Exploring the In Vivo Existence Forms (23 Original Constituents and 147 Metabolites) of Astragali Radix Total Flavonoids and Their Distributions in Rats Using HPLC-DAD-ESI-IT-TOF-MSn
Abstract
1. Introduction
2. Results and Discussion
2.1. Identification of Original Constituents and Metabolites of ARTF in Rats
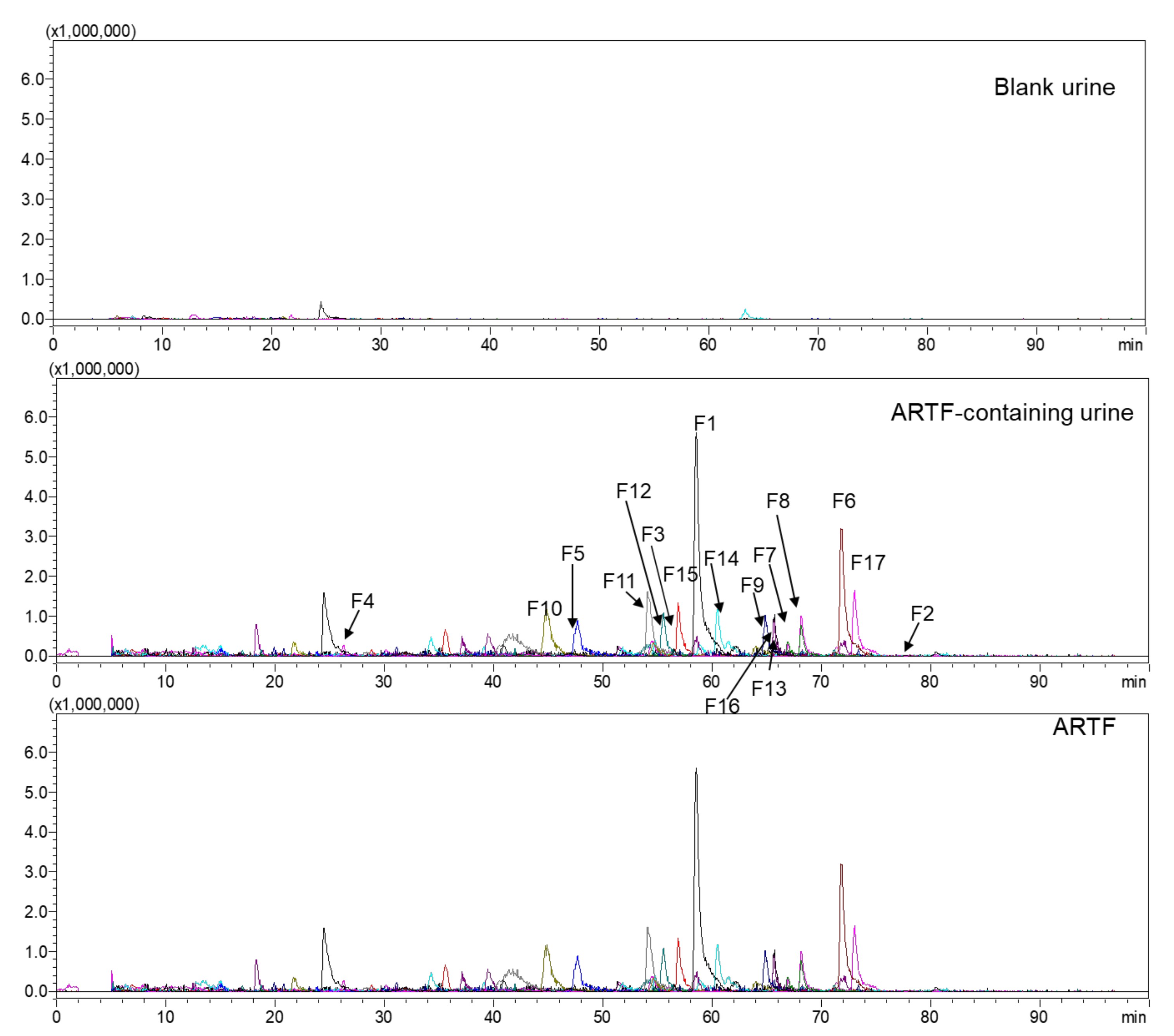
2.1.1. Identification of Original Constituents
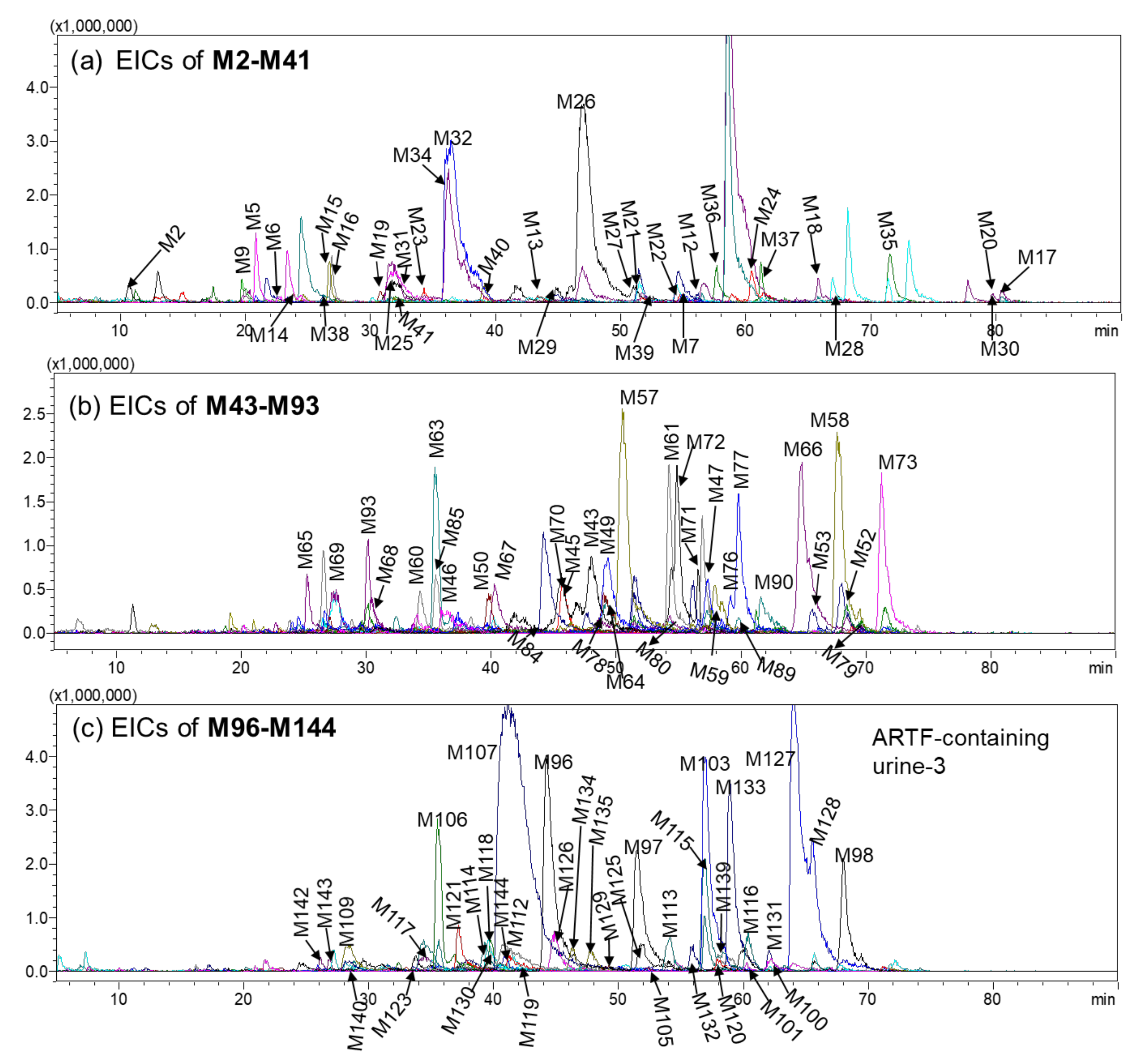
2.1.2. Identification of Metabolites
Identification of the Sulfates of the Ring Cleavage Products of Flavone (M1–M16)
Identification of the Calycosin-Related Metabolites (M17–M72, M146)
Identification of the Formononetin-Related Metabolites (M73–M78)
Identification of the Astrapterocarpan-Related Metabolites (M79–M84)
Identification of the Astraisoflavan-Related Metabolites (M85–M106, M147)
Identification of the Daidzein-Related Metabolites (M107–M117)
Identification of the Genistein-Related Metabolites (M118–M130)
Identification of the Equol-Related Metabolites (M131–M139)
Identification of the other Metabolites (M140–M145)
2.2. Distribution of Original Constituents and Metabolites of ARTF in Rats Organs
2.2.1. Distribution of Original Constituents
2.2.2. Distribution of Metabolites
2.3. Identification of Metabolites Isolated from Rat Urine
2.4. ARTF-Related Pharmacological Effect of Compounds In Vivo
3. Materials and Methods
3.1. Chemicals and Materials
3.2. Animals and ARTF Administration
3.3. Bio-Samples Collection and Pre-Treatment
3.3.1. Urine Collection and Pre-Treatment
3.3.2. Feces Collection and Pre-Treatment
3.3.3. Plasma Collection and Pre-Treatment
3.3.4. Organs Collection and Pre-Treatment
3.4. Isolation and Identification of Metabolites from ARTF-Containing Urine
3.5. Instruments and Conditions
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Jing, L.; Zhao, Z.Z.; Chen, H.B. Review of Astragali Radix. Chin. Herb. Med. 2011, 3, 90–105. [Google Scholar]
- Wang, D.Q.; Zhuang, Y.; Tian, Y.P.; Thomas, G.N.; Ying, M.Z.; Tomlinson, B. Study of the effects of total flavonoids of Astragalus on atherosclerosis formation and potential mechanisms. Oxid. Med. Cell Longev. 2012, 2012, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.Q.; Ding, B.G.; Tomas, G.N.; Tian, Y.P.; Wang, C.B.; Tomlinson, B. Effects of total flavonoids of astragalus on early atheroselerosis in rabbits with diet-induced hyPereholesterolemia. Chin. Pharmacol. Bull. 2003, 19, 637–639. [Google Scholar]
- Liu, Q.; Zhang, L.; Shan, Q.; Ding, Y.; Zhang, Z.; Zhu, M.; Mao, Y. Total flavonoids from Astragalus alleviate endothelial dysfunction by activating the Akt/eNOS pathway. J. Int. Med. Res. 2018, 46, 2096–2103. [Google Scholar] [CrossRef]
- Li, Q. Effects of Total Flavonoids of Astragalus on Inflammatory Response in Brain Tissue of Natural Aging Rats and Its Related Mechanism. J. Beihua Univ. (Nat. Sci.) 2018, 19, 745–749. [Google Scholar]
- Guo, Z.; Xu, H.Y.; Xu, L.; Wang, S.S.; Zhang, X.M. In Vivo and in Vitro Immunomodulatory and Anti-Inflammatory Effects of Total Flavonoids of Astragalus. Afr. J. Tradit. Complement. Altern. Med. 2016, 13, 60–73. [Google Scholar] [CrossRef]
- Li, J.; Xu, L.; Sang, R.; Yu, Y.; Ge, B.; Zhang, X. Immunomodulatory and anti-inflammatory effects of total flavonoids of Astragalus by regulating NF-κB and MAPK signalling pathways in RAW 264.7 macrophages. Pharmazie 2018, 73, 589–593. [Google Scholar]
- Wang, D.Q.; Ding, B.G.; Ma, Y.Q.; Zhao, H.L.; Thomas, G.N.; Tomlinson, B.; Tian, Y.P.; Wang, C.B.; Critchley, J.A. Studies on Protective Effect of Total Flavonoids of Astragalus on Liver Damage Paracetamol-Induced by. Chin. J. Chin. Mater. Med. 2001, 26, 483–486. [Google Scholar]
- Shen, W.M.; Wang, C.B.; Wang, D.Q.; Tian, Y.P.; Yan, G.T.; Hao, X.H. The protective effects of TFA on reperfusion induced hepatic injury in hemorrhagic shock. Chin. Pharmacol. Bull. 1997, 13, 532–534. [Google Scholar]
- Lee, E.J.; Yean, M.H.; Jung, H.S.; Kim, J.S.; Kang, S.S. Phytochemical Studies on Astragalus Root (2); Flavonoids and a Lignan. Nat. Prod. Sci. 2008, 14, 131–137. [Google Scholar]
- Yang, L.P.; Shen, J.G.; Xu, W.C.; Li, J.; Jiang, J.Q. Secondary metabolites of the genus Astragalus: Structure and biological-activity update. Chem. Biodivers. 2013, 10, 1004–1054. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.J.; Liu, H.K.; Hsiao, P.C.; Kuo, L.M.Y.; Lee, I.J.; Wu, T.S.; Chiou, W.F.; Kuo, Y.H. New Isoflavonoid Glycosides and Related Constituents from Astragali Radix (Astragalus membranaceus) and Their Inhibitory Activity on Nitric Oxide Production. J. Agr. Food Chem. 2011, 59, 1131–1137. [Google Scholar] [CrossRef] [PubMed]
- Yan, Z.; Lin, G.; Ye, Y.; Wang, Y.; Yan, R. A generic multiple reaction monitoring based approach for plant flavonoids profiling using a triple quadrupole linear ion trap mass spectrometry. J. Am. Soc. Mass. Spectr. 2014, 25, 955–965. [Google Scholar] [CrossRef]
- Zhang, Y.Z.; Xu, F.; Yang, D.H.; Shang, M.Y.; Yang, D.H.; Wang, X.; Cai, S.Q. Profiling and identification of the metabolites of calycosin in rat hepatic 9000× g supernatant incubation system and the metabolites of calycosin-7-O-β-D-glucoside in rat urine by HPLC-DAD-ESI-IT-TOF-MSn technique. J. Pharm. Biomed. Anal. 2012, 70, 425–439. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.Z. Metabolic research of 8 isoflavone in Astragalus. Ph.D. Thesis, Beijing University, Beijing, China, 2011. [Google Scholar]
- Zhang, Y.Z.; Xu, F.; Dong, J.; Liang, J.; Hashi, Y.; Liu, G.X.; Li, Y.L.; Shang, M.Y.; Wang, X.; Cai, S.Q. Profiling the metabolites of astrapterocarpan in rat hepatic 9000g supernatant. Chin. J. Nat. Med. 2019, 17, 842–857. [Google Scholar] [CrossRef]
- Hu, G.; Siu, S.O.; Li, S.; Chu, I.K.; Kwan, Y.W.; Chan, S.W.; Leung, G.P.H.; Yan, R.; Lee, S.M.Y. Metabolism of calycosin, an isoflavone from Astragali Radix, in zebrafish larvae. Xenobiotica 2012, 42, 294–303. [Google Scholar] [CrossRef]
- Zhang, W.; Jiang, S.; Qian, D.W.; Shang, E.X.; Duan, J.A. Analysis of interaction property of calycosin-7-O-β-D-glucoside with human gut microbiota. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2014, 963, 16–23. [Google Scholar] [CrossRef]
- Davies, H.L.; Hill, J.L. The Effect of Diet on the Metabolism in Sheep of the Tritiated Isoflavones Formononetin and Biochanin-A. Aust. J. Agr. Res. 1989, 40, 157–163. [Google Scholar] [CrossRef]
- Tolleson, W.H.; Doerge, D.R.; Churchwell, M.I.; Marques, M.M.; Roberts, D.W. Metabolism of biochanin A and formononetin by human liver microsomes in vitro. J. Agr. Food Chem. 2002, 50, 4783–4790. [Google Scholar] [CrossRef]
- Zhang, W.; Jiang, S.; Qian, D.W.; Shang, E.X.; Guan, H.L.; Ren, H.; Zhu, Z.H.; Duan, J.A. The interaction between ononin and human intestinal bacteria. Acta Pharm. Sinica 2014, 49, 1162–1168. [Google Scholar]
- Li, H.F. Studies on the Metabolism of Astragali Radix In Vivo. Ph.D. Thesis, Shenyang Pharmaceutical University, Shenyang, China, 2017. [Google Scholar]
- Sun, J. Progress and Application of Astragalus and its classic prescription. Chin. Hosp. Pharm. J. 2019, 39, 1311–1314. [Google Scholar]
- Yang, P. Study on the In Vivo Metabolism of the Rhizomes of Smilax Glabra and Screening of Its Bioactive Components In Vivo. Ph.D. Thesis, Beijing University, Beijing, China, 2016. [Google Scholar]
- Liang, J.; Xu, F.; Zhang, Y.Z.; Zang, X.Y.; Wang, D.; Shang, M.Y.; Wang, X.; Chui, D.H.; Cai, S.Q. The profiling and identification of the metabolites of (+)-catechin and study on their distribution in rats by HPLC-DAD-ESI-IT-TOF-MS(n) technique. Biomed. Chromatogr. 2014, 28, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Xu, F.; Zhang, Y.Z.; Huang, S.; Zang, X.Y.; Zhao, X.; Zhang, L.; Shang, M.Y.; Yang, D.H.; Wang, X.; et al. The profiling and identification of the absorbed constituents and metabolites of Paeoniae Radix Rubra decoction in rat plasma and urine by the HPLC-DAD-ESI-IT-TOF-MS(n) technique: A novel strategy for the systematic screening and identification of absorbed constituents and metabolites from traditional Chinese medicines. J. Pharm. Biomed. Anal. 2013, 83, 108–121. [Google Scholar] [PubMed]
- Gao, X.; Mu, J.; Li, Q.; Guan, S.; Liu, R.; Du, Y.; Zhang, H.; Bi, K. Comprehensive Identification of Guan-Xin-Shu-Tong Capsule via a Mass Defect and Fragment Filtering Approach by High Resolution Mass Spectrometry: In Vitro and In Vivo Study. Molecules 2017, 22, 1007. [Google Scholar] [CrossRef]
- Zhao, X.; Yang, D.H.; Xu, F.; Huang, S.; Zhang, L.; Liu, G.X.; Cai, S.Q. The in vivo absorbed constituents and metabolites of Danshen decoction in rats identified by HPLC with electrospray ionization tandem ion trap and time-of-flight mass spectrometry. Biomed. Chromatogr. 2015, 29, 285–304. [Google Scholar] [CrossRef]
- Li, W.L.; Sun, X.M.; Song, H.; Ding, J.X.; Bai, J.; Chen, Q. HPLC/Q-TOF-MS-Based Identification of Absorbed Constituents and Their Metabolites in Rat Serum and Urine after Oral Administration of Cistanche deserticola Extract. J. Food Sci. 2015, 80, H2079–H2087. [Google Scholar] [CrossRef]
- Hamed, A.I.; Ben Said, R.; Kontek, B.; Al-Ayed, A.S.; Kowalczyk, M.; Moldoch, J.; Stochmal, A.; Olas, B. LC-ESI-MS/MS profile of phenolic and glucosinolate compounds in samh flour (Mesembryanthemum forsskalei Hochst. ex Boiss) and the inhibition of oxidative stress by these compounds in human plasma. Food Res. Int. 2016, 85, 282–290. [Google Scholar] [CrossRef]
- Ren, X.L. Study on the Effective Substances of Buyang Huanwu Decoction—Study on the Chemical Constituents of Buyang Huanwu Decoction in Pigs Urine. Master’s Thesis, Beijing University, Beijing, China, 2013. [Google Scholar]
- Fang, G.; Zhang, P.; Ye, X.L. Elecron spray ion trap mass spectrometry of isoflavones and isoflavone aglycones of Semen Sojae Praeparatum. Acad. J. Second Mil. Med. Univ. 2013, 34, 1108–1115. [Google Scholar] [CrossRef]
- Antignac, J.P.; Cariou, R.; Le Bizec, B.; Andre, F. New data regarding phytoestrogens content in bovine milk. Food Chem. 2004, 87, 275–281. [Google Scholar] [CrossRef]
- Murthy, M.S.R.; Rao, E.V.; Ward, R.S. Carbon-13 nuclear magnetic resonance spectra of isoflavones. Magn. Reson. Chem. 1986, 24, 225–230. [Google Scholar] [CrossRef]
- Nakano, H.; Ogura, K.; Takahashi, E.; Harada, T.; Nishiyama, T.; Muro, K.; Hiratsuka, A.; Kadota, S.; Watabe, T. Regioselective monosulfation and disulfation of the phytoestrogens daidzein and genistein by human liver sulfotransferases. Drug Metab. Pharmacol. 2004, 19, 216–226. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.Z.; Xu, F.; Liang, J.; Tang, J.S.; Shang, M.Y.; Wang, X.; Cai, S.Q. Isoflavonoids from roots of Astragalus membranaceus var. mongholicus. Chin. J. Chin. Mater. Med. 2012, 37, 3243–3248. [Google Scholar]
- Knowlton, A.A.; Lee, A.R. Estrogen and the cardiovascular system. Pharmacol. Ther. 2012, 135, 54–70. [Google Scholar] [CrossRef]
- Straub, R.H. The complex role of estrogens in inflammation. Endocr. Rev. 2007, 28, 521–574. [Google Scholar] [CrossRef] [PubMed]
- Bai, F.; Makino, T.; Kono, K.; Nagatsu, A.; Ono, T.; Mizukami, H. Calycosin and formononetin from astragalus root enhance dimethylarginine dimethylaminohydrolase 2 and nitric oxide synthase expressions in Madin Darby Canine Kidney II cells. J. Nat. Med. 2013, 67, 782–789. [Google Scholar] [CrossRef]
- Yu, D.H.; Bao, Y.M.; An, L.J.; Yang, M. Protection of PC12 Cells against Superoxide-induced Damage by Isoflavonoids from Astragalus mongholicus. Biomed. Environ. Sci. 2009, 22, 50–54. [Google Scholar] [CrossRef]
- Ma, R.; Yuan, F.; Wang, S.; Liu, Y.; Fan, T.; Wang, F. Calycosin alleviates cerulein-induced acute pancreatitis by inhibiting the inflammatory response and oxidative stress via the p38 MAPK and NF-kappaB signal pathways in mice. Biomed. Pharmacother. 2018, 105, 599–605. [Google Scholar] [CrossRef]
- Tian, J.; Wang, Y.; Zhang, X.; Ren, Q.Y.; Li, R.; Huang, Y.; Lu, H.L.; Chen, J. Calycosin inhibits the in vitro and in vivo growth of breast cancer cells through WDR7-7-GPR30 Signaling. J. Exp. Clin. Canc. Res. 2017, 36, 153–166. [Google Scholar] [CrossRef]
- Duan, X.; Meng, Q.; Wang, C.; Liu, Z.; Sun, H.; Huo, X.; Sun, P.; Ma, X.; Peng, J.; Liu, K. Effects of calycosin against high-fat diet-induced nonalcoholic fatty liver disease in mice. J. Gastroenterol Hepatol 2018, 33, 533–542. [Google Scholar] [CrossRef]
- Ren, M.; Wang, X.; Du, G.; Tian, J.; Liu, Y. Calycosin-7-O-β-D-glucoside attenuates ischemia-reperfusion injury in vivo via activation of the PI3K/Akt pathway. Mol. Med. Rep. 2015, 13, 633–640. [Google Scholar] [CrossRef]
- Fu, S.P.; Gu, Y.; Jiang, J.Q.; Chen, X.; Xu, M.J.; Chen, X.M.; Shen, J.G. Calycosin-7-O-beta-D-glucoside regulates nitric oxide/caveolin-1/matrix metalloproteinases pathway and protects blood-brain barrier integrity in experimental cerebral ischemia-reperfusion injury. J. Ethnopharmacol. 2014, 155, 692–701. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.I.; Heo, T.R.; Min, B.H.; Cui, J.H.; Choi, B.H.; Park, S.R. Alleviation of osteoarthritis by calycosin-7-O-β-D-glucopyranoside (CG) isolated from Astragali radix (AR) in rabbit osteoarthritis (OA) model. Osteoarthritis Cartilage 2007, 15, 1086–1092. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.M. Effect of calycosin-7-O-beta-D-glucoside on cell apoptosis in cervical cancer HeLa cell and expression of Bcl-2/Bax. Chin. Tradit. Herbal Drugs 2015, 46, 1498–1502. [Google Scholar]
- Zhu, J.T.T.; Choi, R.C.Y.; Chu, G.K.Y.; Cheung, A.W.H.; Gao, Q.T.; Li, J.; Jiang, Z.Y.; Dong, T.T.X.; Tsim, K.W.K. Flavonoids possess neuroprotective effects on cultured pheochromocytoma PC12 cells: A comparison of different flavonoids in activating estrogenic effect and in preventing β-amyloid-induced cell death. J. Agr Food Chem. 2007, 55, 2438–2445. [Google Scholar] [CrossRef]
- Dong, L.; Yin, L.; Zhang, Y.; Fu, X.; Lu, J. Anti-inflammatory effects of ononin on lipopolysaccharide-stimulated RAW 264.7 cells. Mol. Immunol. 2017, 83, 46–51. [Google Scholar] [CrossRef]
- Jun, M.; Hong, J.; Jeong, W.S.; Ho, C.T. Suppression of arachidonic acid metabolism and nitric oxide formation by kudzu isoflavones in murine macrophages. Mol. Nutr. Food Res. 2005, 49, 1154–1159. [Google Scholar] [CrossRef]
- Jin, Y.M.; Xu, T.M.; Zhao, Y.H.; Wang, Y.C.; Cui, M.H. In vitro and in vivo anti-cancer activity of formononetin on human cervical cancer cell line HeLa. Tumour Biol. 2014, 35, 2279–2284. [Google Scholar] [CrossRef]
- Yang, S.; Wei, L.; Xia, R.; Liu, L.; Chen, Y.; Zhang, W.; Li, Q.; Feng, K.; Yu, M.; Zhang, W.; et al. Formononetin ameliorates cholestasis by regulating hepatic SIRT1 and PPARalpha. Biochem. Biophys. Res. Commun. 2019, 512, 770–778. [Google Scholar] [CrossRef]
- Applova, L.; Karlickova, J.; Riha, M.; Filipsky, T.; Macakova, K.; Spilkova, J.; Mladenka, P. The isoflavonoid tectorigenin has better antiplatelet potential than acetylsalicylic acid. Phytomedicine 2017, 35, 11–17. [Google Scholar] [CrossRef]
- Valeri, A.; Fiorenzani, P.; Rossi, R.; Aloisi, A.M.; Valoti, M.; Pessina, F. The soy phytoestrogens genistein and daidzein as neuroprotective agents against anoxia-glucopenia and reperfusion damage in rat urinary bladder. Pharmacol Res. 2012, 66, 309–316. [Google Scholar] [CrossRef]
- He, Y.; Wu, X.; Cao, Y.; Hou, Y.; Chen, H.; Wu, L.; Lu, L.; Zhu, W.; Gu, Y. Daidzein exerts anti-tumor activity against bladder cancer cells via inhibition of FGFR3 pathway. Neoplasma 2016, 63, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.C.; Portmann, B.; Sherwood, R.; Niemela, O.; Koivisto, H.; Parkkila, S.; Trick, K.; L’Abbe, M.R.; Wilson, J.; Dash, P.R.; et al. The cytoprotective effect of alpha-tocopherol and daidzein against d-galactosamine-induced oxidative damage in the rat liver. Metabolism 2007, 56, 865–875. [Google Scholar] [CrossRef] [PubMed]
- Rajadurai, M.; Prince, P.S. Preventive effect of naringin on isoproterenol-induced cardiotoxicity in Wistar rats: An in vivo and in vitro study. Toxicology 2007, 232, 216–225. [Google Scholar] [CrossRef] [PubMed]
- Golechha, M.; Chaudhry, U.; Bhatia, J.; Saluja, D.; Arya, D.S. Naringin protects against kainic acid-induced status epilepticus in rats: Evidence for an antioxidant, anti-inflammatory and neuroprotective intervention. Biol. Pharm. Bull. 2011, 34, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Dong, Y.; Hao, G.; Wang, B.; Wang, J.; Liang, Y.; Liu, Y.; Zhen, E.; Feng, D.; Liang, G. Naringin suppresses the development of glioblastoma by inhibiting FAK activity. J. Drug Target. 2017, 25, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Lai, Y.; Huang, P.; Xie, L.; Lin, H.; Zhou, Z.; Mo, C.; Deng, G.; Yan, W.; Gao, Z.; et al. Naringin attenuates alcoholic liver injury by reducing lipid accumulation and oxidative stress. Life Sci. 2019, 216, 305–312. [Google Scholar] [CrossRef]
- Guo, D.; Wang, J.; Wang, X.; Luo, H.; Zhang, H.; Cao, D.; Chen, L.; Huang, N. Double directional adjusting estrogenic effect of naringin from Rhizoma drynariae (Gusuibu). J. Ethnopharmacol. 2011, 138, 451–457. [Google Scholar] [CrossRef]
- Pugazhendhi, D.; Watson, K.A.; Mills, S.; Botting, N.; Pope, G.S.; Darbre, P.D. Effect of sulphation on the oestrogen agonist activity of the phytoestrogens genistein and daidzein in MCF-7 human breast cancer cells. J. Endocrinol. 2008, 197, 503–515. [Google Scholar] [CrossRef]
- Kgomotso, T.; Chiu, F.; Ng, K. Genistein- and daidzein 7-O-beta-D-glucuronic acid retain the ability to inhibit copper-mediated lipid oxidation of low density lipoprotein. Mol. Nutr. Food Res. 2008, 52, 1457–1466. [Google Scholar] [CrossRef]
- Morito, K.; Aomori, T.; Hirose, T.; Kinjo, J.; Hasegawa, J.; Ogawa, S.; Inoue, S.; Muramatsu, M.; Masamune, Y. Interaction of phytoestrogens with estrogen receptors α and β (II). Biol. Pharm. Bull. 2002, 25, 48–52. [Google Scholar] [CrossRef]
- Farina, H.G.; Pomies, M.; Alonso, D.F.; Gomez, D.E. Antitumor and antiangiogenic activity of soy isoflavone genistein in mouse models of melanoma and breast cancer. Oncol. Rep. 2006, 16, 885–891. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Huang, R.; Zhang, S.; Lin, J.; Wei, L.; He, M.; Zhuo, L.; Lin, X. Protective effect of genistein isolated from Hydrocotyle sibthorpioides on hepatic injury and fibrosis induced by chronic alcohol in rats. Toxicol. Lett. 2013, 217, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Schrader, C.; Ernst, I.M.; Sinnecker, H.; Soukup, S.T.; Kulling, S.E.; Rimbach, G. Genistein as a potential inducer of the anti-atherogenic enzyme paraoxonase-1: Studies in cultured hepatocytes in vitro and in rat liver in vivo. J. Cell Mol. Med. 2012, 16, 2331–2341. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.F.; XU, Y.J.; YUAN, B.; WANG, L.L.; Lin, L.Q.; Xu, H.Y. Synthesis of genistein sulfates and effects of genistein and its sulfates on proliferation of breast cancer cells. Shizhen Guoyi Guoyao 2011, 22, 284–286. [Google Scholar]
- Rimbach, G.; Weinberg, P.D.; de Pascual-Teresa, S.; Alonso, M.G.; Ewins, B.A.; Turner, R.; Minihane, A.M.; Botting, N.; Fairley, B.; Matsugo, S.; et al. Sulfation of genistein alters its antioxidant properties and its effect on platelet aggregation and monocyte and endothelial function. Biochim. Biophys. Acta. 2004, 1670, 229–237. [Google Scholar] [CrossRef] [PubMed]

| No. | tR (min) | Formula (M) | Ion | Meas. (m/z) | Pred. (m/z) | Diff (ppm) | DBE | Identification | Plasma | Urine | Feces |
|---|---|---|---|---|---|---|---|---|---|---|---|
| F1 ♥ | 58.602 | C16H12O5 | [M − H]− | 283.0623 | 283.0612 | 3.89 | 11 | Calycosin | ▲ | ▲ | |
| F2 | 77.588 | C16H12O5 | [M + H]+ | 285.0753 | 285.0758 | −1.75 | 11 | Calycosin isomer 1 | ▲ | ||
| F3 * | 56.485 | C16H12O5 | [M − H]− | 283.0608 | 283.0612 | −1.41 | 11 | Calycosin isomer 2 | ▲ | ||
| F4 ♥ | 27.200 | C22H22O10 | [M + HCOO]− | 491.1215 | 491.1195 | 4.07 | 12 | Calycosin-7-O-glucoside | ▲ | ▲ | |
| F5 ♥ | 47.743 | C22H22O9 | [M + H]+ | 431.1322 | 431.1337 | −3.48 | 12 | Ononin | ▲ | ▲ | |
| F6 ♥ | 71.750 | C16H12O4 | [M − H]− | 267.0673 | 267.0663 | 3.74 | 11 | Formononetin | ▲ | ▲ | ▲ |
| F7 * | 66.802 | C16H12O6 | [M − H]− | 299.0569 | 299.0561 | 2.68 | 11 | Pratensein/Rhamnocitrin/5,7,4’-trihydroxy-3’-methoxyisoflavone | ▲ | ||
| F8 * | 68.197 | C16H12O6 | [M − H]− | 299.0576 | 299.0561 | 5.02 | 11 | Pratensein/Rhamnocitrin/5,7,4’-trihydroxy-3’-methoxyisoflavone | ▲ | ||
| F9 | 65.018 | C15H12O5 | [M − H]− | 271.0622 | 271.0612 | 3.69 | 10 | Trihydroxy-dihydroisoflavone/flavone | ▲ | ||
| F10 | 44.750 | C15H14O5 | [M − H]− | 273.0777 | 273.0768 | 3.30 | 9 | Trihydroxy-tetrahydroisoflavone/flavone | ▲ | ||
| F11 | 54.377 | C15H10O4 | [M − H]− | 253.0514 | 253.0506 | 3.16 | 11 | Daidzein | ▲ | ||
| F12 | 55.485 | C15H12O4 | [M − H]− | 255.0675 | 255.0663 | 4.70 | 10 | Trihydroxychalcone | ▲ | ▲ | |
| F13 | 65.627 | C15H10O5 | [M − H]− | 269.0452 | 269.0455 | −1.12 | 11 | Trihydroxyisoflavone/flavone | ▲ | ||
| F14 | 60.827 | C17H14O6 | [M + H]+ | 315.0882 | 315.0863 | 6.03 | 11 | Odoratin isomer | ▲ | ||
| F15 | 57.460 | C17H18O5 | [M + H]+ | 303.1216 | 303.1227 | −3.63 | 9 | Astraisoflavane isomer | ▲ | ||
| F16 | 65.852 | C17H16O6 | [M + H]+ | 317.1040 | 317.1020 | 6.31 | 10 | Dihydroxy dimethoxyisoflavone/flavone | ▲ | ||
| F17 ♥ | 73.328 | C17H16O5 | [M + H]+ | 301.1052 | 301.1071 | −6.31 | 10 | Astraptercarpan | ▲ | ▲ | |
| F18 | 35.440 | C27H32O14 | [M − H]− | 579.1748 | 579.1719 | 5.01 | 12 | Naringin | |||
| F19 | 34.635 | C28H36O13 | [M − H]− | 579.2103 | 579.2083 | 3.45 | 11 | Dihydrocalycosin pentose glucoside | |||
| F20 | 51.837 | C28H34O14 | [M − H]− | 593.1899 | 593.1876 | 3.88 | 12 | Astrapterocarpan pentose glucoside | |||
| F21 | 63.302 | C16H14O5 | [M + H]+ | 287.0927 | 287.0914 | 4.53 | 10 | 3,10-dihydroxy-9-methoxypterocarpan | |||
| F22 | 60.812 | C22H22O11 | [M − H]− | 461.1114 | 461.1089 | 5.42 | 12 | Pratensein glucoside/5,7’,4’-trihydroxy-3’-methoxyisoflavone glucoside | |||
| F23 | 22.332 | C22H22O11 | [M − H]− | 461.1112 | 461.1089 | 4.99 | 12 | Pratensein glucoside/5,7’,4’-trihydroxy-3’-methoxyisoflavone glucoside | |||
| Sum | 3 | 17 | 4 | ||||||||
| NO. | tR(min) | Formula (M) | Ion | Meas. (m/z) | Pred. (m/z) | Diff (ppm) | DBE | Identification | Urine | Plasma | Feces |
|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 △ | 19.500 | C7H6O5S | [M − H]− | 200.9862 | 200.9863 | −0.50 | 5 | Hydroxyl-benzaladehyde sulfate or isomer | ▲ | ||
| M2 △ | 10.948 | C7H8O6S | [M − H]− | 218.9967 | 218.9969 | −0.91 | 4 | Methyl pyrogallol sulfate or isomer | ▲ | ||
| M3 △ | 20.550 | C8H8O6S | [M − H]− | 230.9961 | 230.9969 | −3.46 | 5 | Hydroxyphenylacetic acid sulfate | ▲ | ||
| M4 △ | 28.350 | C8H8O6S | [M − H− | 230.9963 | 230.9969 | −2.6 | 5 | Hydroxyphenylacetic acid sulfate isomer | ▲ | ||
| M5 △ | 21.008 | C9H8O6S | [M − H]− | 242.9978 | 242.9969 | 3.7 | 6 | Hydroxycinnamic acid sulfate 1 | ▲ | ▲ | |
| M6 △ | 23.533 | C9H8O6S | [M − H]− | 242.9960 | 242.9969 | −3.70 | 6 | Hydroxycinnamic acid sulfate 2 | ▲ | ||
| M7 △ | 55.018 | C10H12O5S | [M − H]− | 243.0345 | 243.0333 | 4.94 | 5 | Eugenol sulfate | ▲ | ||
| M8 △ | 36.100 | C8H8O7S | [M − H]− | 246.9921 | 246.9918 | 1.21 | 5 | Vanillic acid sulfate | ▲ | ||
| M9 △ | 19.617 | C9H12O6S | [M − H]− | 247.0281 | 247.0282 | −0.40 | 4 | Homovanillyl alcohol sulfate | ▲ | ||
| M10 △ | 20.383 | C10H10O7S | [M − H]− | 273.0080 | 273.0074 | 2.20 | 6 | Ferulic Acid sulfate | ▲ | ||
| M11 △ | 58.818 | C11H14O6S | [M − H]− | 273.0436 | 273.0438 | −0.73 | 5 | Methoxyeugenol sulfate 1 | ▲ | ||
| M12 △ | 55.593 | C11H14O6S | [M − H]− | 273.0433 | 273.0438 | −1.83 | 5 | Methoxyeugenol sulfate 2 | ▲ | ▲ | |
| M13 △ | 43.617 | C11H12O7S | [M − H]− | 287.0237 | 287.0231 | 2.09 | 6 | C11H12O4 sulfate | ▲ | ||
| M14 △ | 23.750 | C11H14O7S | [M − H]− | 289.0393 | 289.0387 | 2.08 | 5 | Ethylhomovanillic acid sulfate 1 | ▲ | ▲ | |
| M15 △ | 26.642 | C11H14O7S | [M − H]− | 289.0397 | 289.0387 | 3.46 | 5 | Ethylhomovanillic acid sulfate 2 | ▲ | ▲ | |
| M16 △ | 27.558 | C11H12O8 S | [M − H]− | 303.0173 | 303.018 | −2.31 | 6 | 3’,5’-dimethoxy-4’-hydroxycinnamic acid sulfate | ▲ | ▲ | |
| M17 | 80.230 | C16H12O5 | [M − H]− | 283.0604 | 283.0612 | −2.83 | 11 | Calycosin isomer 1 | ▲ | ||
| M18 △ | 65.833 | C16H12O5 | [M + H]+ | 285.0767 | 285.0758 | 3.16 | 11 | Calycosin isomer 2 | ▲ | ||
| M19 △ | 31.508 | C16H12O5 | [M + H]+ | 285.0738 | 285.0758 | −7.02 | 11 | Calycosin isomer 3 | ▲ | ▲ | |
| M20 △ | 79.592 | C16H12O5 | [M + H]+ | 285.0777 | 285.0758 | 6.66 | 11 | Calycosin isomer 4 | ▲ | ||
| M21 | 51.610 | C16H12O6 | [M + H]+ | 301.0688 | 301.0707 | −6.31 | 11 | Hydroxycalycosin | ▲ | ||
| M22 | 54.902 | C17H14O6 | [M + H]+ | 315.0883 | 315.0863 | 6.35 | 11 | Methoxycalycosin 1 | ▲ | ||
| M23 | 34.517 | C17H14O6 | [M + H]+ | 315.0836 | 315.0863 | −8.57 | 11 | Methoxycalycosin 2 | ▲ | ||
| M24 | 61.477 | C17H14O6 | [M + H]+ | 315.0840 | 315.0863 | −7.3 | 11 | Methoxycalycosin 3 | ▲ | ||
| M25 | 31.483 | C16H12O8S | [M − H]- | 363.0178 | 363.0180 | −0.55 | 11 | Calycosin sulfate 1 | ▲ | ▲ | |
| M26 | 47.512 | C16H12O8S | [M − H]− | 363.018 | 363.0180 | 0 | 11 | Calycosin sulfate 2 | ▲ | ▲ | |
| M27 | 51.168 | C16H12O8S | [M − H]− | 363.0187 | 363.0180 | 1.93 | 11 | Calycosin sulfate isomer 1 | ▲ | ▲ | |
| M28 △ | 67.248 | C16H12O8S | [M − H]− | 363.0174 | 363.0180 | −1.65 | 11 | Calycosin sulfate isomer 2 | ▲ | ||
| M29 △ | 44.867 | C16H12O8S | [M − H]− | 363.0189 | 363.0180 | 2.48 | 11 | Calycosin sulfate isomer 3 | ▲ | ▲ | |
| M30 △ | 79.697 | C16H12O8S | [M − H]− | 363.0193 | 363.0180 | 3.58 | 11 | Calycosin sulfate isomer 4 | ▲ | ||
| M31 △ | 33.158 | C16H12O11S2 | [M − H]− | 442.9767 | 442.9748 | 4.29 | 11 | Calycosin-7,3’-O-disulfate | ▲ | ▲ | |
| M32 △ | 36.133 | C22H20O11 | [M − H]− | 459.0952 | 459.0933 | 4.14 | 13 | Calycosin-3’-O-glucuronide | ▲ | ▲ | |
| M33 △ | 23.417 | C22H20O14S | [M − H]− | 539.0538 | 539.0501 | 6.86 | 13 | Calycosin glucuronide sulfate 1 | ▲ | ||
| M34 △ | 31.245 | C22H20O14S | [M − H]− | 539.0519 | 539.0501 | 3.34 | 13 | Calycosin glucuronide sulfate 2 | ▲ | ▲ | |
| M35 | 71.298 | C16H12O9S | [M − H]− | 379.0137 | 379.0129 | 2.11 | 11 | Hydroxycalycosin sulfate 1 | ▲ | ▲ | |
| M36 | 57.743 | C16H12O9S | [M − H]- | 379.0153 | 379.0129 | 6.33 | 11 | Hydroxycalycosin sulfate 2 | ▲ | ||
| M37 | 61.243 | C16H12O9S | [M − H]− | 379.0151 | 379.0129 | 5.80 | 11 | Hydroxycalycosin sulfate 3 | ▲ | ||
| M38 △ | 26.125 | C22H20O12 | [M − H]− | 475.0847 | 475.0882 | −7.37 | 13 | Hydroxycalycosin glucuronide 1 | ▲ | ||
| M39 △ | 51.610 | C22H20O12 | [M − H]− | 475.0918 | 475.0882 | 7.58 | 13 | Hydroxycalycosin glucuronide 2 | ▲ | ||
| M40 △ | 39.042 | C23H22O12 | [M − H]− | 489.1063 | 489.1038 | 5.11 | 13 | Methoxycalycosin glucuronide | ▲ | ▲ | |
| M41 △ | 33.123 | C23H22O15S | [M − H]− | 569.0634 | 569.0607 | 4.74 | 13 | Methoxycalycosin glucuronide sulfate | ▲ | ▲ | |
| M42 △ | 20.108 | C28H30O16 | [M − H]− | 621.1451 | 621.1461 | −1.61 | 14 | Calycosin-7-O-glucoside-3’-O-glucuronide | ▲ | ||
| M43 | 48.258 | C16H14O8S | [M − H]− | 365.0341 | 365.0337 | 1.1 | 10 | Dihydrocalycosin sulfate 1 | ▲ | ||
| M44 | 43.285 | C16H14O8S | [M − H]− | 365.0346 | 365.0337 | 2.47 | 10 | Dihydrocalycosin sulfate 2 | ▲ | ||
| M45 | 45.652 | C16H14O8S | [M − H]− | 365.0356 | 365.0337 | 5.2 | 10 | Dihydrocalycosin sulfate 3 | ▲ | ▲ | |
| M46 △ | 38.098 | C22H22O11 | [M − H]− | 461.1111 | 461.1089 | 4.77 | 12 | Dihydrocalycosin glucuronide | ▲ | ||
| M47 | 57.285 | C16H14O9S | [M − H]− | 381.0282 | 381.0286 | −1.05 | 10 | Hydroxy dihydrocalycosin sulfate 1 | ▲ | ▲ | |
| M48 | 93.980 | C16H14O9S | [M − H]− | 381.0296 | 381.0286 | 2.62 | 10 | Hydroxy dihydrocalycosin sulfate 2 | ▲ | ||
| M49 | 49.422 | C16H14O9S | [M − H]− | 381.0300 | 381.0286 | 3.67 | 10 | Hydroxy dihydrocalycosin sulfate 3 | ▲ | ▲ | |
| M50 | 39.792 | C18H18O8S | [M − H]− | 393.0665 | 393.065 | 3.82 | 10 | Dimethyl dihydrocalycosin sulfate | ▲ | ||
| M51 △ | 52.118 | C17H16O9S | [M − H]− | 395.0434 | 395.0442 | −2.03 | 10 | Methoxy dihydrocalycosin sulfate 1 | ▲ | ▲ | |
| M52 △ | 68.430 | C17H16O9S | [M − H]− | 395.0457 | 395.0442 | 3.80 | 10 | Methoxy dihydrocalycosin sulfate 2 | ▲ | ||
| M53 | 66.472 | C16H14O10S | [M − H]− | 397.0251 | 397.0235 | 4.03 | 10 | Dihydroxyl dihydrocalycosin sulfate | ▲ | ||
| M54 | 25.252 | C16H16O8S | [M − H]− | 367.0477 | 367.0493 | −4.36 | 9 | Tetrahydrocalycosin sulfate 1 | ▲ | ||
| M55 | 19.342 | C16H16O8S | [M − H]− | 367.0496 | 367.0493 | 0.82 | 9 | Tetrahydrocalycosin sulfate 2 | ▲ | ||
| M56 | 21.443 | C16H16O8S | [M − H]− | 367.0500 | 367.0493 | 1.91 | 9 | Tetrahydrocalycosin sulfate 3 | ▲ | ||
| M57 | 50.593 | C16H16O8S | [M − H]− | 367.0516 | 367.0493 | 6.27 | 9 | Tetrahydrocalycosin sulfate 4 | ▲ | ▲ | |
| M58 | 67.630 | C16H16O8S | [M − H]− | 367.0517 | 367.0493 | 6.54 | 9 | Tetrahydrocalycosin sulfate 5 | ▲ | ▲ | |
| M59 | 57.860 | C16H16O8S | [M − H]− | 367.0518 | 367.0493 | 6.81 | 9 | Tetrahydrocalycosin sulfate 6 | ▲ | ||
| M60 △ | 34.182 | C22H24O11 | [M − H]− | 463.1257 | 463.1246 | 2.38 | 11 | Tetrahydrocalycosin glucuronide 1 | ▲ | ▲ | |
| M61 △ | 54.027 | C22H24O11 | [M − H]− | 463.1269 | 463.1246 | 4.97 | 11 | Tetrahydrocalycosin glucuronide 2 | ▲ | ▲ | |
| M62 △,★ | 26.975 | C22H24O14S | [M − H]− | 543.0792 | 543.0814 | −4.05 | 11 | Tetrahydrocalycosin glucuronide sulfate | ▲ | ||
| M63 △,★ | 32.350 | C28H32O17 | [M − H]− | 639.1607 | 639.1567 | 6.26 | 13 | Tetrahydrocalycosin diglucuronide | ▲ | ||
| M64 | 48.375 | C16H16O9S | [M − H]− | 383.0449 | 383.0442 | 1.83 | 9 | Hydroxy tetrahydrocalycosin sulfate 1 | ▲ | ||
| M65 | 25.200 | C16H16O9S | [M − H]− | 383.046 | 383.0442 | 4.70 | 9 | Hydroxy tetrahydrocalycosin sulfate 2 | ▲ | ▲ | |
| M66 | 64.843 | C16H16O9S | [M − H]− | 383.0462 | 383.0442 | 5.22 | 9 | Hydroxy tetrahydrocalycosin sulfate 3 | ▲ | ||
| M67 | 40.192 | C16H16O9S | [M − H]− | 383.0467 | 383.0442 | 6.53 | 9 | Hydroxy tetrahydrocalycosin sulfate 4 | ▲ | ||
| M68 | 30.608 | C16H16O9S | [M − H]− | 383.0444 | 383.0442 | 0.52 | 9 | Hydroxy tetrahydrocalycosin sulfate 5 | ▲ | ||
| M69 △,★ | 27.617 | C16H16O12S2 | [M − H]− | 463.0031 | 463.0010 | 4.75 | 9 | Hydroxy tetrahydrocalycosin disulfate | ▲ | ||
| M70 △,★ | 45.733 | C18H20O10S | [M − H]− | 427.0716 | 427.0704 | 2.81 | 9 | Dihydroxy dihydrocalycosin sulfate | ▲ | ||
| M71 △ | 56.593 | C24H28O12 | [M − H]− | 507.1535 | 507.1508 | 5.32 | 11 | Dimethyl hydroxy tetrahydrocalycosin glucuronide 1 | ▲ | ▲ | |
| M72 △ | 54.727 | C24H28O12 | [M − H]− | 507.1539 | 507.1508 | 6.11 | 11 | Dimethyl hydroxy tetrahydrocalycosin glucuronide 2 | ▲ | ▲ | |
| M73 △ | 71.300 | C16H12O7S | [M − H]− | 347.0228 | 347.0231 | −0.86 | 11 | Formononetin-7-O-sulfate | ▲ | ▲ | |
| M74 △ | 49.357 | C22H20O10 | [M − H]- | 443.0977 | 443.0984 | −1.58 | 13 | Formononetin-7-O-glucuronide | ▲ | ||
| M75 | 21.960 | C16H16O7S | [M − H]− | 351.0537 | 351.0544 | −1.99 | 9 | Tetrahydroformononetin sulfate 1 | ▲ | ||
| M76 | 59.352 | C16H16O7S | [M − H]− | 351.0554 | 351.0544 | 2.85 | 9 | Tetrahydroformononetin sulfate 2 | ▲ | ▲ | |
| M77 | 59.860 | C16H16O7S | [M − H]− | 351.0564 | 351.0544 | 5.70 | 9 | Tetrahydroformononetin sulfate 3 | ▲ | ||
| M78 △ | 49.257 | C22H24O10 | [M − H]− | 447.1322 | 447.1297 | 5.59 | 11 | Tetrahydroformononetin glucuronide | ▲ | ▲ | |
| M79 △ | 69.797 | C17H16O8S | [M − H]− | 379.0509 | 379.0493 | 4.22 | 10 | Astrapterocarpan-3-O-sulfate | ▲ | ||
| M80 △ | 56.043 | C23H24O11 | [M − H]− | 475.1276 | 475.1246 | 6.31 | 12 | Astrapterocarpan-3-O-glucuronide | ▲ | ▲ | |
| M81 | 31.018 | C18H18O6 | [M − H]− | 329.1027 | 329.1031 | −1.22 | 10 | Methoxyastrapterocarpan | ▲ | ||
| M82 △ | 53.593 | C23H24O12 | [M − H]− | 491.1225 | 491.1195 | 6.11 | 12 | Hydroxyastrapterocarpan glucuronide 1 | ▲ | ||
| M83 △ | 40.915 | C23H24O12 | [M − H]− | 491.1194 | 491.1195 | −0.20 | 12 | Hydroxyastrapterocarpan glucuronide 2 | ▲ | ||
| M84 △ | 43.618 | C23H24O12 | [M − H]− | 491.1173 | 491.1195 | −4.48 | 12 | Hydroxyastrapterocarpan glucuronide 3 | ▲ | ||
| M85 △ | 35.667 | C17H18O5 | [M +H]+ | 303.1205 | 303.1227 | −7.26 | 9 | Astraisoflavan isomer | ▲ | ||
| M86 △ | 32.868 | C18H20O5 | [M − H]− | 315.1228 | 315.1238 | −3.17 | 9 | Methoxyastraisoflavan | ▲ | ||
| M87 △ | 37.802 | C18H20O5 | [M − H]− | 315.1235 | 315.1238 | −0.95 | 9 | Methoxyastraisoflavan isomer | ▲ | ||
| M88 △ | 34.368 | C19H22O6 | [M − H]- | 345.1360 | 345.1344 | 4.64 | 9 | Hydroxy dimethoxyastraisoflavan | ▲ | ||
| M89 | 59.918 | C17H18O8S | [M − H]− | 381.0639 | 381.0650 | −2.89 | 9 | Astraisoflavan-7-O-sulfate | ▲ | ||
| M90 | 62.510 | C17H18O8S | [M − H]− | 381.0660 | 381.0650 | 2.62 | 9 | Astraisoflavan-2’-O-sulfate | ▲ | ▲ | |
| M91 | 34.427 | C17H18O8S | [M − H]− | 381.0662 | 381.0650 | 3.15 | 9 | Astraisoflavan sulfate isomer | ▲ | ||
| M92 △ | 34.993 | C18H20O8S | [M − H]− | 395.0795 | 395.0806 | −2.78 | 9 | Methyoxyastraisoflavan sulfate 1 | ▲ | ||
| M93 △ | 30.460 | C18H20O8S | [M − H]− | 395.0819 | 395.0806 | 3.29 | 9 | Methyoxyastraisoflavan sulfate 2 | ▲ | ▲ | |
| M94 | 20.252 | C17H18O9S | [M − H]− | 397.0602 | 397.0599 | 0.76 | 9 | Hydroxyastraisoflavan sulfate 1 | ▲ | ||
| M95 | 49.543 | C17H18O9S | [M − H]− | 397.0603 | 397.0599 | 1.01 | 9 | Hydroxyastraisoflavan sulfate 2 | ▲ | ||
| M96 | 44.008 | C17H18O9S | [M − H]− | 397.0608 | 397.0599 | 2.27 | 9 | Hydroxyastraisoflavan sulfate 3 | ▲ | ▲ | |
| M97 △ | 51.435 | C17H18O9S | [M − H]− | 397.0614 | 397.0599 | 3.78 | 9 | Hydroxyastraisoflavan sulfate 4 | ▲ | ||
| M98 △ | 68.372 | C17H18O9S | [M − H]− | 397.0620 | 397.0599 | 5.29 | 9 | Hydroxyastraisoflavan sulfate 5 | ▲ | ||
| M99 △ | 18.817 | C17H18O9S | [M − H]− | 397.0622 | 397.0599 | 5.79 | 9 | Hydroxyastraisoflavan sulfate 6 | ▲ | ||
| M100 △ | 62.393 | C18H20O9S | [M − H]− | 411.0743 | 411.0755 | −2.92 | 9 | Methoxyastraisoflavan sulfate 1 | ▲ | ||
| M101 △ | 60.210 | C18H20O9S | [M − H]− | 411.0758 | 411.0755 | 0.73 | 9 | Methoxyastraisoflavan sulfate 2 | ▲ | ||
| M102 △ | 58.702 | C23H26O11 | [M − H]− | 477.1429 | 477.1402 | 5.66 | 11 | Astraisoflavan-7-O-glucuronide | ▲ | ||
| M103 △ | 56.868 | C23H26O11 | [M − H]− | 477.1430 | 477.1402 | 5.87 | 11 | Astraisoflavan-2’-O-glucuronide | ▲ | ▲ | |
| M104 △,★ | 38.250 | C23H26O14S | [M − H]− | 557.0997 | 557.0970 | 4.85 | 11 | Astraisoflavan glucuronide sulfate 1 | ▲ | ||
| M105 △,★ | 52.510 | C23H26O14S | [M − H]− | 557.1001 | 557.0970 | 5.56 | 11 | Astraisoflavan glucuronide sulfate 2 | ▲ | ||
| M106 △ | 35.633 | C29H36O16 | [M − H]− | 639.1949 | 639.1931 | 2.82 | 12 | Astraisoflavan-7-O-glucoside-2’-O-glucuronide | ▲ | ▲ | |
| M107 | 41.557 | C15H10O7S | [M − H]− | 333.0074 | 333.0074 | 0 | 11 | Daidzein-4’-O-sulfate | ▲ | ▲ | |
| M108 | 28.925 | C15H10O7S | [M − H]− | 333.0080 | 333.0074 | 1.80 | 11 | Daidzein-7-O-sulfate | ▲ | ||
| M109 △ | 28.400 | C15H10O10S2 | [M − H]− | 412.9658 | 412.9643 | 3.63 | 11 | Daidzein-7,4’-O-disulfate | ▲ | ▲ | |
| M110 △ | 23.817 | C21H18O10 | [M − H]− | 429.0835 | 429.0827 | 1.86 | 13 | Daidzein glucuronide | ▲ | ||
| M111 △ | 20.167 | C21H18O13S | [M − H]− | 509.0403 | 509.0395 | 1.57 | 13 | Daidzein glucuronide sulfate | ▲ | ||
| M112 △ | 44.292 | C15H12O7S | [M − H]− | 335.0212 | 335.0231 | −5.67 | 10 | Dihydrodaidzein sulfate | ▲ | ||
| M113 | 53.852 | C15H14O7S | [M − H]− | 337.0389 | 337.0387 | 0.59 | 9 | Tetrahydrodaidzein sulfate 1 | ▲ | ||
| M114 | 39.333 | C15H14O7S | [M − H]− | 337.0400 | 337.0387 | 3.86 | 9 | Tetrahydrodaidzein sulfate 2 | ▲ | ||
| M115 | 57.002 | C15H14O7S | [M − H]− | 337.0402 | 337.0387 | 4.45 | 9 | Tetrahydrodaidzein sulfate 3 | ▲ | ▲ | |
| M116 | 60.560 | C15H14O7S | [M − H]− | 337.0409 | 337.0387 | 6.53 | 9 | Tetrahydrodaidzein sulfate 4 | ▲ | ||
| M117 △ | 34.458 | C15H14O10S2 | [M − H]− | 416.9988 | 416.9956 | 7.67 | 9 | Tetrahydrodaidzein disulfate | ▲ | ||
| M118 | 40.017 | C15H10O5 | [M + H]+ | 271.0617 | 271.0601 | 5.90 | 11 | Gensitein | ▲ | ||
| M119 | 41.833 | C15H10O8S | [M − H]− | 349.0033 | 349.0024 | 2.58 | 11 | Genistein sulfate 1 | ▲ | ||
| M120 | 57.918 | C15H10O8S | [M − H]− | 349.0039 | 349.0024 | 4.30 | 11 | Genistein sulfate 2 | ▲ | ||
| M121 | 37.233 | C15H10O8S | [M − H]− | 349.0030 | 349.0024 | 1.72 | 11 | Genistein sulfate 3 | ▲ | ||
| M122 △ | 25.042 | C21H18O14S | [M − H]− | 525.0367 | 525.0370 | −0.57 | 9 | Genistein glucuronide sulfate | ▲ | ||
| M123 | 33.658 | C15H12O8S | [M − H]− | 351.0180 | 351.0180 | 0 | 10 | Dihydrogenistein sulfate 1 | ▲ | ||
| M124 △ | 74.098 | C15H12O8S | [M − H]− | 351.0184 | 351.0180 | 1.14 | 10 | Dihydrogenistein sulfate 2 | ▲ | ||
| M125 △ | 51.688 | C15H12O8S | [M − H]− | 351.0189 | 351.018 | 2.56 | 10 | Dihydrogenistein sulfate 3 | ▲ | ||
| M126 | 44.758 | C15H14O5 | [M − H]− | 273.0757 | 273.0768 | −4.03 | 9 | Tetrahydrogenistein | ▲ | ||
| M127 | 63.985 | C15H14O8S | [M − H]− | 353.0359 | 353.0337 | 6.23 | 9 | Tetrahydrogenistein sulfate 1 | ▲ | ▲ | |
| M128 | 65.410 | C15H14O8S | [M − H]− | 353.0360 | 353.0337 | 6.51 | 9 | Tetrahydrogenistein sulfate 2 | ▲ | ||
| M129 △,★ | 49.090 | C20H22O12S | [M − H]− | 485.0787 | 485.0759 | 5.77 | 10 | Tetrahydrogenistein pentose sulfate | ▲ | ||
| M130 △,★ | 39.850 | C21H24O13S | [M − H]− | 515.0911 | 515.0865 | 8.93 | 10 | Tetrahydrogenistin sulfate | ▲ | ||
| M131 | 62.235 | C15H14O6S | [M − H]− | 321.0439 | 321.0438 | 0.31 | 9 | Equol sulfate isomer | ▲ | ||
| M132 | 56.152 | C15H14O6S | [M − H]− | 321.0444 | 321.0438 | 1.87 | 9 | Equol sulfate 1 | ▲ | ▲ | |
| M133 | 58.943 | C15H14O6S | [M − H]− | 321.0454 | 321.0438 | 4.98 | 9 | Equol sulfate 2 | ▲ | ||
| M134 △ | 46.017 | C21H22O9 | [M − H]− | 417.1185 | 417.1191 | −1.44 | 11 | Equol glucuronide 1 | ▲ | ▲ | |
| M135 △ | 47.975 | C21H22O9 | [M − H]− | 417.1209 | 417.1191 | 4.32 | 11 | Equol glucuronide 2 | ▲ | ▲ | |
| M136 △,★ | 32.293 | C21H22O12S | [M − H]− | 497.0786 | 497.0759 | 5.43 | 11 | Equol glucuronide sulfate 1 | ▲ | ||
| M137 △,★ | 28.058 | C21H22O12S | [M − H]− | 497.0797 | 497.0759 | 7.64 | 11 | Equol glucuronide sulfate 2 | ▲ | ||
| M138 △ | 37.317 | C21H22O12S | [M − H]− | 497.0757 | 497.0759 | -0.4 | 11 | Equol glucuronide sulfate 3 | ▲ | ||
| M139 △ | 57.977 | C15H16O6S | [M − H]− | 323.0616 | 323.0595 | 6.5 | 8 | Dihydroequol sulfate | ▲ | ||
| M140 | 28.817 | C16H14O6 | [M + H]+ | 303.0878 | 303.0863 | 4.95 | 10 | Dihydropratensein | ▲ | ||
| M141 △ | 24.925 | C22H20O15S | [M − H]− | 555.0487 | 555.0450 | 6.67 | 13 | Pratensein glucuronide sulfate | ▲ | ||
| M142 △,★ | 26.300 | C27H30O17 | [M − H]− | 625.1462 | 625.1410 | 8.32 | 13 | Tetrahydro trihydroxyisoflavone diglucuronide 1 | ▲ | ||
| M143 △,★ | 26.867 | C27H30O17 | [M − H]− | 625.1467 | 625.1410 | 9.12 | 13 | Tetrahydro trihydroxyisoflavone diglucuronide 2 | ▲ | ||
| M144 △ | 41.650 | C15H14O9S | [M − H]− | 369.0303 | 369.0286 | 4.61 | 9 | Tetrahydro-tetrahydroxyisoflavone sulfate | ▲ | ||
| M145 △ | 41.930 | C22H20O15S | [M − H]− | 555.0478 | 555.0450 | 6.76 | 13 | Pratensein glucuronide sulfate | |||
| M146 △ | 61.012 | C22H20O11 | [M − H]− | 459.0925 | 459.0933 | −1.23 | 13 | Calycosin-7-O-glucuronide | |||
| M147 △ | 69.988 | C17H18O8S | [M − H]− | 381.0652 | 381.0650 | 0.52 | 9 | Astraisoflavan sulfate isomer | |||
| Sum | 106 | 64 | 17 | ||||||||
Sample Availability
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, L.-J.; Li, H.-F.; Xu, F.; Wang, H.-Y.; Zhang, Y.-F.; Liu, G.-X.; Shang, M.-Y.; Wang, X.; Cai, S.-Q. Exploring the In Vivo Existence Forms (23 Original Constituents and 147 Metabolites) of Astragali Radix Total Flavonoids and Their Distributions in Rats Using HPLC-DAD-ESI-IT-TOF-MSn. Molecules 2020, 25, 5560. https://doi.org/10.3390/molecules25235560
Liu L-J, Li H-F, Xu F, Wang H-Y, Zhang Y-F, Liu G-X, Shang M-Y, Wang X, Cai S-Q. Exploring the In Vivo Existence Forms (23 Original Constituents and 147 Metabolites) of Astragali Radix Total Flavonoids and Their Distributions in Rats Using HPLC-DAD-ESI-IT-TOF-MSn. Molecules. 2020; 25(23):5560. https://doi.org/10.3390/molecules25235560
Chicago/Turabian StyleLiu, Li-Jia, Hong-Fu Li, Feng Xu, Hong-Yan Wang, Yi-Fan Zhang, Guang-Xue Liu, Ming-Ying Shang, Xuan Wang, and Shao-Qing Cai. 2020. "Exploring the In Vivo Existence Forms (23 Original Constituents and 147 Metabolites) of Astragali Radix Total Flavonoids and Their Distributions in Rats Using HPLC-DAD-ESI-IT-TOF-MSn" Molecules 25, no. 23: 5560. https://doi.org/10.3390/molecules25235560
APA StyleLiu, L.-J., Li, H.-F., Xu, F., Wang, H.-Y., Zhang, Y.-F., Liu, G.-X., Shang, M.-Y., Wang, X., & Cai, S.-Q. (2020). Exploring the In Vivo Existence Forms (23 Original Constituents and 147 Metabolites) of Astragali Radix Total Flavonoids and Their Distributions in Rats Using HPLC-DAD-ESI-IT-TOF-MSn. Molecules, 25(23), 5560. https://doi.org/10.3390/molecules25235560





