Understanding the Impact of Walkability, Population Density, and Population Size on COVID-19 Spread: A Pilot Study of the Early Contagion in the United States
Abstract
:1. Introduction
2. Background: Urban Features and Infectious Diseases Spread
2.1. Walkability
2.2. Population Density
2.3. Population Size
2.4. Related Work
3. Method
3.1. Data
3.2. Best Subsets Regression
4. Results
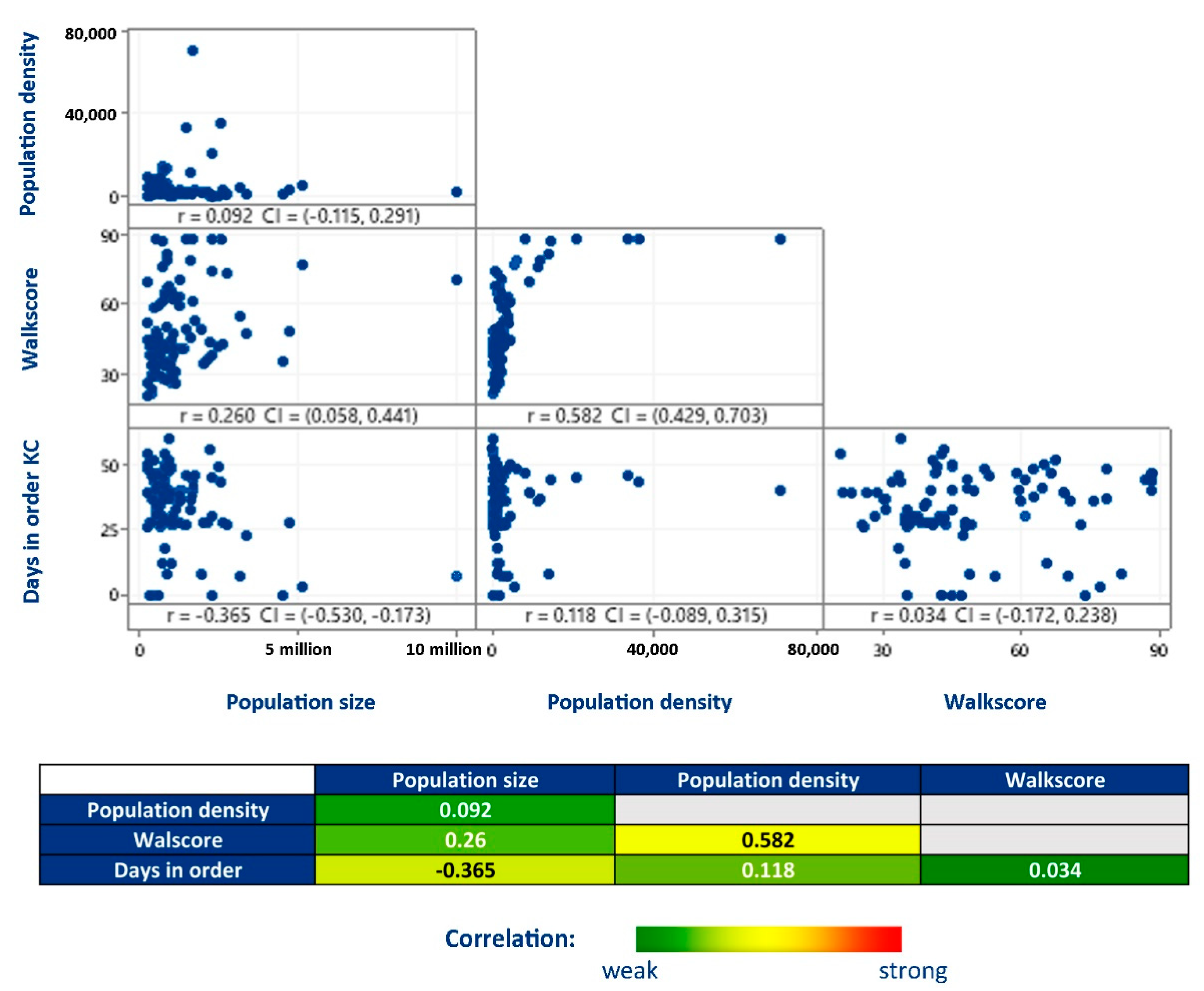
4.1. Correlation Analysis
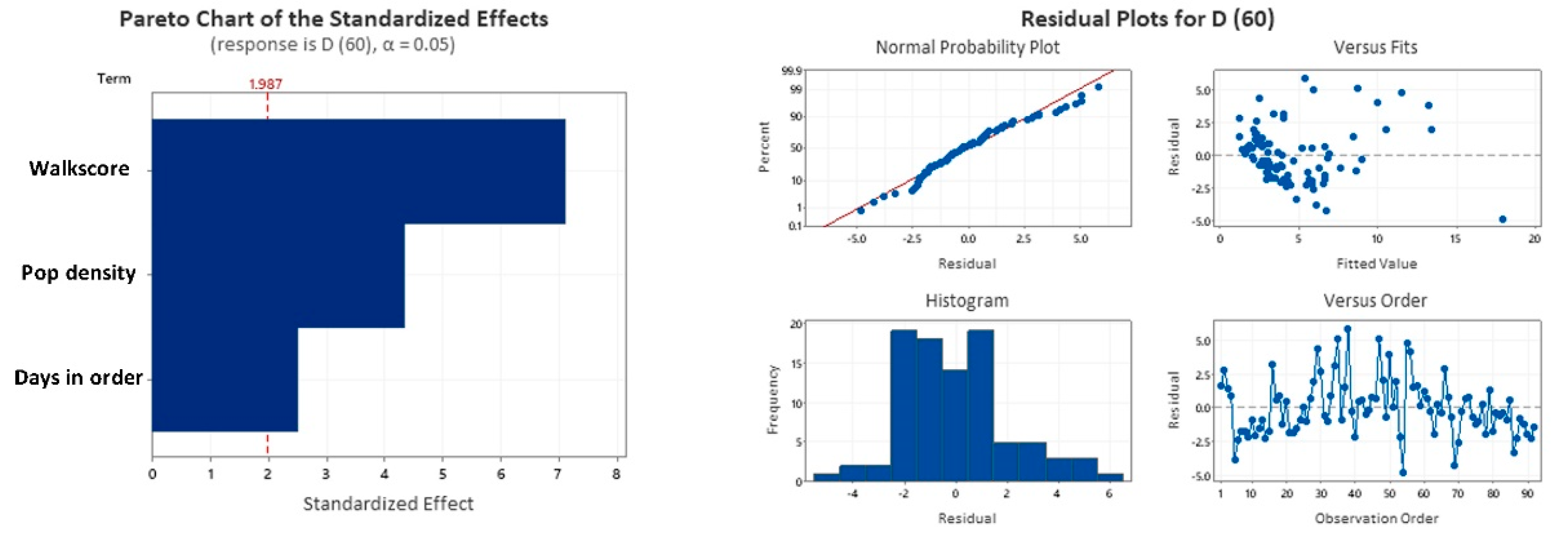
4.2. Best Subsets Regression
4.3. Final Regression Model
4.4. Discussion
5. Final Remarks: Limitations and Further Developments
5.1. Limitations of This Work
5.2. Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andersen, M. Early Evidence on Social Distancing in Response to COVID-19 in the United States; Social Science Research Network: Rochester, NY, USA, 2020. [Google Scholar]
- U.S. Department of Health and Human Services COVID-19 and Your Health. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html (accessed on 7 April 2021).
- Greenstone, M.; Nigam, V. Does Social Distancing Matter? Social Science Research Network: Rochester, NY, USA, 2020. [Google Scholar]
- Lewnard, J.; Lo, N. Scientific and Ethical Basis for Social-Distancing Interventions against COVID-19—The Lancet Infectious Diseases. Lancet 2020, 20, 631–633. [Google Scholar] [CrossRef] [Green Version]
- Alexander, C. A City Is Not a Tree. Archit. Forum 1965, 122, 58–62. [Google Scholar]
- Hillier, B.; Hanson, J. The Social Logic of Space; Cambridge University Press: Cambridge, UK, 1984. [Google Scholar]
- Pflieger, G.; Rozenblat, C. Introduction. Urban Networks and Network Theory: The City as the Connector of Multiple Networks. Urban Stud. 2010, 47, 2723–2735. [Google Scholar] [CrossRef] [Green Version]
- Netto, V.M.; Brigatti, E.; Meirelles, J.; Ribeiro, F.L.; Pace, B.; Cacholas, C.; Sanches, P. Cities, from Information to Interaction. Entropy 2018, 20, 834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batty, M. The Coronavirus Crisis: What Will the Post-Pandemic City Look Like? Environ. Plan. B Urban Anal. City Sci. 2020, 47, 547–552. [Google Scholar] [CrossRef]
- United Nations COVID-19 in an Urban World. Available online: https://www.un.org/en/coronavirus/covid-19-urban-world (accessed on 7 April 2021).
- Farr, D. Sustainable Urbanism: Urban Design With Nature; John Willey and Sons: Hoboken, NJ, USA, 2008. [Google Scholar]
- Gehl, J. Cities for People; Island Press: Washington, DC, USA, 2010. [Google Scholar]
- Lima, F.; Paraízo, R.C.; Kós, J.R. Algorithmic Approach towards Transit-Oriented Development Neighborhoods: (Para)Metric Tools for Evaluating and Proposing Rapid Transit-Based Districts. Int. J. Archit. Comput. 2016, 14, 131–146. [Google Scholar] [CrossRef]
- Lima, F.; Montenegro, N.; Paraizo, R.; Kós, J. Urbanmetrics: An Algorithmic-(Para)Metric Methodology for Analysis and Optimization of Urban Configurations. In Planning Support Science for Smarter Urban Futures; Lecture Notes in Geoinformation and Cartography; Geertman, S., Allan, A., Pettit, C., Stillwell, J., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 47–64. ISBN 978-3-319-57819-4. [Google Scholar]
- Savini, L.; Candeloro, L.; Calistri, P.; Conte, A. A Municipality-Based Approach Using Commuting Census Data to Characterize the Vulnerability to Influenza-Like Epidemic: The COVID-19 Application in Italy. Microorganisms 2020, 8, 911. [Google Scholar] [CrossRef] [PubMed]
- Frank, L.D.; Schmid, T.L.; Sallis, J.F.; Chapman, J.; Saelens, B.E. Linking Objectively Measured Physical Activity with Objectively Measured Urban Form: Findings from SMARTRAQ. Am. J. Prev. Med. 2005, 28, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Buck, C.; Pohlabeln, H.; Huybrechts, I.; De Bourdeaudhuij, I.; Pitsiladis, Y.; Reisch, L.; Pigeot, I. Development and Application of a Moveability Index to Quantify Possibilities for Physical Activity in the Built Environment of Children. Health Place 2011, 17, 1191–1201. [Google Scholar] [CrossRef]
- Dobesova, Z.; Krivka, T. Walkability Index in the Urban Planning: A Case Study in Olomouc City. In Advances in Spatial Planning; Burian, J., Ed.; InTech: Rijeka, Croatia, 2012; pp. 179–196. [Google Scholar]
- Lima, F. Urban metrics: (para)metric system for analysis and optimization of urban configurations. Ph.D. Thesis, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil, 2017. [Google Scholar]
- Brewster, M.; Hurtado, D.; Olson, S.; Yen, J. Walkscore Com: A New Methodology to Explore Associations between Neighborhood Resources, Race, and Health. In Proceedings of the 137th APHA Annual Meeting and Exposition 2009, Philadelphia, PA, USA, 7–11 November 2009. [Google Scholar]
- Walkscore Methodology. Available online: https://www.walkscore.com/methodology.shtml. (accessed on 16 June 2016).
- Carr, L.; Dunsigen, I.; Marcus, B. Validation of Walk Score for Estimating Access to Walkable Amenities. Br. J. Sports Med. 2011, 45, 1144–1158. [Google Scholar] [CrossRef]
- United Nations 68% of the World Population Projected to Live in Urban Areas by 2050, Says UN|UN DESA|United Nations Department of Economic and Social Affairs. Available online: https://www.un.org/development/desa/en/news/population/2018-revision-of-world-urbanization-prospects.html (accessed on 7 April 2021).
- Tarwater, P.M.; Martin, C.F. Effects of Population Density on the Spread of Disease. Complexity 2001, 6, 29–36. [Google Scholar] [CrossRef]
- Hu, H.; Nigmatulina, K.; Eckhoff, P. The Scaling of Contact Rates with Population Density for the Infectious Disease Models. Math. Biosci. 2013, 244, 125–134. [Google Scholar] [CrossRef]
- Kraemer, M.U.G.; Perkins, T.A.; Cummings, D.A.T.; Zakar, R.; Hay, S.I.; Smith, D.L.; Reiner, R.C. Big City, Small World: Density, Contact Rates, and Transmission of Dengue across Pakistan. J. R. Soc. Interface 2015, 12, 20150468. [Google Scholar] [CrossRef] [Green Version]
- Dantzig, G.; Saaty, T. Compact City: A Plan for a Liveable Urban Environment; W. H. Freeman: San Francisco, CA, USA, 1973. [Google Scholar]
- Rogers, R. Cities for a Small Planet; Westview Press: Boulder, CO, USA, 1997. [Google Scholar]
- Chakrabarti, V. A Country of Cities; Metropolis Books: New York, NY, USA, 2013. [Google Scholar]
- Schläpfer, M.; Bettencourt, L.M.A.; Grauwin, S.; Raschke, M.; Claxton, R.; Smoreda, Z.; West, G.B.; Ratti, C. The Scaling of Human Interactions with City Size. J. R. Soc. Interface 2014, 11, 20130789. [Google Scholar] [CrossRef]
- Stier, A.; Berman, M.G.; Bettencourt, L. COVID-19 Attack Rate Increases with City Size; Social Science Research Network: Rochester, NY, USA, 2020. [Google Scholar]
- Liu, L. Emerging Study on the Transmission of the Novel Coronavirus (COVID-19) from Urban Perspective: Evidence from China. Cities 2020, 103, 102759. [Google Scholar] [CrossRef]
- Peng, Z.; Wang, R.; Liu, L.; Wu, H. Exploring Urban Spatial Features of COVID-19 Transmission in Wuhan Based on Social Media Data. ISPRS Int. J. Geo-Inf. 2020, 9, 402. [Google Scholar] [CrossRef]
- Xie, J.; Zhu, Y. Association between Ambient Temperature and COVID-19 Infection in 122 Cities from China. Sci. Total Environ. 2020, 724, 138201. [Google Scholar] [CrossRef] [PubMed]
- Carozzi, F. Urban Density and COVID-19; Social Science Research Network: Rochester, NY, USA, 2020. [Google Scholar]
- Oishi, S.; Cha, Y.; Schimmack, U. The Social Ecology of COVID-19 Cases and Deaths in New York City: The Role of Walkability, Wealth, and Race. Soc. Psychol. Personal. Sci. 2021, 12, 1457–1466. [Google Scholar] [CrossRef]
- Dasgupta, S.; Bowen, V.B.; Leidner, A.; Fletcher, K.; Musial, T.; Rose, C.; Cha, A.; Kang, G.; Dirlikov, E.; Pevzner, E.; et al. Association Between Social Vulnerability and a County’s Risk for Becoming a COVID-19 Hotspot—United States, June 1–July 25, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1535–1541. [Google Scholar] [CrossRef] [PubMed]
- Rocha, R.; Atun, R.; Massuda, A.; Rache, B.; Spinola, P.; Nunes, L.; Lago, M.; Castro, M.C. Effect of Socioeconomic Inequalities and Vulnerabilities on Health-System Preparedness and Response to COVID-19 in Brazil: A Comprehensive Analysis. Lancet Glob. Health 2021, 9, 782–792. [Google Scholar] [CrossRef]
- Subbaraman, N. Why Daily Death Tolls Have Become Unusually Important in Understanding the Coronavirus Pandemic. Available online: https://www.nature.com/articles/d41586-020-01008-1 (accessed on 31 March 2021).
- Kunz, J.; Propper, C. “Does Higher Hospital Quality Save Lives? The Association between” “COVID-19 Deaths and Hospital Quality in the USA; Social Science Research Network: Rochester, NY, USA, 2020. [Google Scholar]
- USAFacts US COVID-19 Cases and Deaths by State|USAFacts. Available online: https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/ (accessed on 7 April 2021).
- NBC news Report: Here Are the Stay-at-Home Orders in Every State. Available online: https://www.nbcnews.com/health/health-news/here-are-stay-home-orders-across-country-n1168736 (accessed on 2 April 2021).
- U.S. Census Census.Gov. Available online: https://www.census.gov/ (accessed on 7 April 2021).
- Hastie, T.; Tibshirani, R.; Tibshirani, R. Best Subset, Forward Stepwise or Lasso? Analysis and Recommendations Based on Extensive Comparisons. Stat. Sci. 2020, 35, 579–592. [Google Scholar] [CrossRef]
- Bertsimas, D.; King, A.; Mazumder, R. Best Subset Selection via a Modern Optimization Lens. Ann. Stat. 2016, 44, 813–852. [Google Scholar] [CrossRef] [Green Version]
- Hofmann, M.; Gatu, C.; Kontoghiorghes, E.J. Efficient Algorithms for Computing the Best Subset Regression Models for Large-Scale Problems. Comput. Stat. Data Anal. 2007, 52, 16–29. [Google Scholar] [CrossRef]
- Zhang, Z. Variable Selection with Stepwise and Best Subset Approaches. Ann. Transl. Med. 2016, 4, 136. [Google Scholar] [CrossRef] [Green Version]
- Kwong, Y.D.; Mehta, K.M.; Miaskowski, C.; Zhuo, H.; Yee, K.; Jauregui, A.; Ke, S.; Deiss, T.; Abbott, J.; Kangelaris, K.N.; et al. Using Best Subset Regression to Identify Clinical Characteristics and Biomarkers Associated with Sepsis-Associated Acute Kidney Injury. Am. J. Physiol.-Ren. Physiol. 2020, 319, F979–F987. [Google Scholar] [CrossRef]
- Ratner, B. The Correlation Coefficient: Its Values Range between +1/−1, or Do They? J. Target. Meas. Anal. Mark. 2009, 17, 139–142. [Google Scholar] [CrossRef] [Green Version]
- Dancey, C.; Reidy, J. Statistics Without Maths for Psychology, 7th ed.; Pearson: London, UK, 2017; ISBN 978-1-292-12888-7. [Google Scholar]
- Burdette, W.J. Planning and Analysis of Clinical Studies; Thomas: New York, NY, USA, 1970. [Google Scholar]
- Arsham, H. Kuiper’s P-Value as a Measuring Tool and Decision Procedure for the Goodness-of-Fit Test. J. Appl. Stat. 1988, 15, 131–135. [Google Scholar] [CrossRef]
- Oraby, T.; Tyshenko, M.G.; Maldonado, J.C.; Vatcheva, K.; Elsaadany, S.; Alali, W.Q.; Longenecker, J.C.; Al-Zoughool, M. Modeling the Effect of Lockdown Timing as a COVID-19 Control Measure in Countries with Differing Social Contacts. Sci. Rep. 2021, 11, 3354. [Google Scholar] [CrossRef]





| Best Subset Regression Results 1—Response Is Know Cases per 100 k hab (after 60 Days from the First Case) | |||||
|---|---|---|---|---|---|
| Vars | R-Sq | R-Sq (adj) | R-Sq (pred) | Mallows Cp | S |
| 1 | 39.2 | 38.5 | 33.7 | 29.1 | 462.24 |
| 1 | 34.8 | 34.1 | 0.0 | 37.4 | 478.43 |
| 2 | 46.9 | 45.7 | 41.0 | 16.1 | 434.22 |
| 2 | 46.9 | 45.7 | 10.9 | 16.2 | 434.36 |
| 3 | 53.0 | 51.4 | 20.1 | 6.5 | 411.03 |
| 3 | 51.7 | 50.0 | 16.9 | 9.0 | 416.65 |
| 4 | 54.8 | 52.7 | 21.8 | 5.0 | 405.32 |
| Vars | PD | WS | DO | PS | |
| 1 | X | ||||
| 1 | X | ||||
| 2 | X | X | |||
| 2 | X | X | |||
| 3 | X | X | X | ||
| 3 | X | X | X | ||
| 4 | X | X | X | X | |
| Best Subset Regression Results 2—Response Is Deaths per 100 k hab (after 60 Days from the First Death) | |||||
|---|---|---|---|---|---|
| Vars | R-Sq | R-Sq (adj) | R-Sq (pred) | Mallows Cp | S |
| 1 | 50.2 | 49.6 | 0.0 | 39.6 | 42.007 |
| 1 | 49.4 | 48.9 | 45.0 | 41.5 | 42.309 |
| 2 | 62.9 | 62.1 | 24.8 | 8.9 | 36.421 |
| 2 | 53.8 | 52.7 | 48.9 | 32.4 | 40.690 |
| 3 | 65.7 | 64.5 | 29.6 | 3.9 | 35.261 |
| 3 | 64.4 | 63.2 | 26.9 | 7.3 | 35.919 |
| 4 | 66.0 | 64.5 | 29.8 | 5.0 | 35.272 |
| Vars | PD | WS | DO | PS | |
| 1 | X | ||||
| 1 | X | ||||
| 2 | X | X | |||
| 2 | X | X | |||
| 3 | X | X | X | ||
| 3 | X | X | X | ||
| 4 | X | X | X | X | |
| Regression Equation | ||||||
| Deaths per 100 k hab^0.5= −2.672 + 0.000130 Population density + 0.1098 Walkscore + 0.0401 Days in order KC | ||||||
| S | R-sq | R-sq(adj) | PRESS | R-sq(pred) | AICc | BIC |
| 2.13467 | 66.01% | 64.85% | 631.932 | 46.44% | 407.22 | 419.13 |
| Term | Coef | S.E. Coef | 95% CI | T-Value | p-Value |
|---|---|---|---|---|---|
| Constant | −2.672 | 0.918 | (−4.496, −0.848) | −2.91 | 0.005 |
| Population density | 0.000130 | 0.000030 | (0.000071, 0.000190) | 4.33 | 0.000 |
| Walkscore | 0.1098 | 0.0155 | (0.0791, 0.1406) | 7.10 | 0.000 |
| Days in order KC | 0.0401 | 0.0160 | (0.0084, 0.0718) | 2.51 | 0.014 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lima, F.T.; Brown, N.C.; Duarte, J.P. Understanding the Impact of Walkability, Population Density, and Population Size on COVID-19 Spread: A Pilot Study of the Early Contagion in the United States. Entropy 2021, 23, 1512. https://doi.org/10.3390/e23111512
Lima FT, Brown NC, Duarte JP. Understanding the Impact of Walkability, Population Density, and Population Size on COVID-19 Spread: A Pilot Study of the Early Contagion in the United States. Entropy. 2021; 23(11):1512. https://doi.org/10.3390/e23111512
Chicago/Turabian StyleLima, Fernando T., Nathan C. Brown, and José P. Duarte. 2021. "Understanding the Impact of Walkability, Population Density, and Population Size on COVID-19 Spread: A Pilot Study of the Early Contagion in the United States" Entropy 23, no. 11: 1512. https://doi.org/10.3390/e23111512
APA StyleLima, F. T., Brown, N. C., & Duarte, J. P. (2021). Understanding the Impact of Walkability, Population Density, and Population Size on COVID-19 Spread: A Pilot Study of the Early Contagion in the United States. Entropy, 23(11), 1512. https://doi.org/10.3390/e23111512







