Differential Expression of Yersinia pseudotuberculosis General Porin Genes during Short- and Long-Term Antibiotic Stresses
Abstract
:1. Introduction
2. Results and Discussion
2.1. Antibiotics and Y. pseudotuberculosis 488 Susceptibility
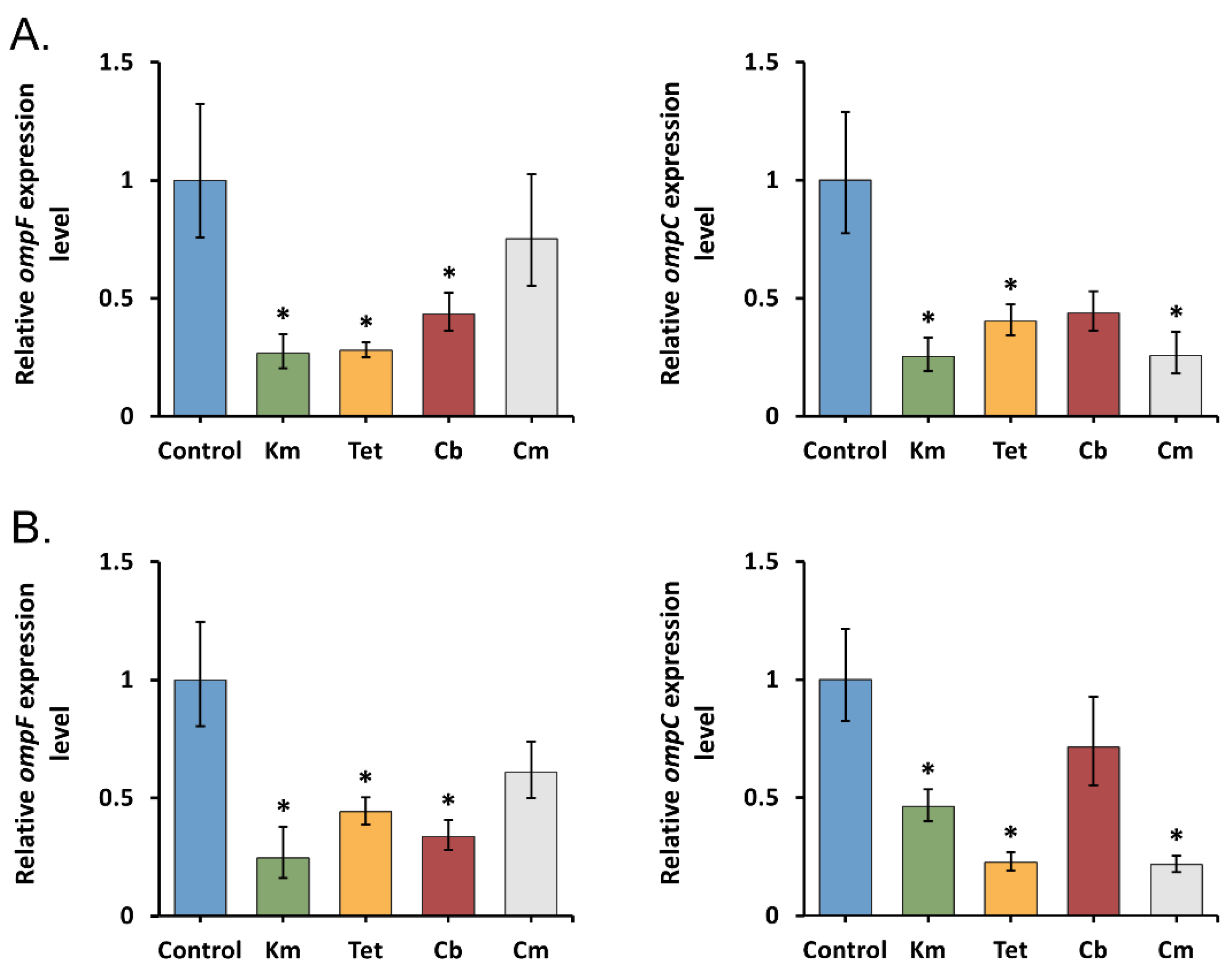
2.2. An Early Transcriptional Response of General Porin Genes to Antibiotic Stress
2.3. Transcriptional Response of General Porin Genes to Prolonged Antibiotic Stress
2.4. ompR and marA Effect on Porin Response under Antibiotic Stress
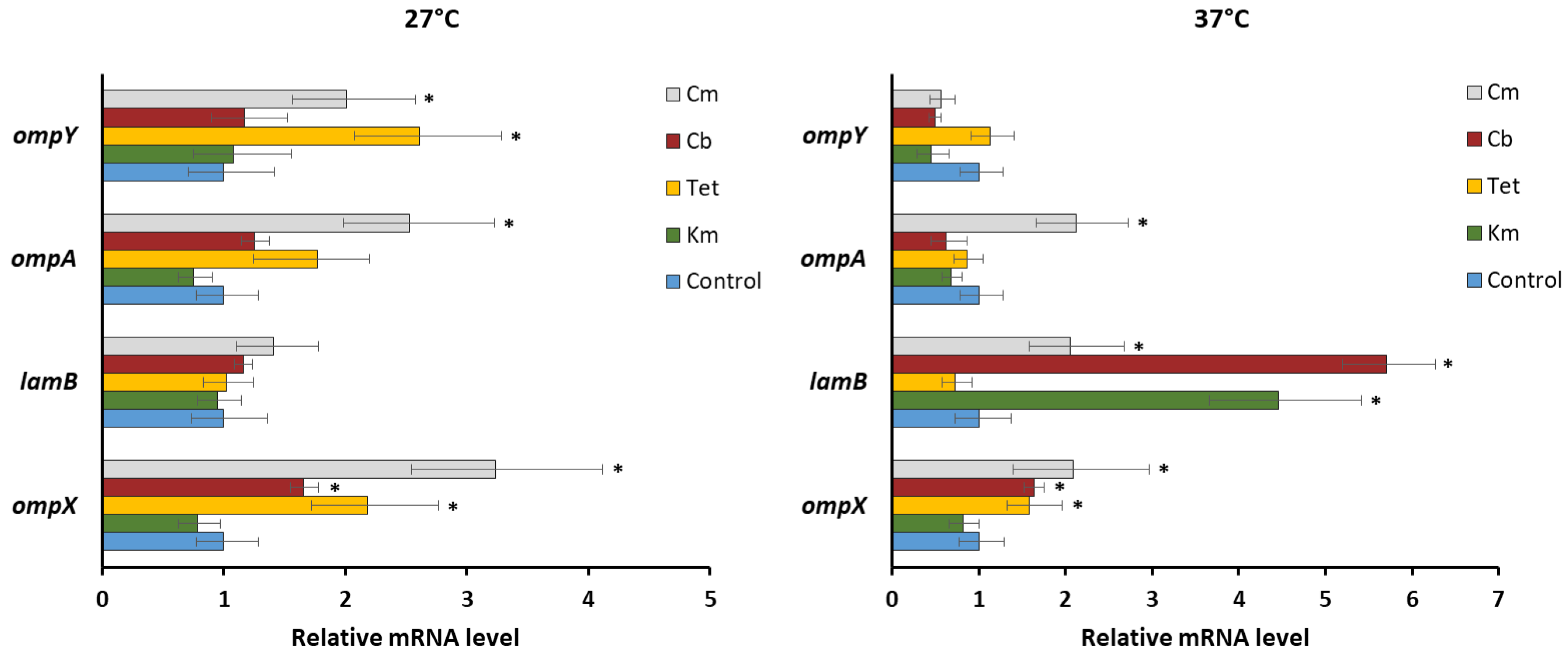
2.5. Transcriptional Response of Y. pseudotuberculosis Alternative Porins to Prolonged Antibiotic Stress
2.6. ompF and ompC Expression within Y. pseudotuberculosis Population
3. Materials and Methods
3.1. Bacterial Strain and Growth Conditions
3.2. MIC Determination
3.3. Gene Expression Measurement by qRT-PCR
3.4. Porin Gene Sequencing
3.5. GFP Reporter System Construction
3.6. Flow Cytometry
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fernandez, L.; Hancock, R.E. Adaptive and mutational resistance: Role of porins and efflux pumps in drug resistance. Clin. Microbiol. Rev. 2012, 25, 661–681. [Google Scholar] [CrossRef] [Green Version]
- Andersson, D.I.; Hughes, D. Microbiological effects of sublethal levels of antibiotics. Nat. Rev. Microbiol. 2014, 12, 465–478. [Google Scholar] [CrossRef]
- Braoudaki, M.; Hilton, A.C. Adaptive resistance to biocides in Salmonella enterica and Escherichia coli o157 and cross-resistance to antimicrobial agents. J. Clin. Microbiol. 2004, 42, 73–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daikos, G.L.; Lolans, V.T.; Jackson, G.G. First-exposure adaptive resistance to aminoglycoside antibiotics in vivo with meaning for optimal clinical use. Antimicrob. Agents Chemother. 1991, 35, 117–123. [Google Scholar] [CrossRef] [Green Version]
- Viveiros, M.; Jesus, A.; Brito, M.; Leandro, C.; Martins, M.; Ordway, D.; Molnar, A.M.; Molnar, J.; Amaral, L. Inducement and reversal of tetracycline resistance in Escherichia coli K-12 and the expression of proton gradient dependent multidrug efflux pump genes. Antimicrob. Agents Chemother. 2005, 49, 3578–3582. [Google Scholar] [CrossRef] [Green Version]
- Somova, L.M.; Antonenko, F.F.; Timchenko, N.F.; Lyapun, I.N. Far Eastern Scarlet-Like Fever is a Special Clinical and Epidemic Manifestation of Yersinia pseudotuberculosis Infection in Russia. Pathogens 2020, 9, 436. [Google Scholar] [CrossRef]
- Bystritskaya, E.P.; Stenkova, A.M.; Portnyagina, O.Y.; Rakin, A.V.; Rasskazov, V.A.; Isaeva, M.P. Regulation of Yersinia pseudotuberculosis major porin expression in response to antibiotic stress. Mol. Gen. Microbiol. Virol. 2014, 29, 63–68. [Google Scholar] [CrossRef]
- Khomenko, V.A.; Portnyagina, O.Y.; Novikova, O.D.; Isaeva, M.P.; Kim, N.Y.; Likhatskaya, G.N.; Vostrikova, O.P.; Solov’eva, T.F. Isolation and characterization of recombinant OmpF-like porin from the Yersinia pseudotuberculosis outer membrane. Russ. J. Bioorg. Chem. 2008, 34, 162–168. [Google Scholar] [CrossRef]
- Novikova, O.D.; Khomenko, V.A.; Emelyanenko, V.I.; Likhatskaya, G.N.; Zelepuga, E.A.; Kim, N.Y.; Isaeva, M.P.; Portnyagina, O.Y.; Vostrikova, O.P.; Sidorova, O.V.; et al. OmpC-like porin from Yersinia pseudotuberculosis: Molecular characteristics, physico-chemical and functional properties. Biochem. Suppl. Ser. A Membr. Cell Biol. 2011, 5, 263–277. [Google Scholar]
- Stenkova, A.M.; Isaeva, M.P.; Shubin, F.N.; Rasskazov, V.A.; Rakin, A.V. Trends of the major porin gene (OmpF) evolution: Insight from the genus Yersinia. PLoS ONE 2011, 6, e20546. [Google Scholar] [CrossRef] [Green Version]
- Stenkova, A.M.; Bystritskaya, E.P.; Guzev, K.V.; Rakin, A.V.; Isaeva, M.P. Molecular Evolution of the Yersinia Major Outer Membrane Protein C (OmpC). Evol. Bioinform. 2016, 12, 185–191. [Google Scholar] [CrossRef] [Green Version]
- Cowan, S.W.; Schirmer, T.; Rummel, G.; Steiert, M.; Ghosh, R.; Pauptit, R.A.; Jansonius, J.N.; Rosenbusch, J.P. Crystal structures explain functional properties of two E. coli porins. Nature 1992, 358, 727–733. [Google Scholar] [CrossRef]
- James, C.E.; Mahendran, K.R.; Molitor, A.; Bolla, J.-M.; Bessonov, A.N.; Winterhalter, M.; Pagès, J.-M. How beta-lactam antibiotics enter bacteria: A dialogue with the porins. PLoS ONE 2009, 4, e5453. [Google Scholar] [CrossRef]
- Bafna, J.A.; Sans-Serramitjana, E.; Acosta-Gutiérrez, S.; Bodrenko, I.V.; Hörömpöli, D.; Berscheid, A.; Brötz-Oesterhelt, H.; Winterhalter, M.; Ceccarelli, M. Kanamycin uptake into Escherichia coli is facilitated by OmpF and OmpC porin channels located in the outer membrane. ACS Infect. Dis. 2020, 6, 1855–1865. [Google Scholar] [CrossRef]
- Neves, P.; Berkane, E.; Gameiro, P.; Winterhalter, M.; De Castro, B. Interaction between quinolones antibiotics and bacterial outer membrane porin OmpF. Biophys. Chem. 2005, 113, 123–128. [Google Scholar] [CrossRef]
- Mortimer, P.G.; Piddock, L.J. The accumulation of five antibacterial agents in porin-deficient mutants of Escherichia coli. J. Antimicrob. Chemother. 1993, 32, 195–213. [Google Scholar] [CrossRef]
- Masi, M.; Réfrigiers, M.; Pos, K.M.; Pagès, J.M. Mechanisms of envelope permeability and antibiotic influx and efflux in Gram-negative bacteria. Nat. Microbiol. 2017, 2, 17001. [Google Scholar] [CrossRef] [PubMed]
- Sousa, A.M.; Machado, I.; Pereira, M.O. Phenotypic switching: An opportunity to bacteria thrive. In Science Against Microbial Pathogens: Communicating Current Research and Technological Advances; Formatex Research Center: Badajoz, Spain, 2012; pp. 252–262. [Google Scholar]
- Dupont, M.; James, C.E.; Chevalier, J.; Pagès, J.-M. An Early Response to Environmental Stress Involves Regulation of OmpX and OmpF, Two Enterobacterial Outer Membrane Pore-Forming Proteins. Antimicrob. Agents Chemother. 2007, 51, 3190–3198. [Google Scholar] [CrossRef] [Green Version]
- Doménech-Sánchez, A.; Hernández-Allés, S.; Martínez-Martínez, L.; Benedí, V.J.; Albertí, S. Identification and characterization of a new porin gene of Klebsiella pneumoniae: Its role in beta-lactam antibiotic resistance. J. Bacteriol. 1999, 181, 2726–2732. [Google Scholar] [CrossRef] [Green Version]
- Knopp, M.; Andersson, D.I. Amelioration of the fitness costs of antibiotic resistance due to reduced outer membrane permeability by upregulation of alternative porins. Mol. Biol. Evol. 2015, 32, 3252–3263. [Google Scholar] [CrossRef] [Green Version]
- Chetri, S.; Singha, M.; Bhowmik, D.; Nath, K.; Chanda, D.D.; Chakravarty, A.; Bhattacharjee, A. Transcriptional response of OmpC and OmpF in Escherichia coli against differential gradient of carbapenem stress. BMC Res. Notes 2019, 12, 138. [Google Scholar] [CrossRef]
- Dam, S.; Pagès, J.-M.; Masi, M. Stress responses, outer membrane permeability control and antimicrobial resistance in Enterobacteriaceae. Microbiology 2018, 164, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Viveiros, M.; Dupont, M.; Rodrigues, L.; Couto, I.; Davin-Regli, A.; Martins, M.; Pagès, J.-M.; Amaral, L. Antibiotic stress, genetic response and altered permeability of E. coli. PLoS ONE 2007, 2, e365. [Google Scholar] [CrossRef]
- Deighan, P.; Free, A.; Dorman, C.J. A role for the Escherichia coli H-NS-like protein StpA in OmpF porin expression through modulation of micF RNA stability. Mol. Microbiol. 2000, 38, 126–139. [Google Scholar] [CrossRef] [Green Version]
- Andersen, J.; Forst, S.A.; Zhao, K.; Inouye, M.; Delihas, N. The function of micF RNA. micF RNA is a major factor in the thermal regulation of OmpF protein in Escherichia coli. J. Biol. Chem. 1989, 264, 17961–17970. [Google Scholar] [CrossRef]
- Begic, S.; Worobec, E.A. Regulation of Serratia marcescens ompF and ompC porin genes in response to osmotic stress, salicylate, temperature and pH. Microbiology 2006, 152, 485–491. [Google Scholar] [CrossRef] [Green Version]
- Bystritskaya, E.; Stenkova, A.; Chistuylin, D.; Chernysheva, N.; Khomenko, V.; Anastyuk, S.; Novikova, O.; Rakin, A.; Isaeva, M. Adaptive responses of outer membrane porin balance of Yersinia ruckeri under different incubation temperature, osmolarity, and oxygen availability. Microbiologyopen 2016, 5, 597–603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Narimisa, N.; Amraei, F.; Kalani, B.S.; Mohammadzadeh, R.; Jazi, F.M. Effects of sub-inhibitory concentrations of antibiotics and oxidative stress on the expression of type II toxin-antitoxin system genes in Klebsiella pneumoniae. J. Glob. Antimicrob. Resist. 2020, 21, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.-F.; Jiang, B.; Xiang, Z.-M.; Wang, S.-Y. Functional characterisation of altered outer membrane proteins for tetracycline resistance in Escherichia coli. Int. J. Antimicrob. Agents 2008, 32, 315–319. [Google Scholar] [CrossRef]
- Chang, C.C.; Yan, C.W.; Onal, R.; Zhang, Y. Genetic characterization and investigation of kanamycin susceptibility of ompC and ompF single gene deletion mutants of Escherichia coli K-12. J. Exp. Microbiol. Immunol. 2018, 22, 1–9. [Google Scholar]
- Hu, W.-C.; MacDonald, R.; Oosthuizen, J.L.; Soeren, M.V. Sub-inhibitory kanamycin changes outer membrane porin ratios in Escherichia coli B23 by increasing the level of OmpC. J. Exp. Microbiol. Immunol. 2011, 15, 96–102. [Google Scholar]
- Fei, Y.; Ma, V.; Maerkl, N.; You, P. The down regulation of E. coli OmpF in response to sub-inhibitory concentrations of kanamycin is not mediated by MarA. J. Exp. Microbiol. Immunol. 2012, 16, 101–107. [Google Scholar]
- Agafitei, O.; Kim, E.J.; Maguire, T.; Sheridan, J. The role of Escherichia coli porins OmpC and OmpF in antibiotic cross resistance induced by sub-inhibitory concentrations of kanamycin. J. Exp. Microbiol. Immunol. 2010, 14, 34–39. [Google Scholar]
- Choi, U.; Lee, C.-R. Distinct roles of outer membrane porins in antibiotic resistance and membrane integrity in Escherichia coli. Front. Microbiol. 2019, 10, 953. [Google Scholar] [CrossRef]
- Moya-Torres, A.; Mulvey, M.R.; Kumar, A.; Oresnik, I.J.; Brassinga, A.K. The lack of OmpF, but not OmpC, contributes to increased antibiotic resistance in Serratia marcescens. Microbiology 2014, 160 Pt 9, 1882–1892. [Google Scholar] [CrossRef]
- Igwe, J.C.; Olayinka, B.O.; Ehnimidu, J.O.; Onaolapo, J.A. Impact of outer membrane protein Ompc and Ompf on antibiotics resistance of E. coli isolated from UTI and diarrhoeic patients in Zaria, Nigeria. Clin. Microbiol. 2016, 5, 1000267. [Google Scholar]
- Toro, C.S.; Lobos, S.R.; Calderón, I.; Rodríguez, M.; Mora, G.C. Clinical isolate of a porinless Salmonella typhi resistant to high levels of chloramphenicol. Antimicrob. Agents. Chemother. 1990, 34, 1715–1719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fajardo-Lubián, A.; Zakour, N.L.B.; Agyekum, A.; Qi, Q.; Iredell, J.R. Host adaptation and convergent evolution increases antibiotic resistance without loss of virulence in a major human pathogen. PLoS Pathog. 2019, 15, e1007218. [Google Scholar] [CrossRef] [Green Version]
- Ferenci, T.; Phan, K. How porin heterogeneity and trade-offs affect the antibiotic susceptibility of Gram-Negative bacteria. Genes 2015, 6, 1113–1124. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.; Ferenci, T. Regulation of porin-mediated outer membrane permeability by nutrient limitation in Escherichia coli. J. Bacteriol. 1998, 180, 3917–3922. [Google Scholar] [CrossRef] [Green Version]
- Tierney, A.R.; Rather, P.N. Roles of two-component regulatory systems in antibiotic resistance. Future Microbiol. 2019, 14, 533–552. [Google Scholar] [CrossRef] [PubMed]
- Flamez, C.; Ricard, I.; Arafah, S.; Simonet, M.; Marceau, M. Phenotypic analysis of Yersinia pseudotuberculosis 32777 response regulator mutants: New insights into two-component system regulon plasticity in bacteria. Int. J. Med. Microbiol. 2008, 298, 193–207. [Google Scholar] [CrossRef]
- Nieckarz, M.; Raczkowska, A.; Jaworska, K.; Stefańska, E.; Skorek, K.; Stosio, D.; Brzostek, K. The role of OmpR in the expression of genes of the KdgR regulon involved in the uptake and depolymerization of oligogalacturonides in Yersinia enterocolitica. Front. Cell Infect. Microbiol. 2017, 7, 366. [Google Scholar] [CrossRef]
- Raczkowska, A.; Trzos, J.; Lewandowska, O.; Nieckarz, M.; Brzostek, K. Expression of the AcrAB components of the AcrAB-TolC multidrug efflux pump of Yersinia enterocolitica is subject to dual regulation by OmpR. PLoS ONE 2015, 10, e0124248. [Google Scholar] [CrossRef]
- Masi, M.; Pagès, J.-M. Structure, function and regulation of outer membrane proteins involved in drug transport in Enterobactericeae: The OmpF/C—TolC case. Open Microbiol. J. 2013, 7, 22–33. [Google Scholar] [CrossRef] [Green Version]
- Cohen, S.P.; McMurry, L.M.; Levy, S.B. MarA locus causes decreased expression of OmpF porin in multiple-antibiotic-resistant (Mar) mutants of Escherichia coli. J. Bacteriol. 1988, 170, 5416–5422. [Google Scholar] [CrossRef] [Green Version]
- Lister, I.M.; Mecsas, J.; Levy, S.B. Effect of MarA-like proteins on antibiotic resistance and virulence in Yersinia pestis. Infect. Immun. 2010, 78, 364–371. [Google Scholar] [CrossRef] [Green Version]
- Udani, R.A.; Levy, S.B. MarA-like regulator of multidrug resistance in Yersinia pestis. Antimicrob. Agents Chemother. 2006, 50, 2971–2975. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dupont, M.; Dé, E.; Chollet, R.; Chevalier, J.; Pagès, J.-M. Enterobacter aerogenes OmpX, a cation-selective channel mar- and osmo-regulated. FEBS Lett. 2004, 569, 27–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castillo-Keller, M.; Vuong, P.; Misra, R. Novel mechanism of Escherichia coli porin regulation. J. Bacteriol. 2006, 188, 576–586. [Google Scholar] [CrossRef] [Green Version]
- Gayet, S.; Chollet, R.; Molle, G.; Pagès, J.-M.; Chevalier, J. Modification of outer membrane protein profile and evidence suggesting an active drug pump in Enterobacter aerogenes clinical strains. Antimicrob. Agents Chemother. 2003, 47, 1555–1559. [Google Scholar] [CrossRef] [Green Version]
- Solov’eva, T.F.; Likhatskaya, G.N.; Khomenko, V.A.; Stenkova, A.M.; Kim, N.Y.; Portnyagina, O.Y.; Novikova, O.D.; Trifonov, E.V.; Nurminski, E.A.; Isaeva, M.P. A novel OmpY porin from Yersinia pseudotuberculosis: Structure, channel-forming activity and trimer thermal stability. J. Biomol. Struct. Dyn. 2011, 28, 517–533. [Google Scholar] [CrossRef]
- Dam, S.; Pagès, J.-M.; Masi, M. Dual Regulation of the small RNA MicC and the quiescent porin OmpN in response to antibiotic stress in Escherichia coli. Antibiotics 2017, 6, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ambriz-Aviña, V.; Contreras-Garduño, J.A.; Pedraza-Reyes, M. Applications of flow cytometry to characterize bacterial physiological responses. BioMed Res. Int. 2014, 2014, 461941. [Google Scholar] [CrossRef]
- de Jong, I.G.; Veening, J.-W.; Kuipers, O.P. Single cell analysis of gene expression patterns during carbon starvation in Bacillus subtilis reveals large phenotypic variation. Environ. Microbiol. 2012, 14, 3110–3121. [Google Scholar] [CrossRef]
- Sánchez-Romero, M.A.; Casadesús, J. Contribution of phenotypic heterogeneity to adaptive antibiotic resistance. Proc. Natl. Acad. Sci. USA 2014, 111, 355–360. [Google Scholar] [CrossRef] [Green Version]
- Magdanova, L.A.; Golyasnaya, N.V. Heterogeneity as an adaptive trait of microbial populations. Microbiology 2013, 82, 1–10. [Google Scholar] [CrossRef]
- Erickson, K.E.; Otoupal, P.B.; Chatterjee, A. Gene expression variability underlies adaptive resistance in phenotypically heterogeneous bacterial populations. ACS Infect. Dis. 2015, 1, 555–673. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bystritskaya, E.; Chernysheva, N.; Stenkova, A.; Guzev, K.; Rakin, A.; Isaeva, M. Differential Expression of Yersinia pseudotuberculosis General Porin Genes during Short- and Long-Term Antibiotic Stresses. Molecules 2021, 26, 3956. https://doi.org/10.3390/molecules26133956
Bystritskaya E, Chernysheva N, Stenkova A, Guzev K, Rakin A, Isaeva M. Differential Expression of Yersinia pseudotuberculosis General Porin Genes during Short- and Long-Term Antibiotic Stresses. Molecules. 2021; 26(13):3956. https://doi.org/10.3390/molecules26133956
Chicago/Turabian StyleBystritskaya, Evgeniya, Nadezhda Chernysheva, Anna Stenkova, Konstantin Guzev, Alexander Rakin, and Marina Isaeva. 2021. "Differential Expression of Yersinia pseudotuberculosis General Porin Genes during Short- and Long-Term Antibiotic Stresses" Molecules 26, no. 13: 3956. https://doi.org/10.3390/molecules26133956
APA StyleBystritskaya, E., Chernysheva, N., Stenkova, A., Guzev, K., Rakin, A., & Isaeva, M. (2021). Differential Expression of Yersinia pseudotuberculosis General Porin Genes during Short- and Long-Term Antibiotic Stresses. Molecules, 26(13), 3956. https://doi.org/10.3390/molecules26133956





