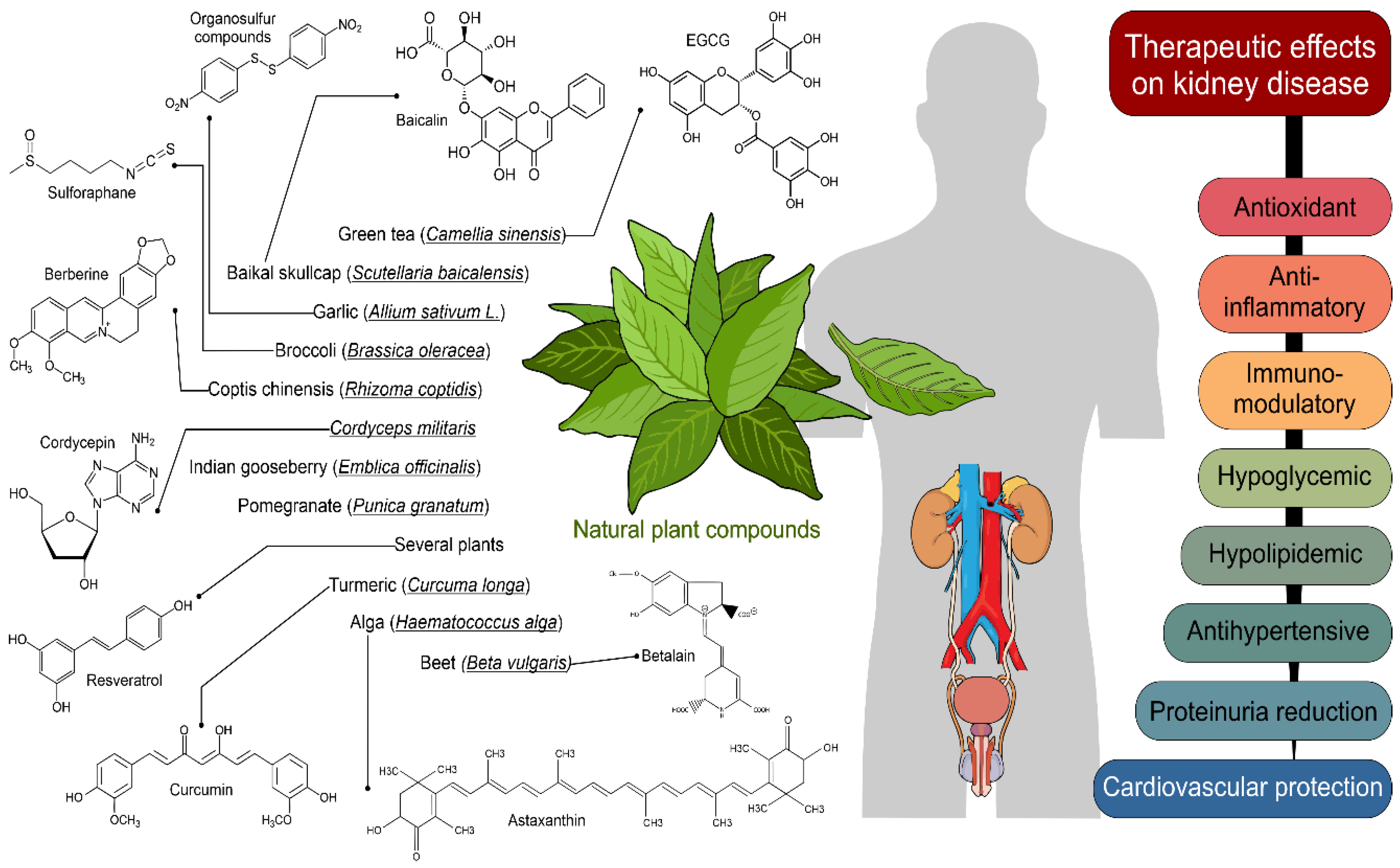
Potential Therapeutic Effects of Natural Plant Compounds in Kidney Disease
Abstract
:1. Introduction
2. Methods
3. Results
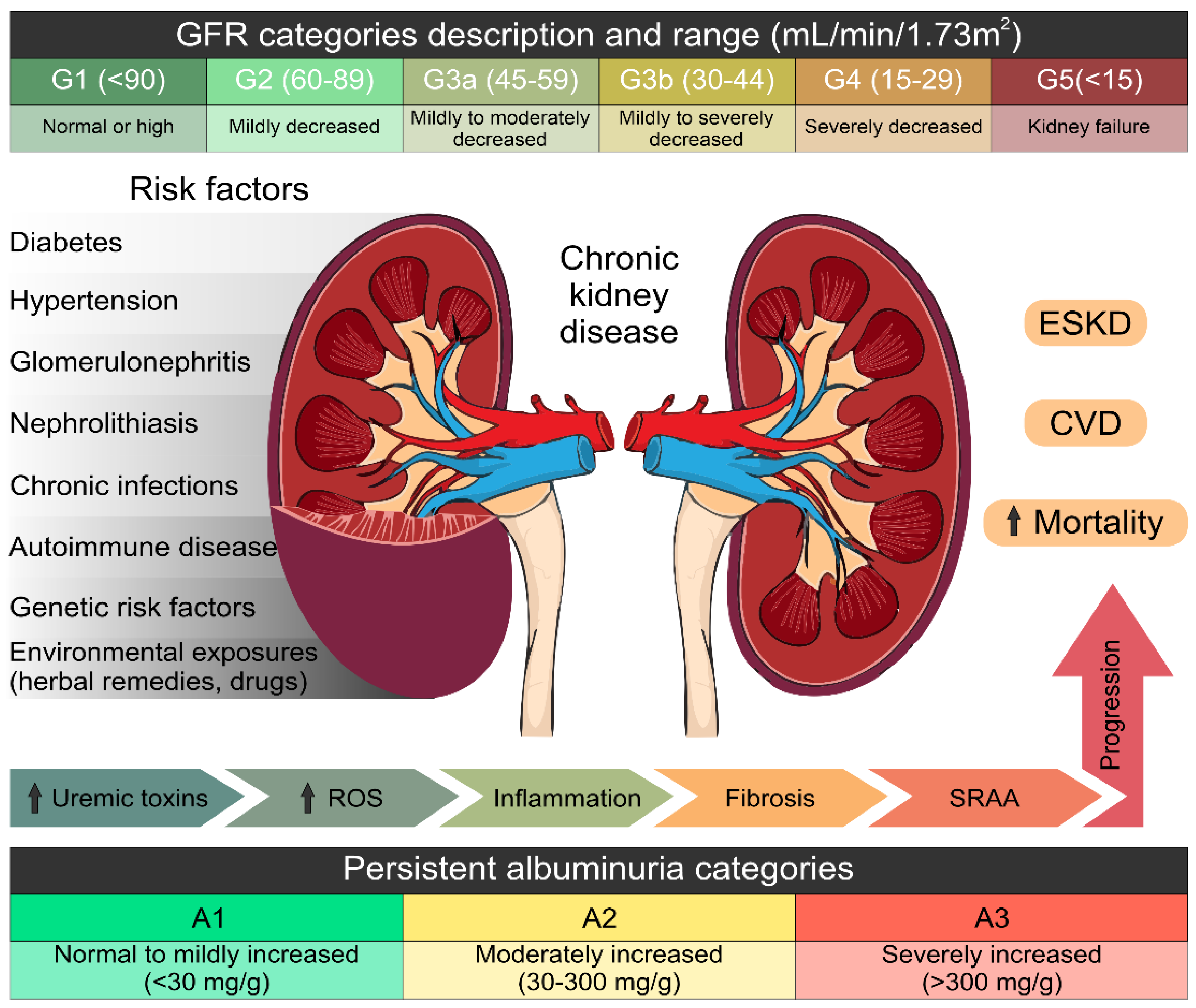
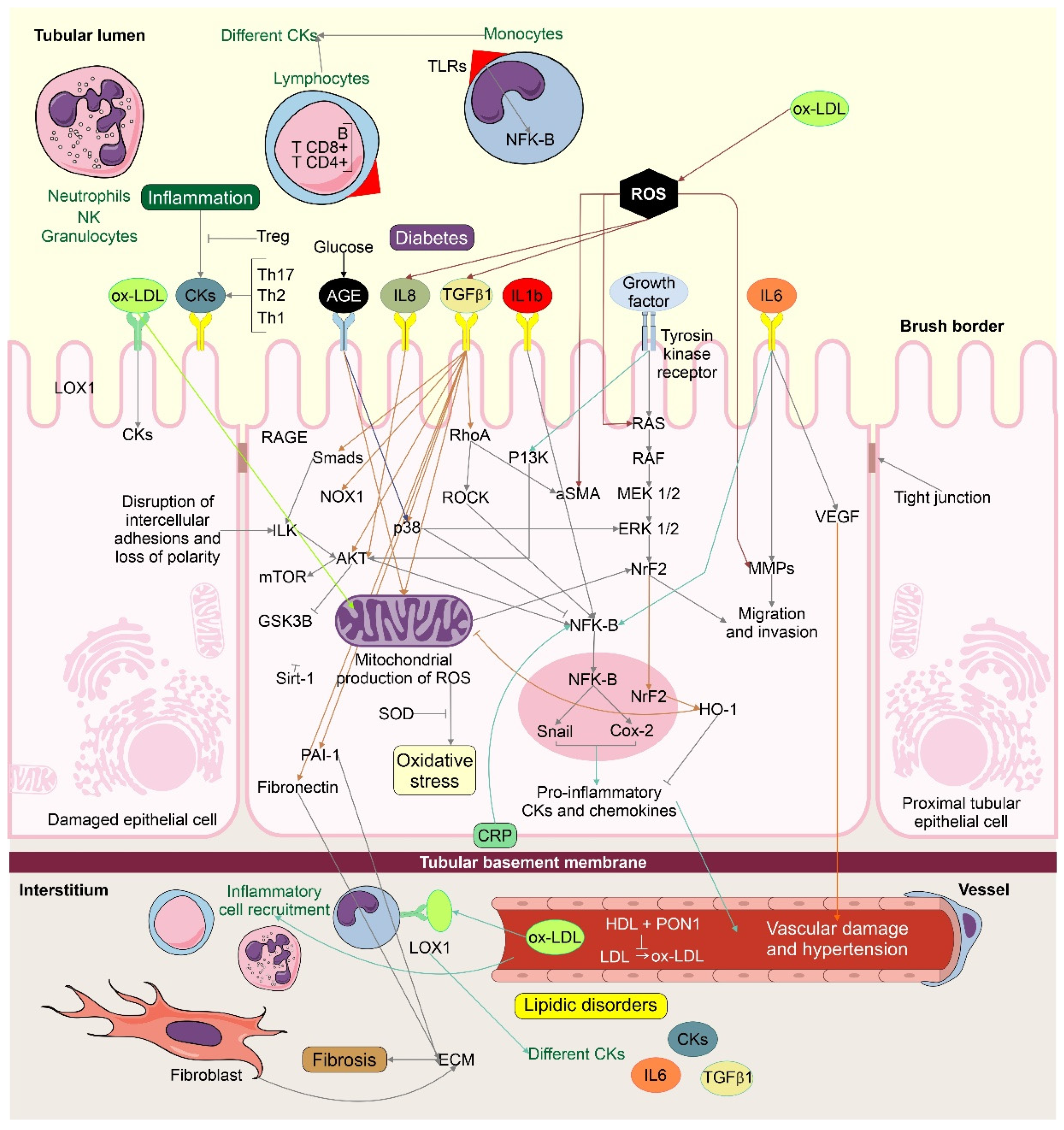
3.1. Molecular Mechanisms Involved in Kidney Damage
3.2. Potential Renoprotective Effects of Some Natural Plant Compounds
3.2.1. Allicin (Diallyl Thiosulfinate)
3.2.2. Astaxanthin
3.2.3. Baicalin
3.2.4. Betalain
3.2.5. Beetroot Juice
3.2.6. Berberine (BBR)
3.2.7. Cordycepin
3.2.8. Curcumin
3.2.9. Epicatechin-3-gallate, Epicatechin, Epigallocatechin
3.2.10. Pomegranate (Punica granatum)
3.2.11. Resveratrol
3.2.12. Sulforaphane
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Avila-Carrasco, L.; Majano, P.; Sánchez-Toméro, J.A.; Selgas, R.; López-Cabrera, M.; Aguilera, A.; González Mateo, G. Natural Plants Compounds as Modulators of Epitelial-to-Mesenchymal Transition. Front. Pharmacol. 2019, 10, 715. [Google Scholar] [CrossRef] [Green Version]
- Lv, J.C.; Zhang, L.X. Prevalence and Disease Burden of Chronic Kidney Disease. Adv. Exp. Med. Biol. 2019, 1165, 3–15. [Google Scholar] [CrossRef]
- Chen, T.K.; Knicely, D.H.; Grams, M.E. Chronic Kidney Disease Diagnosis and Management: A Review. JAMA 2019, 322, 1294–1304. [Google Scholar] [CrossRef]
- Zare, E.; Alirezaei, A.; Bakhtiyari, M.; Mansouri, A. Evaluating the effect of garlic extract on serum inflammatory markers of peritoneal dialysis patients: A randomized double-blind clinical trial study. BMC Nephrol. 2019, 20, 26. [Google Scholar] [CrossRef] [PubMed]
- Mashhadi, N.S.; Zakerkish, M.; Mohammadiasl, J.; Zarei, M.; Mohammadshahi, M.; Haghighizadeh, M.H. Astaxanthin improves glucose metabolism and reduces blood pressure in patients with type 2 diabetes mellitus. Asia Pac. J. Clin. Nutr. 2018, 27, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Shokri-Mashhadi, N.; Tahmasebi, M.; Mohammadi-Asl, J.; Zakerkish, M.; Mohammadshahi, M. The antioxidant and anti-inflammatory effects of astaxanthin supplementation on the expression of miR-146a and miR-126 in patients with type 2 diabetes mellitus: A randomised, double-blind, placebo-controlled clinical trial. Int. J. Clin. Pract. 2021, 75, e14022. [Google Scholar] [CrossRef] [PubMed]
- Dong, S.; Sun, L. Traditional Chinese drug baicalin and insulin therapy on pancreatic beta-cell function in newly diagnosed type 2 diabetes. Chin. Med. 2013, 8, 348–350. [Google Scholar]
- Yang, M.; Kan, L.; Wu, L.; Zhu, Y.; Wang, Q. Effect of baicalin on renal function in patients with diabetic nephropathy and its therapeutic mechanism. Exp. Ther. Med. 2019, 17, 2071–2076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahimi, P.; Mesbah-Namin, S.A.; Ostadrahimi, A.; Abedimanesh, S.; Separham, A.; Asghari jafarabadi, M. Effects of Betalains on Atherogenic Risk Factors in Patients with Atherosclerotic Cardiovascular Disease. Food Funct. 2019, 10, 8286–8297. [Google Scholar] [CrossRef]
- Kemmner, S.; Lorenz, G.; Wobst, J.; Kessler, T.; Wen, M.; Günthner, R.; Stock, K.; Heemann, U.; Burkhardt, K.; Baumann, M.; et al. Dietary nitrate load lowers blood pressure and renal resistive index in patients with chronic kidney disease: A pilot study. Nitric Oxide 2017, 64, 7–15. [Google Scholar] [CrossRef]
- Li, Z.Y.; Liu, B.; Zhuang, X.J.; Shen, Y.D.; Tian, H.R.; Ji, Y.; Li, L.X.; Liu, F. Effects of berberine on the serum cystatin C levels and urine albumin/creatine ratio in patients with type 2 diabetes mellitus. Zhonghua Yi Xue Za Zhi Chin. 2018, 98, 3756–3761. [Google Scholar] [CrossRef]
- Sun, T.; Dong, W.; Jiang, G.; Yang, J.; Liu, J.; Zhao, L.; Ma, P. Cordyceps militaris mejora la enfermedad renal crónica al afectar la vía de señalización redox TLR4/NF-κ B. Oxid Med. Cell Longev. 2019, 7850863. [Google Scholar] [CrossRef] [Green Version]
- Alvarenga, L.; Salarolli, R.; Cardozo, L.F.M.F.; Santos, R.S.; de Brito, J.S.; Kemp, J.A.; Reis, D.; de Paiva, B.R.; Stenvinkel, P.; Lindholm, B.; et al. Impact of curcumin supplementation on expression of inflammatory transcription factors in hemodialysis patients: A pilot randomized, double-blind, controlled study. Clin. Nutr. 2020, 39, 3594–3600. [Google Scholar] [CrossRef]
- Panahi, Y.; Kianpour, P.; Mohtashami, R.; Jafari, R.; Simental-Mendía, L.E.; Sahebkar, A. curcumin lowers serum lipids and uric acid in subjects with nonalcoholic fatty liver disease: A randomized controlled trial. J. Cardiovasc. Pharmacol. 2016, 68, 223–229. [Google Scholar] [CrossRef]
- Jiménez-Osorio, A.S.; García-Niño, W.R.; González-Reyes, S.; Álvarez-Mejía, A.E.; Guerra-León, S.; Salazar-Segovia, J.; Falcón, I.; Montes de Oca-Solano, H.; Madero, M.; Pedraza-Chaverri, J. The effect of dietary supplementation with curcumin on redox status and Nrf2 activation in patients with nondiabetic or diabetic proteinuric chronic kidney disease: A Pilot Study. J. Ren. Nutr. 2016, 26, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Khajehdehi, P.; Pakfetrat, M.; Javidnia, K.; Azad, F.; Malekmakan, L.; Nasab, M.H.; Dehghanzadeh, G. Oral supplementation of turmeric attenuates proteinuria, transforming growth factor-β and interleukin-8 levels in patients with overt type 2 diabetic nephropathy: A randomized, double-blind and placebo-controlled study. Scand. J. Urol. Nephrol. 2011, 45, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Khajehdehi, P.; Zanjaninejad, B.; Aflaki, E.; Nazarinia, M.; Azad, F.; Malekmakan, L. Oral supplementation of turmeric decreases proteinuria, hematuria, and systolic blood pressure in patients suffering from relapsing or refractory lupus nephritis: A randomized and placebo-controlled study. J. Ren. Nutr. 2012, 22, 50–57. [Google Scholar] [CrossRef] [Green Version]
- Pakfetrat, M.; Basiri, F.; Malekmakan, L.; Roozbeh, J. Effects of turmeric on uremic pruritus in end stage renal disease patients: A double-blind randomized clinical trial. J. Nephrol. 2014, 27, 203–207. [Google Scholar] [CrossRef]
- Shoskes, D.; Lapierre, C.; Cruz-Correa, M.; Muruve, N.; Rosario, R.; Fromkin, B.; Braun, M.; Copley, J. Beneficial effects of the bioflavonoids curcumin and quercetin on early function in cadaveric renal transplantation: A randomized placebo controlled trial. Transplantation 2005, 80, 1556–1559. [Google Scholar] [CrossRef] [PubMed]
- Borges, C.M.; Papadimitriou, A.; Duarte, D.A.; Lopes de faria, J.M.; Lopes de faria, J.B. The use of green tea polyphenols for treating residual albuminuria in diabetic nephropathy: A double-blind randomised clinical trial. Sci. Rep. 2016, 6, 28282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, T.-S.; Liou, S.-Y.; Wu, H.-C.; Tsai, F.-J.; Tsai, C.-H.; Huang, C.-Y.; Chang, Y.-L. Efficacy of Epigallocatechin-3-Gallate and Amla (Emblica officinalis) Extract for the Treatment of Diabetic-Uremic Patients. J. Med. Food 2011, 14, 718–723. [Google Scholar] [CrossRef]
- Ushida, Y.; Suganuma, H.; Yanaka, A. Low-dose of the sulforaphane precursor glucoraphanin as a dietary supplement induces chemoprotective enzymes in humans. Food Nutr. Sci. 2015, 6, 1603–1612. [Google Scholar] [CrossRef] [Green Version]
- Tracy, C.R.; Henning, J.R.; Newton, M.R.; Aviram, M.; Zimmerman, M.B. Oxidative stress and nephrolithiasis: A comparative pilot study evaluating the effect of pomegranate extract on stone risk factors and elevated oxidative stress levels of recurrent stone formers and controls. Urolithiasis 2014, 42, 401–408. [Google Scholar] [CrossRef]
- Sattarinezhad, A.; Roozbeh, J.; Shirazi Yeganeh, B.; Omrani, G.R.; Shams, M. Resveratrol reduces albuminuria in diabetic nephropathy: A randomized double-blind placebo-controlled clinical trial. Diabetes Metab. 2019, 45, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Brasnyó, P.; Molnár, G.A.; Mohás, M.; Markó, L.; Laczy, B.; Cseh, J.; Mikolás, E.; Szijártó, I.A.; Mérei, A.; Halmai, R.; et al. Resvera-trol improves insulin sensitivity, reduces oxidative stress and activates the akt pathway in type 2 diabetic patients. Br. J. Nutr. 2011, 106, 383–389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, C.-T.; Sun, X.-Y.; Lin, A.-X. Supplementation with high-dose trans-resveratrol improves ultrafiltration in peritoneal dialysis patients: A prospective, randomized, double-blind study. Ren. Fail. 2016, 38, 214–221. [Google Scholar] [CrossRef] [Green Version]
- Marques, B.C.A.A.; Trindade, M.; Aquino, J.C.F.; Cunha, A.R.; Gismondi, R.O.; Neves, M.F.; Oigman, W. Beneficial effects of acute trans-resveratrol supplementation in treated hypertensive patients with endothelial dysfunction. Clin. Exp. Hypertens. 2018, 40, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Mirmiran, P.; Bahadoran, Z.; Hosseinpanah, F.; Keyzadc, A.; Azizid, F. Effects of broccoli sprout with high sulforaphane concentration on in-flammatory markers in type 2 diabetic patients: A randomized double-blind placebo-controlled clinical trial. J. Funct. Foods 2012, 4, 837–841. [Google Scholar] [CrossRef]
- Cockwell, P.; Fisher, L.-A. The global burden of chronic kidney disease. Lancet 2020, 395, 662–664. [Google Scholar] [CrossRef] [Green Version]
- Webster, A.C.; Nagler, E.V.; Morton, R.L.; Masson, P. Chronic kidney disease. Lancet 2017, 389, 1238–1252. [Google Scholar] [CrossRef]
- Kovács, N.; Nagy, A.; Dombrádi, V.; Bíró, K. Inequalities in the Global Burden of Chronic Kidney Disease Due to Type 2 Diabetes Mellitus: An Analysis of Trends from 1990 to 2019. Int. J. Environ. Res. Public Health 2021, 18, 4723. [Google Scholar] [CrossRef] [PubMed]
- Jha, V.; Garcia-Garcia, G.; Iseki, K.; Li, Z.; Naicker, S.; Plattner, B.; Saran, R.; Wang, A.Y.; Yang, C.W. Chronic kidney disease: Global dimension and perspectives. Lancet 2013, 382, 260–272. [Google Scholar] [CrossRef]
- Minutolo, R.; Lapi, F.; Chiodini, P.; Simonetti, M.; Bianchini, E.; Pecchioli, S.; Cricelli, I.; Cricelli, C.; Piccinocchi, G.; Conte, G.; et al. Risk of ESRD and death in patients with CKD not referred to a nephrologist: A 7-year prospective study. Clin. J. Am. Soc. Nephrol. 2014, 9, 1586–1593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Nicola, L.; Donfrancesco, C.; Minutolo, R.; Lo Noce, C.; De Curtis, A.; Palmieri, L.; Iacoviello, L.; Conte, G.; Chiodini, P.; Sorrentino, F.; et al. Epidemiology of chronic kidney disease in Italy: Current state and contribution of the CARHES study. G. Ital. Nefrol. 2011, 28, 401–407. [Google Scholar] [PubMed]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013, 3, 1–150. [Google Scholar]
- da Silveira, K.D.; Pompermayer Bosco, K.S.; Diniz, L.R.; Carmona, A.K.; Cassali, G.D.; Bruna-Romero, O.; de Sousa, L.P.; Teixeira, M.M.; Santos, R.A.; Simões e Silva, A.C.; et al. ACE2-angiotensin-(1-7)-Mas axis in renal ischaemia/reperfusion injury in rats. Clin. Sci. 2010, 119, 385–394. [Google Scholar] [CrossRef] [Green Version]
- Mezzano, S.A.; Ruiz-Ortega, M.; Egido, J. Angiotensin II and renal fibrosis. Hypertension 2001, 38, 635–638. [Google Scholar] [CrossRef] [Green Version]
- Navar, L.G. Intrarenal renin-angiotensin system in regulation of glomerular function. Curr. Opin. Nephrol. Hypertens. 2014, 23, 38–45. [Google Scholar] [CrossRef] [Green Version]
- Lv, L.-L.; Liu, B.-C. Role of non-classical renin-angiotensin system axis in renal fibrosis. Front. Physiol. 2015, 6, 117. [Google Scholar] [CrossRef] [Green Version]
- Yamagishi, S.; Matsui, T. Advanced glycation end products, oxidative stress and diabetic nephropathy. Oxid. Med. Cell Longev. 2010, 3, 101–108. [Google Scholar] [CrossRef]
- Cellek, S. Point of NO return for nitrergic nerves in diabetes: A new insight into diabetic complications. Curr. Pharm. Des. 2004, 10, 3683–3695. [Google Scholar] [CrossRef]
- Denis, U.; Lecomte, M.; Paget, C.; Ruggiero, D.; Wiernsperger, N.; Lagarde, M. Advanced glycation end-products induce apoptosis of bovine retinal pericytes in culture: Involvement of diacylglycerol/ceramide production and oxidative stress induction. Free Radic. Biol. Med. 2002, 33, 236–247. [Google Scholar] [CrossRef]
- Ramasamy, R.; Vannucci, S.J.; Yan, S.S.D.; Herold, K.; Yan, S.F.; Schmidt, A.M. Advanced glycation end products and RAGE: A common thread in aging, diabetes, neurodegeneration, and inflammation. Glycobiology 2005, 15, 16R–28R. [Google Scholar] [CrossRef]
- Raghavan, C.T.; Nagaraj, R.H. AGE-RAGE interaction in the TGFβ2-mediated epithelial to mesenchymal transition of human lens epithelial cells. Glycoconj. J. 2016, 33, 631–643. [Google Scholar] [CrossRef] [Green Version]
- Wautier, M.P.; Chappey, O.; Corda, S.; Stern, D.M.; Schmidt, A.M.; Wautier, J.L. Activation of NADPH oxidase by AGE links oxidant stress to altered gene expression via RAGE. Am. J. Physiol. Endocrinol. Metab. 2001, 280, E685–E694. [Google Scholar] [CrossRef]
- Panizo, S.; Martínez-Arias, L.; Alonso-Montes, C.; Cannata, P.; Martín-Carro, B.; Fernández-Martín, J.L.; Naves-Díaz, M.; Carrillo-López, N.; Cannata-Andía, J.B. Fibrosis in Chronic Kidney Disease: Pathogenesis and Consequences. Int. J. Mol. Sci. 2021, 22, 408. [Google Scholar] [CrossRef]
- Weidinger, A.; Kozlov, A.V. Biological activities of reactive oxygen and nitrogen species: Oxidative stress versus signal transduction. Biomolecules 2015, 5, 472–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.M.; Cho, M. Activation of NADPH oxidase subunit NCF4 induces ROS-mediated EMT signaling in HeLa cells. Cell. Signal. 2014, 26, 784–796. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.H.; Kim, K.M.; Jeong, J.U.; Shin, J.M.; Kang, J.H.; Bang, K.; Kim, J.H. Nrf2-Heme Oxygenase-1 Attenuates High-Glucose-Induced Epithelial-to-Mesenchymal Transition of Renal Tubule Cells by Inhibiting ROS-Mediated PI3K/Akt/GSK-3β Signaling. J. Diabetes Res. 2019, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Margetts, P.J.; Bonniaud, P.; Liu, L.; Hoff, C.M.; Holmes, C.J.; West-Mays, J.A.; Kelly, M.M. Transient overexpression of TGF-(beta)1 induces epithelial mesenchymal transition in the rodent peritoneum. J. Am. Soc. Nephrol. 2005, 16, 425–436. [Google Scholar] [CrossRef] [Green Version]
- Chapman, A. Epithelial-mesenchymal interactions in pulmonary fibrosis. Ann. Rev. Physiol. 2011, 73, 413–435. [Google Scholar] [CrossRef]
- Derynck, R.; Muthusamy, B.P.; Saeteurn, K.Y. Signaling pathway cooperation in TGF-beta-induced epithelial–mesenchymal transition. Curr. Opin. Cell Biol. 2014, 31, 56–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lamouille, S.; Xu, J.; Derynck, R. Molecular mechanisms of epithelial–mesenchymal transition. Nat. Rev. Mol. Cell Biol. 2014, 15, 178–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ishikawa, F.; Kaneko, E.; Sugimoto, T.; Ishijima, T.; Wakamatsu, M.; Yuasa, A.; Sampei, R.; Mori, K.; Nose, K.; Shibanuma, M. A mitochondrial thioredoxin-sensitive mechanism regulates TGF-beta-mediated gene expression associated with epithelial–mesenchymal transition. Biochem. Biophys. Res. Commun. 2014, 443, 821–827. [Google Scholar] [CrossRef]
- Boudreau, H.E.; Casterline, B.W.; Rada, B.; Korzeniowska, A.; Leto, T.L. Nox4 involvement in TGF-beta and SMAD3-driven induction of the epithelial-to-mesenchymal transition and migration of breast epithelial cells. Free Radic. Biol. Med. 2012, 53, 1489–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hiraga, R.; Kato, M.; Miyagawa, S.; Kamata, T. Nox4-derived ROS signaling contributes to TGF-β-induced epithelial-mesenchymal transition in pancreatic cancer cells. Anticancer Res. 2013, 33, 4431–4438. [Google Scholar]
- Rhyu, D.Y.; Park, J.; Sharma, B.R.; Ha, H. Role of Reactive Oxygen Species in Transforming Growth Factor-Beta1–Induced Extracellular Matrix Accumulation in Renal Tubular Epithelial Cells. Transplant. Proc. 2012, 44, 625–628. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.X.; Zhou, H.J.; Cai, L.; Zhang, W.; Ma, J.L.; Tao, X.J.; Yu, J.N. NADPH oxidase-dependent formation of reactive oxygen species contributes to transforming growth factor beta1-induced epithelial–mesenchymal transition in rat peritoneal mesothelial cells, and the role of astragalus intervention. Chin. J. Integr. Med. 2014, 20, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, J.H.; Kim, J.S.; Chang, J.W.; Kim, S.B.; Park, J.S.; Lee, S.K. AMP-activated protein kinase inhibits TGF-beta-, angiotensin II-, aldosterone-, high glucose-, and albumin-induced epithelial–mesenchymal transition. Am. J. Physiol. Ren. Physiol. 2013, 304, F686–F697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lawson, L.D.; Lawson, L.D.; Bauer, R. Garlic: A Review of Its Medicinal Effects and Indicated Active Compounds. In Phytomedicines of Europe; Lawson, L.D., Ed.; American Chemical Society: Washington, DC, USA, 1998; pp. 177–209. [Google Scholar]
- Borlinghaus, J.; Albrecht, F.; Gruhlke, M.C.H.; Nwachukwu, I.D.; Slusarenko, A.J. Allicin: Chemistry and biological properties. Molecules 2014, 19, 12591–12618. [Google Scholar] [CrossRef] [Green Version]
- Arreola, R.; Quintero-Fabián, S.; López-Roa, R.I.; Flores-Gutiérrez, E.O.; Reyes-Grajeda, J.P.; Carrera-Quintanar, L.; Ortuño-Sahagún, D. Immunomodulation and anti-inflammatory effects of garlic compounds. J. Immunol. Res. 2015, 2015, 1–13. [Google Scholar] [CrossRef]
- Prasad, K.; Laxdal, V.A.; Yu, M.; Raney, B.L. Antioxidant activity of allicin, an active principle in garlic. Mol. Cell Biochem. 1995, 148, 183–189. [Google Scholar] [CrossRef]
- Sharma, N. Efficacy of garlic and onion against virus. Int. J. Res. Pharm. Sci. 2019, 10, 3578–3586. [Google Scholar] [CrossRef] [Green Version]
- Higuera-Ciapara, I.; Félix-Valenzuela, L.; Goyocoolea, F.M. Astaxanthin: A review of its chemistry and applications. Crit. Rev. Food Sci. Nutr. 2006, 46, 186–196. [Google Scholar] [CrossRef] [PubMed]
- Guerin, M.; Huntley, M.E.; Olaizola, M. Haematococcus astaxanthin: Applications for human health and nutrition. Trends Biotechnol. 2003, 21, 210–216. [Google Scholar] [CrossRef]
- Andersen, L.P.; Holck, S.; Kupcinskas, L.; Kiudelis, G.; Jonaitis, L.; Janciauskas, D.; Permin, H.; Wadstrom, T. Gastric inflammatory markers and interleukins in patients with functional dyspepsia treated with astaxanthin. FEMS Immunol. Med. Microbiol. 2007, 50, 244–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iwamoto, T.; Hosoda, K.; Hirano, R.; Kurata, H.; Matsumoto, A.; Miki, W.; Kamiyama, M.; Itakura, H.; Yamamoto, S.; Kondo, K. Inhi-bition of low-density lipoprotein oxidation by astaxanthin. J. Atheroscler. Thromb. 2000, 7, 216–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fassett, R.G.; Healy, H.; Driver, R.; Robertson, I.K.; Geraghty, D.P.; Sharman, J.E.; Coombes, J.S. Astaxanthin vs. placebo on arterial stiffness, oxidative stress and inflammation in renal transplant patients (Xanthin): A randomised controlled trial. BMC Nephrol. 2008, 9, 17. [Google Scholar] [CrossRef] [Green Version]
- Coombes, J.S.; Sharman, J.E.; Fassett, R.G. Astaxanthin has no effect on arterial stiffness, oxidative stress, or inflammation in renal transplant recipients: A randomized controlled trial (the XANTHIN trial). Am. J. Clin. Nutr. 2015, 103, 283–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diao, W.; Chen, W.; Cao, W.; Yuan, H.; Ji, H.; Wang, T.; Chen, W.; Zhu, X.; Zhou, H.; Guo, H.; et al. Astaxanthin protects against renal fibrosis through inhibiting myofibroblast activation and promoting CD8+ T cell recruitment. Biochim. Biophys. Acta Gen. Subj. 2019, 1863, 1360–1370. [Google Scholar] [CrossRef]
- Li, L.; Chen, Y.; Jiao, D.; Yang, S.; Li, L.; Li, P. Protective Effect of Astaxanthin on Ochratoxin A-Induced Kidney Injury to Mice by Regulating Oxidative Stress-Related NRF2/KEAP1 Pathway. Molecules 2020, 25, 1386. [Google Scholar] [CrossRef] [Green Version]
- Yu, F.Y.; Huang, S.G.; Zhang, H.Y.; Ye, H.; Chi, H.G.; Zou, Y.; Lv, R.X.; Zheng, X.B. Effects of baicalin in CD4 + CD29 + T cell subsets of ulcerative colitis patients. World J. Gastroenterol. 2014, 20, 15299–15309. [Google Scholar] [CrossRef]
- Li, F.; He, M.; Li, R. Influence of baicalin and telbivudine on chronic hepatitis B cirrhosis and early serum indexes of liver fibrosis. Med. J. West China 2011, 23, 2112–2114. [Google Scholar]
- Liu, C.; Li, P. Effects of baicalin on erythrocyte aldose reductase activity and early diabetes nephropathy. Chin. J. Gerontol. 2001, 21, 334–335. [Google Scholar]
- Zhu, Y.; Fu, Y.; Lin, H. Baicalin Inhibits Renal Cell Apoptosis and Protects Against Acute Kidney Injury in Pediatric Sepsis. Med. Sci. Monit. 2016, 22, 5109–5115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gandía-Herrero, F.; Jiménez-Atiénzar, M.; Cabanes, J.; García-Carmona, F.; Escribano, J. Stabilization of the Bioactive Pigment of Opuntia Fruits through Maltodextrin Encapsulation. J. Agric. Food Chem. 2010, 58, 10646–10652. [Google Scholar] [CrossRef] [PubMed]
- Sarnak, M.J.; Amann, K.; Bangalore, S.; Cavalcante, J.L.; Charytan, D.M.; Craig, J.C.; Gill, J.S.; Hlatky, M.A.; Jardine, A.G.; Landmesser, U.; et al. Conference Participants. Chronic Kidney Disease and Coronary Artery Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 74, 1823–1838. [Google Scholar] [CrossRef] [PubMed]
- Naqvi, S.F.H.; Husnain, M. Betalains: Potential Drugs with Versatile Phytochemistry. Crit. Rev. Eukaryot. Gene Expr. 2020, 30, 169–189. [Google Scholar] [CrossRef]
- Madadi, E.; Mazloum-Ravasan, S.; Yu, J.S.; Ha, J.W.; Hamishehkar, H.; Kim, K.H. Therapeutic Application of Betalains: A Review. Plants 2020, 9, 1219. [Google Scholar] [CrossRef] [PubMed]
- Sahebkar, A.; Watts, G.F. Mode of action of berberine on lipid metabolism: A new-old phytochemical with clinical applications? Curr. Opin. Lipidol. 2017, 28, 282–283. [Google Scholar] [CrossRef]
- Yin, J.; Gao, Z.; Liu, D.; Liu, Z.; Ye, J. Berberine improves glucose metabolism through induction of glycolysis. Am. J. Physiol. Endocrinol. Metabol. 2008, 294, E148–E156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ni, W.; Ding, H.; Tang, L. Berberine as a promising anti-diabetic nephropathy drug: An analysis of its effects and mechanisms. Eur. J. Pharmacol. 2015, 760, 103–112. [Google Scholar] [CrossRef]
- Lin, Y.; Sheng, M.; Ding, Y.; Zhang, N.; Song, Y.; Du, H.; Lu, N.; Yu, W. Berberine protects renal tubular cells against hypoxia/reoxygenation injury via the Sirt1/p53 pathway. J. Nat. Med. 2018, 72, 715–723. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.Y.; Kim, J.H.; Baek, K.S.; Kim, G.S.; Lee, S.E.; Lee, D.Y.; Choi, J.H.; Kim, S.Y.; Park, H.B.; Sung, G.H.; et al. A direct protein kinase B-targeted anti inflammatory activity of cordycepin from artifi-cially cultured fruit body of Cordyceps militaris. Pharm. Mag. 2015, 11, 477–485. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.T.; Huang, K.S.; Shaw, J.F.; Chen, J.R.; Kuo, W.S.; Shen, G.; Grumezescu, A.M.; Holban, A.M.; Wang, Y.T.; Wang, J.S.; et al. Trends in the Immunomodulatory Effects of Cordyceps militaris: Total Extracts, Polysaccharides and Cordycepin. Front. Pharmacol. 2020, 11, 575704. [Google Scholar] [CrossRef]
- Cui, J.D. Biotechnological production and applications of Cordyceps militaris, a valued traditional Chinese medicine. Crit. Rev. Biotechnol. 2015, 35, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Song, J.; Teng, M.; Zheng, X.; Li, X.; Tian, Y.; Pan, M.; Li, Y.; Lee, R.J.; Wang, D. Antidiabetic and antinephritic activities of aqueous extract of Cordyceps militaris fruit body in diet-streptozotocin-induced diabetic Sprague Dawley rats. Oxid. Med. Cell Longev. 2016, 2016, 9685257. [Google Scholar] [CrossRef]
- Gu, Y.-Y.; Liu, X.-S.; Huang, X.-R.; Yu, X.-Q.; Lan, H.-Y. Diverse Role of TGF-β in Kidney Disease. Front. Cell Dev. Biol. 2020, 8, 123. [Google Scholar] [CrossRef]
- Aggarwal, B.B.; Gupta, S.C.; Sung, B. Curcumin: An orally bioavailable blocker of TNF and other pro-inflammatory biomarkers. Br. J. Pharmacol. 2013, 169, 1672–1692. [Google Scholar] [CrossRef] [Green Version]
- Aydin, M.; Ozkok, E.; Ozturk, O.; Agachan, B.; Yilmaz, H.; Yaylim, I.; Kebabcioglu, S.; Ispir, T. Relationship between interleukin-8 and the oxidant-antioxidant system in end-stage renal failure patients. Exp. Clin. Transplant. 2007, 5, 610–613. [Google Scholar]
- Zhang, D.W.; Fu, M.; Gao, S.H.; Liu, J.L. Curcumin and diabetes: A systematic review. Evid. Based Complement. Altern. Med. 2013, 1–16. [Google Scholar] [CrossRef]
- Vanaie, A.; Shahidi, S.; Iraj, B.; Siadat, Z.D.; Kabirzade, M.; Shakiba, F.; Mohammadi, M.; Parvizian, H. Curcumin as a major active component of turmeric attenuates proteinuria in patients with overt diabetic nephropathy. J. Res. Med. Sci. 2019, 24, 77. [Google Scholar] [CrossRef]
- Hidaka, H.; Ishiko, T.; Furuhashi, T.; Kamohara, H.; Suzuki, S.; Miyazaki, M.; Ikeda, O.; Mita, S.; Setoguchi, T.; Ogawa, M. Curcumin inhibits interleukin 8 production and improves interleukin 8 receptor expression on the cell surface: Impact on human pancreatic carcinoma cell growth by autocrine regulation. Cancer 2002, 95, 1206–1214. [Google Scholar] [CrossRef]
- Wickenberg, J.; Ingemansson, S.L.; Hlebowicz, J. Effects of Curcuma longa (turmeric) on postprandial plasma glucose and insulin in healthy subjects. Nutr. J. 2010, 9, 43. [Google Scholar] [CrossRef] [Green Version]
- Hill-Kapturczak, N.; Thamilselvan, V.; Liu, F.; Nick, H.S.; Agarwal, A. Mechanism of heme oxygenase-1 gene induction by curcumin in human renal proximal tubule cells. Am. J. Physiol Ren. Physiol. 2001, 281, F851. [Google Scholar] [CrossRef]
- Balogun, E.; Hoque, M.; Gong, P.; Killeen, E.; Green, C.J.; Foresti, R.; Alam, J.; Motterlini, R. Curcumin activates the heme oxygenase-1 gene via regulation of Nrf2 and the antioxidant responsive element. Biochem. J. 2003, 371, 887. [Google Scholar] [CrossRef] [Green Version]
- Weir, M.A.; Walsh, M.; Cuerden, M.S.; Sontrop, J.M.; Chambers, L.C.; Garg, A.X. Micro-Particle Curcumin for the Treatment of Chronic Kidney Disease-1: Study Protocol for a Multicenter Clinical Trial. Can. J. Kidney Health Dis. 2018, 5, 2054358118813088. [Google Scholar] [CrossRef]
- Kanwar, J.; Taskeen, M.; Mohammad, I.; Huo, C.; Chan, T.H.; Dou, Q.P. Recent advances on tea polyphenols. Front. Biosci. 2012, 4, 111–131. [Google Scholar] [CrossRef]
- Bao, H.; Peng, A. The green tea polyphenol (-)-epigallocatechin-3-gallate and its beneficial roles in chronic kidney disease. J. Transl. Int. Med. 2016, 4, 99–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Twal, M.; Kiefer, P.; Salameh, A.; Schnabel, J.; Ossmann, S.; von Salisch, S.; Krämer, K.; Sobiraj, A.; Kostelka, M.; Mohr, F.W.; et al. Renoprotective effects of epigallocatechin gallate in a small piglet model of extracorporeal circulation. Pharm. Res. 2013, 67, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Kanlaya, R.; Thongboonkerd, V. Protective Effects of Epigallocatechin-3-Gallate from Green Tea in Various Kidney Diseases. Adv. Nutr. 2019, 10, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.S.; Liou, S.Y.; Chang, Y.L. Supplementation of Emblica officinalis (Amla) extract reduces oxidative stress in uremic patients. Am. J. Chin. Med. 2009, 37, 19–25. [Google Scholar] [CrossRef]
- Bhandari, P.R. Pomegranate (Punica granatum L). Ancient seeds for modern cure? Review of potential therapeutic applica-tions. Int. J. Nutr. Pharmacol. Neurol. Dis. 2012, 2, 171–184. [Google Scholar] [CrossRef]
- Tugcu, V.; Kemahli, E.; Ozbek, E.; Arinci, Y.V.; Uhri, M.; Erturkuner, P.; Metin, G.; Seckin, I.; Karaca, C.; Ipekoglu, N. Protective effect of a potent antioxidant, pomegranate juice, in the kidney of rats with nephrolithiasis induced by ethylene glycol. J. Endourol. 2008, 22, 2723–2732. [Google Scholar] [CrossRef] [PubMed]
- Reichert, C.O.; Levy, D.; Bydlowski, S.P. Paraoxonase Role in Human Neurodegenerative Diseases. Antioxidants 2021, 10, 11. [Google Scholar] [CrossRef]
- Den Hartogh, D.J.; Tsiani, E. Health Benefits of Resveratrol in Kidney Disease: Evidence from In Vitro and In Vivo Studies. Nutrients 2019, 11, 1624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saldanha, J.F.; Leal, V.O.; Rizzetto, F.; Grimmer, G.H.; Ribeiro-Alves, M.; Daleprane, J.B.; Carraro-Eduardo, J.C.; Mafra, D. Effects of Resveratrol Supplementation in Nrf2 and NF-κB Expressions in Nondialyzed Chronic Kidney Disease Patients: A Random-ized, Double-Blind, Placebo-Controlled, Crossover Clinical Trial. J. Ren. Nutr. 2016, 26, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Gal, R.; Deres, L.; Toth, K.; Halmosi, R.; Habon, T. The Effect of Resveratrol on the Cardiovascular System from Molecular Mechanisms to Clinical Results. Int. J. Mol. Sci. 2021, 22, 10152. [Google Scholar] [CrossRef]
- Gowd, V.; Kang, Q.; Wang, Q.; Wang, Q.; Chen, F.; Cheng, K.W. Resveratrol: Evidence for Its Nephroprotective Effect in Diabetic Nephropathy. Adv. Nutr. 2020, 11, 1555–1568. [Google Scholar] [CrossRef]
- Fahey, J.; Talalay, P. Antioxidant function of sulforaphane: A potent inducer of phase 2 detoxyfication enzymes. Food Chem. Toxicol. 1999, 37, 973–979. [Google Scholar] [CrossRef]
- Vanduchova, A.; Anzenbacher, P.; Anzenbacherova, E. Isothiocyanate from Broccoli, Sulforaphane, and Its Properties. J. Med. Food. 2019, 22, 121–126. [Google Scholar] [CrossRef]
- Uddin, M.J.; Kim, E.H.; Hannan, M.A.; Ha, H. Pharmacotherapy against Oxidative Stress in Chronic Kidney Disease: Prom-ising Small Molecule Natural Products Targeting Nrf2-HO-1 Signaling. Antioxidants 2021, 10, 258. [Google Scholar] [CrossRef]
- Riedl, M.A.; Saxon, A.; Diaz-Sanchez, D. Oral sulforaphane increases Phase II antioxidant enzymes in the human upper airway. Clin. Immunol. 2009, 130, 244–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopez-Chillon, M.T.; Carazo-Dıaz, C.; Prieto-Merino, D.; Zafrilla, P.; Moreno, D.A.; Villaño, D. Effects of long-term consumption of broccoli sprouts on inflammatory markers in overweight subjects. Clin. Nutr. 2019, 38, 745–752. [Google Scholar] [CrossRef]
- Navarro, S.L.; Schwarz, Y.; Song, X.; Wang, C.Y.; Chen, C.; Trudo, S.P.; Kristal, A.R.; Kratz, M.; Eaton, D.L.; Lampe, J.W. Cruciferous vegetables have variable effects on biomarkers of systemic inflammation in a randomized controlled trial in healthy young adults. J. Nutr. 2014, 144, 1850–1857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gajjala, P.R.; Sanati, M.; Jankowski, J. Cellular and molecular mechanisms of chronic kidney disease with diabetes mellitus and cardiovascular diseases as its comorbidities. Front. Immunol. 2015, 6, 340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gewin, L.; Zent, R.; Pozzi, A. Progression of chronic kidney disease: Too much cellular talk causes damage. Kidney Int. 2017, 91, 552–560. [Google Scholar] [CrossRef] [Green Version]
- Zoja, C.; Abbate, M.; Remuzzi, G. Progression of renal injury toward interstitial inflammation and glomerular sclerosis is dependent on abnormal protein filtration. Nephrol. Dial. Transplant. 2015, 30, 706–712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turner, J.M.; Bauer, C.; Abramowitz, M.K.; Melamed, M.L.; Hostetter, T.H. Treatment of chronic kidney disease. Kidney Int. 2012, 81, 351–362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stefan, N.; Häring, H.-U.; Schulze, M.B. Metabolically healthy obesity: The low-hanging fruit in obesity treatment? Lancet Diabetes Endocrinol. 2018, 6, 249–258. [Google Scholar] [CrossRef]
- Kuzma, J.N.; Schmidt, K.A.; Kratz, M. Prevention of metabolic diseases: Fruits (including fruit sugars) vs. vegetables. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 286–293. [Google Scholar] [CrossRef]
- Vieira, A.R.; Abar, L.; Vingeliene, S.; Chan, D.S.M.; Aune, D.; Navarro-Rosenblatt, D.; Stevens, C.; Greenwood, D.; Norat, T. Fruits, vegetables, and lung cancer risk: A systematic review and meta-analysis. Ann. Oncol. 2016, 27, 81–96. [Google Scholar] [CrossRef]
| Bioactive Compound | Chemical Class and Natural Sources | Study Type | Mechanisms of Renoprotection | Molecular Markers | Refs. |
|---|---|---|---|---|---|
| Alliin | Garlic (Allium sativum L.), Diallyl thiosulfinate | Clinical trial | Anti-inflammation | ↓ IL-6, ↓ CRP, and ↓ ESR | [4] |
| Astaxanthin (3,3′-dihydroxy-β,β’-carotene-4,4′-dione) | Xanthophyll carotenoid; algae, shrimp, lobster, crab, salmon, and other organisms | Clinical trial | Hypolipidemic effects Hypoglycemic effects | ↑ Serum adiponectin ↓ Visceral body fat mass. ↓ TG, ↓ VLDL, ↓ cholesterol, ↓ Systolic blood pressure ↑ BMR | [5] |
| Clinical trial | Antioxidation Anti-inflammation | ↓ MDA and ↓ IL-6 Downregulation of miR-146a | [6] | ||
| Baicalin | Flavonoid; roots of Scutellaria baicalensis Georgi | Clinical studies | Attenuate AKI | Decreased BUN and Cr levels | [7] |
| Clinical studies | Antioxidation Anti-inflammation | ↑ GSH, ↑ SOD ↑ aldose reductase (AR) activity. ↓ NF-κB and VEGF | [8] | ||
| Betalains/betacyanins | Red beetroot (betalain), Opuntia stricta (betacyanin) | Clinical trial | Anti-inflammation Antioxidation Anti-atherosclerosis | ↓ hs-CRP ↓ Hcy levels, ↓ SBP, and ↓ FBG ↓ TC, ↓ TG, ↓ non-HDL-c, and ↓ LDL | [9] |
| Beetroot juice | Beta vulgaris (nitrate (NO3) is reduced to nitrite (NO2) in the oral cavity and is converted to nitric oxide (NO) in the circulation | Pilot study | Decreased renal resistive index Lowered peripheral blood pressure | ↓ cDBP ↓ RRI | [10] |
| Berberine | Isoquinoline alkaloid; Coptidis rhizoma and Cortex phellodendri | Clinical trial | Improved diabetic kidney disease | ↓ UACR and ↓ serum Cys C | [11] |
| Cordycepin | Cordyceps militaris | Clinical studies | Increased kidney function Improved redox properties Lipid-improving | ↓ Urinal protein, ↓ BUN, and ↓ creatinine ↓ Cys C, ↓TG, ↓TC, ↓ LDL-c, and ↑ HDL-C ↓ MPO and MDA ↑ NO and SOD | [12] |
| Curcumin | Curcuminoid; turmeric (Curcuma longa) | Pilot study | Antioxidant Anti-inflammation | ↓ NF-kB mRNA expression. ↓ hs-CRP plasma levels | [13] |
| Clinical trial | Reduces serum lipids and uric acid concentrations | ↓ Serum urea and induced urinary excretion ↓TG, ↓TC, ↓ LDL-c, and ↑ HDL-C | [14] | ||
| Pilot study | Antioxidant | ↓ Lipid peroxidation ↑ Antioxidant capacity | [15] | ||
| Clinical trial | Anti-inflammation Attenuated proteinuria Decreased hematuria and systolic blood pressure | ↓ TGF-β, ↓ IL-8 ↓ Creatinine | [16] | ||
| Clinical trial | Slowed the progression of CKD | ↓ Proteinuria, hematuria, and systolic blood pressure | [17] | ||
| Clinical trial | Decreased uremic pruritus in ESRD patients Anti-inflammation | ↓ hs-CRP | [18] | ||
| Curcumin/quercetin | Bioflavonoids | Clinical trial | Improved early outcomes in cadaveric renal transplantation | ↓ Serum Cr Induction of HO-1 DGF lowered | [19] |
| Epigallocatechin-3-gallate (EGCG) | Green tea (Camellia sinensis), natural polyphenolic component of green tea leaves | Clinical trial | Antiproteinuric effect Anti-apoptotic effect | ↓ Albuminuria ↓ Caspase 3 | [20] |
| Epigallocatechin-3-gallate (EGCG)/Amla extract (AE) 1:1 | Amla extract (Emblica officinalis), the Indian gooseberry | Clinical study | Improved diabetic markers in uremic patients Antioxidant effect Anti-atherosclerosis | ↓ AGEs formation ↓ NOx ↓ plasma FRAP HDL and LDL/HDL ratio improved | [21] |
| Glucoraphanin (GR) | Hydrolyzed to SFN by the intestinal microbiota | Clinical trial | Anti-inflammation Anti-OS | ↑ NQO1 and GST | [22] |
| Pomegranate extract | Pomegranate (Punica granatum); polyphenols, alkaloids, and anthocyanins | Pilot study | Antioxidant effect Prevention of nephrolithiasis | Scavenging free radicals ↑ levels of PON1 ↓ SSCaOx | [23] |
| Resveratrol (RSV; trans-3,5,4-trihydroxystilbene) | Phytoalexin; red grapes (Vitis vinifera L.), peanuts (Arachis spp.), and berries (Vaccinium spp.) | Clinical trial | Reduction of urine albumin/creatinine ratio Antioxidant effect | ↓ FPG, ↓ HbA1c, ↓ insulin levels and ↓ HOMA-IR. ↑ SOD, GSH-Px, CAT and NO | [24] |
| Clinical study | Reduction of insulin resistance and oxidative stress | ↑ pAkt:Akt ratio in platelets. ↓ Urinary ortho-tyrosine excretion ↑ Insulin sensitivity | [25] | ||
| Clinical study | ↓UF volume and rate Ameliorating angiogenesis | ↓ PDE VEGF, Flk-1 and Ang-2 ↑ PDE Tie-2 and Tsp-1 | [26] | ||
| Clinical study | Improvement in endothelial function | ↑ Brachial flow-mediated dilatation (FMD); ↓LDL-c | [27] | ||
| Sulforaphane (1-isothiocyanate-4-methylsulphinylbutane) | Isothiocyanate (organosulfur compound); cruciferous vegetables such as broccoli, brussels sprouts, and cabbages | Clinical trial | Anti-inflammation | ↓ hs-CRP and ↓ IL-6 | [28] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Avila-Carrasco, L.; García-Mayorga, E.A.; Díaz-Avila, D.L.; Garza-Veloz, I.; Martinez-Fierro, M.L.; González-Mateo, G.T. Potential Therapeutic Effects of Natural Plant Compounds in Kidney Disease. Molecules 2021, 26, 6096. https://doi.org/10.3390/molecules26206096
Avila-Carrasco L, García-Mayorga EA, Díaz-Avila DL, Garza-Veloz I, Martinez-Fierro ML, González-Mateo GT. Potential Therapeutic Effects of Natural Plant Compounds in Kidney Disease. Molecules. 2021; 26(20):6096. https://doi.org/10.3390/molecules26206096
Chicago/Turabian StyleAvila-Carrasco, Lorena, Elda Araceli García-Mayorga, Daisy L. Díaz-Avila, Idalia Garza-Veloz, Margarita L Martinez-Fierro, and Guadalupe T González-Mateo. 2021. "Potential Therapeutic Effects of Natural Plant Compounds in Kidney Disease" Molecules 26, no. 20: 6096. https://doi.org/10.3390/molecules26206096
APA StyleAvila-Carrasco, L., García-Mayorga, E. A., Díaz-Avila, D. L., Garza-Veloz, I., Martinez-Fierro, M. L., & González-Mateo, G. T. (2021). Potential Therapeutic Effects of Natural Plant Compounds in Kidney Disease. Molecules, 26(20), 6096. https://doi.org/10.3390/molecules26206096







