Kallikrein-11, in Association with Coiled-Coil Domain Containing 25, as a Potential Prognostic Marker for Cholangiocarcinoma with Lymph Node Metastasis
Abstract
:1. Introduction
2. Results
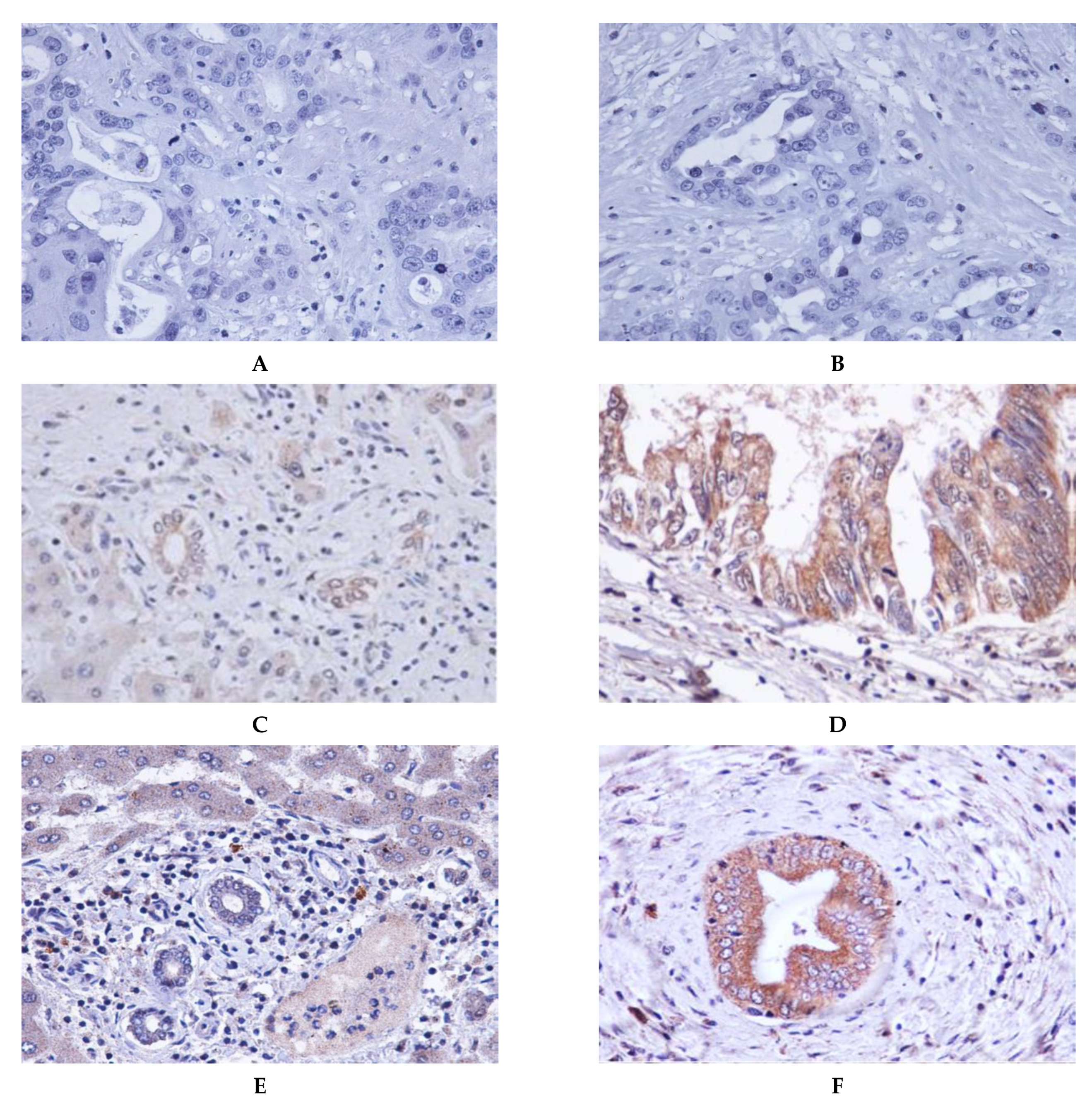
2.1. Expression of CCDC25 and KLK11 in Cholangiocarcinoma Tissue
2.2. Expression of CCDC25 and KLK11 in Cholangiocarcinoma with or without Lymph Node Metastasis
2.3. Correlation between CCDC25 and KLK11 Expression in Cancerous Tissues
2.4. Associations between CCDC25 and KLK11 Expression in CCA Tissues with the Overall Survival Time of Patients
2.5. CCDC25 and KLK11 mRNA Expressions in CCA Tissue and Overall Survival Time of CCA Patients Using GEPIA
2.6. Potential Protein–Protein Interaction Analysis
3. Discussion
4. Materials and Methods
4.1. Patients and Specimens
4.2. Immunohistochemistry
4.3. Immunohistochemical Evaluation of CCDC25 and KLK11 Expressions in CCA Tissues
4.4. Evaluation of CCDC25 and KLK11 Expression in Tissue and Overall Survival Time
4.5. Prediction of CCDC25 and Signaling Pathway
4.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Vatanasapt, V.; Uttaravichien, T.; Mairiang, E.O.; Pairojkul, C.; Chartbanchachai, W.; Haswell-Elkins, M. Cholangiocarcinoma in north-east Thailand. Lancet 1990, 335, 116–117. [Google Scholar] [CrossRef]
- Sripa, B.; Pairojkul, C. Cholangiocarcinoma: Lessons from Thailand. Curr. Opin. Gastroenterol. 2008, 24, 349–356. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.Y.; Shiesh, S.C.; Tsao, H.C.; Lin, X.Z. The assessment of biliary CA 125, CA 19-9 and CEA in diagnosing cholangiocarcinoma-The influence of sampling time and hepatolithiasis. Hepato-Gastroenterology 2002, 49, 616–620. [Google Scholar]
- Ong, S.L.; Sachdeva, A.; Garcea, G.; Gravante, G.; Metcalfe, M.S.; Lloyd, D.M.; Berry, D.P.; Dennison, A.R. Elevation of carbohydrate antigen 19.9 in benign hepatobiliary conditions and its correlation with serum bilirubin concentration. Dig. Dis. Sci. 2008, 53, 3213–3217. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, S.; Gores, G.J. Pathogenesis, diagnosis, and management of cholangiocarcinoma. Gastroenterology 2013, 145, 1215–1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Proungvitaya, S.; Klinthong, W.; Proungvitaya, T.; Limpaiboon, T.; Jearanaikoon, P.; Roytrakul, S.; Wongkham, C.; Nimboriboonporn, A.; Wongkham, S. High expression of CCDC25 in cholangiocarcinoma tissue samples. Oncol. Lett. 2017, 14, 2566–2572. [Google Scholar] [CrossRef] [Green Version]
- Chanakankun, R.; Proungvitaya, T.; Chua-On, D.; Limpaiboon, T.; Roytrakul, S.; Jusakul, A.; Titapun, A.; Jarearnrat, A.; Proungvitaya, S. Serum coiled-coil domain containing 25 protein as a potential screening/diagnostic biomarker for cholangiocarcinoma. Oncol. Lett. 2020, 19, 930–942. [Google Scholar] [CrossRef] [PubMed]
- Chanakankun, R. Binding Proteins Profiling for Prediction of CCDC25 Function in Cholangiocarcinoma. Master’ Thesis, Khon Kaen University, Khon Kaen, Thailand, 28 November 2018. [Google Scholar]
- Zhang, Y.; Xu, Z.; Sun, Y.; Chi, P.; Lu, X. Knockdown of KLK11 reverses oxaliplatin resistance by inhibiting proliferation and activating apoptosis via suppressing the PI3K/AKT signal pathway in colorectal cancer cell. Onco Targets Ther. 2018, 11, 809–821. [Google Scholar] [CrossRef] [Green Version]
- Liu, R.; Zhao, E.; Wang, F.; Cui, H. CCDC25: Precise navigator for neutrophil extracellular traps on the prometastatic road. Signal Transduct. Target. Ther. 2020, 5, 162. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Liu, Q.; Zhang, X.; Liu, X.; Zhou, B.; Chen, J.; Huang, D.; Li, J.; Li, H.; Chen, F.; et al. DNA of neutrophil extracellular traps promotes cancer metastasis via CCDC25. Nature 2020, 583, 133–138. [Google Scholar] [CrossRef]
- Dickson, I. NETs promote liver metastasis via CCDC25. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 451. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Tang, H.Y.; Li, X.R.; He, X.W.; Xiang, K.M. Over-expression of human kallikrein 11 is associated with poor prognosis in patients with low rectal carcinoma. Med. Oncol. 2010, 27, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Albrengues, J.; Shields, M.A.; Ng, D.; Park, C.G.; Ambrico, A.; Poindexter, M.E.; Upadhyay, P.; Uyeminami, D.L.; Pommier, A.; Küttner, V.; et al. Neutrophil extracellular traps produced during inflammation awaken dormant cancer cells in mice. Science 2018, 361, 4227. [Google Scholar] [CrossRef] [Green Version]
- Xu, Z.; Chi, P.; Pan, J.; Shen, S.; Sun, Y.; Wang, X.; Lu, X. Knockdown of KLK11 inhibits cell proliferation and increases oxaliplatin sensitivity in human colorectal cancer. Exp. Ther. Med. 2016, 12, 2855–2860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolin, D.L.; Sy, K.; Rotondo, F.; Bassily, M.N.; Kovacs, K.; Brezden-Masley, C.; Streutker, C.J.; Yousef, G.M. Prognostic significance of human tissue kallikrein-related peptidases 11 and 15 in gastric cancer. Tumor. Biol. 2016, 37, 437–446. [Google Scholar] [CrossRef]
- Shigemasa, K.; Gu, L.; Tanimoto, H.; O’Brien, T.J.; Ohama, K. Human Kallikrein Gene 11 (KLK11) mRNA Overexpression Is Associated with Poor Prognosis in Patients with Epithelial Ovarian Cancer. Clin. Cancer Res. 2004, 10, 2766–2770. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, H.; Fang, W.; Liu, M.; Fu, D. Complement component 1, q subcomponent binding protein (C1QBP) in lipid rafts mediates hepatic metastasis of pancreatic cancer by regulating IGF-1/IGF-1R signaling. Int. J. Cancer 2017, 141, 1389–1401. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Zhang, F.; Guo, L.; Wang, Y.; Zhang, P.; Wang, R.; Zhang, N.; Chen, R. Interactome analysis reveals that C1QBP (complement component 1, q subcomponent binding protein) is associated with cancer cell chemotaxis and metastasis. Mol. Cell Proteom. 2013, 12, 3199–3209. [Google Scholar] [CrossRef] [Green Version]
- Quesada-Calvo, F.; Massot, C.; Bertrand, V.; Longuespée, R.; Blétard, N.; Somja, J.; Mazzucchelli, G.; Smargiasso, N.; Baiwir, D.; Pauw-Gillet, M.-C.D.; et al. OLFM4, KNG1 and SEC24C identified by proteomics and immunohistochemistry as potential markers of early colorectal cancer stages. Clin. Proteom. 2017, 14, 9. [Google Scholar] [CrossRef] [Green Version]
- Dimri, M.; Satyanarayana, A. Molecular signaling pathways and therapeutic targets in hepatocellular carcinoma. Cancers 2020, 12, 491. [Google Scholar] [CrossRef] [Green Version]
- Ye, M.X.; Li, Y.; Yin, H.; Zhang, J. Curcumin: Updated molecular mechanisms and intervention targets in human lung cancer. Int. J. Mol. Sci. 2012, 13, 3959–3978. [Google Scholar] [CrossRef]
- Lee, H.S.; Kim, W.H.; Kwak, Y.; Koh, J.; Bae, J.M.; Kim, K.M.; Chang, M.S.; Han, H.S.; Kim, J.M.; Kim, H.W.; et al. Molecular testing for gastrointestinal cancer. J. Pathol. Transl. Med. 2017, 51, 103–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freudlsperger, C.; Burnett, J.R.; Friedman, J.A.; Kannabiran, V.R.; Chen, Z.; Van, W.C. EGFR-PI3K-AKT-mTOR signaling in head and neck squamous cell carcinomas: Attractive targets for molecular-oriented therapy. Expert Opin. Ther. Targets 2011, 15, 63–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seystahl, K.; Tritschler, I.; Szabo, E.; Tabatabai, G.; Weller, M. Differential regulation of TGF-β 2-induced, ALK-5-mediated VEGF release by SMAD2/3 versus SMAD1/5/8 signaling in glioblastoma. Neuro Oncol. 2015, 17, 254–265. [Google Scholar] [CrossRef]
- Caja, L.; Bertran, E.; Campbell, J.; Fausto, N.; Fabregat, I. The transforming growth factor-beta (TGF-β) mediates acquisition of a mesenchymal stem cell-like phenotype in human liver cells. J. Cell Physiol. 2011, 226, 1214–1223. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.; Lv, A.; Deng, Q.; Zhang, G.; Hu, X.; Cui, H. TROP2 promotes the proliferation and metastasis of glioblastoma cells by activating the JAK2/STAT3 signaling pathway. Oncol. Rep. 2019, 41, 753–764. [Google Scholar] [CrossRef] [Green Version]
- Kryza, T.; Silva, M.L.; Loessner, D.; Heuzé-Vourc’h, N.; Clements, J.A. The kallikrein-related peptidase family: Dysregulation and functions during cancer progression. Biochimie 2016, 122, 283–299. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Zhang, H.; Xie, F.; Tao, D.; Xiao, X.; Huang, C.; Wang, M.; Gu, C.; Zhang, X.; Jiang, G. Hsa_circ_0001361 promotes bladder cancer invasion and metastasis through miR-491-5p/MMP9 axis. Oncogene 2020, 39, 1696–1709. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.J.; Wang, N.; Sun, Z.W.; Chen, J.; Cui, H.W. MiR-5692a promotes the invasion and metastasis of hepatocellular carcinoma via MMP9. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 4869–4878. [Google Scholar] [PubMed]
- Pan, S.; Hu, Y.; Hu, M.; Jian, H.; Chen, M.; Gan, L.; Zheng, P.; He, Y.; Wang, J. Platelet-derived PDGF promotes the invasion and metastasis of cholangiocarcinoma by upregulating MMP2/MMP9 expression and inducing EMT via the p38/MAPK signalling pathway. Am. J. Transl. Res. 2020, 12, 3577–3595. [Google Scholar]
- Wang, X.; Yang, B.; She, Y.; Ye, Y. The lncRNA TP73-AS1 promotes ovarian cancer cell proliferation and metastasis via modulation of MMP2 and MMP9. J. Cell Biochem. 2018, 119, 7790–7799. [Google Scholar] [CrossRef]
- Serrano, I.; Mcdonald, P.C.; Lock, F.E.; Dedhar, S. Role of the integrin-linked kinase (ILK)/Rictor complex in TGFβ-1-induced epithelial-mesenchymal transition (EMT). Oncogene 2013, 32, 50–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erdfelder, E.; Faul, F.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar]
- Kim, S.W.; Roh, J.; Park, C.S. Immunohistochemistry for pathologists: Protocols, pitfalls, and tips. J. Pathol. Transl. Med. 2016, 50, 411–418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pierceall, W.E.; Wolfe, M.; Suschak, J.; Chang, H.; Chen, Y.; Sprott, K.M.; Kutok, J.L.; Quan, S.; Weaver, D.T.; Ward, B.E. Strategies for H-score normalization of preanalytical technical variables with potential utility to immunohistochemical-based biomarker quantitation in therapeutic reponse diagnostics. Anal. Cell. Pathol. 2011, 34, 159–168. [Google Scholar] [CrossRef]
- Tang, Z.; Li, C.; Kang, B.; Gao, G.; Li, C.; Zhang, Z. GEPIA: A web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 2017, 45, W98–W102. [Google Scholar] [CrossRef] [Green Version]
- Szklarczyk, D.; Gable, A.L.; Lyon, D.; Junge, A.; Wyder, S.; Huerta-Cepas, J.; Simonovic, M.; Doncheva, N.T.; Morris, J.H.; Bork, P.; et al. STRING v11: Protein-protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res. 2019, 47, D607–D613. [Google Scholar] [CrossRef] [Green Version]







Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siriphak, S.; Chanakankun, R.; Proungvitaya, T.; Roytrakul, S.; Tummanatsakun, D.; Seubwai, W.; Wongwattanakul, M.; Proungvitaya, S. Kallikrein-11, in Association with Coiled-Coil Domain Containing 25, as a Potential Prognostic Marker for Cholangiocarcinoma with Lymph Node Metastasis. Molecules 2021, 26, 3105. https://doi.org/10.3390/molecules26113105
Siriphak S, Chanakankun R, Proungvitaya T, Roytrakul S, Tummanatsakun D, Seubwai W, Wongwattanakul M, Proungvitaya S. Kallikrein-11, in Association with Coiled-Coil Domain Containing 25, as a Potential Prognostic Marker for Cholangiocarcinoma with Lymph Node Metastasis. Molecules. 2021; 26(11):3105. https://doi.org/10.3390/molecules26113105
Chicago/Turabian StyleSiriphak, Saeranee, Ravinnipa Chanakankun, Tanakorn Proungvitaya, Sittiruk Roytrakul, Doungdean Tummanatsakun, Wunchana Seubwai, Molin Wongwattanakul, and Siriporn Proungvitaya. 2021. "Kallikrein-11, in Association with Coiled-Coil Domain Containing 25, as a Potential Prognostic Marker for Cholangiocarcinoma with Lymph Node Metastasis" Molecules 26, no. 11: 3105. https://doi.org/10.3390/molecules26113105
APA StyleSiriphak, S., Chanakankun, R., Proungvitaya, T., Roytrakul, S., Tummanatsakun, D., Seubwai, W., Wongwattanakul, M., & Proungvitaya, S. (2021). Kallikrein-11, in Association with Coiled-Coil Domain Containing 25, as a Potential Prognostic Marker for Cholangiocarcinoma with Lymph Node Metastasis. Molecules, 26(11), 3105. https://doi.org/10.3390/molecules26113105






