.
Full article
Open AccessReview
A Decade of Transformation in the Management of Childhood Acute Lymphoblastic Leukemia: From Conventional Chemotherapy to Precision Medicine
by
Maurizio Aricò and Valentino Conter
Pediatr. Rep. 2025, 17(5), 108; https://doi.org/10.3390/pediatric17050108 - 16 Oct 2025
Abstract
►▼
Show Figures
Over the past decade, the management of childhood acute lymphoblastic leukemia (ALL) has undergone remarkable advancements. This review explores the transition from conventional chemotherapy protocols to precision medicine approaches, highlighting improvements in diagnostic techniques, therapeutic strategies, and personalized treatments within front-line protocols. Key
[...] Read more.
Over the past decade, the management of childhood acute lymphoblastic leukemia (ALL) has undergone remarkable advancements. This review explores the transition from conventional chemotherapy protocols to precision medicine approaches, highlighting improvements in diagnostic techniques, therapeutic strategies, and personalized treatments within front-line protocols. Key developments include enhanced minimal residual disease detection, the advent of immunotherapies, targeted therapies, and the integration of artificial intelligence. Despite these advancements, challenges remain in ensuring global access and equity. This article discusses the current state of ALL treatment and anticipates future directions in the field.
Full article
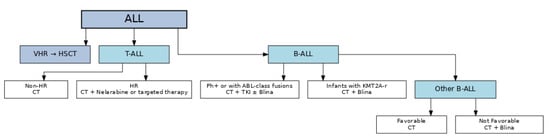
Figure 1
Open AccessArticle
Clinical and Laboratory Characteristics of Neonates Treated Due to Suspected Serious Bacterial Infection: Single Center Cross-Sectional Study
by
Klara Rezic, Ivan Simunovic, Hrvoje Saric and Josko Markic
Pediatr. Rep. 2025, 17(5), 107; https://doi.org/10.3390/pediatric17050107 - 14 Oct 2025
Abstract
Background: Serious bacterial infections (SBIs) in neonates present a significant diagnostic challenge due to nonspecific symptoms and immature immune responses. Early identification is essential to ensure timely treatment and prevent adverse outcomes. This study investigates clinical, laboratory, and epidemiological parameters associated with
[...] Read more.
Background: Serious bacterial infections (SBIs) in neonates present a significant diagnostic challenge due to nonspecific symptoms and immature immune responses. Early identification is essential to ensure timely treatment and prevent adverse outcomes. This study investigates clinical, laboratory, and epidemiological parameters associated with SBI in febrile neonates. Methods: A retrospective analysis was conducted on neonates hospitalized for suspected SBI at University Hospital Split from 1 January 2023 until 31 December 2024). The data was analyzed using descriptive statistics, Mann–Whitney U test and Chi-square test. Results: The study included 71 neonates hospitalized with suspected SBI, of whom 38 (53.5%) had a confirmed SBI. Neonates with SBI had a significantly longer hospital stay (p < 0.001). C-reactive protein (CRP) levels at admission were significantly higher in the SBI group (p = 0.020), while other laboratory parameters showed no significant differences. The most common diagnosis in the SBI group was urinary tract infection (50%). In urine analysis, abundant bacterial presence, strongly positive leukocyte esterase (3+), and positive nitrite findings were significantly associated with the presence of urinary tract infection (UTI). Conclusions: In neonates with suspected SBI, elevated CRP levels and prolonged hospital stay were significantly associated with confirmed SBI. Among specific diagnoses, UTI were most frequent, with urinalysis parameters (bacteria, leukocyte esterase, and nitrites) proving useful in identifying affected cases. However, individual clinical signs showed limited diagnostic value, highlighting the importance of combining clinical and laboratory data in early recognition of SBI.
Full article
Open AccessReview
Is General Anesthesia Safe for a Child with Acute Upper Respiratory Tract Infection? A Narrative Review
by
Jowita Rosada-Kurasińska, Alicja Bartkowska-Śniatkowska, Anna Wiernik, Bartłomiej Kociński and Małgorzata Grześkowiak
Pediatr. Rep. 2025, 17(5), 106; https://doi.org/10.3390/pediatric17050106 - 13 Oct 2025
Abstract
Anesthesia for children with a current respiratory infection or a history of infection within the last two weeks is always associated with a high risk of respiratory complications. However, this risk decreases significantly when the interval between the last symptoms of the infection
[...] Read more.
Anesthesia for children with a current respiratory infection or a history of infection within the last two weeks is always associated with a high risk of respiratory complications. However, this risk decreases significantly when the interval between the last symptoms of the infection and the planned anesthesia and medical procedure is extended to at least 2–4 weeks. The most common adverse events include bronchospasm, laryngospasm, and apnea. For children requiring unplanned procedures—such as emergency, urgent, or immediate general anesthesia—guidelines should be followed to maximize their safety and minimize the risk of complications.
Full article
Open AccessArticle
The Feasibility of the Arabic Version of Ages and Stages Questionnaire 3 to Identify Preterm Infants at Risk of Developmental Delays in Saudi Arabia
by
Turki Aljuhani, Waad Aljurayyad, Ibrahim F. Almudayfir, Ruyuf M. Alhassan, Monerah I. Alharran, Razan A. Aloushan, Reem S. Alsaleem, Nassar M. Althunayyan and Reem A. Albesher
Pediatr. Rep. 2025, 17(5), 105; https://doi.org/10.3390/pediatric17050105 - 13 Oct 2025
Abstract
►▼
Show Figures
Objectives: Preterm infants are at higher risk for developmental delays (DDs) and long-term complications compared with term infants. With the high prevalence of preterm births in Arabic-speaking countries, an Arabic-language screening tool is crucial. The aim of the study is to examine the
[...] Read more.
Objectives: Preterm infants are at higher risk for developmental delays (DDs) and long-term complications compared with term infants. With the high prevalence of preterm births in Arabic-speaking countries, an Arabic-language screening tool is crucial. The aim of the study is to examine the feasibility of utilizing an Arabic version of the Ages and Stages Questionnaire, Third Edition (A-ASQ-3), at 4 months corrected age (CA). Methods: Infants born at or after 28 weeks of gestational age were recruited in this longitudinal study. A total of 48 infants underwent the developmental assessment at 4 months CA using the A-ASQ-3. The primary outcome was identifying the infants at risk for DDs. Descriptive statistics, t-tests, and Firth’s logistic regression were used for analysis. Results: Of the 48 infants, 37 (77.1%) had a DD at in least one of the five A-ASQ-3 domains at 4-months CA. None of the risk factors assessed in this study were associated with a high risk of DDs among preterm infants. Conclusions: The A-ASQ-3 is a feasible tool for identifying infants at risk for DDs at 4 months CA. This finding underscores the need for early screening and tailored intervention programs for preterm infants in Saudi Arabia. The A-ASQ-3 can help identify infants at high risk of DDs and enable prompt referral to healthcare providers.
Full article

Figure 1
Open AccessReview
Glucagon in Pediatric Metabolic Disorders: Pathophysiology and Therapeutic Perspectives
by
Giada Di Pietro, Francesco Chiarelli and Angelika Mohn
Pediatr. Rep. 2025, 17(5), 104; https://doi.org/10.3390/pediatric17050104 - 8 Oct 2025
Abstract
►▼
Show Figures
Over the past century of research, it has become increasingly evident that glucagon should no longer be regarded solely as a counter-regulatory hormone to insulin. Its role in the pathophysiology of metabolic disorders—including diabetes, obesity, and non-alcoholic fatty liver disease—appears to be critical.
[...] Read more.
Over the past century of research, it has become increasingly evident that glucagon should no longer be regarded solely as a counter-regulatory hormone to insulin. Its role in the pathophysiology of metabolic disorders—including diabetes, obesity, and non-alcoholic fatty liver disease—appears to be critical. Hyperglucagonemia is a common feature across several metabolic conditions, not only in adults but also in pediatric populations, suggesting that glucagon may represent both a pathogenic factor and a potential therapeutic target in metabolic disease. Accordingly, therapeutic strategies have been developed that either inhibit or enhance glucagon activity, depending on the clinical context, and some of these approaches are being applied in pediatric care as well. This review aims to provide a comprehensive overview of the pathophysiological role of glucagon in metabolic diseases, synthesizing recent findings that support novel hypotheses for the management and prevention of these conditions.
Full article

Figure 1
Open AccessReview
Role of NLRP3 Inflammasomes in Disorders of Children’s Digestive Systems: A Narrative Review
by
Safaa ELMeneza
Pediatr. Rep. 2025, 17(5), 103; https://doi.org/10.3390/pediatric17050103 - 7 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: This review article highlights the role of the nucleotide-binding domain, leucine-rich repeat, pyrin domain-containing 3 protein (NLRP3) inflammasomes in various gastrointestinal and hepatic disorders in the pediatric age group. NLRP3 inflammasomes are one of the principal intracellular innate immune sensors. During inflammation,
[...] Read more.
Background/Objectives: This review article highlights the role of the nucleotide-binding domain, leucine-rich repeat, pyrin domain-containing 3 protein (NLRP3) inflammasomes in various gastrointestinal and hepatic disorders in the pediatric age group. NLRP3 inflammasomes are one of the principal intracellular innate immune sensors. During inflammation, molecules such as caspase-1 and the release of IL-1β and IL-18 are produced. The NLRP3 inflammasome participates in the preservation of intestinal homeostasis and mucosal immune response. The objective is to evaluate the published articles related to the role of NLRP3 inflammasomes in common pediatric gastrointestinal and hepatic disorders in order to identify the future perspective regarding their possible therapeutic values. Methods: We searched Medline for NLRP3 inflammasomes and disorders of the digestive system during childhood. Results: Although the majority of articles were related to various disorders of adults, such as Alzheimer’s disease, Parkinson’s disease, atherosclerosis, as well as neurodevelopmental disorders, such as schizophrenia, a few published datasets were related to the roles of NLRP3 in the pediatric age group: they addressed autism, rheumatoid arthritis, and other autoimmune diseases, as well as inflammatory bowel diseases (IBD) and hepatic infection. Some research demonstrated that the NLRP3 inflammasome has a protective role; however, it also has a pathogenic function. Conclusions: This review focused on the comprehensive role of inflammasome NLRP3 in the most common pediatric and neonatal gastrointestinal and hepatic diseases, including clinical and experimental studies, as well as the pharmacological inhibitors for NLRP3 inflammasomes, which may provide future therapy for GIT problems, such as IBD.
Full article

Figure 1
Open AccessCase Report
Multisystem Infantile Hemangiomatosis with Cutaneous, Hepatic, and Splenic Involvement
by
Elvira Ioana Buda, Alina Grama, Mădălina Bota, Alexandra Mititelu, Gabriel Bența, Diana Borcău, Otilia Fufezan, Cristina Blag and Tudor Lucian Pop
Pediatr. Rep. 2025, 17(5), 102; https://doi.org/10.3390/pediatric17050102 - 3 Oct 2025
Abstract
►▼
Show Figures
Background: Hemangiomatosis is a rare condition characterized by the presence of multiple benign vascular tumors that may affect various organs, including the skin, liver, and spleen. Complications are closely linked to the location and size of the lesions. Case Presentation: We describe a
[...] Read more.
Background: Hemangiomatosis is a rare condition characterized by the presence of multiple benign vascular tumors that may affect various organs, including the skin, liver, and spleen. Complications are closely linked to the location and size of the lesions. Case Presentation: We describe a rare presentation of infantile hemangiomatosis with widespread cutaneous and oral mucosal lesions, further complicated by splenic and hepatic involvement and secondary cholestasis. The initial progression was unfavorable, with an increase in both the number and size of the lesions. Cardiologic evaluation identified minor valvular insufficiencies, but no secondary cardiac failure. Treatment with propranolol and prednisone was initiated, with a slow favorable evolution. There were no new hemangiomas developed, and those on the face and limbs decreased in size, some disappearing entirely. Hepatic and splenic hemangiomas regressed more slowly, but their reduction and the improvement of cholestasis were progressive. Due to significant iatrogenic Cushing’s syndrome, prednisone was gradually tapered. Transient subclinical hypothyroidism occurred during treatment, resolving spontaneously. Conclusions: The present case illustrates the rarity and complexity of multifocal infantile haemangiomatosis and highlights the importance of early diagnosis, comprehensive organ evaluation, and tailored multidisciplinary management. It clearly demonstrates that prompt intervention and careful therapy adjustment can lead to favorable outcomes even in the setting of extensive visceral involvement.
Full article

Figure 1
Open AccessCase Report
Extremely Premature Infant and Digestive Malformations: Case Report of Atypical Postoperative Journeys
by
Elena Roxana Matran, Alexandru Dinulescu, Ana Prejmereanu, Oana-Alexandra Peta, Radu-Ioan Tiron and Mirela Luminița Pavelescu
Pediatr. Rep. 2025, 17(5), 101; https://doi.org/10.3390/pediatric17050101 - 1 Oct 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Extremely premature infants face complex medical challenges requiring comprehensive multidisciplinary care. Gastrointestinal malformations, while rare, pose significant diagnostic and therapeutic challenges in this vulnerable population. Case Presentation: We report a case of an extremely premature infant born at 26
[...] Read more.
Background and Clinical Significance: Extremely premature infants face complex medical challenges requiring comprehensive multidisciplinary care. Gastrointestinal malformations, while rare, pose significant diagnostic and therapeutic challenges in this vulnerable population. Case Presentation: We report a case of an extremely premature infant born at 26 weeks gestation with very low birth weight (950 g) who developed a digestive pathology rarely encountered in neonatal intensive care: microcolon, which required surgical consultation and intervention, followed by an atypical postoperative course. Conclusions: The early recognition of gastrointestinal malformations in extremely premature infants requires high clinical suspicion and prompt multidisciplinary intervention. Despite complex postoperative course, favorable outcomes are achievable with coordinated care.
Full article

Figure 1
Open AccessCase Report
Life-Threatening Noninfectious Complications of Peritoneal Dialysis in an Infant with End-Stage Kidney Disease
by
Chao-Ting Teng, Yi-Hsuan Tang, Hsin-Hui Wang, Yu-Sheng Lee, Chin-Su Liu, Pei-Chen Tsao, Meei-Chyi Guo, Hui-Lan Chen and Chien-Hung Lin
Pediatr. Rep. 2025, 17(5), 100; https://doi.org/10.3390/pediatric17050100 - 1 Oct 2025
Abstract
►▼
Show Figures
Background: Noninfectious complications of peritoneal dialysis (PD) are common in infants. Mechanical dysfunctions with abdominal compartment syndrome, hydrothorax with respiratory failure, and medication-induced chyloperitoneum are rare during PD. In this case report, we aim to present several life-threatening events and the timely
[...] Read more.
Background: Noninfectious complications of peritoneal dialysis (PD) are common in infants. Mechanical dysfunctions with abdominal compartment syndrome, hydrothorax with respiratory failure, and medication-induced chyloperitoneum are rare during PD. In this case report, we aim to present several life-threatening events and the timely management of a PD infant. Case Presentation: This male infant is a case of infantile nephronophthisis, NPHP3/renal-hepatic–pancreatic dysplasia type 1, with end-stage kidney disease, and he received PD therapy at 4 months of age. Because of the young age with low body weight and hepatosplenomegaly with a limited abdominal cavity, intra-abdominal pressure-associated noninfectious complications frequently occurred. Acute respiratory failure with abdominal dullness was detected at 5 months of age. Abdominal compartment syndrome caused by PD catheter outflow obstruction from omental wrapping was diagnosed via laparoscopic revision surgery. Hyperkalemia, decreased PD drainage volume, and sudden respiratory distress occurred at 10 months old. Hydrothorax due to pleuroperitoneal communication was confirmed by scintigraphy. After thoracoscopic diaphragmatic bleb repair and plication surgery were performed, no recurrence of hydrothorax was observed. Calcium channel blocker-induced chyloperitoneum was observed at 13 months of age. Chylous ascites disappeared after tapering off the calcium channel blocker in 3 days. After the patient grew up with a larger peritoneal cavity, no more pressure-associated complications of PD occurred. Conclusions: The key to successful treatment of rare and life-threatening noninfectious complications of PD in young infants lies in early detection and timely intervention. A limited abdominal cavity is not a contraindication for PD therapy, especially in very young infants with low body weight, because hemodialysis is not a choice of long-term dialysis modality.
Full article

Figure 1
Open AccessArticle
Use of Technological Devices in Children Aged 3–11 Years: Possible Effects on Sleep and Behavioral Difficulties
by
Marta Tremolada, Roberta Maria Incardona, Sabrina Bonichini and Livia Taverna
Pediatr. Rep. 2025, 17(5), 99; https://doi.org/10.3390/pediatric17050099 - 29 Sep 2025
Abstract
Background: The use of technological devices by children has increased in recent years, as several Italian studies have shown, even if limited studies assessed the possible effects on sleep and psychological wellbeing in preschool and schoolchildren. Objectives: This cross-sectional study seeks to examine
[...] Read more.
Background: The use of technological devices by children has increased in recent years, as several Italian studies have shown, even if limited studies assessed the possible effects on sleep and psychological wellbeing in preschool and schoolchildren. Objectives: This cross-sectional study seeks to examine the prevalence and typology of usage, as well as the potential socio-demographic factors associated with it. Additionally, it aims to assess emotional behavior and sleeping difficulties, and their possible correlations with children’s attitudes towards technological devices. Methods: The study included 314 children (52.2% males), with an average age of 7.86 years (SD = 2.02) and mainly their mothers (80.2%). Participants were given a series of self- and proxy-report questionnaires about the digital age, type of activities, hours of sleep, and their behavioral/emotional difficulties (CBCL and SDQ questionnaires). The analyses were descriptive and correlational because of the explorative nature of this study. Results: Parents declared tablets as the device most used by children (49.8%), with an average daily use time of 22.86 min (SD = 33.62). Their digital starting age was on average 5.91 years (SD = 2.25) with mostly recreational activities (Mean = 3.15; SD = 0.72). Parents and children agreed on the time spent with the technological devices reports, while they discorded on the means of creative activities use (t109 = −8.86; p < 0.001), with children reporting a higher frequency (M = 2.45; SD = 0.69) than their parents (M = 1.89; SD = 0.76). The tablet time was significantly different by gender (t309 = −2.34; p = 0.02), with boys using tablets for a longer mean time than girls (27.8 versus 18.22) and having more ADHD problems (t312 = −3.11; p = 0.002; 2.68 versus 1.74). Parents declared an average of 9.55 (SD = 0.55) hours of sleep per night for their children. A significant correlation was found between PC usage time and sleep hours duration (r = −0.13; p = 0.019). The frequency of tablet use was correlated with both the Behavioral Problems Scale (r = 0.15; p = 0.010) and the ADHD Scale (r = 0.11; p = 0.049). Conclusions: Based on these empirical results, preventive programmes and educational activities should be established.
Full article
(This article belongs to the Special Issue Mental Health and Psychiatric Disorders of Children and Adolescents)
►▼
Show Figures

Figure 1
Open AccessArticle
Measuring Vitality and Depletion During Adolescence: Validation of the Subjective Vitality/Subjective Depletion Scale in a Sample of Italian Students
by
Giulia Raimondi, Michele Zacchilli, Christina M. Frederick, Fabio Alivernini, Sara Manganelli, Elisa Cavicchiolo, Fabio Lucidi, Tommaso Palombi, Andrea Chirico and James Dawe
Pediatr. Rep. 2025, 17(5), 98; https://doi.org/10.3390/pediatric17050098 - 25 Sep 2025
Abstract
Background/Objectives: Adolescence is a critical developmental phase marked by rapid cognitive, emotional, and social changes that influence how individuals experience psychological energy and exhaustion. Self-Determination Theory recently proposed a dual-process model, based on two distinct, yet related, constructs: Subjective Vitality, associated with
[...] Read more.
Background/Objectives: Adolescence is a critical developmental phase marked by rapid cognitive, emotional, and social changes that influence how individuals experience psychological energy and exhaustion. Self-Determination Theory recently proposed a dual-process model, based on two distinct, yet related, constructs: Subjective Vitality, associated with well-being and positive health outcomes, and Subjective Depletion, associated with illbeing and negative emotions. Since, to date, no study has investigated vitality and depletion during adolescence, this study aims to validate the Subjective Vitality/Depletion Scale (SVDS) in a large sample of adolescents. Methods: A total of 1111 Italian adolescents (Mage = 14.49, SDage = 1.49; 48% females) completed the SVDS and other validated self-report measures. Specifically, the psychometric properties of the SVDS across biological sex and age groups and latent mean differences across these groups were assessed. Results: Findings supported the dimensionality of the SVDS with two correlated factors, and its construct validity through associations with positive and negative affect and basic psychological needs satisfaction. Full invariance for the SVDS was achieved across biological sex and age groups. Latent mean analyses indicated that males reported higher levels of vitality compared to females (Cohen’s d = 0.46), with no significant differences for depletion; older adolescents reported lower levels of vitality (d = −0.23) and higher levels of depletion (d = 0.20) compared to younger adolescents. Conclusions: These findings support the SVDS as a valid and reliable instrument for assessing energy-related experiences in adolescence. The results suggest meaningful sex differences and a potential developmental trend of declining subjective energy from early to later adolescence.
Full article
(This article belongs to the Section Pediatric Psychology)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Parent but Not Peer Attachment Mediates the Relations Between Childhood Poverty and Rural Adolescents’ Internalizing Problem Behaviors
by
Qingfang Song, Sara S. Whipple, Stacey N. Doan, Rochelle C. Cassells and Gary W. Evans
Pediatr. Rep. 2025, 17(5), 97; https://doi.org/10.3390/pediatric17050097 - 17 Sep 2025
Abstract
►▼
Show Figures
Objectives: The purpose of this study was to examine the prospective, longitudinal relations among childhood poverty and rural adolescents’ internalizing and externalizing problem behaviors, and the mediational roles of adolescent attachment to parents and peers. Methods: Participants were from a longitudinal study of
[...] Read more.
Objectives: The purpose of this study was to examine the prospective, longitudinal relations among childhood poverty and rural adolescents’ internalizing and externalizing problem behaviors, and the mediational roles of adolescent attachment to parents and peers. Methods: Participants were from a longitudinal study of rural poverty. Two home visits were conducted, roughly four years apart (Time 1: N = 226; Mage = 13.36, 52.7% male; Time 2: N = 215; Mage = 17.47 years, 51.2% male). Each family’s income-to-needs ratio was assessed at each visit. At Time 2, participants completed questionnaires reporting their attachments to parents and peers, and their externalizing and internalizing symptoms. Results: Parent attachment was found to mediate the relationship between Time 1 family income-to-needs ratio and Time 2 internalizing problems. The mediational effects of peer attachment predicting Time 2 internalizing or externalizing symptoms were not significant. Conclusions: The long-term impact of childhood poverty on adolescents’ parent attachment and their well-being is discussed.
Full article

Figure 1
Open AccessCase Report
An Infant Autopsy Case of Acute Appendicitis with Lymphoid Hyperplasia
by
Momoka Tanabe, Kazuho Maeda, Hikaru Kuninaka, Moe Mukai, Noriko Ogawa, Ayako Nasu, Chiaki Fuke, Yosuke Usumoto and Yoko Ihama
Pediatr. Rep. 2025, 17(5), 96; https://doi.org/10.3390/pediatric17050096 - 17 Sep 2025
Abstract
►▼
Show Figures
Acute appendicitis is a common cause of acute abdominal pain but is rare in infants because of anatomical and physiological characteristics that reduce the risk of the luminal obstruction of the appendix. However, when it occurs in infants, it is often difficult to
[...] Read more.
Acute appendicitis is a common cause of acute abdominal pain but is rare in infants because of anatomical and physiological characteristics that reduce the risk of the luminal obstruction of the appendix. However, when it occurs in infants, it is often difficult to diagnose clinically and may progress rapidly to a fatal outcome. We report a forensic autopsy case of an 11-month-old infant who died 2 d after developing fever and decreased oral intake, without antemortem diagnosis. Autopsy revealed fibrinous ascitic fluid and an edematous, dark-red appendix with fibrin deposits, but no macroscopic luminal obstruction or perforation. Histopathological examination showed diffuse inflammatory cell infiltration and hemorrhage across all layers of the middle and peripheral portions of the appendix, along with lymphoid hyperplasia in the middle portion. Intestinal bacteria were detected in the ascitic fluid. The cause of death was identified as acute appendicitis with subsequent generalized peritonitis. Although luminal obstruction is a common cause of appendicitis, it was not observed macroscopically in this case. However, histopathological findings suggested that lymphoid hyperplasia in the middle portion of the appendix caused luminal narrowing and impaired circulation in the appendiceal wall, triggering appendicitis. This case demonstrates that infantile appendicitis can be fatal even without perforation and highlights the potential role of lymphoid hyperplasia in the pathogenesis. It also underscores the importance of considering appendicitis in the differential diagnosis of infants with nonspecific symptoms and illustrates the value of postmortem histopathological investigation in elucidating the disease mechanism.
Full article

Figure 1
Open AccessCase Report
Respiratory Syncytial Virus Infection in Children with Acute Lymphoblastic Leukemia (ALL): A Contemporary Emerging and Struggling Clinical Event
by
Marta Arrabito, Emanuela Cannata and Luca Lo Nigro
Pediatr. Rep. 2025, 17(5), 95; https://doi.org/10.3390/pediatric17050095 - 17 Sep 2025
Abstract
►▼
Show Figures
Systemic viral infections are frequently life-threatening in immunocompromised children. Many viral pathogens are reported to be the cause of morbidity and mortality in these pediatric patients, but scarce evidence is related to respiratory syncytial virus infection (RSV), which is one of the main
[...] Read more.
Systemic viral infections are frequently life-threatening in immunocompromised children. Many viral pathogens are reported to be the cause of morbidity and mortality in these pediatric patients, but scarce evidence is related to respiratory syncytial virus infection (RSV), which is one of the main viral causes of lower respiratory tract infection in infants and young children. Herein we report the experience of the Center of Pediatric Hematology Oncology of Catania regarding RSV infection in pediatric leukemia patients, describing four cases: three with only respiratory involvement and complete recovery (two of them presented mild symptoms and one evolved into severe respiratory failure) and a fourth case with an initial hepatic and pulmonary involvement leading to death. Unfortunately, some viral infections have delayed diagnoses because of lack of awareness and atypical presentation. Therefore, our intent is to highlight the importance of mindfulness of the occurrence of this infection and of its typical and atypical manifestations in order to detect it early and decrease the risk of morbidity and mortality.
Full article

Figure 1
Open AccessCase Report
Case Report of Salmonella and HHV-6 Meningitis in an Infant
by
Sara Abed, Tahani Asiri, Razan Alzahrani and Wujud Hunjur
Pediatr. Rep. 2025, 17(5), 94; https://doi.org/10.3390/pediatric17050094 - 15 Sep 2025
Abstract
►▼
Show Figures
Bacterial meningitis is one of the most serious infections. Salmonella meningitis is associated with a high prevalence of long-term adverse outcomes, often linked to acute complications and a broad range of potential neurological sequelae following the infection. Acute complications such as brain abscesses
[...] Read more.
Bacterial meningitis is one of the most serious infections. Salmonella meningitis is associated with a high prevalence of long-term adverse outcomes, often linked to acute complications and a broad range of potential neurological sequelae following the infection. Acute complications such as brain abscesses and chronic complications such as hearing loss and developmental delay. In this report, we present a case of a 2-month-old male patient with seizures, hypoactivity and respiratory symptoms, who was found to have Salmonella bacteremia complicated by Salmonella and Human Herpes Virus-6 (HHV-6) meningitis, as well as rhinovirus bronchiolitis, along with follow-up findings. The patient’s data, including demographics, presenting symptoms, physical examination findings, and whole exome sequence results, as well as investigations such as complete blood count (CBC), cerebrospinal fluid (CSF) analysis, liver enzyme levels, and imaging findings, were collected from the electronic medical record system using a case report form. In addition, immunological workups were performed, as serious Salmonella infections were more common in immunocompromised patients. In the literature, there was no clear correlation between Salmonella and HHV-6 meningitis, rhinovirus bronchiolitis, and the complications that developed in this infant. This case report provides valuable insights into the clinical spectrum and long-term outcomes of patients with Salmonella meningitis.
Full article

Graphical abstract
Open AccessArticle
Alarmin Levels and Gastroesophageal Reflux Disease in Children: Significant Elevation of Thymic Stromal Lymphopoietin
by
Ola Sobieska-Poszwa, Szymon Suwała, Aneta Mańkowska-Cyl and Aneta Krogulska
Pediatr. Rep. 2025, 17(5), 93; https://doi.org/10.3390/pediatric17050093 - 15 Sep 2025
Abstract
►▼
Show Figures
Background/Objectives: In children, gastroesophageal reflux disease (GERD) may lead to epithelial barrier dysfunction and the release of thymic stromal lymphopoietin (TSLP), interleukin-25 (IL-25), interleukin-33 (IL-33) and periostin, known as alarmins. These cytokines are associated with type 2 inflammation and may contribute to
[...] Read more.
Background/Objectives: In children, gastroesophageal reflux disease (GERD) may lead to epithelial barrier dysfunction and the release of thymic stromal lymphopoietin (TSLP), interleukin-25 (IL-25), interleukin-33 (IL-33) and periostin, known as alarmins. These cytokines are associated with type 2 inflammation and may contribute to respiratory and allergic conditions. The main purpose of this study is to evaluate serum concentrations of TSLP, IL-25, IL-33, and periostin in children with and without GERD and to assess their relationships with bronchial hyperresponsiveness (BHR) and sensitization to inhaled allergens. Methods: The study included 93 children aged 7–17 years. GERD was diagnosed based on 24-h esophageal pH impedance monitoring. Serum levels of TSLP, IL-25, IL-33, and periostin were measured using enzyme-linked immunosorbent assay (ELISA). It should be noted that the assay used does not distinguish between TSLP isoforms, which represents a limitation of the study. BHR was assessed via a methacholine challenge test, and allergen sensitization was determined using skin prick tests and allergen-specific immunoglobulin E (asIgE). Results: Serum TSLP levels were significantly higher in children with GERD compared to those without, whereas IL-25, IL-33 and periostin did not differ notably between groups. Periostin was associated with the degree of sensitization to inhalant allergens, but no significant links were found between cytokine levels and bronchial hyperresponsiveness. Conclusions: Significantly higher TSLP levels were noted in children with GERD than in those without. Hence, TSLP may have a potential role as a biomarker of epithelial immune activation in pediatric GERD. In addition, periostin was associated with sensitization to inhalant allergens, although it did not differentiate between children with and without GERD.
Full article

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Adolescents, Children, Dietetics, Foods, Nutrients, Pediatric Reports
Personalized and Sustainable Nutrition for Children and Adolescents: An Important Step for the 2030 Agenda
Topic Editors: Amelia Martí, Valentina De CosmiDeadline: 30 October 2025

Conferences
Special Issues
Special Issue in
Pediatric Reports
Mental Health and Psychiatric Disorders of Children and Adolescents
Guest Editor: Artemis K. TsitsikaDeadline: 31 October 2025
Special Issue in
Pediatric Reports
Global Neonatal Screening: Expanding Horizons in Diagnostic Technologies
Guest Editor: Victoria KainDeadline: 31 January 2026
Special Issue in
Pediatric Reports
Feature Papers on Child Developmental Disorders and Neurology Research
Guest Editors: Giovanni Battista Dell’Isola, Alberto Verrotti di PianellaDeadline: 30 April 2026
Special Issue in
Pediatric Reports
Diagnosis and Treatment of the Maxillofacial Region in Pediatric Patients
Guest Editors: Maciej Chęciński, Maciej SikoraDeadline: 30 June 2026
Topical Collections
Topical Collection in
Pediatric Reports
COVID-19: What Happens in Pediatric Research in the Era of Pandemic
Collection Editor: Maurizio Aricò
Topical Collection in
Pediatric Reports
Recent Advances and Critical Issues in Pediatrics: a Collection of Feature Review Articles
Collection Editors: Maurizio Aricò, Claudia Mandato, Pietro Vajro