The Role of Structural Inequality on COVID-19 Incidence Rates at the Neighborhood Scale in Urban Areas
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Timeline
2.2. Data Sources
2.3. Statistical Methods
3. Results
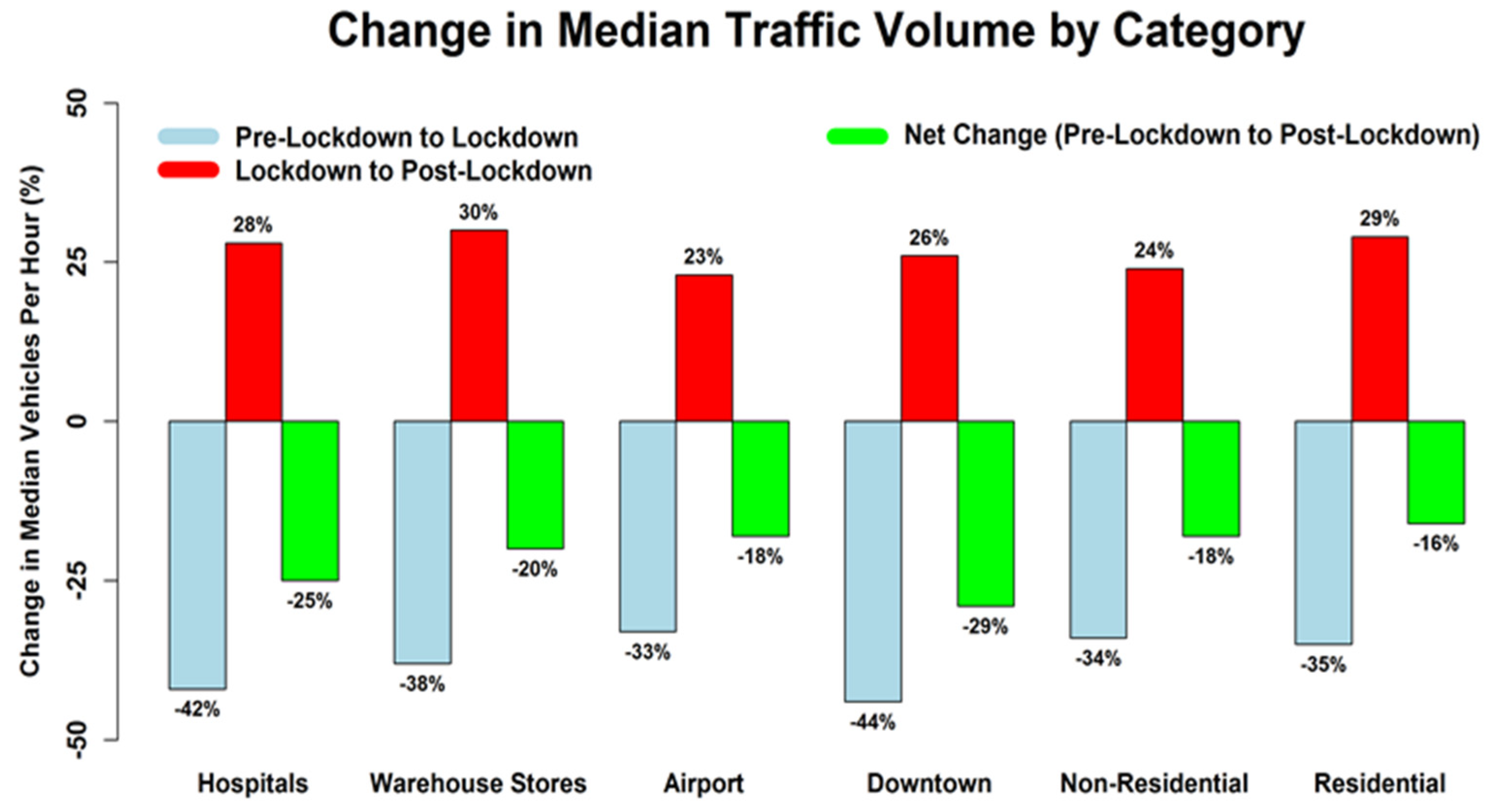
3.1. Proposition 1: Do Social Distancing Policies Keep People at Home (or Impact Mobility) as Intended?
3.2. Proposition 2: Do Stay-at-Home Orders Benefit All Populations Equally?
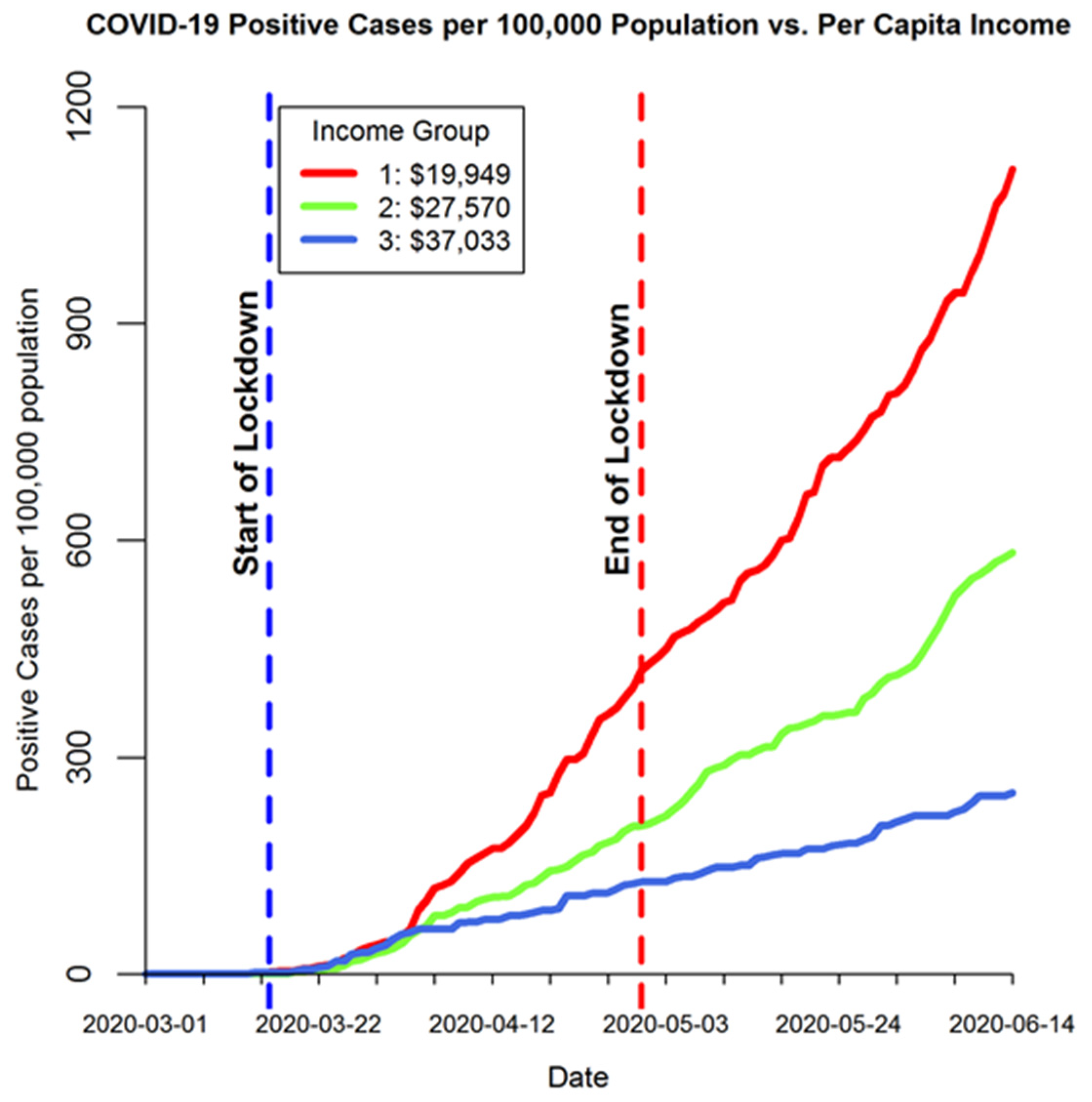
3.3. Proposition 3: Do All Groups Have Similar COVID-19 Incidence Rates?
4. Discussion
4.1. Implications
4.2. Limitations
4.3. Implications for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix A.1. Zip Code Data
Appendix A.2. Sociodemographic Data
Appendix A.3. Traffic Count Data
Appendix A.4. COVID-19 Confirmed Cases Data
| ZIP Code | Income Group | Per Capita Income (Low to High) (USD) | Percent White Group | Percent White Population | White-Collar Group | Percent White-Collar | Pre-Lockdown Vehicles per Hour (VPH) | Lockdown Vehicle per Hour (VPH) | Post-Lockdown Vehicles per Hour (VPH) |
|---|---|---|---|---|---|---|---|---|---|
| 84104 | 1 | 14,534 | 1 | 50.13 | 1 | 43.19 | 1200 | 1020 | 1177 |
| 84116 | 1 | 16,302 | 1 | 50.65 | 1 | 44.21 | 1462 | 1012 | 1225 |
| 84119 | 1 | 18,911 | 1 | 58.27 | 1 | 46.19 | 361 | 241 | 284 |
| 84115 | 1 | 19,797 | 1 | 63.24 | 1 | 56.96 | 698 | 492 | 609 |
| 84120 | 1 | 19,807 | 1 | 57.93 | 1 | 47.85 | 1159 | 865 | 1021 |
| 84118 | 1 | 19,949 | 1 | 64.09 | 1 | 51.85 | 453 | 357 | 409 |
| 84044 | 1 | 20,443 | 1 | 74.48 | 1 | 50.44 | 970 | 757 | 856 |
| 84128 | 1 | 20,502 | 1 | 59.98 | 1 | 50.07 | 74 | 51 | 71 |
| 84111 | 1 | 23,069 | 1 | 75.00 | 2 | 68.99 | 669 | 342 | 380 |
| 84123 | 1 | 23,296 | 1 | 74.76 | 2 | 60.59 | 976 | 713 | 829 |
| 84088 | 1 | 23,611 | 2 | 78.79 | 1 | 59.91 | 1678 | 1186 | 1487 |
| 84129 | 2 | 23,834 | 1 | 74.48 | 1 | 56.46 | 830 | 591 | 704 |
| 84084 | 2 | 24,260 | 2 | 77.02 | 1 | 59.4 | 1816 | 1191 | 1235 |
| 84081 | 2 | 24,554 | 2 | 77.91 | 2 | 62.7 | 1413 | 994 | 1288 |
| 84107 | 2 | 25,396 | 2 | 79.40 | 2 | 63.11 | 1508 | 917 | 1196 |
| 84102 | 2 | 26,141 | 2 | 80.45 | 3 | 73.42 | 313 | 183 | 226 |
| 84047 | 2 | 26,417 | 2 | 75.83 | 2 | 65.36 | 54 | 42 | 53 |
| 84096 | 2 | 28,722 | 3 | 90.66 | 2 | 73.25 | 1125 | 851 | 1149 |
| 84070 | 2 | 28,849 | 2 | 82.41 | 2 | 66.24 | 1378 | 864 | 1093 |
| 84065 | 2 | 29,558 | 3 | 92.55 | 2 | 70.72 | 1143 | 845 | 1270 |
| 84094 | 2 | 30,528 | 3 | 87.73 | 2 | 72.48 | 1056 | 633 | 843 |
| 84101 | 2 | 30,600 | 2 | 77.67 | 2 | 68.77 | 870 | 419 | 564 |
| 84106 | 2 | 31,440 | 2 | 83.93 | 2 | 72.61 | 890 | 450 | 754 |
| 84095 | 3 | 33,995 | 3 | 89.28 | 3 | 77.48 | 790 | 466 | 650 |
| 84124 | 3 | 35,433 | 3 | 89.19 | 3 | 77.15 | 1036 | 679 | 971 |
| 84109 | 3 | 36,024 | 3 | 89.74 | 3 | 76.78 | 1036 | 679 | 971 |
| 84103 | 3 | 36,325 | 2 | 85.41 | 3 | 76.45 | 580 | 335 | 403 |
| 84020 | 3 | 36,443 | 3 | 88.78 | 3 | 79.33 | 876 | 619 | 832 |
| 84093 | 3 | 37,033 | 3 | 90.73 | 3 | 76.52 | 1386 | 885 | 1154 |
| 84121 | 3 | 37,328 | 3 | 89.63 | 3 | 74.85 | 478 | 275 | 375 |
| 84117 | 3 | 38,282 | 2 | 87.65 | 2 | 72.71 | 1304 | 750 | 1121 |
| 84092 | 3 | 39,177 | 3 | 90.84 | 3 | 77.12 | 425 | 298 | 405 |
| 84105 | 3 | 39,472 | 3 | 88.76 | 3 | 76.65 | 794 | 477 | 698 |
| 84108 | 3 | 43,068 | 2 | 85.77 | 3 | 84.89 | 380 | 127 | 136 |
| Metric | Group | Mean | Traffic Counts (VPH) | Traffic Change (%) | |||
|---|---|---|---|---|---|---|---|
| Pre- Lockdown | Lockdown | Post-Lockdown | Pre-Lockdown to Lockdown | Lockdown to Post-Lockdown | |||
| Income (USD) | 1 | 20,020 | 882 | 640 | 759 | −28.48 | 19.61 |
| 2 | 27,525 | 1033 | 665 | 865 | −35.41 | 31.64 | |
| 3 | 37,507 | 826 | 508 | 701 | −39.91 | 35.07 | |
| Percent White | 1 | 63.91% | 805 | 586 | 688 | −28.43 | 19.04 |
| 2 | 81.02% | 1015 | 622 | 796 | −40.52 | 28.69 | |
| 3 | 89.81% | 922 | 610 | 847 | −34.38 | 38.85 | |
| Percent White Collar | 1 | 51.50% | 973 | 706 | 825 | −27.33 | 19.20 |
| 2 | 68.13% | 1032 | 652 | 878 | −36.54 | 34.18 | |
| 3 | 77.33% | 736 | 457 | 620 | −39.82 | 32.71 | |

References
- Ferguson, N.M.; Laydon, D.; Nedjati-Gilani, G.; Imai, N.; Ainslie, K.; Baguelin, M.; Bhatia, S.; Boonyasiri, A.; Cucunubá, Z.; Cuomo-Dannenburg, G. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. Imp. Coll. Lond. 2020, 10, 77482. [Google Scholar] [CrossRef]
- Van Bavel, J.J.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- McKibbin, W.J.; Fernando, R. The global macroeconomic impacts of COVID-19: Seven scenarios. Asian Econ. Pap. 2021, 20, 1–30. [Google Scholar] [CrossRef]
- Gross, C.P.; Essien, U.R.; Pasha, S.; Gross, J.R.; Wang, S.-Y.; Nunez-Smith, M. Racial and Ethnic Disparities in Population Level Covid-19 Mortality. MedRxiv 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- Chin, V.; Ioannidis, J.P.; Tanner, M.A.; Cripps, S. Effect estimates of COVID-19 non-pharmaceutical interventions are non-robust and highly model-dependent. J. Clin. Epidemiol. 2021, 136, 96–132. [Google Scholar] [CrossRef]
- De Larochelambert, Q.; Marc, A.; Antero, J.; Le Bourg, E.; Toussaint, J.-F. Covid-19 mortality: A matter of vulnerability among nations facing limited margins of adaptation. Front. Public Health 2020, 8, 782. [Google Scholar] [CrossRef] [PubMed]
- Savaris, R.F.; Pumi, G.; Dalzochio, J.; Kunst, R. Stay-at-home policy is a case of exception fallacy: An internet-based ecological study. Sci. Rep. 2021, 11, 5313. [Google Scholar] [CrossRef]
- Townsend, M.J.; Kyle, T.K.; Stanford, F.C. Outcomes of COVID-19: Disparities in Obesity and by Ethnicity/Race; Nature Publishing Group: New York, NY, USA, 2020. [Google Scholar]
- Kirby, T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir. Med. 2020, 8, 547–548. [Google Scholar] [CrossRef]
- Rentsch, C.T.; Kidwai-Khan, F.; Tate, J.P.; Park, L.S.; King, J.T., Jr.; Skanderson, M.; Hauser, R.G.; Schultze, A.; Jarvis, C.I.; Holodniy, M. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: A nationwide cohort study. PLoS Med. 2020, 17, e1003379. [Google Scholar] [CrossRef]
- Mahajan, U.V.; Larkins-Pettigrew, M. Racial demographics and COVID-19 confirmed cases and deaths: A correlational analysis of 2886 US counties. J. Public Health 2020, 42, 445–447. [Google Scholar] [CrossRef]
- Adhikari, S.; Pantaleo, N.P.; Feldman, J.M.; Ogedegbe, O.; Thorpe, L.; Troxel, A.B. Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US metropolitan areas. JAMA Netw. Open 2020, 3, e2016938. [Google Scholar] [CrossRef]
- Rodriguez-Diaz, C.E.; Guilamo-Ramos, V.; Mena, L.; Hall, E.; Honermann, B.; Crowley, J.S.; Baral, S.; Prado, G.J.; Marzan-Rodriguez, M.; Beyrer, C. Risk for COVID-19 infection and death among Latinos in the United States: Examining heterogeneity in transmission dynamics. Ann. Epidemiol. 2020, 52, 46–53.e42. [Google Scholar] [CrossRef]
- Khazanchi, R.; Evans, C.T.; Marcelin, J.R. Racism, not race, drives inequity across the COVID-19 continuum. JAMA Netw. Open 2020, 3, e2019933. [Google Scholar] [CrossRef]
- Louis-Jean, J.; Cenat, K.; Njoku, C.V.; Angelo, J.; Sanon, D. Coronavirus (COVID-19) and racial disparities: A perspective analysis. J. Racial Ethn. Health Disparities 2020, 7, 1039–1045. [Google Scholar] [CrossRef]
- van Ingen, T.; Brown, K.A.; Buchan, S.A.; Akingbola, S.; Daneman, N.; Smith, B.T. Neighbourhood-level risk factors of COVID-19 incidence and mortality. medRxiv 2021. [Google Scholar] [CrossRef]
- Iacobucci, G. Covid-19: Increased risk among ethnic minorities is largely due to poverty and social disparities, review finds. BMJ Br. Med. J. Online 2020, 371, m4099. [Google Scholar] [CrossRef]
- Haug, N.; Geyrhofer, L.; Londei, A.; Dervic, E.; Desvars-Larrive, A.; Loreto, V.; Pinior, B.; Thurner, S.; Klimek, P. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat. Hum. Behav. 2020, 4, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- Turner-Musa, J.; Ajayi, O.; Kemp, L. Examining social determinants of health, stigma, and COVID-19 disparities. Healthcare 2020, 8, 168. [Google Scholar] [CrossRef]
- Bilal, U.; Tabb, L.P.; Barber, S.S.; Roux, A.V.D. Spatial Inequities in COVID-19 Testing, Positivity, Confirmed Cases, and Mortality in 3 U.S. Cities. Ann. Intern. Med. 2021, 174, 936–944. [Google Scholar] [CrossRef] [PubMed]
- Liao, T.F.; De Maio, F. Association of Social and Economic Inequality with Coronavirus Disease 2019 Incidence and Mortality Across US Counties. JAMA Netw. Open 2021, 4, e2034578. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.M.; Harden, S.R.; Sugg, M.M.; Runkle, J.D.; Lundquist, T.E. Analyzing the spatial determinants of local Covid-19 transmission in the United States. Sci. Total Environ. 2021, 754, 142396. [Google Scholar] [CrossRef]
- Muñoz-Price, L.S.; Nattinger, A.B.; Rivera, F.; Hanson, R.; Gmehlin, C.G.; Perez, A.; Singh, S.; Buchan, B.W.; Ledeboer, N.A.; Pezzin, L.E. Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Netw. Open 2020, 3, e2021892. [Google Scholar] [CrossRef]
- Killerby, M.E.; Link-Gelles, R.; Haight, S.C.; Schrodt, C.A.; England, L.; Gomes, D.J.; Shamout, M.; Pettrone, K.; O’Laughlin, K.; Kimball, A. Characteristics associated with hospitalization among patients with COVID-19—Metropolitan Atlanta, Georgia, March–April 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 790. [Google Scholar] [CrossRef]
- Gold, J.A. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19—Georgia, March 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Price-Haywood, E.G.; Burton, J.; Fort, D.; Seoane, L. Hospitalization and mortality among black patients and white patients with Covid-19. N. Engl. J. Med. 2020, 382, 2534–2543. [Google Scholar] [CrossRef]
- Millett, G.A.; Jones, A.T.; Benkeser, D.; Baral, S.; Mercer, L.; Beyrer, C.; Honermann, B.; Lankiewicz, E.; Mena, L.; Crowley, J.S. Assessing differential impacts of COVID-19 on Black communities. Ann. Epidemiol. 2020, 47, 37–44. [Google Scholar] [CrossRef]
- Oluyomi, A.O.; Gunter, S.M.; Leining, L.M.; Murray, K.O.; Amos, C. COVID-19 Community Incidence and Associated Neighborhood-Level Characteristics in Houston, Texas, USA. Int. J. Environ. Res. Public Health 2021, 18, 1495. [Google Scholar] [CrossRef] [PubMed]
- Stolte, J.; Emerson, R. Structural inequality: Position and power in network structures. Behav. Theory Sociol. 1977, 117–138. [Google Scholar]
- Royce, E. Poverty and Power: The Problem of Structural Inequality; Rowman & Littlefield: Lanham, MD, USA, 2018. [Google Scholar]
- Bowleg, L. We’re Not All in This Together: On COVID-19, Intersectionality, and Structural Inequality; American Public Health Association: Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- Sørensen, A.B. The structural basis of social inequality. Am. J. Sociol. 1996, 101, 1333–1365. [Google Scholar] [CrossRef]
- Lin, J.C.; Mitchell, L.; Crosman, E.; Mendoza, D.L.; Buchert, M.; Bares, R.; Fasoli, B.; Bowling, D.R.; Pataki, D.; Catharine, D.; et al. CO2 and Carbon Emissions from Cities: Linkages to Air Quality, Socioeconomic Activity, and Stakeholders in the Salt Lake City Urban Area. Bull. Am. Meteorol. Soc. 2018, 99, 2325–2339. [Google Scholar] [CrossRef]
- Mendoza, D.L.; Crosman, E.T.; Mitchell, L.E.; Jacques, A.; Fasoli, B.; Park, A.M.; Lin, J.C.; Horel, J. The TRAX Light-Rail Train Air Quality Observation Project. Urban Sci. 2019, 3, 108. [Google Scholar] [CrossRef] [Green Version]
- Utah Department of Transportation. Automated Traffic Signal Performance Measures; Utah Department of Transportation: Taylorsville, UT, USA, 2020.
- Utah Department of Transportation. Performance Measurement System (PeMS); Utah Department of Transportation: Taylorsville, UT, USA, 2020.
- Mendoza, D.L. The Relationship between Land Cover and Sociodemographic Factors. Urban Sci. 2020, 4, 68. [Google Scholar] [CrossRef]
- Mendoza, D.L.; Benney, T.M.; Boll, S. Long-term analysis of the relationships between indoor and outdoor fine particulate pollution: A case study using research grade sensors. Sci. Total Environ. 2021, 776, 145778. [Google Scholar] [CrossRef]
- Akanbi, M.O.; Rivera, A.S.; Akanbi, F.O.; Shoyinka, A. An ecologic study of disparities in covid-19 incidence and case fatality in oakland county, mi, usa, during a state-mandated shutdown. J. Racial Ethn. Health Disparities 2020, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Federgruen, A.; Naha, S. Crowding Effects Dominate Demographic Attributes in COVID-19 Cases. Int. J. Infect. Dis. 2020, 102, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.T.; Krieger, N. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US county versus zip code analyses. J. Public Health Manag. Pract. 2020, 27, S43–S56. [Google Scholar] [CrossRef]
- Harris, R. Exploring the neighbourhood-level correlates of Covid-19 deaths in London using a difference across spatial boundaries method. Health Place 2020, 66, 102446. [Google Scholar] [CrossRef] [PubMed]
- Lan, F.-Y.; Wei, C.-F.; Hsu, Y.-T.; Christiani, D.C.; Kales, S.N. Work-related COVID-19 transmission in six Asian countries/areas: A follow-up study. PLoS ONE 2020, 15, e0233588. [Google Scholar] [CrossRef]
- Vahidy, F.S.; Nicolas, J.C.; Meeks, J.R.; Khan, O.; Jones, S.L.; Masud, F.; Sostman, H.D.; Phillips, R.A.; Andrieni, J.D.; Kash, B.A. Racial and ethnic disparities in SARS-CoV-2 pandemic: Analysis of a COVID-19 observational registry for a diverse US metropolitan population. BMJ Open 2020, 10, e039849. [Google Scholar] [CrossRef]
- Hatef, E.; Chang, H.-Y.; Kitchen, C.; Weiner, J.P.; Kharrazi, H. Assessing the impact of neighborhood socioeconomic characteristics on COVID-19 prevalence across seven states in the United States. Front. Public Health 2020, 8, 571808. [Google Scholar] [CrossRef]
- Chetty, R.; Hendren, N. The Impacts of Neighborhoods on Intergenerational Mobility I: Childhood Exposure Effects. Q. J. Econ. 2018, 133, 1107–1162. [Google Scholar] [CrossRef]
- DiMaggio, C.; Klein, M.; Berry, C.; Frangos, S. Black/African American Communities are at highest risk of COVID-19: Spatial modeling of New York City ZIP Code–level testing results. Ann. Epidemiol. 2020, 51, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Brauer, M. How much, how long, what, and where: Air pollution exposure assessment for epidemiologic studies of respiratory disease. Proc. Am. Thorac. Soc. 2010, 7, 111–115. [Google Scholar] [CrossRef] [PubMed]
- McCreanor, J.; Cullinan, P.; Nieuwenhuijsen, M.J.; Stewart-Evans, J.; Malliarou, E.; Jarup, L.; Harrington, R.; Svartengren, M.; Han, I.-K.; Ohman-Strickland, P. Respiratory effects of exposure to diesel traffic in persons with asthma. N. Engl. J. Med. 2007, 357, 2348–2358. [Google Scholar] [CrossRef] [Green Version]
- Pirozzi, C.S.; Mendoza, D.; Xu, Y.; Zhang, Y.; Scholand, M.; Baughman, R. Short-Term Particulate Air Pollution Exposure is Associated with Increased Severity of Respiratory and Quality of Life Symptoms in Patients with Fibrotic Sarcoidosis. Int. J. Environ. Res. Public Health 2018, 15, 1077. [Google Scholar] [CrossRef] [Green Version]
- DeMarco, A.L.; Hardenbrook, R.; Rose, J.; Mendoza, D.L. Air pollution-related health impacts on individuals experiencing homelessness: Environmental justice and health vulnerability in Salt Lake County, Utah. Int. J. Environ. Res. Public Health 2020, 17, 8413. [Google Scholar] [CrossRef] [PubMed]
- Bekkar, B.; Pacheco, S.; Basu, R.; DeNicola, N. Association of Air Pollution and Heat Exposure with Preterm Birth, Low Birth Weight, and Stillbirth in the US: A Systematic Review. JAMA Netw. Open 2020, 3, e208243. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.-G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.-H. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef]
- Von Gaudecker, H.-M.; Holler, R.; Janys, L.; Siflinger, B.; Zimpelmann, C. Labour Supply in the Early Stages of the CoViD-19 Pandemic: Empirical Evidence on Hours, Home Office, and Expectations. 2020. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3579251 (accessed on 25 June 2021).
- Blau, P.M.; Duncan, O.D. The American Occupational Structure; John Wiley & Sons, Inc.: New York, NY, USA, 1967. [Google Scholar]
- Parkin, F. Class Inequality and Political Order: Social Stratification in Capitalist and Communist Societies; Praeger Publishers: Westport, CT, USA, 1971. [Google Scholar]
- Rose, D.; Pevalin, D. (Eds.) The ns-sec explained. In A Researcher’s Guide to the National Statistics Socio-Economic Classification; SAGE Publications, Ltd.: Thousand Oaks, CA, USA, 2003; pp. 28–43. [Google Scholar] [CrossRef]
- Connelly, R.; Gayle, V.; Lambert, P.S. A Review of occupation-based social classifications for social survey research. Methodol. Innov. 2016, 9, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Salt Lake County Health Department. COVID-19 Data Dashboard. 2020. Available online: https://slco.org/health/COVID-19/data/ (accessed on 10 December 2020).
- Healthy Salt Lake. 2020 Demographics. 2020. Available online: http://www.healthysaltlake.org/demographicdata (accessed on 5 June 2020).
- McGrath, S.; Sohn, H.; Steele, R.; Benedetti, A. Meta-analysis of the difference of medians. Biom. J. 2020, 62, 69–98. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.A. When to use the B onferroni correction. Ophthalmic Physiol. Opt. 2014, 34, 502–508. [Google Scholar] [CrossRef] [PubMed]
- MATLAB. Version R2019b; The MathWorks Inc.: Natick, MA, USA, 2020. [Google Scholar]
- R Core Team. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2012; Available online: https://www.R-project.org (accessed on 20 May 2019).
- Dempsey, W. The Hypothesis of Testing: Paradoxes arising out of reported coronavirus case-counts. arXiv 2020, arXiv:2005.10425. [Google Scholar]
- Mendoza, D.L.; Benney, T.M.; Bares, R.; Crosman, E.T. Intra-city variability of fine particulate matter during COVID-19 lockdown: A case study from Park City, Utah. Environ. Res. 2021, 201, 111471. [Google Scholar] [CrossRef]
- United States Department of Transportation. National Transportation Statistics 2011; USDOT, Bureau of Transportation Statistics: Washington, DC, USA, 2012.

| Metric | Group | Median | Traffic Counts (VPH) | Traffic Change (%) | |||
|---|---|---|---|---|---|---|---|
| Pre-Lockdown | Lockdown | Post-Lockdown | Pre-Lockdown to Lockdown | Lockdown to Post-Lockdown | |||
| Income (USD) | 1 | 19,949 | 970 | 713 | 829 | −29.32 | 17.84 |
| 2 | 27,570 | 1091 | 739 | 968 | −35.86 | 30.00 | |
| 3 | 37,033 | 794 | 477 | 698 | −39.92 | 36.36 | |
| Percent White | 1 | 63.24% | 830 | 591 | 704 | −28.80 | 17.84 |
| 2 | 79.93% | 1097 | 600 | 924 | −40.36 | 26.35 | |
| 3 | 89.63% | 1036 | 633 | 843 | −34.46 | 36.36 | |
| Percent White Collar | 1 | 50.44% | 970 | 757 | 856 | −29.32 | 18.03 |
| 2 | 68.88% | 1091 | 732 | 968 | −38.25 | 31.80 | |
| 3 | 76.78% | 790 | 466 | 650 | −39.92 | 35.91 | |
| Metric | Pre-Lockdown to Lockdown Traffic Change (%) | Lockdown to Post-Lockdown Traffic Change (%) |
|---|---|---|
| Income | 0.0147 * | 6.23 × 10−3 ** |
| Percent White | 0.0155 * | 4.45 × 10−4 *** |
| Percent White Collar | 6.12 × 10−3 ** | 0.0109 * |
| Metric | Pre-Lockdown to Lockdown Traffic Change (%) | Lockdown to Post-Lockdown Traffic Change (%) | ||||
|---|---|---|---|---|---|---|
| Income | Group | 1 | 2 | Group | 1 | 2 |
| 2 | 0.254 | - | 2 | 0.0823 | - | |
| 3 | 0.0115 * | 0.658 | 3 | 5.72 × 10−3 ** | 1.00 | |
| Percent White | Group | 1 | 2 | Group | 1 | 2 |
| 2 | 0.0124 * | - | 2 | 0.239 | - | |
| 3 | 0.249 | 0.818 | 3 | 2.68 × 10−4 *** | 0.0735 | |
| Percent White-Collar | Group | 1 | 2 | Group | 1 | 2 |
| 2 | 0.0665 | - | 2 | 0.0328 * | - | |
| 3 | 6.14 × 10−3 ** | 1.00 | 3 | 0.0223 * | 1.00 | |
| Metric | Pre-Lockdown to Lockdown Positive Case Change (%) | Lockdown to Post-Lockdown Positive Case Change (%) |
|---|---|---|
| Income | 3.61 × 10−5 *** | 0.976 |
| Percent White | 6.15 × 10−4 *** | 0.792 |
| Percent White-Collar | 1.72 × 10−5 *** | 0.279 |
| Metric | Pre-Lockdown to Lockdown COVID-19 Positive Case Outcome Change (%) | Lockdown to Post-Lockdown COVID-19 Positive Case Outcome Change (%) | ||||
|---|---|---|---|---|---|---|
| Income | Group | 1 | 2 | Group | 1 | 2 |
| 2 | 0.370 | - | 2 | 1.00 | - | |
| 3 | 2.66 × 10−5 *** | 8.17 × 10−3 ** | 3 | 1.00 | 1.00 | |
| Percent White | Group | 1 | 2 | Group | 1 | 2 |
| 2 | 7.47 × 10−3 ** | - | 2 | 1.00 | - | |
| 3 | 1.01 × 10−3 ** | 1.00 | 3 | 1.00 | 1.00 | |
| Percent White-Collar | Group | 1 | 2 | Group | 1 | 2 |
| 2 | 0.123 | - | 2 | 0.377 | - | |
| 3 | 9.14 × 10−6 *** | 0.0193 * | 3 | 0.716 | 1.00 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mendoza, D.L.; Benney, T.M.; Ganguli, R.; Pothina, R.; Pirozzi, C.S.; Quackenbush, C.; Baty, S.R.; Crosman, E.T.; Zhang, Y. The Role of Structural Inequality on COVID-19 Incidence Rates at the Neighborhood Scale in Urban Areas. COVID 2021, 1, 186-202. https://doi.org/10.3390/covid1010016
Mendoza DL, Benney TM, Ganguli R, Pothina R, Pirozzi CS, Quackenbush C, Baty SR, Crosman ET, Zhang Y. The Role of Structural Inequality on COVID-19 Incidence Rates at the Neighborhood Scale in Urban Areas. COVID. 2021; 1(1):186-202. https://doi.org/10.3390/covid1010016
Chicago/Turabian StyleMendoza, Daniel L., Tabitha M. Benney, Rajive Ganguli, Rambabu Pothina, Cheryl S. Pirozzi, Cameron Quackenbush, Samuel R. Baty, Erik T. Crosman, and Yue Zhang. 2021. "The Role of Structural Inequality on COVID-19 Incidence Rates at the Neighborhood Scale in Urban Areas" COVID 1, no. 1: 186-202. https://doi.org/10.3390/covid1010016
APA StyleMendoza, D. L., Benney, T. M., Ganguli, R., Pothina, R., Pirozzi, C. S., Quackenbush, C., Baty, S. R., Crosman, E. T., & Zhang, Y. (2021). The Role of Structural Inequality on COVID-19 Incidence Rates at the Neighborhood Scale in Urban Areas. COVID, 1(1), 186-202. https://doi.org/10.3390/covid1010016









