Proposal of Treatment Strategy for Pedicle Fractures of the C2: An Analysis of 49 Cases
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Demographic Data
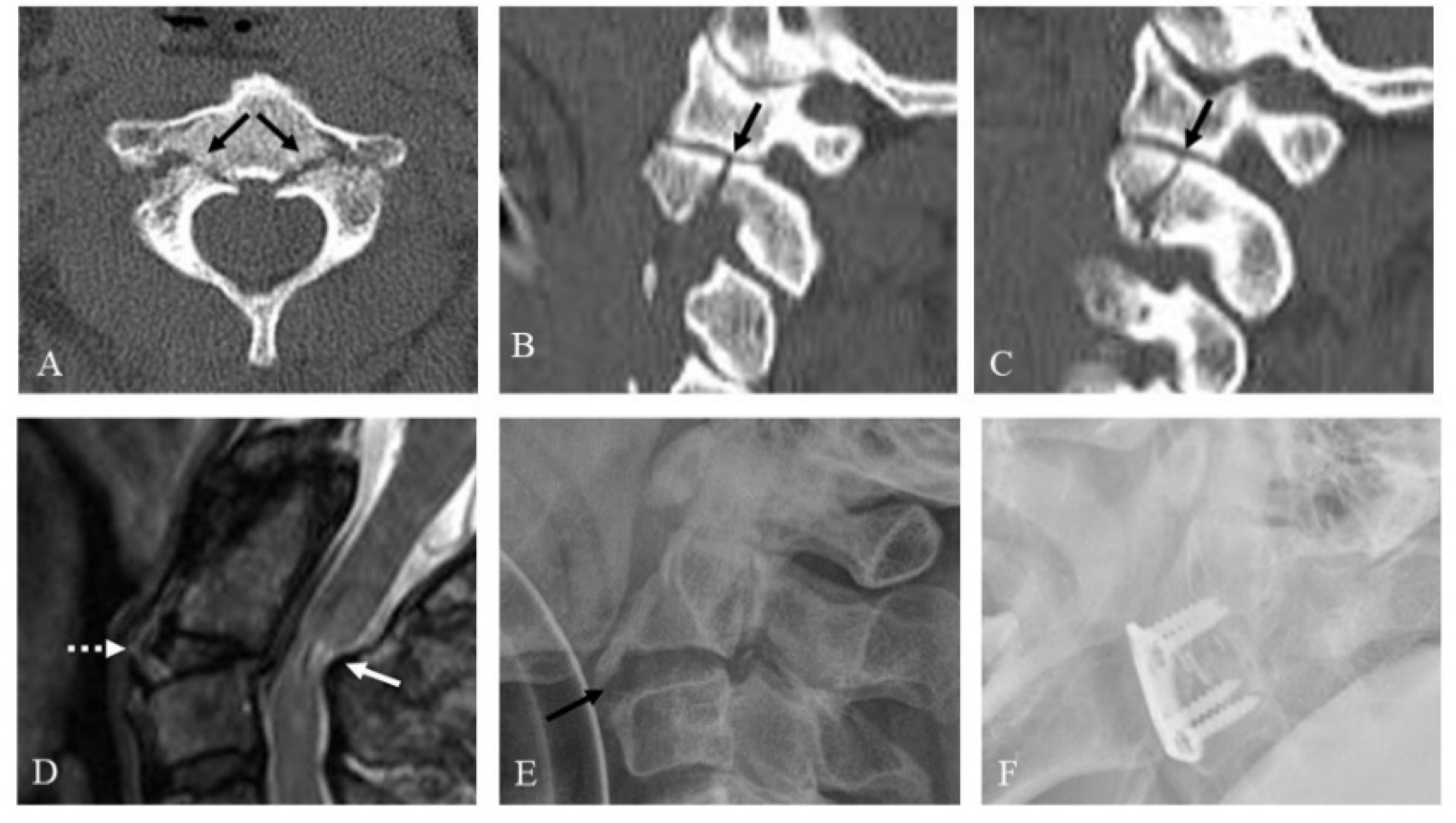
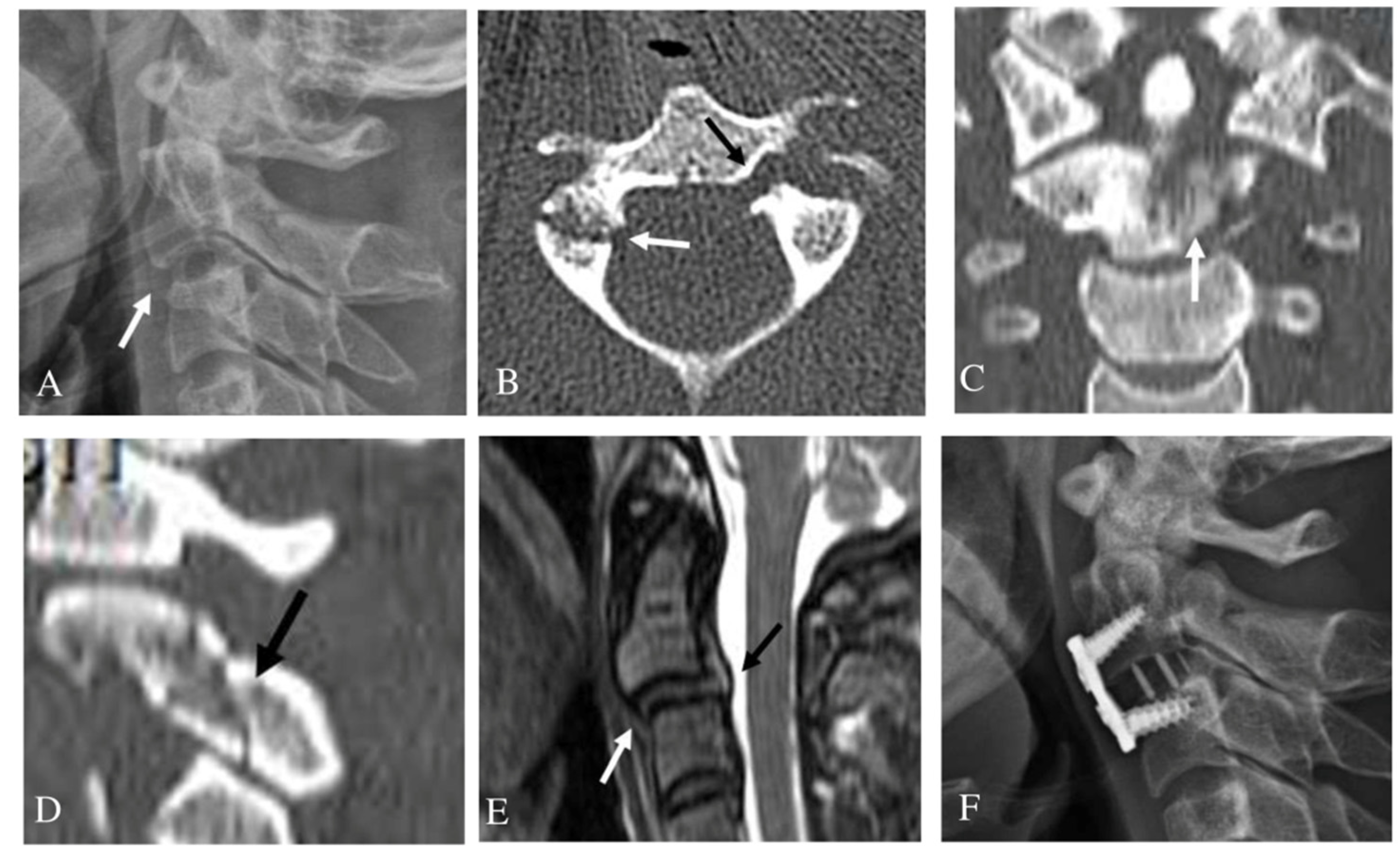
3.2. Unilateral Pedicle Fracture
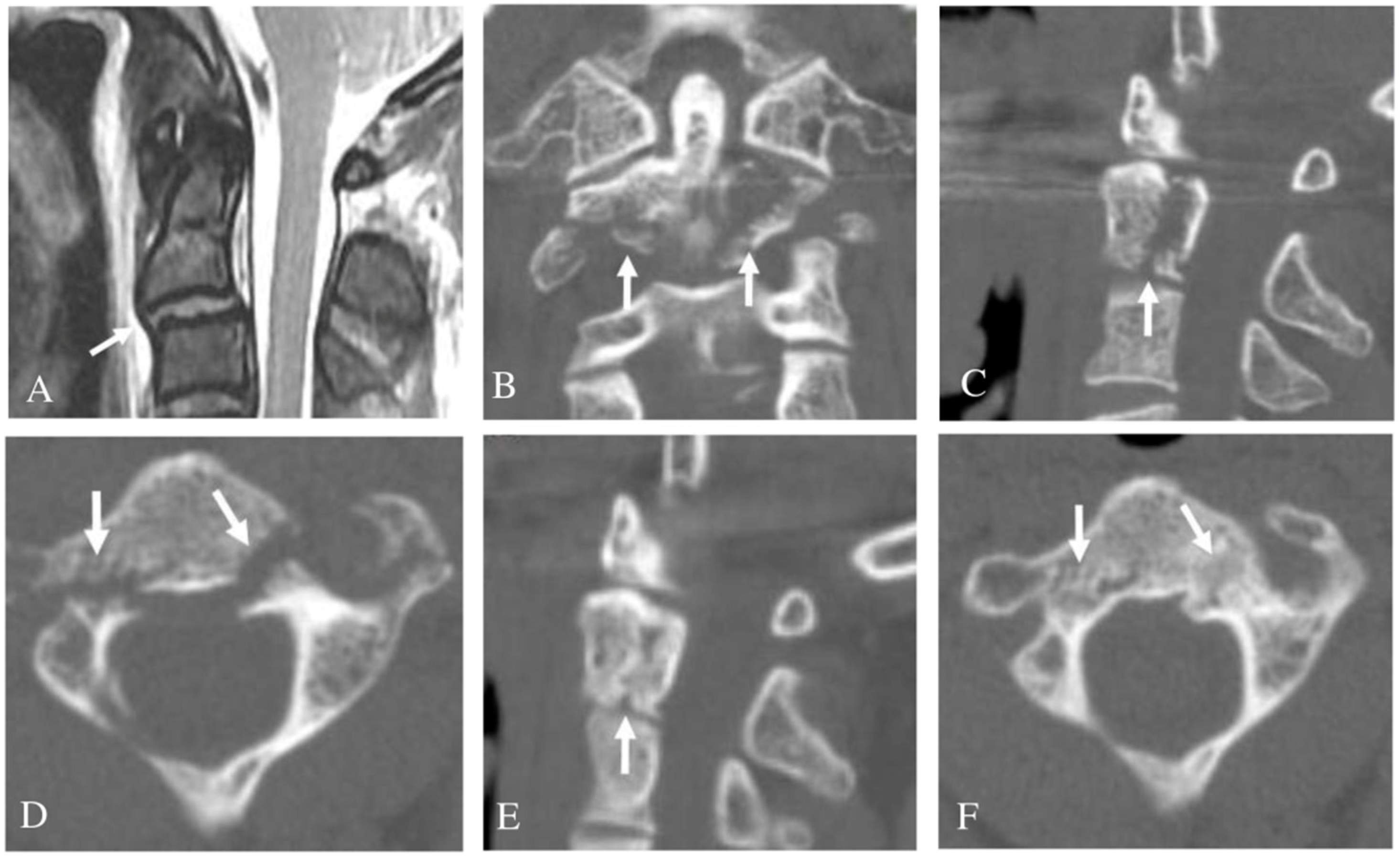
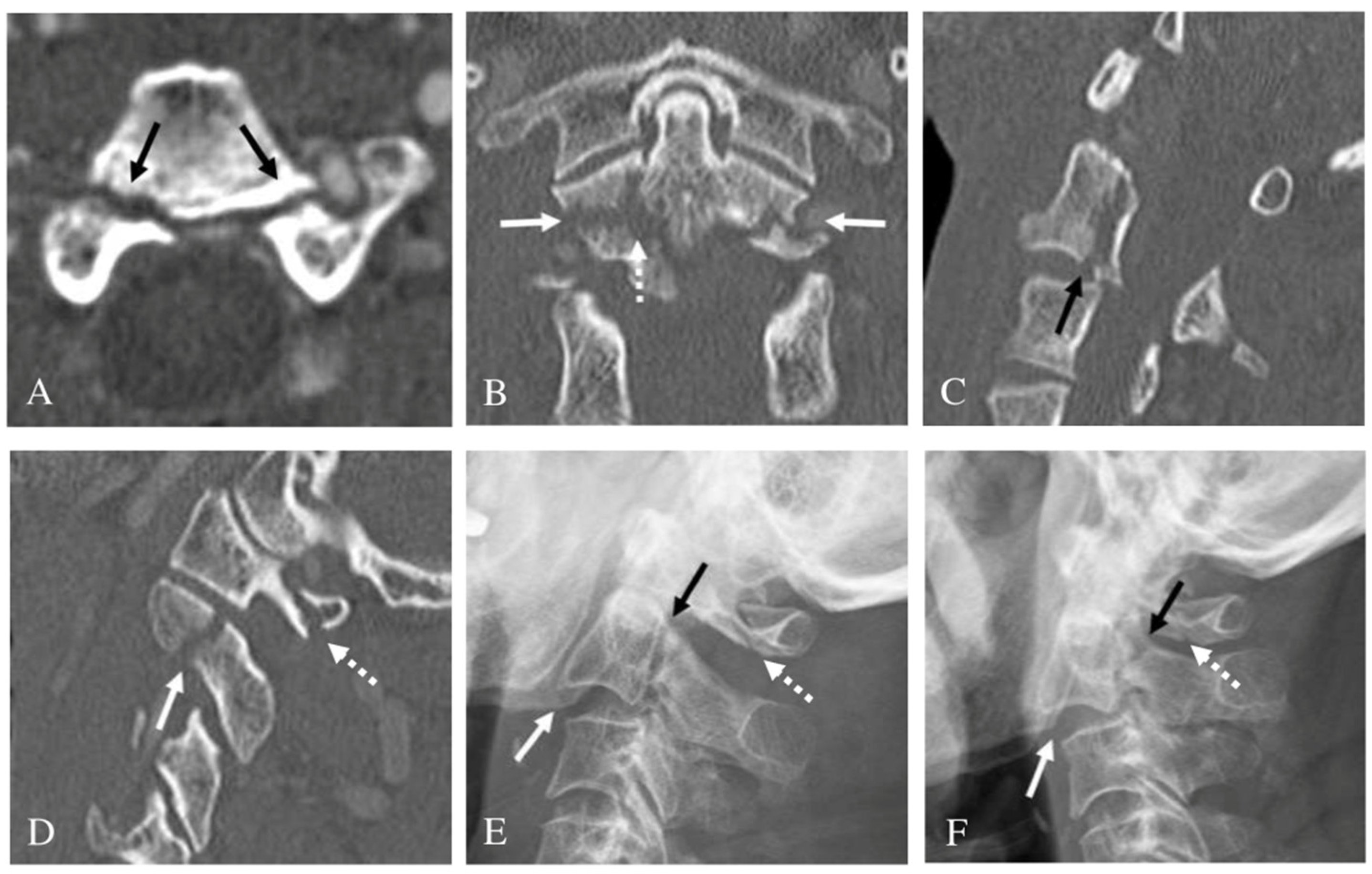
3.3. Bilateral Pedicle Fracture
3.4. Treatment Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Borne, G.M.; Bedou, G.L.; Pinaudeau, M. Treatment of pedicular fractures of the axis. A clinical study and screw fixation technique. J. Neurosurg. 1984, 60, 88–93. [Google Scholar] [CrossRef]
- Cokluk, C.; Takayasu, M.; Yoshida, J. Pedicle fracture of the axis: Report of two cases and a review of literature. Clin. Neurol. Neurosurg. 2005, 107, 136–139. [Google Scholar] [CrossRef] [PubMed]
- Ebraheim, N.A.; Fow, J.; Xu, R.; Yeasting, R.A. The location of the pedicle and pars interarticularis in the axis. Spine 2001, 26, E34–E37. [Google Scholar] [CrossRef]
- Chan, H.Y.H.; Segreto, F.A.; Horn, S.R.; Bortz, C.; Choy, G.G.; Passias, P.G.; Deverall, H.H.; Baker, J.F. C2 fractures in the elderly: Single-center evaluation of risk factors for mortality. Asian Spine J. 2019, 13, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Li, X.F.; Dai, L.Y.; Lu, H.; Chen, X.D. A systematic review of the management of hangman’s fractures. Eur. Spine J. 2006, 15, 257–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Longo, U.G.; Denaro, L.; Campi, S.; Maffulli, N.; Denaro, V. Upper cervical spine injuries: Indications and limits of the conservative management in Halo vest. A systematic review of efficacy and safety. Injury 2010, 41, 1127–1135. [Google Scholar] [CrossRef] [PubMed]
- Morel, E.; Ilharreborde, B.; Zadegan, F.; Rillardon, L.; Guigui, P. An unusual Hangman’s fracture: Description and surgical management. Orthop. Traumatol. Surg. Res. 2009, 95, 229–233. [Google Scholar] [CrossRef] [Green Version]
- Hadley, M.N.; Dickman, C.A.; Browner, C.M.; Sonntag, V.K.H. Acute axis fractures: A review of 229 cases. J. Neurosurg. 1989, 71, 642–647. [Google Scholar] [CrossRef]
- Hadley, M.N.; Browner, C.; Sonntag, V.K. Axis fractures: A comprehensive review of management and treatment in 107 cases. Neurosurgery 1985, 17, 281–290. [Google Scholar] [CrossRef]
- Kothari, M.K.; Dalvie, S.S.; Gupta, S.; Tikoo, A.; Singh, D.K. The C2 Pedicle Width, Pars Length, and Laminar Thickness in Concurrent Ipsilateral Ponticulus Posticus and High-Riding Vertebral Artery: A Radiological Computed Tomography Scan-Based Study. Asian Spine J. 2019, 13, 290–295. [Google Scholar] [CrossRef]
- Pryputniewicz, D.M.; Hadley, M.N. Axis fractures. Neurosurgery 2010, 66, 68–82. [Google Scholar] [CrossRef]
- Craig, J.B.; Hodgson, B.F. Superior facet fractures of the axis vertebra. Spine 1991, 16, 875–877. [Google Scholar] [CrossRef]
- Signoret, F.; Feron, J.M.; Bonfait, H.; Patel, A. Fractured odontoid with fractured superior articular process of the axis. Report of three cases. J. Bone Jt. Surg Br. 1986, 68, 182–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryken, T.C.; Hadley, M.N.; Aarabi, B.; Dhall, S.S.; Gelb, D.E.; Hurlbert, R.J.; Rozzelle, C.J.; Theodore, N.; Walters, B.C. Isolated fractures of the axis in adults. Neurosurgery 2002, 50, S125–S139. [Google Scholar]
- Martin, G.J.; Haid, R.W.; Rodts, G.E. Injuries to the atlantoaxial complex: Diagnosis & classification. Contemp. Neurosurg. 1997, 19, 1–8. [Google Scholar]
- Greene, K.A.; Dickman, C.A.; Marciano, F.F.; Drabier, J.B.; Hadley, M.N.; Sonntag, V.K. Acute axis fractures: Analysis of management and outcome in 340 consecutive cases. Spine 1997, 22, 1843–1852. [Google Scholar] [CrossRef] [PubMed]
- Benzel, E.C.; Hart, B.L.; Ball, P.A.; Baldwin, N.G.; Orrison, W.W.; Espinosa, M. Fractures of the C-2 vertebral body. J. Neurosurg. 1994, 81, 206–212. [Google Scholar] [CrossRef] [Green Version]
- Oliveira, E.D.; Rhoton, A.L.; Peace, D. Microsurgical anatomy of the region of the foramen magnum. Surg. Neurol. 1985, 24, 293–352. [Google Scholar] [CrossRef]
- Panjabi, M.M.; Duranceau, J.; Goel, V.; Oxland, T.; Takata, K. Cervical human vertebrae. Quantitative three dimensional anatomy of the middle and lower regions. Spine 1991, 16, 861–869. [Google Scholar] [CrossRef]
- Heller, J.G.; Pedlow, F.X., Jr.; Gill, S.S. Anatomy of the cervical spine. In The Cervical Spine, 4th ed.; Clark, C.R., Benzel, E.C., Currier, B.L., Dormans, J.P., Dvorak, J., Eismont, F., Garfin, S.R., Herkowitz, H.N., Ullrich, C.G., Vaccaro, A.R., Eds.; JB Lippincott: Philadelphia, PA, USA, 2005; pp. 3–36. [Google Scholar]
- Smith, M.D.; Anderson, P.; Grady, M.S. Occipitocervical arthrodesis using contoured plate fixation. An early report on a versatile fixation technique. Spine 1993, 18, 1984–1990. [Google Scholar] [CrossRef]
- Williams, P.L.; Bannister, L.H.; Berry, M.M.; Collins, P.; Dyson, M.; Dussek, J.E.; Ferguson, M.W.J. Skeletal system. In Gray’s Anatomy, 38th ed.; Churchill Livingstone: New York, NY, USA, 1995; pp. 519–520. [Google Scholar]
- Kepler, C.K.; Vaccaro, A.R.; Fleischman, A.N.; Traynelis, V.C.; Patel, A.A.; Dekutoski, M.B.; Harrop, J.; Wood, K.B.; Schroeder, G.D.; Bransford, R. Treatment of Axis Body Fractures: A Systematic Review. Clin. Spine Surg. 2017, 30, 442–456. [Google Scholar] [CrossRef] [PubMed]
- Ankith, N.V.; Avinash, M.; Srivijayanand, K.S.; Shetty, A.P.; Kanna, R.M.; Rajasekaran, S. Congenital Osseous Anomalies of the Cervical Spine: Occurrence, Morphological Characteristics, Embryological Basis and Clinical Significance: A Computed Tomography Based Study. Asian Spine J. 2019, 14, 535–543. [Google Scholar]
- German, J.W.; Hart, B.L.; Benzel, E.C. Nonoperative management of vertical C2 body fractures. Neurosurgery 2005, 56, 516–521. [Google Scholar] [CrossRef] [PubMed]

| Age (Years) | 59.1 ± 15.4 (Range: 31–86) |
|---|---|
| Sex | Male: Female = 32:17 |
| Follow-up (months) | 12.6 ± 2.6 (range: 12–26) |
| Fracture type | |
| Unilateral pedicle fracture | 22 (44.9%) |
| Bilateral pedicle fracture | 27 (55.1%) |
| Injury mechanism | |
| Motor-vehicle accident | 28 (57.1%) |
| Falling down | 16 (32.7%) |
| Slipping down | 3 (6.1%) |
| Direct external force | 2 (4.1%) |
| Neurologic status | |
| Normal | 48 (98.0%) |
| Deficit | 1 (2.0%) |
| Other associated C2 fractures | |
| Yes | 49 (100%) |
| No | 0 (0%) |
| Unilateral Pedicle Fx. (N = 22) | Bilateral Pedicle Fx. (N = 27) | p | |
|---|---|---|---|
| Other associated C2 injuries | 22 (100%) | 27 (100%) | |
| Pars interarticularis Fx. | 13 | 13 | |
| Superior articular facet Fx. | 20 | 24 | |
| Inferior articular facet Fx. | 3 | 0 | |
| Transverse foramen Fx. | 13 | 16 | |
| Lamina Fx. | 2 | 0 | |
| Spinous process Fx. | 1 | 1 | |
| Body Fx. | 20 (90.9%) | 27 (100%) | 0.196 |
| Dens Fx. (type III) | 11 | 13 | |
| Vertical Fx. | 5 | 14 | |
| Transverse Fx. | 0 | 1 | |
| Comminuted Fx. | 2 | 0 | |
| Teardrop Fx. (Anterior: Posterior) | 4 (1:3) | 2 (0:2) | |
| Anterior slip C2-3 | 2 | 5 | 0.303 |
| Spinal cord injury at C2-3 | 0 | 1 | 1.000 |
| Other cervical injury | 2 | 6 | 0.269 |
| Total (N = 49) | Unilateral Pedicle Fx. (N = 22) | Bilateral Pedicle Fx. (N = 27) | p | |
|---|---|---|---|---|
| Conservative treatment | 43 (87.8%) | 19 (86.4%) | 24 (88.9%) | 0.362 |
| Halovest | 33 | 14 | 19 | |
| Philadelphia brace | 10 | 5 | 5 (1 non-union) | |
| Surgery | 6 (12.2%) | 3 (13.6%) | 3 (11.1%) | 0.500 |
| ACDF C2-3 | 4 | 2 | 2 | |
| Posterior fusion C1-2 | 1 | 1 | 0 | |
| Dens screw fixation | 1 | 0 | 1 | |
| Success rate of treatment | 48/49 (98.0%) | 100% | 96.3% (1 non-union) | 0.449 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-B.; Kim, S.-K.; Seo, H.-Y.; Ko, J.-H.; Hong, T.-M. Proposal of Treatment Strategy for Pedicle Fractures of the C2: An Analysis of 49 Cases. J. Clin. Med. 2021, 10, 3987. https://doi.org/10.3390/jcm10173987
Park J-B, Kim S-K, Seo H-Y, Ko J-H, Hong T-M. Proposal of Treatment Strategy for Pedicle Fractures of the C2: An Analysis of 49 Cases. Journal of Clinical Medicine. 2021; 10(17):3987. https://doi.org/10.3390/jcm10173987
Chicago/Turabian StylePark, Jong-Beom, Sung-Kyu Kim, Hyoung-Yeon Seo, Jong-Hyun Ko, and Tae-Min Hong. 2021. "Proposal of Treatment Strategy for Pedicle Fractures of the C2: An Analysis of 49 Cases" Journal of Clinical Medicine 10, no. 17: 3987. https://doi.org/10.3390/jcm10173987






