Cardiovascular Signal Entropy Predicts All-Cause Mortality: Evidence from The Irish Longitudinal Study on Ageing (TILDA)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Cardiovascular Measurements
2.3. Entropy Analysis
2.4. RHR and HRV Analyses
2.5. Mortality Data Linkage
2.6. Covariates
2.7. Statistical Analysis
3. Results
3.1. Participant Characteristics
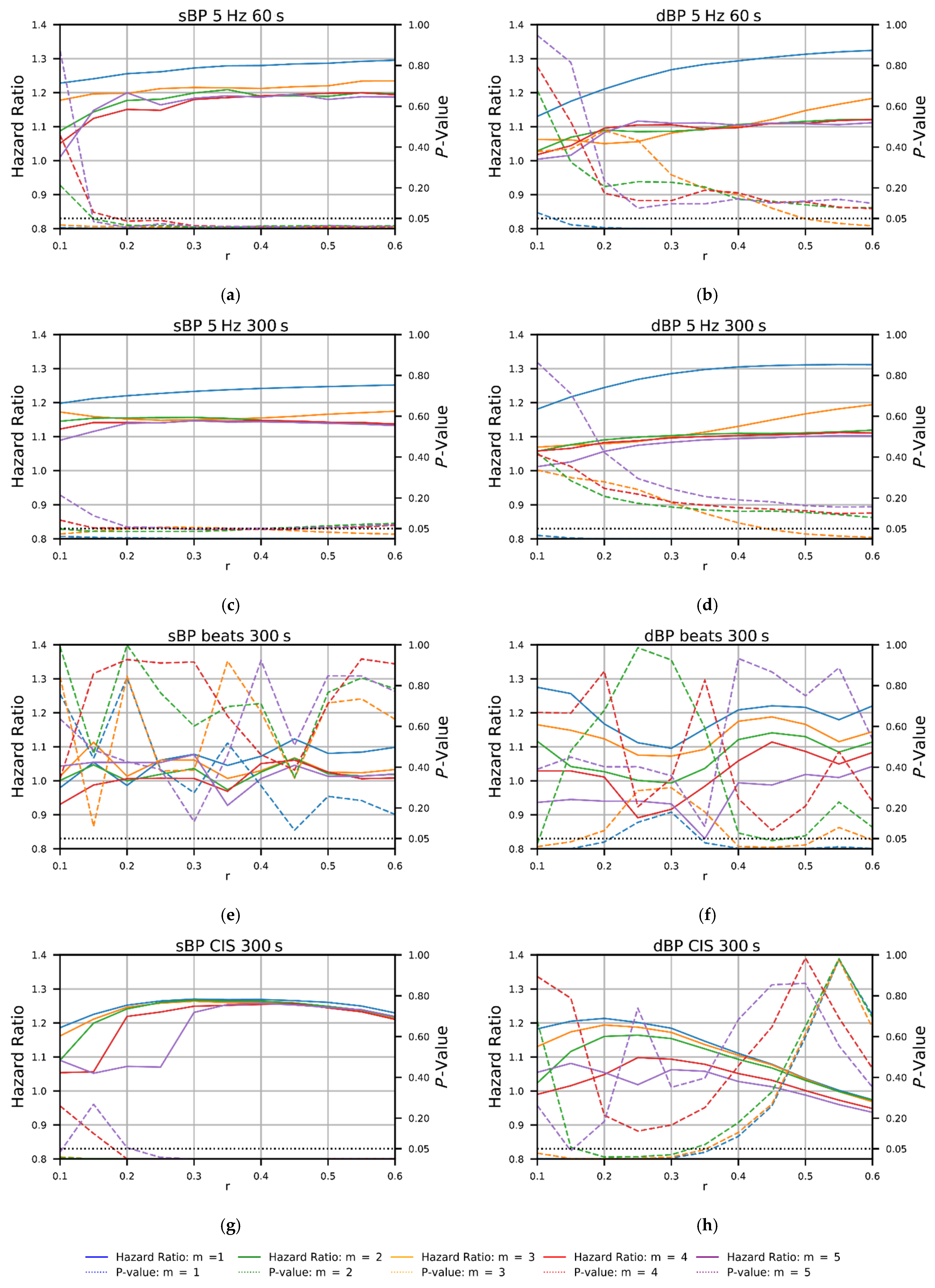
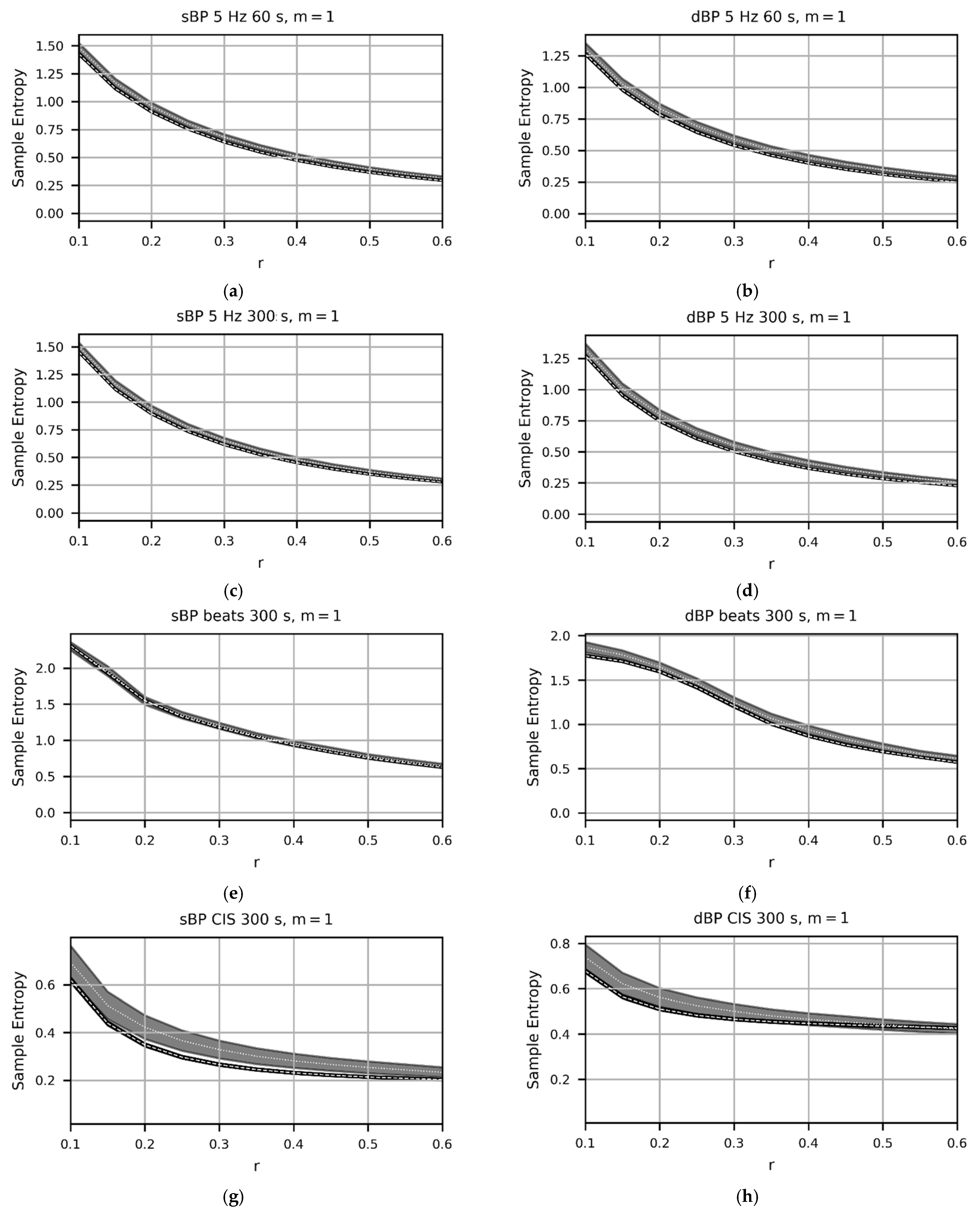
3.2. Effects of ‘m’ and ‘r’ Paramater Choice on Mortality Prediction and Mean SampEn Values
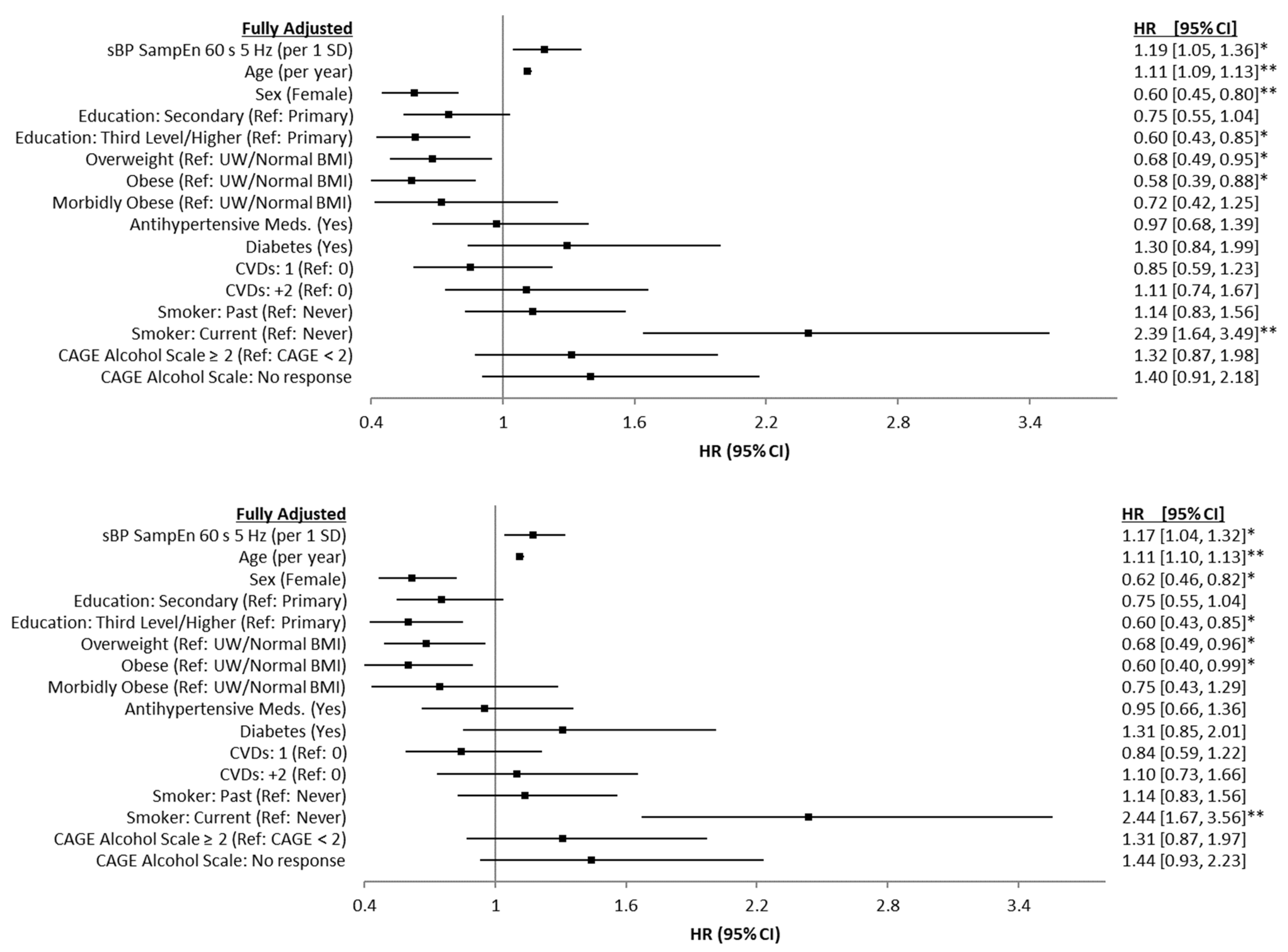
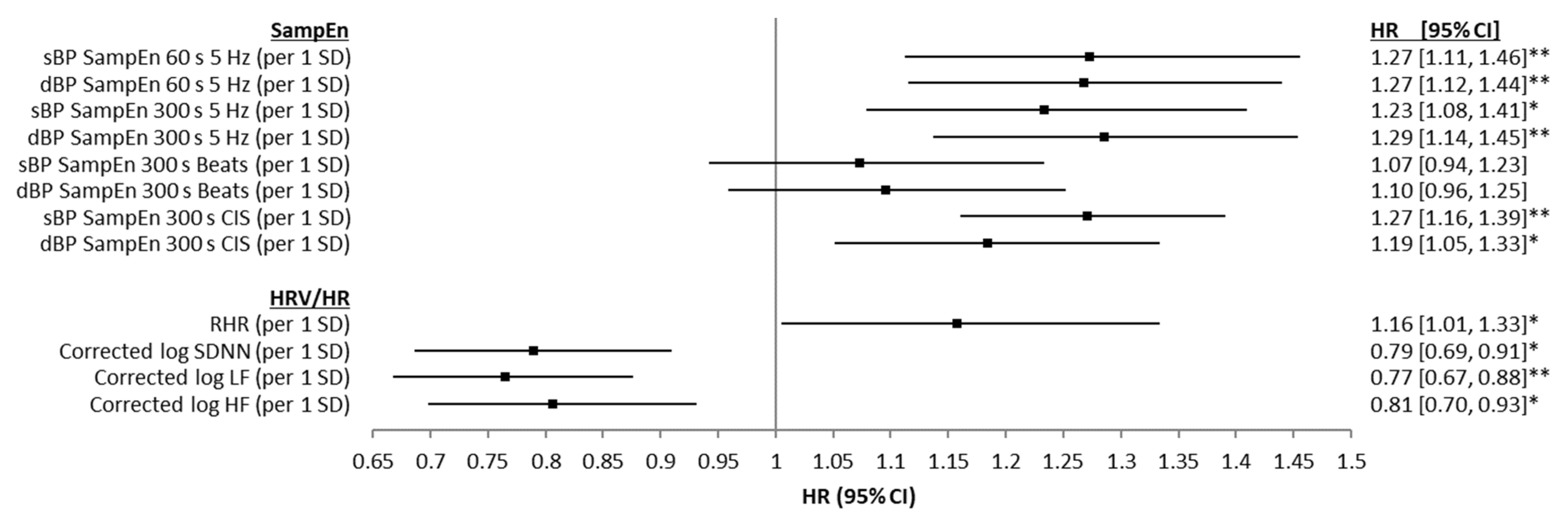
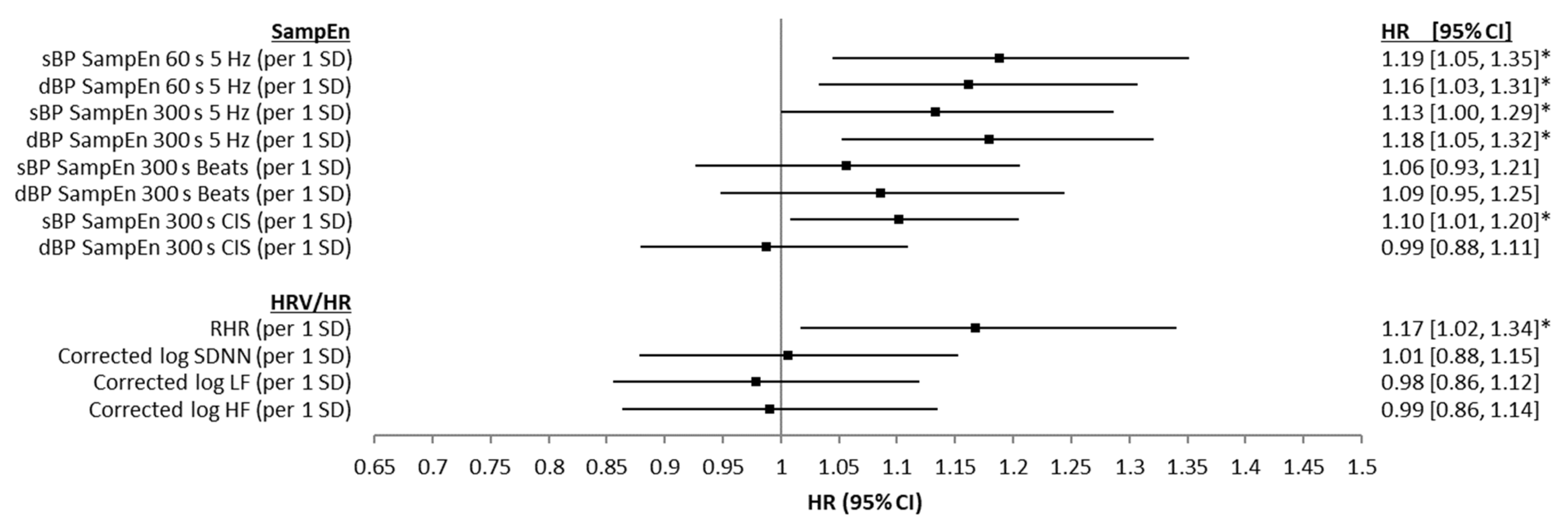
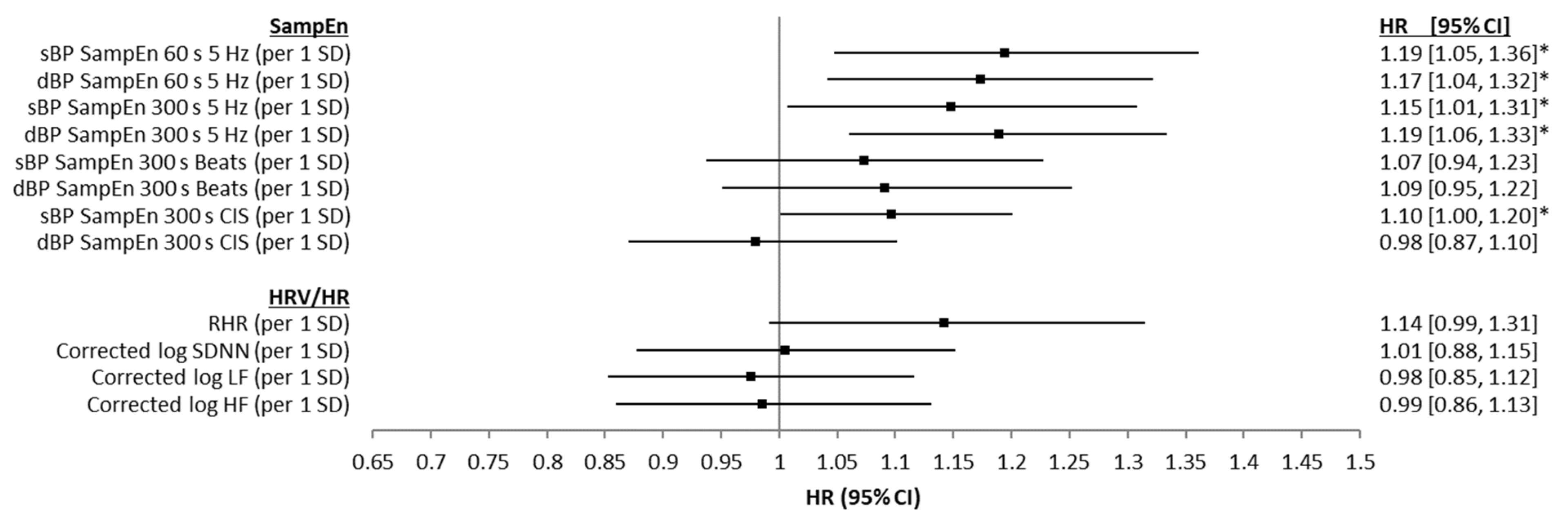
3.3. Associations of Entropy with Mortality Risk
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

Appendix B
References
- He, W.; Goodkind, D.; Kowal, P. An Aging World: 2015; U.S. Census Bureau, U.S. Government Publishing Office: Washington, DC, USA, 2016; Volume P95/16-1.
- Knight, S.P.; Newman, L.; O’Connor, J.D.; Davis, J.; Kenny, R.A.; Romero-Ortuno, R. Associations between Neurocardiovascular Signal Entropy and Physical Frailty. Entropy 2021, 23, 4. [Google Scholar] [CrossRef] [PubMed]
- Knight, S.P.; Newman, L.; Scarlett, S.; O’Connor, J.D.; Davis, J.; De Looze, C.; Kenny, R.A.; Romero-Ortuno, R. Associations between Cardiovascular Signal Entropy and Cognitive Performance over Eight Years. Entropy 2021, 23, 1337. [Google Scholar] [CrossRef] [PubMed]
- Knight, S.; Boyle, R.; Newman, L.; Davis, J.; Rizzo, R.; Duggan, E.; De Looze, C.; Whelan, R.; Kenny, R.A.; Romero-Ortuno, R. Higher neurovascular signal entropy is associated with accelerated brain ageing. Age Ageing 2021, 50 (Suppl. S3), afab219.78. [Google Scholar]
- O’Callaghan, S.; Kenny, R.A. Neurocardiovascular Instability and Cognition. Yale J. Biol. Med. 2016, 89, 59–71. [Google Scholar]
- Romero-Ortuno, R.; Wilson, K.; Hampton, J. Disorders of the Autonomic Nervous System. In Brocklehurst’s Textbook of Geriatric Medicine and Gerontology, 8th ed.; Fillit, H., Rockwood, K., Young, J.B., Eds.; Elsevier: Amsterdam, The Netherlands, 2016; pp. 496–509. [Google Scholar]
- Chon, K.H.; Scully, C.G.; Lu, S. Approximate entropy for all signals. IEEE Eng. Med. Biol. Mag. 2009, 28, 18–23. [Google Scholar] [CrossRef]
- Liu, G.; Xia, Y.; Yang, C.; Zhang, L. The Review of the Major Entropy Methods and Applications in Biomedical Signal Research. In Proceedings of the International Symposium on Bioinformatics Research and Applications (ISBRA), Beijing, China, 8–11 June 2018; Springer: Beijing, China, 2018; pp. 87–100. [Google Scholar]
- Mayer, C.; Bachler, M.; Holzinger, A.; Stein, P.K.; Wassertheurer, S. The effect of threshold values and weighting factors on the association between entropy measures and mortality after myocardial infarction in the cardiac arrhythmia suppression trial (CAST). Entropy 2016, 18, 129. [Google Scholar] [CrossRef] [Green Version]
- Costa, M.; Goldberger, A.L.; Peng, C.K. Multiscale entropy analysis of complex physiologic time series. Phys. Rev. Lett. 2002, 89, 68102. [Google Scholar] [CrossRef] [Green Version]
- Richman, J.S.; Moorman, J.R. Physiological time-series analysis using approximate entropy and sample entropy. Am. J. Physiol. Heart Circ. Physiol. 2000, 278, H2039–H2049. [Google Scholar] [CrossRef] [Green Version]
- Gow, B.J.; Peng, C.-K.; Wayne, P.M.; Ahn, A.C. Multiscale Entropy Analysis of Center-of-Pressure Dynamics in Human Postural Control: Methodological Considerations. Entropy 2015, 17, 7926–7947. [Google Scholar] [CrossRef]
- Bajić, D.; Japundžić-Žigon, N. On Quantization Errors in Approximate and Sample Entropy. Entropy 2022, 24, 73. [Google Scholar] [CrossRef]
- Liu, C.; Gao, R. Multiscale Entropy Analysis of the Differential RR Interval Time Series Signal and Its Application in Detecting Congestive Heart Failure. Entropy 2017, 19, 251. [Google Scholar] [CrossRef] [Green Version]
- Sykora, M.; Szabo, J.; Siarnik, P.; Turcani, P.; Krebs, S.; Lang, W.; Czosnyka, M.; Smielewski, P. Heart rate entropy is associated with mortality after intracereberal hemorrhage. J. Neurol. Sci. 2020, 418, 117033. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Sen, A.; ó’Hartaigh, B.; Janszky, I.; Romundstad, P.R.; Tonstad, S.; Vatten, L.J. Resting heart rate and the risk of cardiovascular disease, total cancer, and all-cause mortality–A systematic review and dose–response meta-analysis of prospective studies. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 504–517. [Google Scholar] [CrossRef] [PubMed]
- Hartaigh, B.ó.; Allore, H.G.; Trentalange, M.; McAvay, G.; Pilz, S.; Dodson, J.A.; Gill, T.M. Elevations in time-varying resting heart rate predict subsequent all-cause mortality in older adults. Eur. J. Prev. Cardiol. 2020, 22, 527–534. [Google Scholar] [CrossRef]
- Sen, J.; McGill, D. Fractal analysis of heart rate variability as a predictor of mortality: A systematic review and meta-analysis. Chaos Interdiscip. J. Nonlinear Sci. 2018, 28, 072101. [Google Scholar] [CrossRef]
- Villareal, R.P.; Liu, B.C.; Massumi, A. Heart rate variability and cardiovascular mortality. Curr. Atheroscler. Rep. 2002, 4, 120–127. [Google Scholar] [CrossRef]
- Donoghue, O.A.; McGarrigle, C.A.; Foley, M.; Fagan, A.; Meaney, J.; Kenny, R.A. Cohort Profile Update: The Irish Longitudinal Study on Ageing (TILDA). Int. J. Epidemiol. 2018, 47, 1398–1398l. [Google Scholar] [CrossRef]
- Kearney, P.M.; Cronin, H.; O’Regan, C.; Kamiya, Y.; Savva, G.M.; Whelan, B.; Kenny, R. Cohort profile: The Irish Longitudinal Study on Ageing. Int. J. Epidemiol. 2011, 40, 877–884. [Google Scholar] [CrossRef]
- Tarvainen, M.P.; Ranta-Aho, P.O.; Karjalainen, P.A. An advanced detrending method with application to HRV analysis. IEEE Trans. Biomed. Eng. 2002, 49, 172–175. [Google Scholar] [CrossRef]
- Martínez-Cagigal, V. Sample Entropy. Available online: https://uk.mathworks.com/matlabcentral/fileexchange/69381-sample-entropy (accessed on 10 January 2020).
- Pardey, J.; Jouravleva, S. The Next-Generation Holter Revolution: From Analyse-Edit-Print to Analyse-Print. In Proceedings of the Computers in Cardiology, Chicago, IL, USA, 19–22 September 2004; pp. 373–376. [Google Scholar]
- Camm, A.J.; Kirchhof, P.; Lip, G.Y.; Schotten, U.; Savelieva, I.; Ernst, S.; Van Gelder, I.C.; Al-Attar, N.; Hindricks, G.; Prendergast, B.; et al. Guidelines for the management of atrial fibrillation: The Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur. Heart J. 2010, 31, 2369–2429. [Google Scholar]
- Sacha, J. Interaction between Heart Rate and Heart Rate Variability. Ann. Noninvasive Electrocardiol. 2014, 19, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Ward, M.; May, P.; Briggs, R.; McNicholas, T.; Normand, C.; Kenny, R.; Nolan, A. Linking death registration and survey data: Procedures and cohort profile for The Irish Longitudinal Study on Ageing (TILDA) [version 2; peer review: 3 approved]. HRB Open Res. 2020, 3, 43. [Google Scholar] [PubMed]
- Ewing, J.A. Detecting alcoholism. The CAGE questionnaire. Jama 1984, 252, 1905–1907. [Google Scholar] [CrossRef] [PubMed]
- Bhaskaran, K.; Dos-Santos-Silva, I.; Leon, D.A.; Douglas, I.J.; Smeeth, L. Association of BMI with overall and cause-specific mortality: A population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018, 6, 944–953. [Google Scholar] [CrossRef] [Green Version]
- WHO Physical Status. Physical status: The use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ. Tech. Rep. Ser. 1995, 854, 1–452. [Google Scholar]
- Brown, A.M.; Ransom, B.R. Astrocyte glycogen and brain energy metabolism. Glia 2007, 55, 1263–1271. [Google Scholar] [CrossRef]
- Koepchen, H.P. Physiology of Rhythms and Control Systems: An Integrative Approach; Springer: Berlin/Heidelberg, Germany, 1991; pp. 3–20. [Google Scholar]
- Porta, A.; Castiglioni, P.; Rienzo, M.D.; Bari, V.; Bassani, T.; Marchi, A.; Takahashi, A.C.M.; Tobaldini, E.; Montano, N.; Catai, A.M.; et al. Short-term complexity indexes of heart period and systolic arterial pressure variabilities provide complementary information. J. Appl. Physiol. 2012, 113, 1810–1820. [Google Scholar] [CrossRef] [Green Version]
- Buckles, K.; Hagemann, A.; Malamud, O.; Morrill, M.; Wozniak, A. The effect of college education on mortality. J. Health Econ. 2016, 50, 99–114. [Google Scholar] [CrossRef]
- Case, A.; Paxson, C. Sex differences in morbidity and mortality. Demography 2005, 42, 189–214. [Google Scholar] [CrossRef] [Green Version]
- Moguilner, S.; Knight, S.P.; Davis, J.R.C.; O’Halloran, A.M.; Kenny, R.A.; Romero-Ortuno, R. The Importance of Age in the Prediction of Mortality by a Frailty Index: A Machine Learning Approach in the Irish Longitudinal Study on Ageing. Geriatrics 2021, 6, 84. [Google Scholar] [CrossRef]
- Peto, R.; Lopez, A.D.; Boreham, J.; Thun, M.; Heath, C., Jr.; Doll, R. Mortality from smoking worldwidea. Br. Med. Bull. 1996, 52, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M.; Kit, B.K.; Orpana, H.; Graubard, B.I. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 2013, 309, 71–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Full Cohort (n = 4543) | Non-Deceased (n = 4329) | Deceased (n = 214) | p | |
|---|---|---|---|---|
| Age [years] | 61.9 (SD: 8.4, range: [50–91]) | 61.5 (SD: 8.2, range: [50–90]) | 70.0 (SD: 9.0, range: [50–91]) | ≤0.001 |
| Sex [% (n)] | Female: 54.1% (2458) | Female: 54.8% (2371) | Female: 40.7% (87) | ≤0.001 |
| Education [% (n)] | ≤0.001 | |||
| Primary/None | 21.5% (977) | 20.7% (895) | 38.3% (82) | |
| Secondary | 41.6% (1890) | 41.9% (1814) | 29.3% (76) | |
| Third/Higher | 36.9% (1676) | 37.4% (1620) | 26.2% (56) | |
| Body Mass Index (BMI) [% (n)] | 0.248 | |||
| Underweight/Normal BMI | 22.9% (1041) | 22.7% (980) | 28.5% (61) | |
| Overweight | 44.0% (1997) | 44.0% (1908) | 41.6% (89) | |
| Obese | 23.9% (1086) | 24.0% (1041) | 21.0% (45) | |
| Morbidly Obese | 9.2% (419) | 9.3% (400) | 8.9% (19) | |
| Antihypertensive Medication Use [% (n)] | 33.1% (1503) | 32.4% (1401) | 47.7% (102) | ≤0.001 |
| Self-reported diabetic [%] | 6.5% (295) | 6.2% (269) | 12.2% (26) | 0.001 |
| Number of Cardiovascular Conditions [% (n)] | ≤0.001 | |||
| 0 | 39.3% (1786) | 39.6% (1715) | 33.2% (71) | |
| 1 | 34.2% (1555) | 34.5% (1494) | 28.5% (61) | |
| 2+ | 26.5% (1202) | 25.9% (1120) | 38.3% (82) | |
| Smoker [% (n)] | ≤0.001 | |||
| Never | 45.9% (2084) | 46.4% (2010) | 34.6% (74) | |
| Past | 39.2% (1784) | 39.1% (1693) | 42.5% (91) | |
| Current | 14.9% (675) | 14.5% (626) | 22.9% (49) | |
| CAGE Alcohol Scale | 0.461 | |||
| CAGE < 2 | 78.1% (3550) | 78.3% (3389) | 75.2% (161) | |
| CAGE ≥ 2 | 12.9% (584) | 12.8% (555) | 13.6% (29) | |
| No response | 9.0% (409) | 8.9% (385) | 11.2% (24) | |
| SampEn sBP* (60 s 5 Hz) | 0.641 (SD: 0.179, range: [0.022–1.254]) | 0.639 (SD: 0.178, range: [0.022–1.178]) | 0.682 (SD: 0.190, range: [0.135–1.254]) | ≤0.001 |
| SampEn dBP * (60 s 5 Hz) | 0.543 (SD: 0.189, range: [0.024–1.414]) | 0.540 (SD: 0.187, range: [0.024–1.414]) | 0.588 (SD: 0.220, range: [0.058–1.227]) | ≤0.001 |
| SampEn sBP * (300 s 5 Hz) | 0.618 (SD: 0.169, range: [0.074–1.228]) | 0.616 (SD: 0.168, range: [0.074–1.206]) | 0.652 (SD: 0.184, range: [0.178–1.228]) | 0.002 |
| SampEn dBP * (300 s 5 Hz) | 0.505 (SD: 0.176, range: [0.052–1.328]) | 0.502 (SD: 0.173, range: [0.052–1.328]) | 0.551 (SD: 0.214, range: [0.138–1.253]) | ≤0.001 |
| SampEn sBP * (300 s Beats) | 1.179 (SD: 0.291, range: [0.001–2.294]) | 1.178 (SD: 0.290, range: [0.001–2.294]) | 1.201 (SD: 0.312, range: [0.239–1.878]) | 0.272 |
| SampEn dBP * (300 s Beats) | 1.207 (SD: 0.435, range: [0.001–2.367]) | 1.205 (SD: 0.435, range: [0.001–2.367]) | 1.246 (SD: 0.434, range: [0.368–2.266]) | 0.179 |
| SampEn sBP * (300 s CIS) | 0.268 (SD: 0.174, range: [0.001–1.594]) | 0.265 (SD: 0.166, range: [0.001–1.594]) | 0.329 (SD: 0.278, range: [0.076–1.568]) | ≤0.001 |
| SampEn dBP * (300 s CIS) | 0.468 (SD: 0.177, range: [0.001–1.534]) | 0.466 (SD: 0.173, range: [0.001–1.534]) | 0.501 (SD: 0.239, range: [0.128–1.526]) | 0.005 |
| RHR [bpm] | 64.0 (SD: 10.1, range: [37.6–117.2]) | 63.9 (SD: 9.9, range: [37.6–111.7]) | 65.4 (SD: 12.3, range: [40.8–117.2]) | 0.047 |
| HRV SDNN ** [ms] | 37.8 (SD: 17.8, range: [1.8–164.9]) | 37.9 (SD: 17.8, range: [1.8–164.9]) | 34.2 (SD: 16.5, range: [3.1–108.2]) | 0.006 |
| HRV LF ** [ms2] | 427.9 (SD: 579.3, range: [0.2–9152.3]) | 431.8 (SD: 582.8, range: [0.5–9152.3]) | 340.9 (SD: 486.8, range: [0.2–3734.5]) | 0.041 |
| HRV HF ** [ms2] | 218.8 (SD: 310.5, range: [0.5–4109.5]) | 219.8 (SD: 311.7, range: [0.5–4109.5]) | 196.1 (SD: 282.4, range: [1.2–1994.4]) | 0.318 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knight, S.P.; Ward, M.; Newman, L.; Davis, J.; Duggan, E.; Kenny, R.A.; Romero-Ortuno, R. Cardiovascular Signal Entropy Predicts All-Cause Mortality: Evidence from The Irish Longitudinal Study on Ageing (TILDA). Entropy 2022, 24, 676. https://doi.org/10.3390/e24050676
Knight SP, Ward M, Newman L, Davis J, Duggan E, Kenny RA, Romero-Ortuno R. Cardiovascular Signal Entropy Predicts All-Cause Mortality: Evidence from The Irish Longitudinal Study on Ageing (TILDA). Entropy. 2022; 24(5):676. https://doi.org/10.3390/e24050676
Chicago/Turabian StyleKnight, Silvin P., Mark Ward, Louise Newman, James Davis, Eoin Duggan, Rose Anne Kenny, and Roman Romero-Ortuno. 2022. "Cardiovascular Signal Entropy Predicts All-Cause Mortality: Evidence from The Irish Longitudinal Study on Ageing (TILDA)" Entropy 24, no. 5: 676. https://doi.org/10.3390/e24050676
APA StyleKnight, S. P., Ward, M., Newman, L., Davis, J., Duggan, E., Kenny, R. A., & Romero-Ortuno, R. (2022). Cardiovascular Signal Entropy Predicts All-Cause Mortality: Evidence from The Irish Longitudinal Study on Ageing (TILDA). Entropy, 24(5), 676. https://doi.org/10.3390/e24050676










