Use of Plasma Technologies for Antibacterial Surface Properties of Metals
Abstract
:1. Introduction
2. Antibacterial Metal Surfaces in Medicine
2.1. Antibacterial Strategies
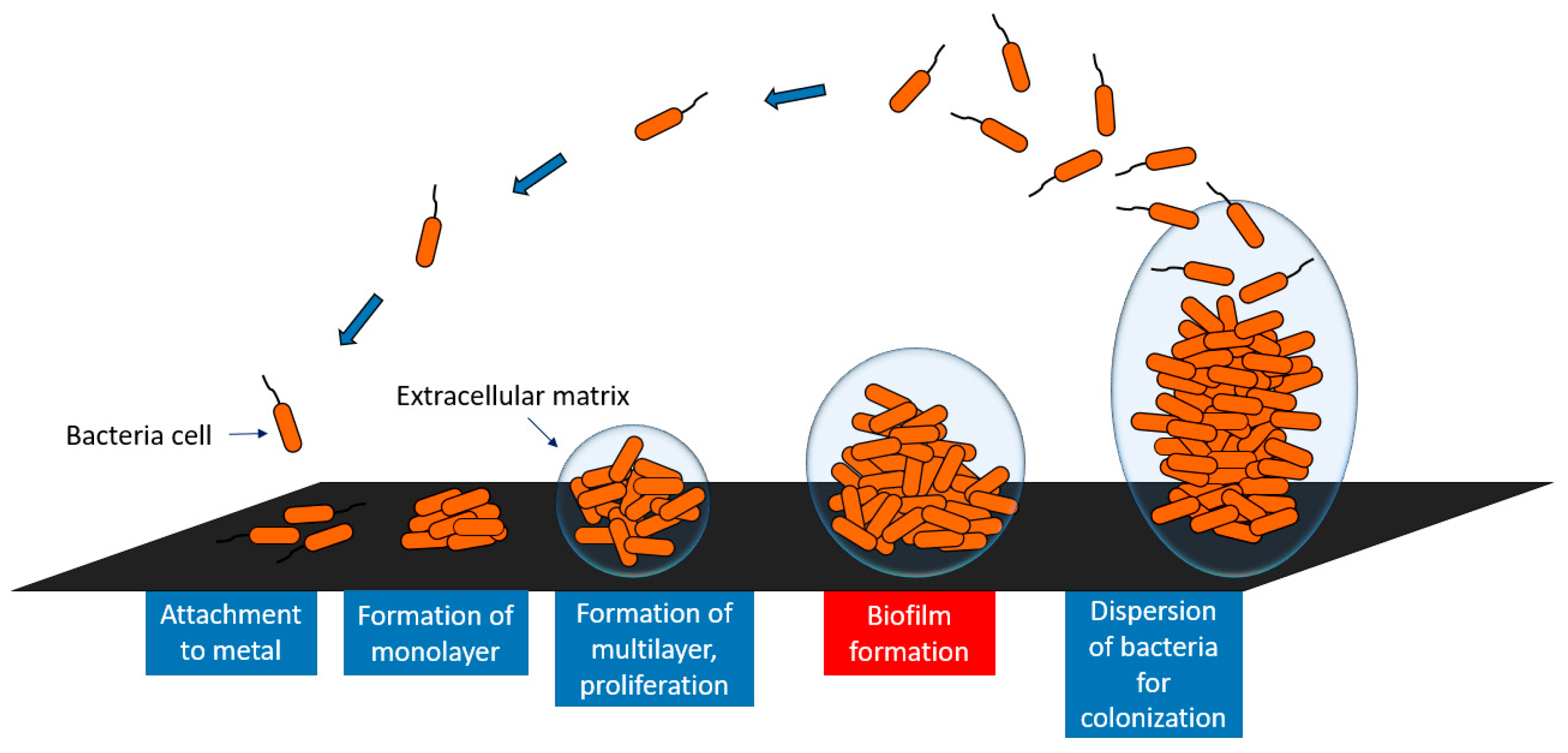
2.2. Bacterial Adhesion and Biofilm Formation on Metal Surfaces
3. Plasma Technologies in Medicine
3.1. Types of Plasma
3.1.1. Low-Pressure Plasma
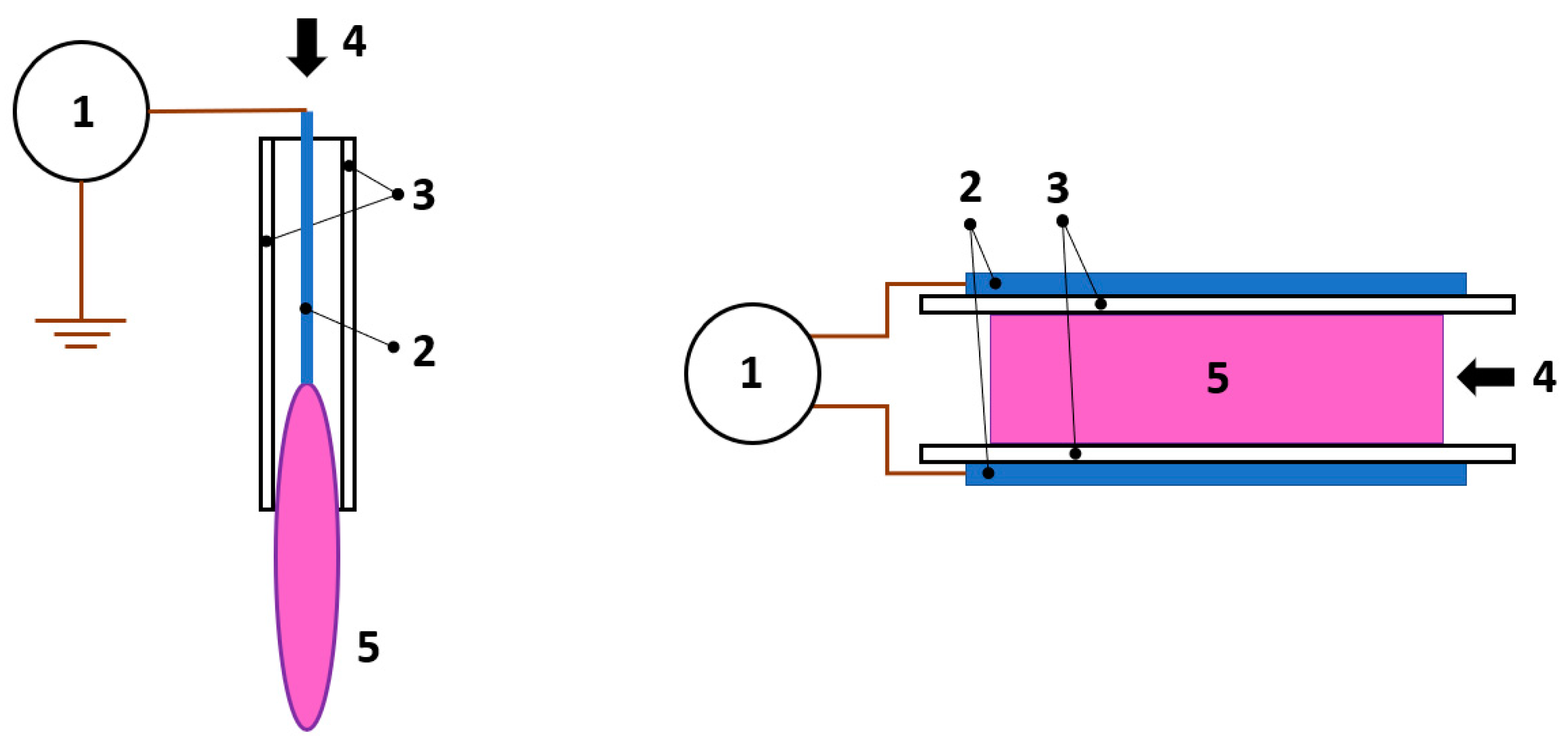
3.1.2. Atmospheric Pressure Plasma
3.2. Commonly Employed Plasma Treatment Techniques
3.2.1. Plasma Spraying
3.2.2. Plasma Induced Physical and Chemical Vapor Deposition
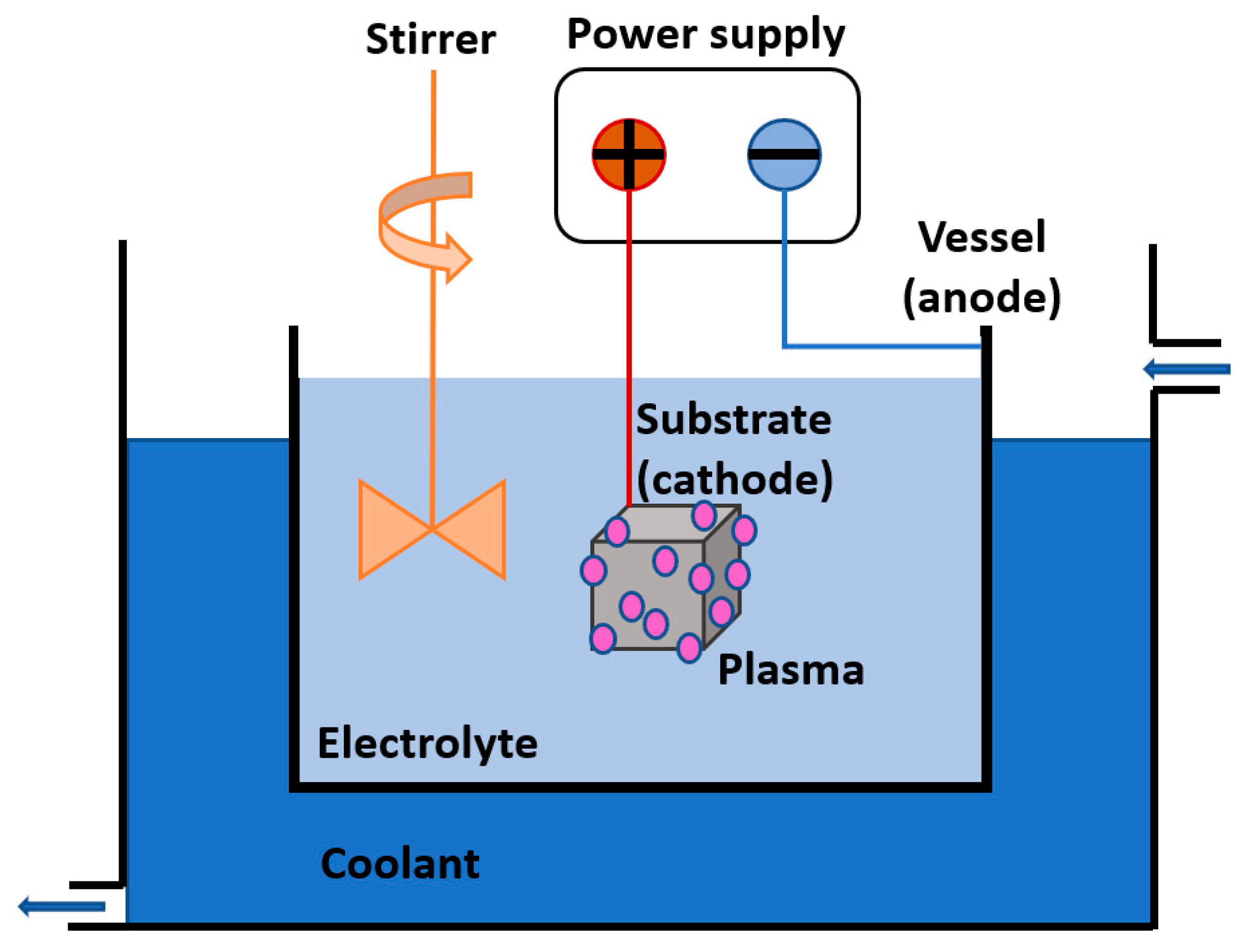
3.2.3. Plasma Electrolytic Oxidation (PEO)
3.2.4. Plasma Immersion Ion Implantation and Deposition (PIII)
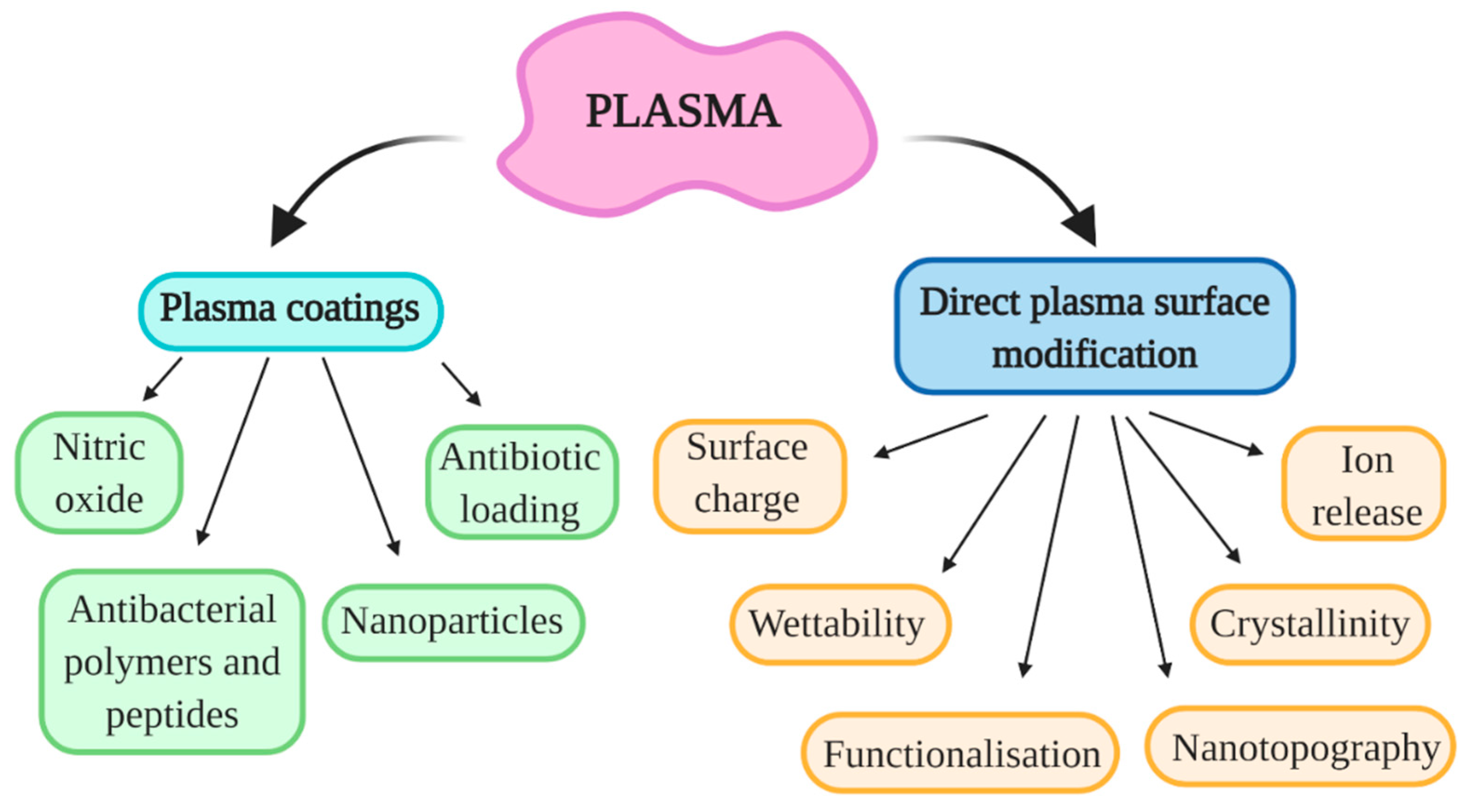
4. Overview of Plasma Treatment Techniques: Antibacterial Surfaces
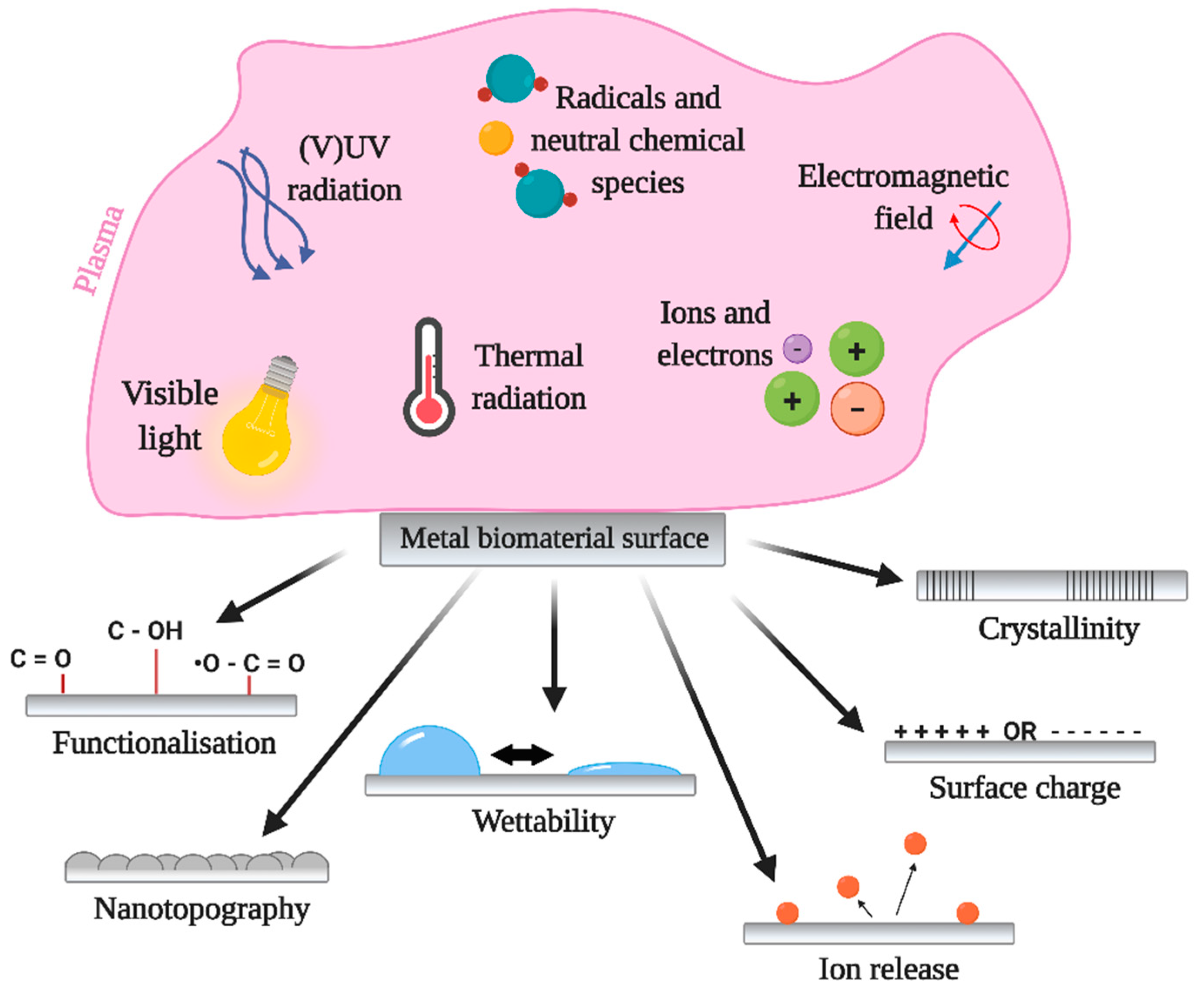
5. Plasma induced Antibacterial Properties of Metals
5.1. Influence of Surface Chemistry, Crystallinity, and Ion Release
5.2. Influence of Nanotopography
5.3. Influence of Surface Charge and Wettability
6. Influence of Gaseous Plasma Treatment on Surface Properties
6.1. Surface Chemistry
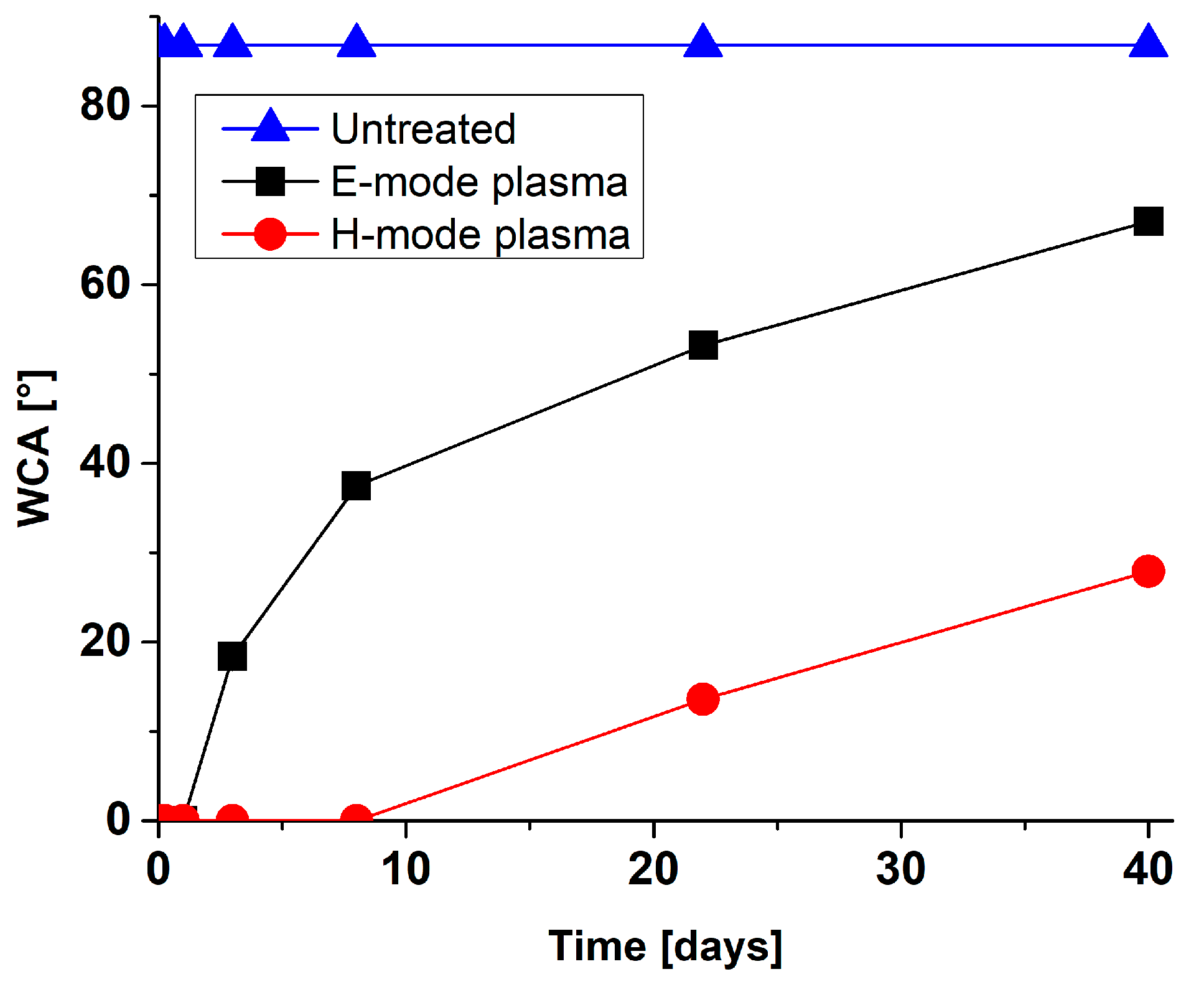
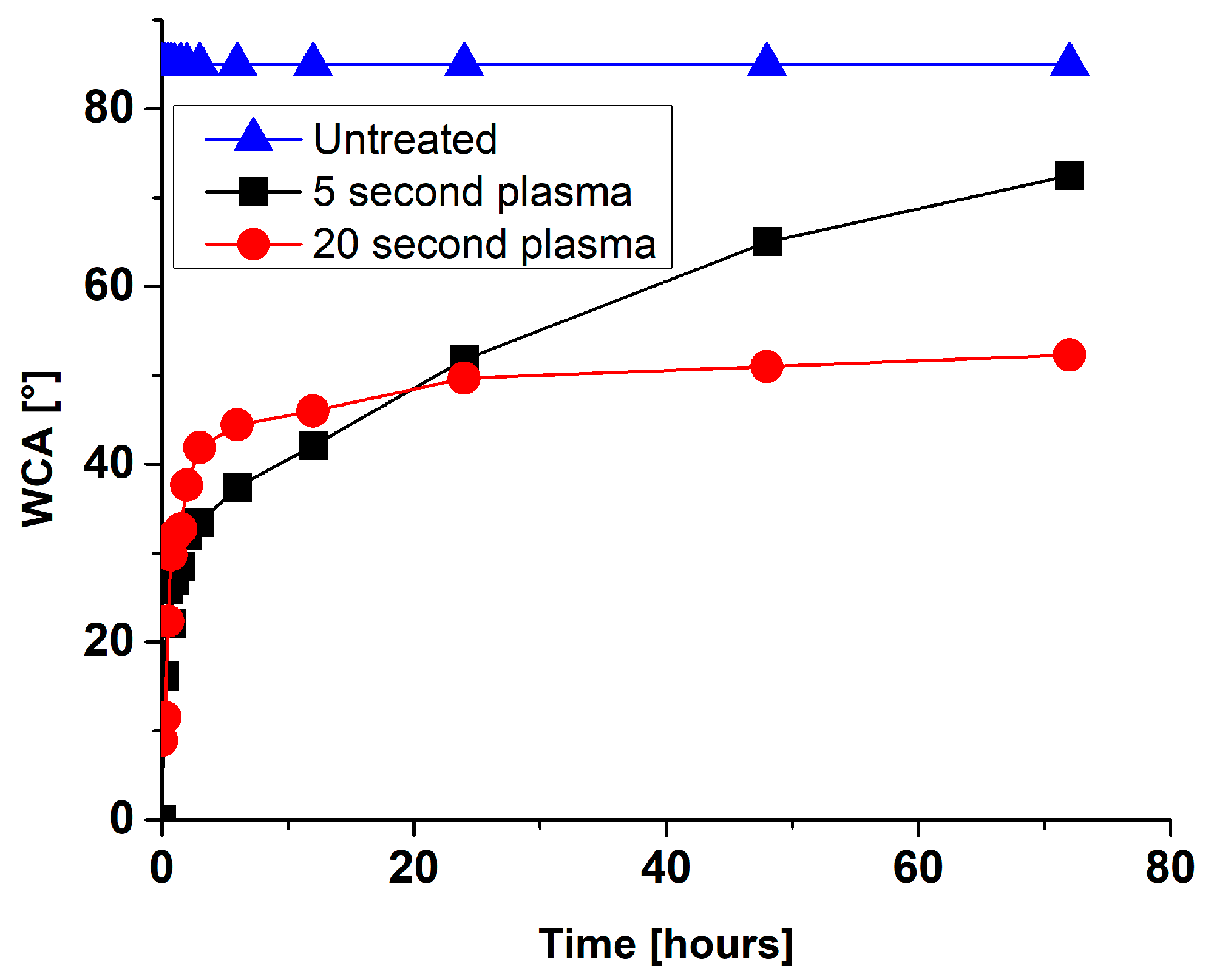
6.2. Surface Wettability
6.3. Surface Nanostructuring
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; E Kretzschmar, M.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef] [Green Version]
- Navarro, M.; Michiardi, A.; Castaño, O.; Planell, J.A. Biomaterials in orthopaedics. J. R. Soc. Interface 2008, 5, 1137–1158. [Google Scholar] [CrossRef] [Green Version]
- Esposito, M.; Coulthard, P.; Oliver, R.; Thomsen, P.; Worthington, H. Antibiotics to prevent complications following dental implant treatment. Aust. Dent. J. 2004, 49, 205. [Google Scholar] [CrossRef]
- Ren, L.; Yang, K. Antibacterial design for metal implants. In Metallic Foam Bone; Elsevier: Amsterdam, The Netherlands, 2017; pp. 203–216. [Google Scholar]
- Pallavicini, P.; Dacarro, G.; Diaz-Fernandez, Y.A.; Taglietti, A. Coordination chemistry of surface-grafted ligands for antibacterial materials. Coord. Chem. Rev. 2014, 275, 37–53. [Google Scholar] [CrossRef]
- García-Gareta, E.; Hua, J.; Orera, A.; Kohli, N.; Knowles, J.C.; Blunn, G.W. Biomimetic surface functionalization of clinically relevant metals used as orthopaedic and dental implants. Biomed. Mater. 2017, 13, 015008. [Google Scholar] [CrossRef] [PubMed]
- Bandara, C.D.; Singh, S.; Afara, I.O.; Wolff, A.; Tesfamichael, T.; Ostrikov, K.; Oloyede, A. Bactericidal Effects of Natural Nanotopography of Dragonfly Wing onEscherichia coli. ACS Appl. Mater. Interfaces 2017, 9, 6746–6760. [Google Scholar] [CrossRef] [Green Version]
- Bazaka, K.; Jacob, M.V.; Chrzanowski, W.; Ostrikov, K. Anti-bacterial surfaces: Natural agents, mechanisms of action, and plasma surface modification. RSC Adv. 2015, 5, 48739–48759. [Google Scholar] [CrossRef] [Green Version]
- Getzlaf, M.A.; Lewallen, E.A.; Kremers, H.M.; Jones, D.L.; Bonin, C.A.; Dudakovic, A.; Thaler, R.; Cohen, R.C.; Lewallen, D.G.; Van Wijnen, A.J. Multi-disciplinary antimicrobial strategies for improving orthopaedic implants to prevent prosthetic joint infections in hip and knee. J. Orthop. Res. 2016, 34, 177–186. [Google Scholar] [CrossRef] [Green Version]
- Lu, T.; Qiao, Y.; Liu, X. Surface modification of biomaterials using plasma immersion ion implantation and deposition. Interface Focus 2012, 2, 325–336. [Google Scholar] [CrossRef] [Green Version]
- Junkar, I.; Kulkarni, M.; Benčina, M.; Kovač, J.; Mrak-Poljšak, K.; Lakota, K.; Sodin-Šemrl, S.; Mozetič, M.; Iglič, A. Titanium Dioxide Nanotube Arrays for Cardiovascular Stent Applications. ACS Omega 2020, 5, 7280–7289. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Huang, X.; Deng, W.; Chang, C.; Hang, R.; Tang, B. A nano-silver composite based on the ion-exchange response for the intelligent antibacterial applications. Mater. Sci. Eng. C 2014, 41, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Gao, L.; Liu, E.; Yu, F.; Shu, X.; Wang, H. Microstructure, corrosion and tribological and antibacterial properties of Ti–Cu coated stainless steel. J. Mech. Behav. Biomed. Mater. 2015, 50, 23–32. [Google Scholar] [CrossRef] [Green Version]
- Balestriere, M.; Schuhladen, K.; Seitz, K.H.; Boccaccini, A.; Cere, S.; Ballarre, J. Sol-gel coatings incorporating borosilicate bioactive glass enhance anti corrosive and surface performance of stainless steel implants. J. Electroanal. Chem. 2020, 876, 114735. [Google Scholar] [CrossRef]
- Hui, R.; Wang, Z.; Kesler, O.; Rose, L.; Jankovic, J.; Yick, S.; Maric, R.; Ghosh, D. Thermal plasma spraying for SOFCs: Applications, potential advantages, and challenges. J. Power Sources 2007, 170, 308–323. [Google Scholar] [CrossRef]
- Fauchais, P.; Vardelle, A.; Vardelle, M. Modelling of plasma spraying of ceramic coatings at atmospheric pressure. Ceram. Int. 1991, 17, 367–379. [Google Scholar] [CrossRef]
- Ferraris, S.; Spriano, S. Antibacterial titanium surfaces for medical implants. Mater. Sci. Eng. C 2016, 61, 965–978. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Qiao, Y.; Liu, X.; Lu, T.; Cui, T.; Meng, F.; Chu, P.K. Electron storage mediated dark antibacterial action of bound silver nanoparticles: Smaller is not always better. Acta Biomater. 2013, 9, 5100–5110. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wu, G.; Liu, X.; Sun, G.; Li, D.; Wei, H. A decomposable silica-based antibacterial coating for percutaneous titanium implant. Int. J. Nanomed. 2017, 12, 371–379. [Google Scholar] [CrossRef] [Green Version]
- Costa, B.C.; Rodrigues, E.A.; Tokuhara, C.K.; Oliveira, R.C.; Lisboa-Filho, P.N.; Rocha, L.A. ZnO Nanoparticles with Different Sizes and Morphologies for Medical Implant Coatings: Synthesis and Cytotoxicity. BioNanoScience 2018, 8, 587–595. [Google Scholar] [CrossRef] [Green Version]
- Astasov-Frauenhoffer, M.; Koegel, S.; Waltimo, T.; Zimmermann, A.; Walker, C.; Hauser-Gerspach, I.; Jung, C. Antimicrobial efficacy of copper-doped titanium surfaces for dental implants. J. Mater. Sci. Mater. Med. 2019, 30, 84. [Google Scholar] [CrossRef]
- Di, H.; Qiaoxia, L.; Yujie, Z.; Jingxuan, L.; Yan, W.; Yinchun, H.; Xiaojie, L.; Song, C.; Weiyi, C. Ag nanoparticles incorporated tannic acid/nanoapatite composite coating on Ti implant surfaces for enhancement of antibacterial and antioxidant properties. Surf. Coat. Technol. 2020, 399, 126169. [Google Scholar] [CrossRef]
- Brar, H.S.; Platt, M.O.; Sarntinoranont, M.; Martin, P.I.; Manuel, M.V. Magnesium as a biodegradable and bioabsorbable material for medical implants. JOM 2009, 61, 31–34. [Google Scholar] [CrossRef]
- Resnik, M.; Benčina, M.; Levičnik, E.; Rawat, N.; Iglič, A.; Junkar, I. Strategies for improving antimicrobial properties of stainless steel. Materials 2020, 13, 2944. [Google Scholar] [CrossRef] [PubMed]
- Jahanmard, F.; Dijkmans, F.; Majed, A.; Vogely, H.C.; Van Der Wal, B.; Stapels, D.; Ahmadi, S.M.; Vermonden, T.; Yavari, S.A. Toward Antibacterial Coatings for Personalized Implants. ACS Biomater. Sci. Eng. 2020, 6, 5486–5492. [Google Scholar] [CrossRef] [PubMed]
- Dangas, G.; Kuepper, F.J.C. Restenosis: Repeat narrowing of a coronary artery: Prevention and treatment. Circulation 2002, 105, 2586–2587. [Google Scholar] [CrossRef] [Green Version]
- Basko-Plluska, J.L.; Thyssen, J.P.; Schalock, P.C. Cutaneous and Systemic Hypersensitivity Reactions to Metallic Implants. Dermatitis 2011, 22, 65–79. [Google Scholar] [CrossRef] [PubMed]
- Sansone, V.; Pagani, D.; Melato, M.J.C.C.i.M.; Metabolism, B. The effects on bone cells of metal ions released from orthopaedic implants. A review. Clin. Cases Miner Bone Metab. 2013, 10, 34. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.; Akhavan, B.; Wise, S.G.; Bilek, M.M. A review of biomimetic surface functionalization for bone-integrating orthopedic implants: Mechanisms, current approaches, and future directions. Prog. Mater. Sci. 2019, 106, 100588. [Google Scholar] [CrossRef]
- Wapner, K.L. Implications of metallic corrosion in total knee arthroplasty. Clin. Orthop. Relat. Res. 1991, 271, 12–20. [Google Scholar] [CrossRef]
- Hallab, N.J.; Vermes, C.; Messina, C.; Roebuck, K.A.; Glant, T.T.; Jacobs, J.J. Concentration-and composition-dependent effects of metal ions on human MG-63 osteoblasts. J. Biomed. Mater. Res. 2002, 60, 420–433. [Google Scholar] [CrossRef]
- Hobman, J.L.; Crossman, L.C. Bacterial antimicrobial metal ion resistance. J. Med. Microbiol. 2015, 64, 471–497. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Manolache, S.; Wong, A.C.L.; Denes, F.S. Plasma-enhanced deposition of silver nanoparticles onto polymer and metal surfaces for the generation of antimicrobial characteristics. J. Appl. Polym. Sci. 2004, 93, 1411–1422. [Google Scholar] [CrossRef]
- Fattah-Alhosseini, A.; Molaei, M.; Attarzadeh, N.; Babaei, K.; Attarzadeh, F. On the enhanced antibacterial activity of plasma electrolytic oxidation (PEO) coatings that incorporate particles: A review. Ceram. Int. 2020, 46, 20587–20607. [Google Scholar] [CrossRef]
- Harrison, J.J.; Ceri, H.; Stremick, C.A.; Turner, R.J. Biofilm susceptibility to metal toxicity. Environ. Microbiol. 2004, 6, 1220–1227. [Google Scholar] [CrossRef]
- Turner, R.J. Metal-based antimicrobial strategies. Microb. Biotechnol. 2017, 10, 1062–1065. [Google Scholar] [CrossRef]
- Wang, L.; Hu, C.; Shao, L. The antimicrobial activity of nanoparticles: Present situation and prospects for the future. Int. J. Nanomed. 2017, 12, 1227–1249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, R.; Hao, L.; Song, L.; Tian, L.; Fan, Y.; Zhao, J.; Liu, C.; Ming, W.; Ren, L. Lotus-leaf-inspired hierarchical structured surface with non-fouling and mechanical bactericidal performances. Chem. Eng. J. 2020, 398, 125609. [Google Scholar] [CrossRef]
- Watson, G.S.; Green, D.W.; Schwarzkopf, L.; Li, X.; Cribb, B.W.; Myhra, S.; Watson, J.A. A gecko skin micro/nano structure—A low adhesion, superhydrophobic, anti-wetting, self-cleaning, biocompatible, antibacterial surface. Acta Biomater. 2015, 21, 109–122. [Google Scholar] [CrossRef]
- Liu, Q.; Brookbank, L.; Ho, A.; Coffey, J.; Brennan, A.B.; Jones, C.J. Surface texture limits transfer of S. aureus, T4 bacteriophage, influenza B virus and human coronavirus. PLoS ONE 2020, 15, e0244518. [Google Scholar] [CrossRef]
- Narendrakumar, K.; Kulkarni, M.V.; Addison, O.; Mazare, A.; Junkar, I.; Schmuki, P.; Sammons, R.L.; Iglič, A. Adherence of oral streptococci to nanostructured titanium surfaces. Dent. Mater. 2015, 31, 1460–1468. [Google Scholar] [CrossRef] [PubMed]
- Junkar, I.; Kulkarni, M.; Drašler, B.; Rugelj, N.; Mazare, A.; Flašker, A.; Drobne, D.; Humpolíček, P.; Resnik, M.; Schmuki, P.; et al. Influence of various sterilization procedures on TiO2 nanotubes used for biomedical devices. Bioelectrochemistry 2016, 109, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Flašker, A.; Kulkarni, M.; Mrak-Poljsak, K.; Junkar, I.; Čučnik, S.; Žigon, P.; Mazare, A.; Schmuki, P.; Iglič, A.; Sodin-Semrl, S. Binding of human coronary artery endothelial cells to plasma-treated titanium dioxide nanotubes of different diameters. J. Biomed. Mater. Res. Part A 2016, 104, 1113–1120. [Google Scholar] [CrossRef]
- Bagherifard, S.; Hickey, D.J.; De Luca, A.C.; Malheiro, V.N.; Markaki, A.E.; Guagliano, M.; Webster, T.J. The influence of nanostructured features on bacterial adhesion and bone cell functions on severely shot peened 316L stainless steel. Biomaterials 2015, 73, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Arciola, C.R.; Campoccia, D.; Ehrlich, G.D.; Montanaro, L. Biofilm-Based Implant Infections in Orthopaedics. Adv. Exp. Med. Biol. 2015, 830, 29–46. [Google Scholar] [PubMed]
- Montanaro, L.; Speziale, P.; Campoccia, D.; Ravaioli, S.; Cangini, I.; Pietrocola, G.; Giannini, S.; Arciola, C.R. Scenery of Staphylococcus implant infections in orthopedics. Future Microbiol. 2011, 6, 1329–1349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, J.M.; Rodriguez, A.; Chang, D.T. Foreign body reaction to biomaterials. Semin. Immunol. 2008, 20, 86–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franz, S.; Rammelt, S.; Scharnweber, D.; Simon, J.C. Immune responses to implants—A review of the implications for the design of immunomodulatory biomaterials. Biomaterials 2011, 32, 6692–6709. [Google Scholar] [CrossRef]
- Speziale, P.; Pietrocola, G.; Rindi, S.; Provenzano, M.; Provenza, G.; Di Poto, A.; Visai, L.; Arciola, C.R. Structural and functional role of Staphylococcus aureus surface components recognizing adhesive matrix molecules of the host. Future Microbiol 2009, 4, 1337–1352. [Google Scholar] [CrossRef]
- Wilson, C.J.; Clegg, R.E.; Leavesley, D.I.; Pearcy, M.J. Mediation of Biomaterial–Cell Interactions by Adsorbed Proteins: A Review. Tissue Eng. 2005, 11, 1–18. [Google Scholar] [CrossRef]
- Bos, R.; Van der Mei, H.C.; Busscher, H.J. Physico-chemistry of initial microbial adhesive interactions—Its mechanisms and methods for study. FEMS Microbiol. Rev. 1999, 23, 179–230. [Google Scholar] [CrossRef]
- Ribeiro, M.; Monteiro, F.J.; Ferraz, M.P. Infection of orthopedic implants with emphasis on bacterial adhesion process and techniques used in studying bacterial-material interactions. Biomatter 2012, 2, 176–194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeo, I.-S.; Kim, H.-Y.; Lim, K.S.; Han, J.-S. Implant Surface Factors and Bacterial Adhesion: A Review of the Literature. Int. J. Artif. Organs 2012, 35, 762–772. [Google Scholar] [CrossRef] [PubMed]
- Flemming, H.-C.; Wingender, J.J. The biofilm matrix. Nat. Rev. Microbiol. 2010, 8, 623–633. [Google Scholar] [CrossRef] [PubMed]
- Orapiriyakul, W.; Young, P.S.; Damiati, L.; Tsimbouri, P.M. Antibacterial surface modification of titanium implants in orthopaedics. J. Tissue Eng. 2018, 9, 2041731418789838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dufrêne, Y.F.; Martínez-Martín, D.; Medalsy, I.; Alsteens, D.; Müller, D.J. Multiparametric imaging of biological systems by force-distance curve–based AFM. Nat. Methods 2013, 10, 847–854. [Google Scholar] [CrossRef]
- An, Y.H.; Friedman, R.J. Concise review of mechanisms of bacterial adhesion to biomaterial surfaces. J. Biomed. Mater. Res. 1998, 43, 338–348. [Google Scholar] [CrossRef]
- Bernhardt, T.; Semmler, M.L.; Schäfer, M.; Bekeschus, S.; Emmert, S.; Boeckmann, L. Plasma Medicine: Applications of Cold Atmospheric Pressure Plasma in Dermatology. Oxidative Med. Cell. Longev. 2019, 2019, 3873928. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.-J.; Kwon, J.-S.; Jiang, H.B.; Choi, E.H.; Park, G.; Kim, K.-M. The antibacterial effect of non-thermal atmospheric pressure plasma treatment of titanium surfaces according to the bacterial wall structure. Sci. Rep. 2019, 9, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.-Y.; Huang, X.-B.; Jiang, L.; Ma, Y.; Fan, A.-L.; Tang, B. Antibacterial Property of Cu Modified Stainless Steel by Plasma Surface Alloying. J. Iron Steel Res. Int. 2012, 19, 75–79. [Google Scholar] [CrossRef]
- Yang, J.; Bei, J.; Wang, S. Enhanced cell affinity of poly (d,l-lactide) by combining plasma treatment with collagen anchorage. Biomaterials 2002, 23, 2607–2614. [Google Scholar] [CrossRef]
- Wang, W.; Qi, W.; Xie, L.; Yang, X.; Li, J.; Zhang, Y. Microstructure and Corrosion Behavior of (CoCrFeNi)95Nb5 High-Entropy Alloy Coating Fabricated by Plasma Spraying. Materials 2019, 12, 694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koshuro, V.; Fomin, A.; Rodionov, I. Composition, structure and mechanical properties of metal oxide coatings produced on titanium using plasma spraying and modified by micro-arc oxidation. Ceram. Int. 2018, 44, 12593–12599. [Google Scholar] [CrossRef]
- Dinklage, A.; Klinger, T.; Marx, G.; Schweikhard, L. Plasma Physics: Confinement, Transport and Collective Effects; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2005; Volume 670. [Google Scholar]
- Chen, F.F. Introduction to Plasma Physics and Controlled Fusion; Springer: Berlin/Heidelberg, Germany, 1984; Volume 1. [Google Scholar]
- Laroussi, M.; Akan, T. Arc-Free Atmospheric Pressure Cold Plasma Jets: A Review. Plasma Process. Polym. 2007, 4, 777–788. [Google Scholar] [CrossRef]
- Von Keudell, A.; Schulz-Von Der Gathen, V.J. Foundations of low-temperature plasma physics—An introduction. Plasma Sources Sci. Technol. 2017, 26, 113001. [Google Scholar] [CrossRef] [Green Version]
- Fridman, G.; Friedman, G.; Gutsol, A.; Shekhter, A.B.; Vasilets, V.N.; Fridman, A. Applied Plasma Medicine. Plasma Process. Polym. 2008, 5, 503–533. [Google Scholar] [CrossRef]
- von Woedtke, T.; Reuter, S.; Masur, K.; Weltmann, K.-D. Plasmas for medicine. Phys. Rep. 2013, 530, 291–320. [Google Scholar] [CrossRef]
- Weltmann, K.D.; Kindel, E.; von Woedtke, T.; Hähnel, M.; Stieber, M.; Brandenburg, R.J.P. Atmospheric-pressure plasma sources: Prospective tools for plasma medicine. Pure Appl. Chem. 2010, 82, 1223–1237. [Google Scholar] [CrossRef]
- Tendero, C.; Tixier, C.; Tristant, P.; Desmaison, J.; Leprince, P. Atmospheric pressure plasmas: A review. Spectrochim. Acta Part B At. Spectrosc. 2006, 61, 2–30. [Google Scholar] [CrossRef]
- Lu, X.; Jiang, Z.; Xiong, Q.; Tang, Z.; Pan, Y. A single electrode room-temperature plasma jet device for biomedical applications. Appl. Phys. Lett. 2008, 92, 151504. [Google Scholar] [CrossRef]
- Kanazawa, S.; Kogoma, M.; Moriwaki, T.; Okazaki, S. Stable glow plasma at atmospheric pressure. J. Phys. D Appl. Phys. 1988, 21, 838–840. [Google Scholar] [CrossRef]
- Lu, X.; Laroussi, M.; Puech, V. On atmospheric-pressure non-equilibrium plasma jets and plasma bullets. Plasma Sources Sci. Technol. 2012, 21, 034005. [Google Scholar] [CrossRef]
- Kong, M.G.; Kroesen, G.; Morfill, G.; Nosenko, T.; Shimizu, T.; Van Dijk, J.; Zimmermann, J.L. Plasma medicine: An introductory review. New J. Phys. 2009, 11, 115012. [Google Scholar] [CrossRef]
- Kogelschatz, U.J.P. Silent discharges for the generation of ultraviolet and vacuum ultraviolet excimer radiation. Pure Appl. Chem. 1990, 62, 1667–1674. [Google Scholar] [CrossRef]
- Massines, F.; Rabehi, A.; Decomps, P.; Ben Gadri, R.; Ségur, P.; Mayoux, C. Experimental and theoretical study of a glow discharge at atmospheric pressure controlled by dielectric barrier. J. Appl. Phys. 1998, 83, 2950–2957. [Google Scholar] [CrossRef]
- Laroussi, M. Nonthermal decontamination of biological media by atmospheric-pressure plasmas: Review, analysis, and prospects. IEEE Trans. Plasma Sci. 2002, 30, 1409–1415. [Google Scholar] [CrossRef]
- Vasilev, K.; Griesser, S.S.; Griesser, H.J. Antibacterial Surfaces and Coatings Produced by Plasma Techniques. Plasma Process. Polym. 2011, 8, 1010–1023. [Google Scholar] [CrossRef]
- Kulkarni, M.; Patil-Sen, Y.; Junkar, I.; Kulkarni, C.V.; Lorenzetti, M.; Iglič, A. Wettability studies of topologically distinct titanium surfaces. Colloids Surfaces B Biointerfaces 2015, 129, 47–53. [Google Scholar] [CrossRef]
- Fauchais, P.; Vardelle, A.; Dussoubs, B. Quo Vadis Thermal Spraying? J. Therm. Spray Technol. 2001, 10, 44–66. [Google Scholar] [CrossRef]
- Cloutier, M.; Mantovani, D.; Rosei, F. Antibacterial Coatings: Challenges, Perspectives, and Opportunities. Trends Biotechnol. 2015, 33, 637–652. [Google Scholar] [CrossRef]
- Smith, R.W.; Mutasim, Z.Z. Reactive plasma spraying of wear-resistant coatings. J. Therm. Spray Technol. 1992, 1, 57–63. [Google Scholar] [CrossRef]
- Gérard, B.J.S. Application of thermal spraying in the automobile industry. Surf. Coat. Technol. 2006, 201, 2028–2031. [Google Scholar] [CrossRef]
- Yoshiba, M. Effect of hot corrosion on the mechanical performances of superalloys and coating systems. Corros. Sci. 1993, 35, 1115–1124. [Google Scholar] [CrossRef]
- Lee, J.-J.J.S. Application of inductively coupled plasma to CVD and PVD. Surf. Coat. Technol. 2005, 200, 31–34. [Google Scholar] [CrossRef]
- Schneider, J.M.; Rohde, S.; Sproul, W.D.; Matthews, A. Recent developments in plasma assisted physical vapour deposition. J. Phys. D Appl. Phys. 2000, 33, R173–R186. [Google Scholar] [CrossRef]
- Choy, K. Chemical vapour deposition of coatings. Prog. Mater. Sci. 2003, 48, 57–170. [Google Scholar] [CrossRef]
- Sardella, E.; Palumbo, F.; Camporeale, G.; Favia, P. Non-Equilibrium Plasma Processing for the Preparation of Antibacterial Surfaces. Materials 2016, 9, 515. [Google Scholar] [CrossRef] [Green Version]
- He, X.; Zhang, X.; Wang, X.; Qin, L. Review of Antibacterial Activity of Titanium-Based Implants’ Surfaces Fabricated by Micro-Arc Oxidation. Coatings 2017, 7, 45. [Google Scholar] [CrossRef] [Green Version]
- Simchen, F.; Sieber, M.; Kopp, A.; Lampke, T. Introduction to Plasma Electrolytic Oxidation—An Overview of the Process and Applications. Coatings 2020, 10, 628. [Google Scholar] [CrossRef]
- Rizwan, M.; Alias, R.; Zaidi, U.Z.; Mahmoodian, R.; Hamdi, M. Surface modification of valve metals using plasma electrolytic oxidation for antibacterial applications: A review. J. Biomed. Mater. Res. Part A 2018, 106, 590–605. [Google Scholar] [CrossRef]
- Dunleavy, C.; Golosnoy, I.; Curran, J.; Clyne, T. Characterisation of discharge events during plasma electrolytic oxidation. Surf. Coat. Technol. 2009, 203, 3410–3419. [Google Scholar] [CrossRef] [Green Version]
- Anders, A.J.S. Metal plasma immersion ion implantation and deposition: A review. Surf. Coat. Technol. 1997, 93, 158–167. [Google Scholar] [CrossRef] [Green Version]
- Anders, A.J.S. From plasma immersion ion implantation to deposition: A historical perspective on principles and trends. Surf. Coat. Technol. 2002, 156, 3–12. [Google Scholar] [CrossRef] [Green Version]
- Mändl, S.; Rauschenbach, B. Improving the biocompatibility of medical implants with plasma immersion ion implantation. Surf. Coat. Technol. 2002, 156, 276–283. [Google Scholar] [CrossRef]
- Lin, S.S.-H.; Yang, C.-M.; Chern, C.S.; Lin, C.-H. Inductive Plasma Doping. Google Patents, EP1501911A1, 2 February 2005. [Google Scholar]
- Nikiforov, A.; Deng, X.; Xiong, Q.; Cvelbar, U.; Degeyter, N.; Morent, R.; Leys, C. Non-thermal plasma technology for the development of antimicrobial surfaces: A review. J. Phys. D Appl. Phys. 2016, 49, 204002. [Google Scholar] [CrossRef]
- Bergemann, C.; Zaatreh, S.; Wegner, K.; Arndt, K.; Podbielski, A.; Bader, R.; Prinz, C.; Lembke, U.; Nebe, J.B. Copper as an alternative antimicrobial coating for implants—An in vitro study. World J. Transplant. 2017, 7, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Yonezawa, K.; Kawaguchi, M.; Kaneuji, A.; Ichiseki, T.; Iinuma, Y.; Kawamura, K.; Shintani, K.; Oda, S.; Taki, M.; Kawahara, N. Evaluation of Antibacterial and Cytotoxic Properties of a Fluorinated Diamond-Like Carbon Coating for the Development of Antibacterial Medical Implants. Antibiotics 2020, 9, 495. [Google Scholar] [CrossRef]
- Fielding, G.A.; Roy, M.; Bandyopadhyay, A.; Bose, S.J.A.b. Antibacterial and biological characteristics of plasma sprayed silver and strontium doped hydroxyapatite coatings. Acta Biomater. 2012, 8, 3144. [Google Scholar] [CrossRef] [Green Version]
- Ganjian, M.; Modaresifar, K.; Zhang, H.; Hagedoorn, P.-L.; Fratila-Apachitei, L.E.; Zadpoor, A.A. Reactive ion etching for fabrication of biofunctional titanium nanostructures. Sci. Rep. 2019, 9, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Kulkarni, M.; Mazare, A.; Gongadze, E.; Perutkova, Š.; Kralj-Iglič, V.; Milošev, I.; Schmuki, P.; Iglič, A.; Mozetič, M. Titanium nanostructures for biomedical applications. Nanotechnology 2015, 26, 062002. [Google Scholar] [CrossRef] [PubMed]
- Iglič, A.; Kulkarni, M.; Flasker, A.; Lokar, M.; Mrak-Poljšak, K.; Mazare, A.; Artenjak, A.; Cucnik, S.; Kralj, S.; Velikonja, A.; et al. Binding of plasma proteins to titanium dioxide nanotubes with different diameters. Int. J. Nanomed. 2015, 10, 1359–1373. [Google Scholar] [CrossRef] [Green Version]
- Monetta, T.; Bellucci, F. Strong and Durable Antibacterial Effect of Titanium Treated in Rf Oxygen Plasma: Preliminary Results. Plasma Chem. Plasma Process. 2014, 34, 1247–1256. [Google Scholar] [CrossRef]
- Huang, N.; Yang, P.; Leng, Y.; Chen, J.; Sun, H.; Wang, J.; Wang, G.; Ding, P.; Xi, T. Hemocompatibility of titanium oxide films. Biomater. 2003, 24, 2177–2187. [Google Scholar] [CrossRef]
- Riedel, N.A.; Smith, B.S.; Williams, J.D.; Popat, K.C. Improved thrombogenicity on oxygen etched Ti6Al4V surfaces. Mater. Sci. Eng. C 2012, 32, 1196–1203. [Google Scholar] [CrossRef]
- Chen, M.; Zamora, P.O.; Peña, L.; Som, P.; Osaki, S. NH3/O2 mixed gas plasmas alter the interaction of blood components with stainless steel. J. Biomed. Mater. Res. 2003, 67, 994–1000. [Google Scholar] [CrossRef]
- Modic, M.; Junkar, I.; Stana-Kleinschek, K.; Kostanjšek, R.; Mozetič, M.J.P.P. Morphology transformations of platelets on plasma activated surfaces. Plasma Process. Polym. 2014, 11, 596–605. [Google Scholar] [CrossRef]
- Junkar, I. Plasma treatment of amorphous and semicrystalline polymers for improved biocompatibility. Vacuum 2013, 98, 111–115. [Google Scholar] [CrossRef]
- Yeung, K.W.; Wu, S.; Zhao, Y.; Liu, X.; Kao, R.; Luk, K.; Cheung, K.; Chu, P.K.J.V. Antimicrobial effects of oxygen plasma modified medical grade Ti–6Al–4V alloy. Vacuum 2013, 89, 271–279. [Google Scholar] [CrossRef]
- Junkar, I.; Cvelbar, U.; Vesel, A.; Hauptman, N.; Mozetič, M. The Role of Crystallinity on Polymer Interaction with Oxygen Plasma. Plasma Process. Polym. 2009, 6, 667–675. [Google Scholar] [CrossRef]
- Coen, M.C.; Lehmann, R.; Groening, P.; Schlapbach, L. Modification of the micro- and nanotopography of several polymers by plasma treatments. Appl. Surf. Sci. 2003, 207, 276–286. [Google Scholar] [CrossRef]
- Duday, D.; Vreuls, C.; Moreno, M.; Frache, G.; Boscher, N.D.; Zocchi, G.; Archambeau, C.; Van De Weerdt, C.; Martial, J.; Choquet, P. Atmospheric pressure plasma modified surfaces for immobilization of antimicrobial nisin peptides. Surf. Coat. Technol. 2013, 218, 152–161. [Google Scholar] [CrossRef]
- Santos-Coquillat, A.; Tenorio, R.G.; Mohedano, M.; Martinez-Campos, E.; Arrabal, R.; Matykina, E. Tailoring of antibacterial and osteogenic properties of Ti6Al4V by plasma electrolytic oxidation. Appl. Surf. Sci. 2018, 454, 157–172. [Google Scholar] [CrossRef]
- Ponomarev, V.A.; Orlov, E.A.; Malikov, N.A.; Tarasov, Y.V.; Sheveyko, A.N.; Permyakova, E.S.; Kuptsov, K.A.; Dyatlov, I.A.; Ignatov, S.G.; Ilnitskaya, A.S.; et al. Ag(Pt) nanoparticles-decorated bioactive yet antibacterial Ca- and P-doped TiO2 coatings produced by plasma electrolytic oxidation and ion implantation. Appl. Surf. Sci. 2020, 516, 146068. [Google Scholar] [CrossRef]
- Zhou, T.; Liu, J.; Zhang, X.; Shen, B.; Yang, J.; Hu, W.; Liu, L. The antibacterial W-containing microarc oxidation coating on Ti6Al4V. Surf. Coat. Technol. 2019, 374, 242–252. [Google Scholar] [CrossRef]
- Miola, M.; Ferraris, S.; Di Nunzio, S.; Robotti, P.F.; Bianchi, G.; Fucale, G.; Maina, G.; Cannas, M.; Gatti, S.; Masse’, A.; et al. Surface silver-doping of biocompatible glasses to induce antibacterial properties. Part II: Plasma sprayed glass-coatings. J. Mater. Sci. Mater. Electron. 2008, 20, 741–749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brohede, U.; Forsgren, J.; Roos, S.; Mihranyan, A.; Engqvist, H.; Strømme, M. Multifunctional implant coatings providing possibilities for fast antibiotics loading with subsequent slow release. J. Mater. Sci. Mater. Med. 2009, 20, 1859–1867. [Google Scholar] [CrossRef] [PubMed]
- Kang, B.-M.; Jeong, W.-J.; Park, G.-C.; Yoon, D.-J.; Ahn, H.-G.; Lim, Y.-S. The Characteristics of an Antibacterial TiAgN Thin Film Coated by Physical Vapor Deposition Technique. J. Nanosci. Nanotechnol. 2015, 15, 6020–6023. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zheng, X.; Xie, Y.; Ding, C.; Ruan, H.; Fan, C. Anti-bacterial and cytotoxic properties of plasma sprayed silver-containing HA coatings. J. Mater. Sci. Mater. Med. 2008, 19, 3603–3609. [Google Scholar] [CrossRef]
- Yoshinari, M.; Oda, Y.; Kato, T.; Okuda, K. Influence of surface modifications to titanium on antibacterial activity in vitro. Biomaterials 2001, 22, 2043–2048. [Google Scholar] [CrossRef]
- Xu, J.; Ding, G.; Li, J.; Yang, S.; Fang, B.; Sun, H.; Zhou, Y. Zinc-ion implanted and deposited titanium surfaces reduce adhesion of Streptococccus mutans. Appl. Surf. Sci. 2010, 256, 7540–7544. [Google Scholar] [CrossRef]
- Xu, J.; Li, Y.; Zhou, X.; Li, Y.; Gao, Z.D.; Song, Y.Y.; Schmuki, P.J.C.A.E.J. Graphitic C3N4-Sensitized TiO2 Nanotube Layers: A Visible-Light Activated Efficient Metal-Free Antimicrobial Platform. Chem. Eur. J. 2016, 22, 3947–3951. [Google Scholar] [CrossRef] [Green Version]
- Gu, M.; Lv, L.; Du, F.; Niu, T.; Chen, T.; Xia, D.; Wang, S.; Zhao, X.; Liu, J.; Liu, Y.; et al. Effects of thermal treatment on the adhesion strength and osteoinductive activity of single-layer graphene sheets on titanium substrates. Sci. Rep. 2018, 8, 1–15. [Google Scholar] [CrossRef]
- Cerchier, P.; Pezzato, L.; Brunelli, K.; Dolcet, P.; Bartolozzi, A.; Bertani, R.; Dabalà, M. Antibacterial effect of PEO coating with silver on AA7075. Mater. Sci. Eng. C 2017, 75, 554–564. [Google Scholar] [CrossRef] [PubMed]
- Karabudak, F.; Yeşildal, R.; Şüküroğlu, E.E.; Şüküroğlu, S.; Zamanlou, H.; Dikbaş, N.; Bayındır, F.; Şen, S.; Totik, Y. An Investigation of Corrosion Resistance and Antibacterial Sensitivity Properties of Nano-Ag-Doped TiO2 Coating and TiO2 Coating Grown on NiTi Alloy with the Micro-Arc Oxidation Process. Arab. J. Sci. Eng. 2017, 42, 2329–2339. [Google Scholar] [CrossRef]
- Li, Y.; Chen, D.; Sheng, Y.; Li, W.; Wang, X. In situ preparation of antibacterial Ag particles on Ti6Al4V surfaces by spray deposition. Surf. Innov. 2021, 9, 166–173. [Google Scholar] [CrossRef]
- Hryniewicz, T. Plasma Electrolytic Oxidation of Metals and Alloys. Metals 2018, 8, 1058. [Google Scholar] [CrossRef] [Green Version]
- Benčina, M.; Junkar, I.; Zaplotnik, R.; Valant, M.; Iglič, A.; Mozetič, M. Plasma-Induced Crystallization of TiO2 Nanotubes. Materials 2019, 12, 626. [Google Scholar] [CrossRef] [Green Version]
- Del Curto, B.; Brunella, M.; Giordano, C.; Pedeferri, M.; Valtulina, V.; Visai, L.; Cigada, A. Decreased Bacterial Adhesion to Surface-Treated Titanium. Int. J. Artif. Organs 2005, 28, 718–730. [Google Scholar] [CrossRef] [Green Version]
- Gallardomoreno, A.; Pachaolivenza, M.; Saldaña, L.; Perezgiraldo, C.; Bruque, J.M.; Vilaboa, N.; Gonzalezmartin, M. In vitro biocompatibility and bacterial adhesion of physico-chemically modified Ti6Al4V surface by means of UV irradiation. Acta Biomater. 2009, 5, 181–192. [Google Scholar] [CrossRef]
- Sumita, T.; Yamaki, T.; Yamamoto, S.; Miyashita, A. Photo-induced surface charge separation of highly oriented TiO2 anatase and rutile thin films. Appl. Surf. Sci. 2002, 200, 21–26. [Google Scholar] [CrossRef]
- Jalvo, B.; Faraldos, M.; Bahamonde, A.; Rosal, R. Antimicrobial and antibiofilm efficacy of self-cleaning surfaces functionalized by TiO2 photocatalytic nanoparticles against Staphylococcus aureus and Pseudomonas putida. J. Hazard. Mater. 2017, 340, 160–170. [Google Scholar] [CrossRef]
- Mitoraj, D.; Jańczyk, A.; Strus, M.; Kisch, H.; Stochel, G.; Heczko, P.B.; Macyk, W. Visible light inactivation of bacteria and fungi by modified titanium dioxide. Photochem. Photobiol. Sci. 2007, 6, 642–648. [Google Scholar] [CrossRef]
- Foster, H.A.; Ditta, I.B.; Varghese, S.; Steele, A. Photocatalytic disinfection using titanium dioxide: Spectrum and mechanism of antimicrobial activity. Appl. Microbiol. Biotechnol. 2011, 90, 1847–1868. [Google Scholar] [CrossRef]
- Mccullagh, C.; Robertson, J.M.C.; Bahnemann, D.W.; Robertson, P.K.J. The application of TiO2 photocatalysis for disinfection of water contaminated with pathogenic micro-organisms: A review. Res. Chem. Intermed. 2007, 33, 359–375. [Google Scholar] [CrossRef]
- Watanabe, T.; Nakajima, A.; Wang, R.; Minabe, M.; Koizumi, S.; Fujishima, A.; Hashimoto, K. Photocatalytic activity and photoinduced hydrophilicity of titanium dioxide coated glass. Thin Solid Films 1999, 351, 260–263. [Google Scholar] [CrossRef]
- Sakai, N.; Fujishima, A.; Watanabe, T.; Hashimoto, K. Quantitative Evaluation of the Photoinduced Hydrophilic Conversion Properties of TiO2Thin Film Surfaces by the Reciprocal of Contact Angle. J. Phys. Chem. B 2003, 107, 1028–1035. [Google Scholar] [CrossRef]
- Bonetta, S.; Bonetta, S.; Motta, F.; Strini, A.; Carraro, E. Photocatalytic bacterial inactivation by TiO2-coated surfaces. AMB Express 2013, 3, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aita, H.; Hori, N.; Takeuchi, M.; Suzuki, T.; Yamada, M.; Anpo, M.; Ogawa, T. The effect of ultraviolet functionalization of titanium on integration with bone. Biomaterials 2009, 30, 1015–1025. [Google Scholar] [CrossRef]
- Choi, S.-H.; Jeong, W.-S.; Cha, J.-Y.; Lee, J.-H.; Yu, H.-S.; Choi, E.-H.; Kim, K.-M.; Hwang, C.-J. Erratum: Corrigendum: Time-dependent effects of ultraviolet and nonthermal atmospheric pressure plasma on the biological activity of titanium. Sci. Rep. 2016, 6, 36430. [Google Scholar] [CrossRef] [Green Version]
- Helbig, R.; Günther, D.; Friedrichs, J.; Rößler, F.; Lasagni, A.-F.; Werner, C. The impact of structure dimensions on initial bacterial adhesion. Biomater. Sci. 2016, 4, 1074–1078. [Google Scholar] [CrossRef] [Green Version]
- Hizal, F.; Rungraeng, N.; Lee, J.; Jun, S.; Busscher, H.J.; Van Der Mei, H.C.; Choi, C.-H. Nanoengineered Superhydrophobic Surfaces of Aluminum with Extremely Low Bacterial Adhesivity. ACS Appl. Mater. Interfaces 2017, 9, 12118–12129. [Google Scholar] [CrossRef]
- Lu, N.; Zhang, W.; Weng, Y.; Chen, X.; Cheng, Y.; Zhou, P. Fabrication of PDMS surfaces with micro patterns and the effect of pattern sizes on bacteria adhesion. Food Control. 2016, 68, 344–351. [Google Scholar] [CrossRef]
- Kovach, Y.E.; Zhang, F.; Gao, F.; Foster, J.E. Study of plasma induced nanostructure formation and surface morphology changes on tungsten and stainless steel at atmospheric pressure. J. Vacuum Sci. Technol. Vacuum Surf. Films 2019, 37, 011301. [Google Scholar] [CrossRef]
- Aliofkhazraei, M.; Rouhaghdam, A.S.; Gupta, P. Nano-Fabrication by Cathodic Plasma Electrolysis. Crit. Rev. Solid State Mater. Sci. 2011, 36, 174–190. [Google Scholar] [CrossRef]
- Vassallo, E.; Pedroni, M.; Silvetti, T.; Morandi, S.; Toffolatti, S.L.; Angella, G.; Brasca, M. Bactericidal performance of nanostructured surfaces by fluorocarbon plasma. Mater. Sci. Eng. C 2017, 80, 117–121. [Google Scholar] [CrossRef]
- Veerachamy, S.; Hameed, P.; Sen, D.; Dash, S.; Manivasagam, G. Studies on Mechanical, Biocompatibility and Antibacterial Activity of Plasma Sprayed Nano/Micron Ceramic Bilayered Coatings on Ti–6Al–4V Alloy for Biomedical Application. J. Nanosci. Nanotechnol. 2018, 18, 4515–4523. [Google Scholar] [CrossRef]
- Jaggessar, A.; Shahali, H.; Mathew, A.; Yarlagadda, P.K.D.V. Bio-mimicking nano and micro-structured surface fabrication for antibacterial properties in medical implants. J. Nanobiotechnology 2017, 15, 1–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elbourne, A.; Coyle, V.E.; Truong, V.K.; Sabri, Y.M.; Kandjani, A.E.; Bhargava, S.K.; Ivanova, E.P.; Crawford, R.J. Multi-directional electrodeposited gold nanospikes for antibacterial surface applications. Nanoscale Adv. 2018, 1, 203–212. [Google Scholar] [CrossRef] [Green Version]
- Ivanova, E.P.; Hasan, J.; Webb, H.K.; Vervinskas, G.; Juodkazis, S.; Truong, V.K.; Wu, A.H.; Lamb, R.N.; Baulin, V.A.; Watson, G.S.; et al. Bactericidal activity of black silicon. Nat. Commun. 2013, 4, 2838. [Google Scholar] [CrossRef]
- Berne, C.; Ellison, C.K.; Ducret, A.; Brun, Y.V. Bacterial adhesion at the single-cell level. Nat. Rev. Genet. 2018, 16, 616–627. [Google Scholar] [CrossRef] [PubMed]
- Khorasani, M.; Mirzadeh, H. Effect of oxygen plasma treatment on surface charge and wettability of PVC blood bag—In vitro assay. Radiat. Phys. Chem. 2007, 76, 1011–1016. [Google Scholar] [CrossRef]
- Huang, H.-H.; Shiau, D.-K.; Chen, C.-S.; Chang, J.-H.; Wang, S.; Pan, H.; Wu, M.-F. Nitrogen plasma immersion ion implantation treatment to enhance corrosion resistance, bone cell growth, and antibacterial adhesion of Ti-6Al-4V alloy in dental applications. Surf. Coat. Technol. 2019, 365, 179–188. [Google Scholar] [CrossRef]



| Author | Plasma Treatment Technique | Material | Bacteria | Effect |
|---|---|---|---|---|
| Miola et al. [118] | Plasma spray | Silver doped glass-coating on Ti alloy | Staphylococcus Aureus | The coating induced antibacterial activity. The surface gained bacteriostatic properties without any cytotoxicity. |
| Brohede et al. [119] | PVD | Bioactive TiO2 anatase with hydroxyapatite (HA) loaded with an antibiotic (Amoxicillin, Gentamicin sulfate, Tobramycin, and Cephalothin) | Staphylococcus Aureus | After 24 the drug release was high enough to achieve bacterial inhibition. Longer loading times do not mean higher drug release. |
| Kang et al. [120] | PVD | TiAgN thin film on Ti | Streptococcus mutans | Antibacterial properties of TiAgN coating were evident at 5 wt% Ag concentration. No cytotoxic effect on (human gingival fibroblast (HGF) cells was detected. The proliferation of HGF cells even increased after exposure to various AG content on TiAg alloy. |
| Cao et al. [18] | Plasma spray/PIII | Ag nano particles (NP) 5–25 nm incorporated into titanium oxide coating | Streptococcus aureus, Echerichia coli | The size of Ag NP influenced the biocidal activity. Larger particles (5–25 nm) stimulate tougher oxidation reactions than smaller ones (~4 nm). No cytotoxic effect of Ag NP on osteoblast-like cells from mouse (MG63 and MC3T3 cell lines), the cytocompatibility was improved. |
| Fielding et al. [101] | Plasma spray | Pure titanium coated with HA with silver and strontium 155 | Pseudomonas aeruginosa | Improved antibacterial activity against P. aeruginosa and increased viability, proliferation, and differentiation of human osteoblast cells (hFOB), compared to only HA-coated samples. |
| Chen et al. [121] | Plasma spray | Titanium substrate coated with HA with silver 158 | Escherichia coli, Pseudomonas aeruginosa, and Staphylococcus aureus | The HA-Ag coating exhibited high antibacterial activity against all three bacteria. The in vitro study on fibroblast cell line L929 showed no cytotoxicity or hemolytic characteristics for the HA-Ag coating |
| Yoshinari et al. [122] | PIII and deposition 162 | F+ ion implementation | Porphyromonas gingivalis, Actinobacillus actinomycetemcomitans | F+ implanted samples exhibited significant inhibition of bacterial growth for both bacteria. Other surface modified samples did not exhibit antibacterial activity. The F+ implanted samples did not inhibit the proliferation of fibroblast cells (L929 cell line) |
| Xu et al. [123] | PIII and deposition | Zn ion deposition on titanium surface | Streptococcus mutans | With increasing Zn concentration on the titanium surface, the bacterial adhesion on samples decreased |
| Xu et al. [124] | CVD 167 | Graphitic C3N4 on aligned TiO2 nanotube layer | Escherichia coli | Graphitic C3N4 composite showed bactericidal properties under visible-light-induced photocatalytic formation of reactive oxidative species. |
| Gu et al. [125] | CVD 176 | Single-layer graphene sheets onto titanium discs | Staphylococcus aureus, Escherichia coli | Graphene coating of titanium discs improved cell adhesion and osteogenic differentiation of hASC, hGF and hBMMSC cell lines. Graphene surface showed antibacterial properties on both E. Coli and S. aureus bacteria. |
| Cerchier et al. [126] | PEO | Ag particles onto Al surface in an electrolyte | Staphylococcus aureus, Escherichia coli | Silver NP on the substrate depicted antibacterial activity against both E. coli and S. aureus. |
| Karabudak et al. [127] | MS and MAO | Ag/TO2 and Ag NP/TiO2 onto NiTi | Staphylococcus aureus, Pseudomonas aeruginosa, Listeria monocytogenes, Escherichia coli, Yersinia enterocolitica, Salmonella Enteritidis, Bacillis subtilis | Samples with Ag NP TiO2 showed antibacterial activity on S. aureus, P. aeruginosa, L. monocytogenes, E. coli bacteria, which are classified as moderately sensitive, while Y. enterocolitica, S. Enteritidis, B. subtilis were classified as resistant to the antibacterial coating. Non-coated NiTi surface was found with the best antibacterial activity for all bacteria. |
| Jin, et al. [13] | PVD | Cu-Ti ions coated onto 316L stainless steel | Escherichia coli | The Cu-Ti coating exhibited great antibacterial activity with an effective reduction of 99.9% of E. coli bacteria in the first 12 h. The authors predict that the release of Cu ions has bactericidal properties on E. coli. |
| Li et al. [128] | Plasma spray | Ag nanoparticles onto Ti6Al4V | Staphylococcus aureus, Escherichia coli | Ag coated surface exhibited excellent antibacterial activity. |
| Lee et al. [59] | APPJ Direct plasma treatment of bacteria | Titanium surface | Streptococcus. mutans, Staphylococcus. aureus, Klebsiella oxytoca and Klebsiella pneumoniae on NTAPPJ treated titanium | Lower adhesion of bacteria and biofilm formation rate compared to untreated samples. The adhesion of cells and biofilm formation rate of gram-negative bacteria was significantly lower than gram-positive bacteria. |
| Material | Concentration at% | |||||
|---|---|---|---|---|---|---|
| C | O | Ti | N | Al | V | |
| Ti | 68.4 | 26.1 | 4.6 | 0.9 | / | / |
| Ti + P | 36.4 | 51.1 | 12.5 | / | / | / |
| Ti6Al4V | 69.1 | 27.2 | 2.9 | / | 0.7 | 0.1 |
| Ti6Al4V + P | 43.8 | 42.3 | 11.4 | / | 2.3 | 0.2 |
| NiTi | 71.7 | 25.0 | 2.0 | 1.3 | / | / |
| NiTi + P | 21.0 | 50.5 | 28.5 | / | / | / |
| Untreated | Plasma Treated | |
|---|---|---|
| Ti6Al4V (AFM) | 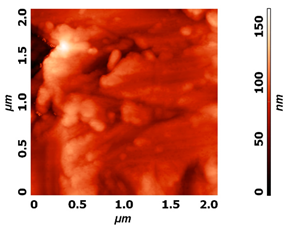 | 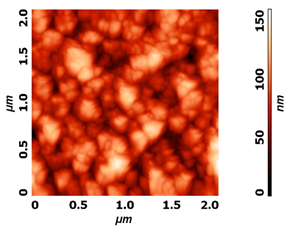 |
| NiTi (AFM) | 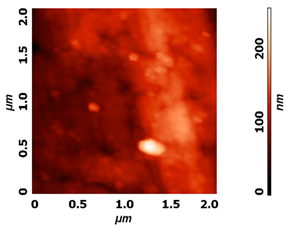 | 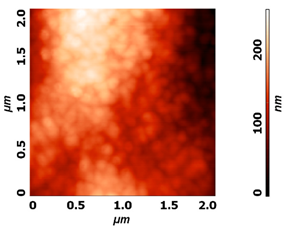 |
| Ti (SEM) |  |  |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benčina, M.; Resnik, M.; Starič, P.; Junkar, I. Use of Plasma Technologies for Antibacterial Surface Properties of Metals. Molecules 2021, 26, 1418. https://doi.org/10.3390/molecules26051418
Benčina M, Resnik M, Starič P, Junkar I. Use of Plasma Technologies for Antibacterial Surface Properties of Metals. Molecules. 2021; 26(5):1418. https://doi.org/10.3390/molecules26051418
Chicago/Turabian StyleBenčina, Metka, Matic Resnik, Pia Starič, and Ita Junkar. 2021. "Use of Plasma Technologies for Antibacterial Surface Properties of Metals" Molecules 26, no. 5: 1418. https://doi.org/10.3390/molecules26051418








