Effect of Extract and Synthesized Derivatives of Isolated Compound from Symplocos chinensis f. Pilosa Ohwi on Neuropathic Pain in Mice
Abstract
1. Introduction
2. Results
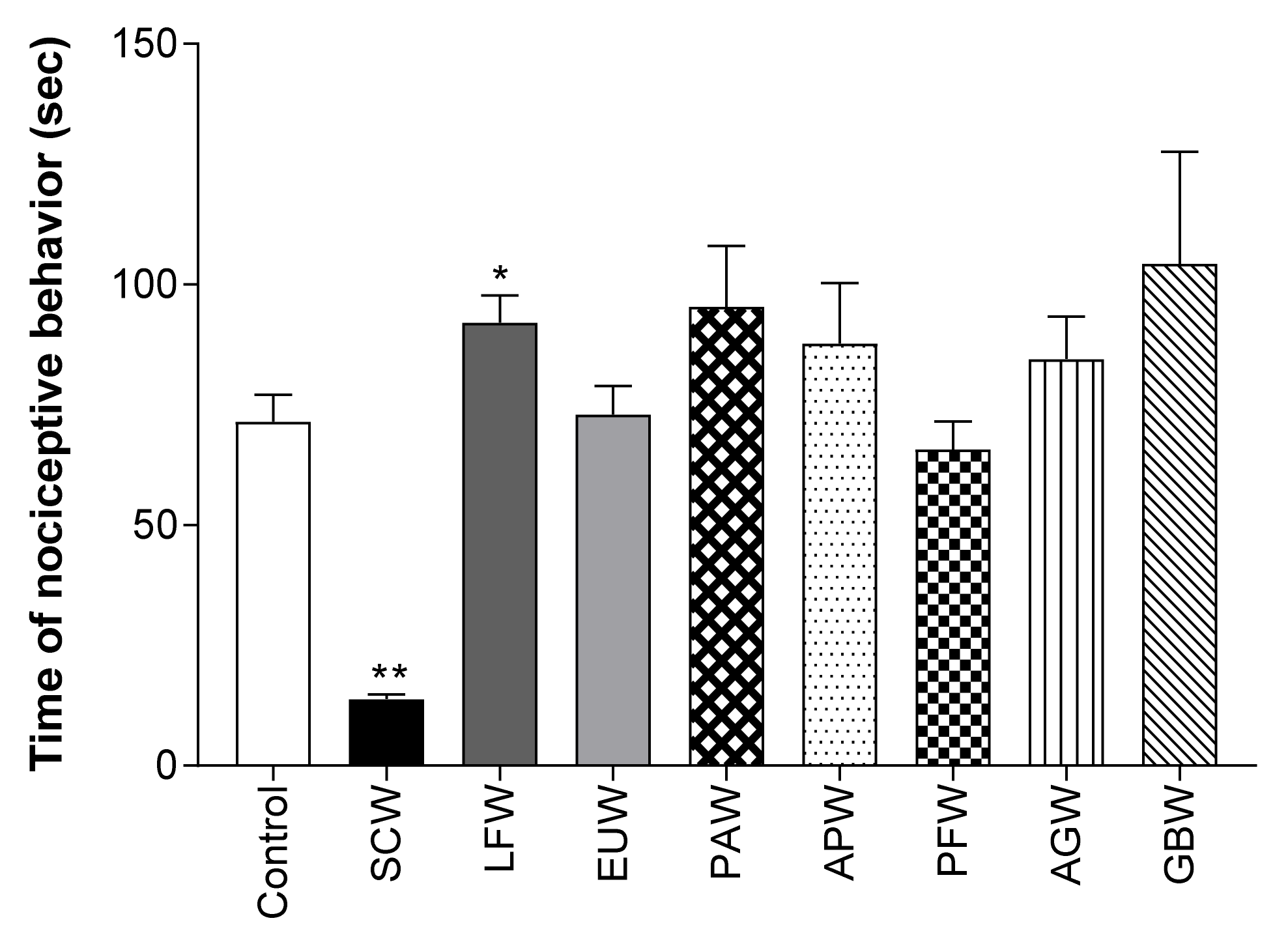
2.1. Antinociceptive Effect of Various Plant Water Extracts in Acetic Acid-Induced Writhing Test
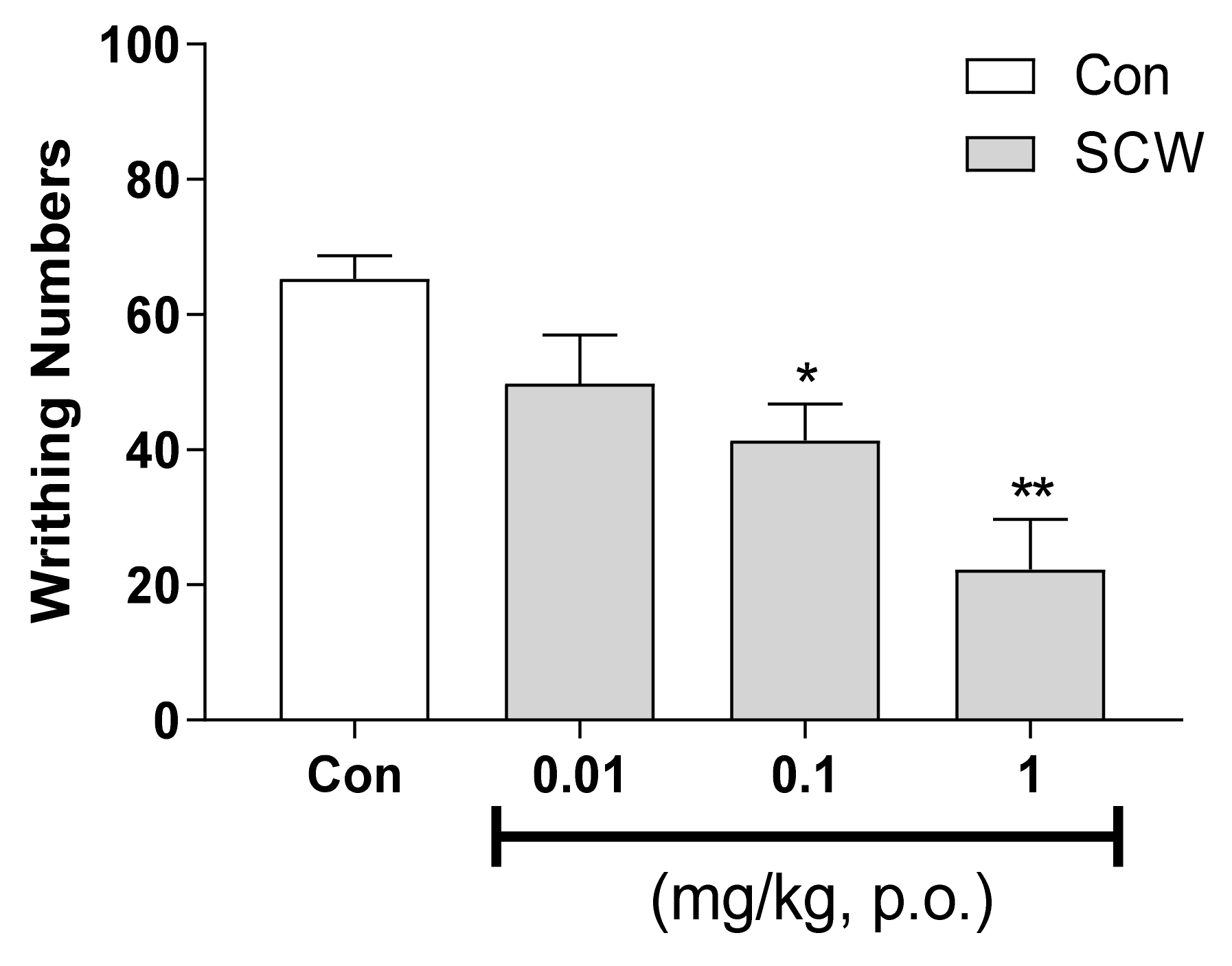
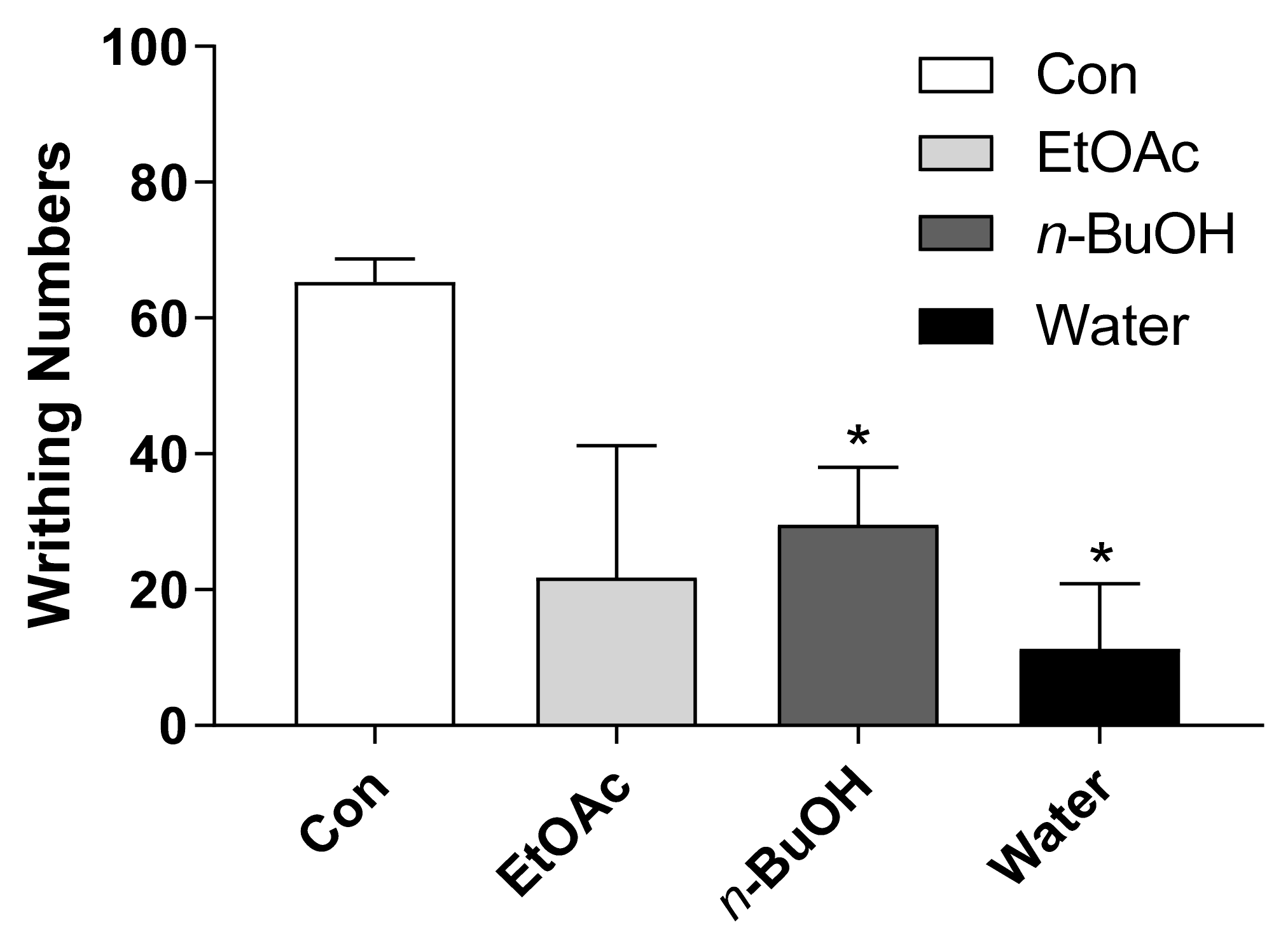
2.2. Antinociceptive Effect of SCW in Acetic Acid-Induced Writhing Test
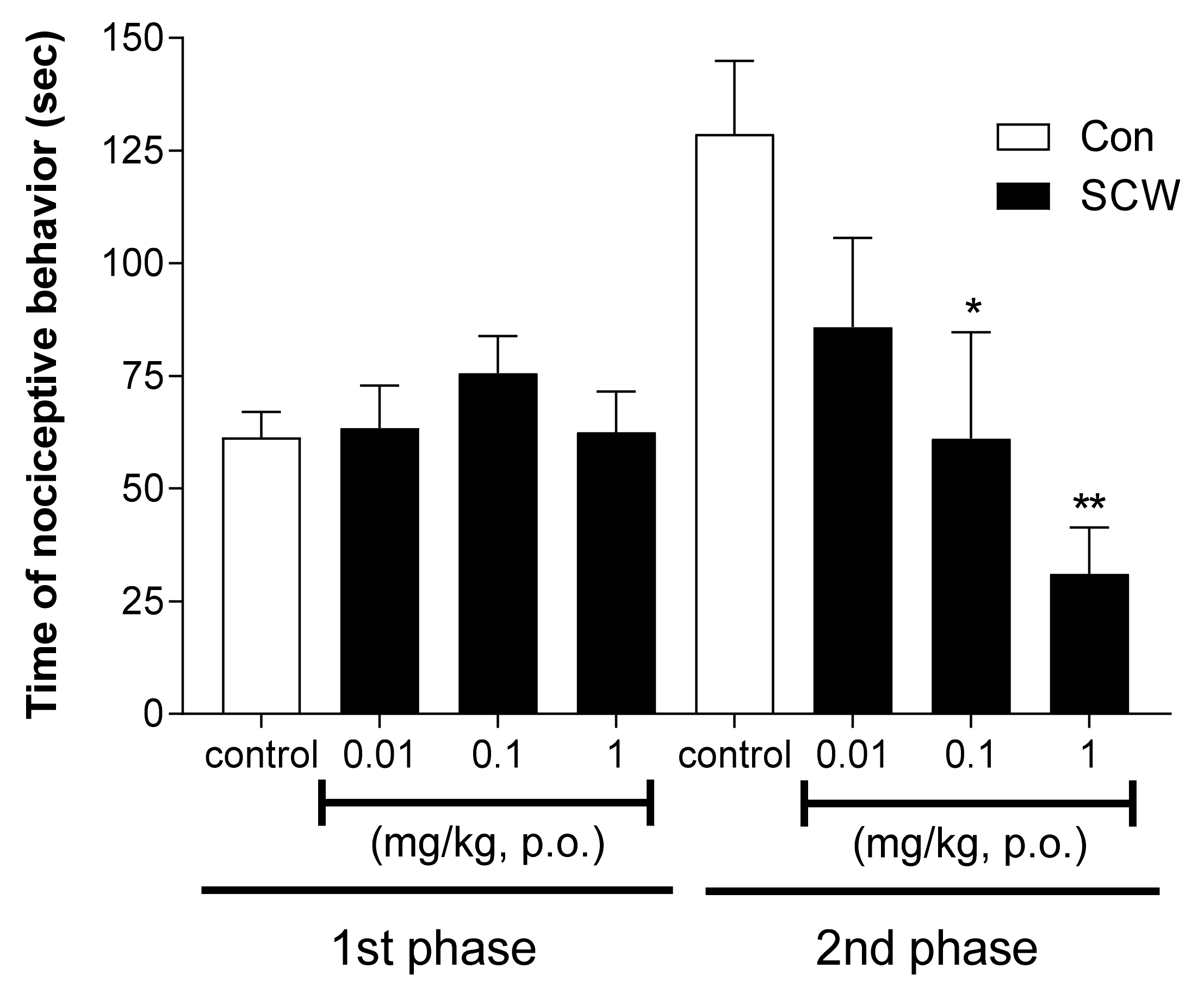
2.3. Antinociceptive Effect of SCW on 5% Formalin-Induced Nociception
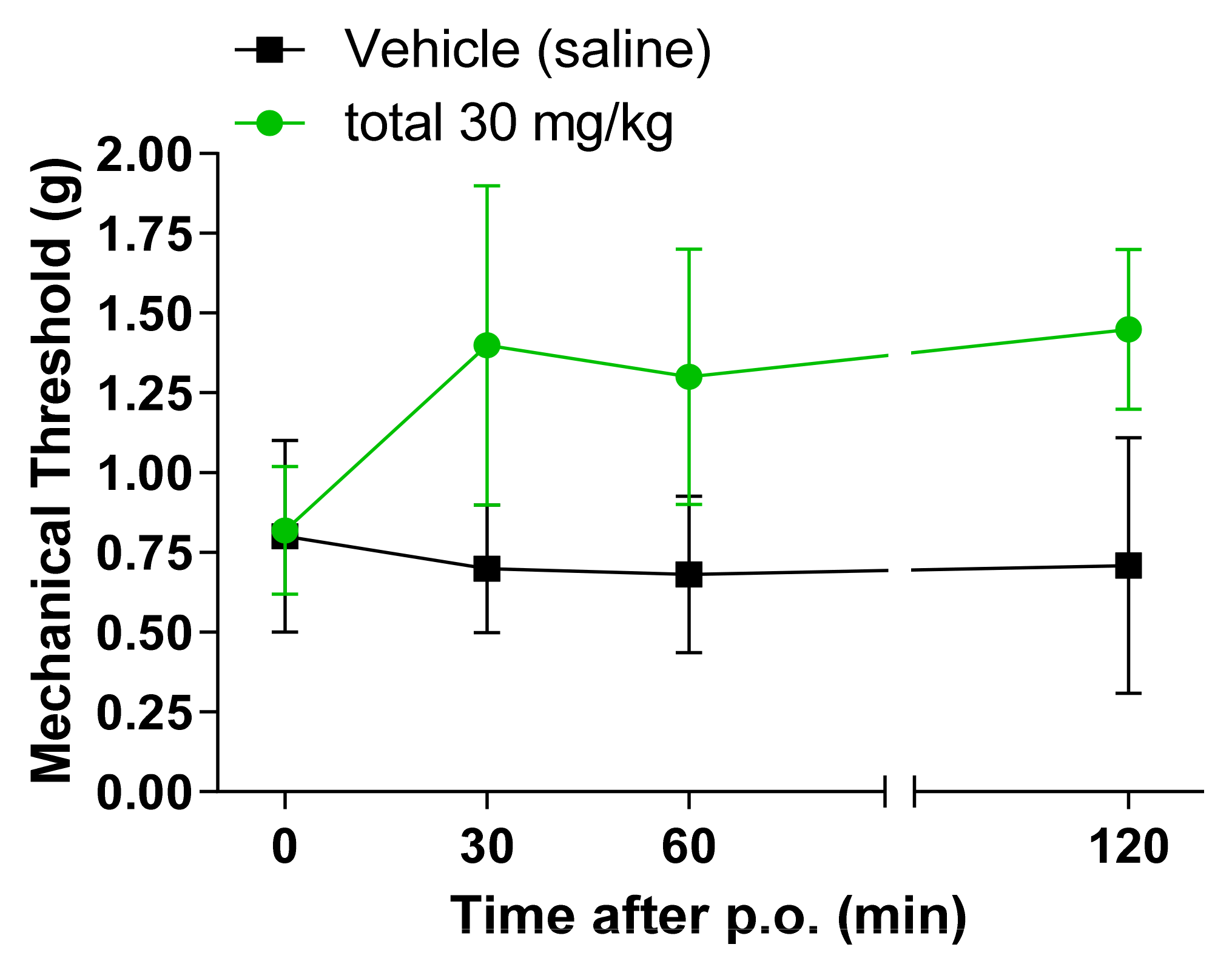
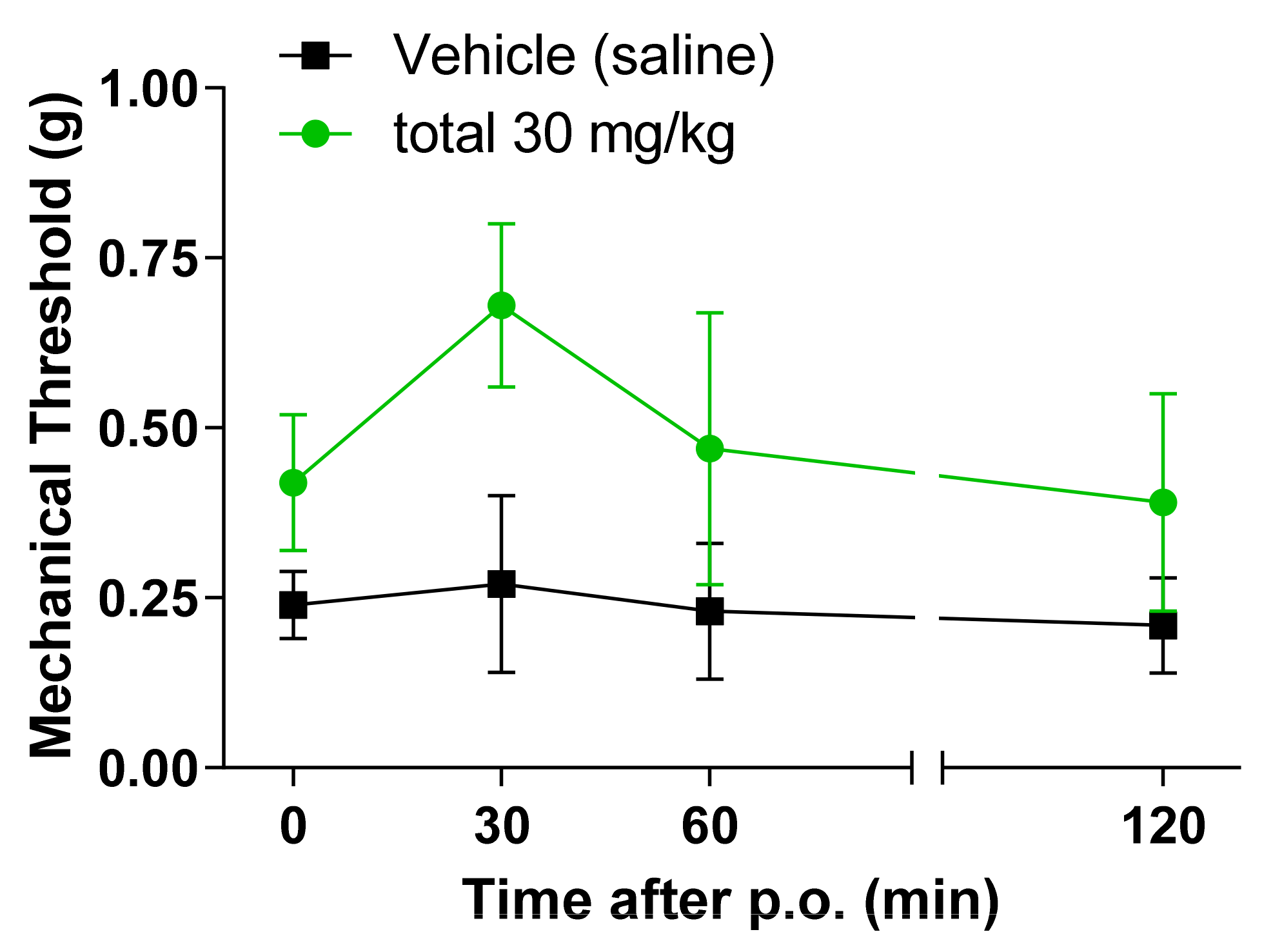
2.4. Antinociceptive Effect of SCW on Mechanical Pain Thresholds in CCI and SNI Neuropathic Pain Model
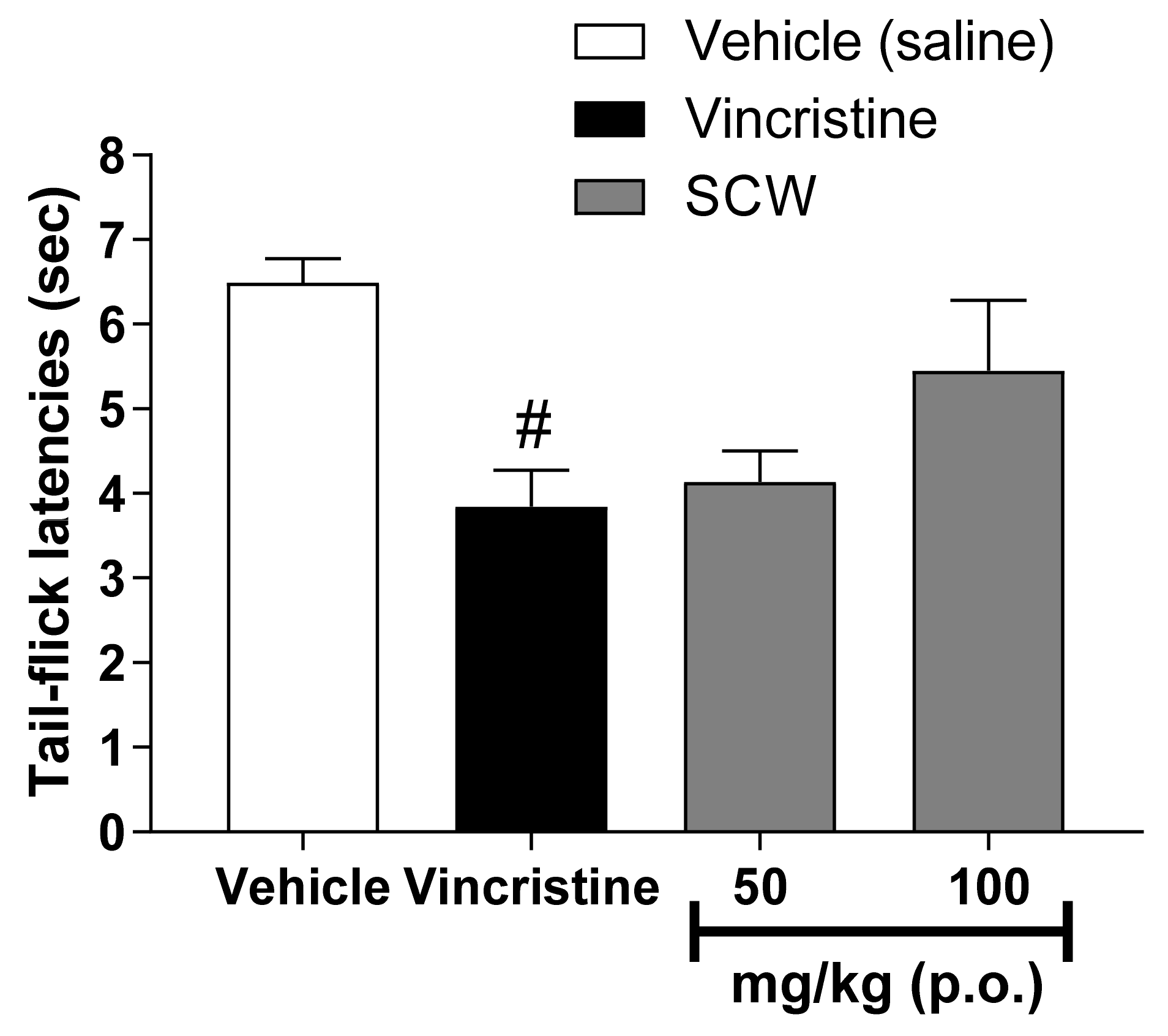
2.5. Antinociceptive Effect of SCW on the Tail-Flick Test in Vincristine Induced Pain Model
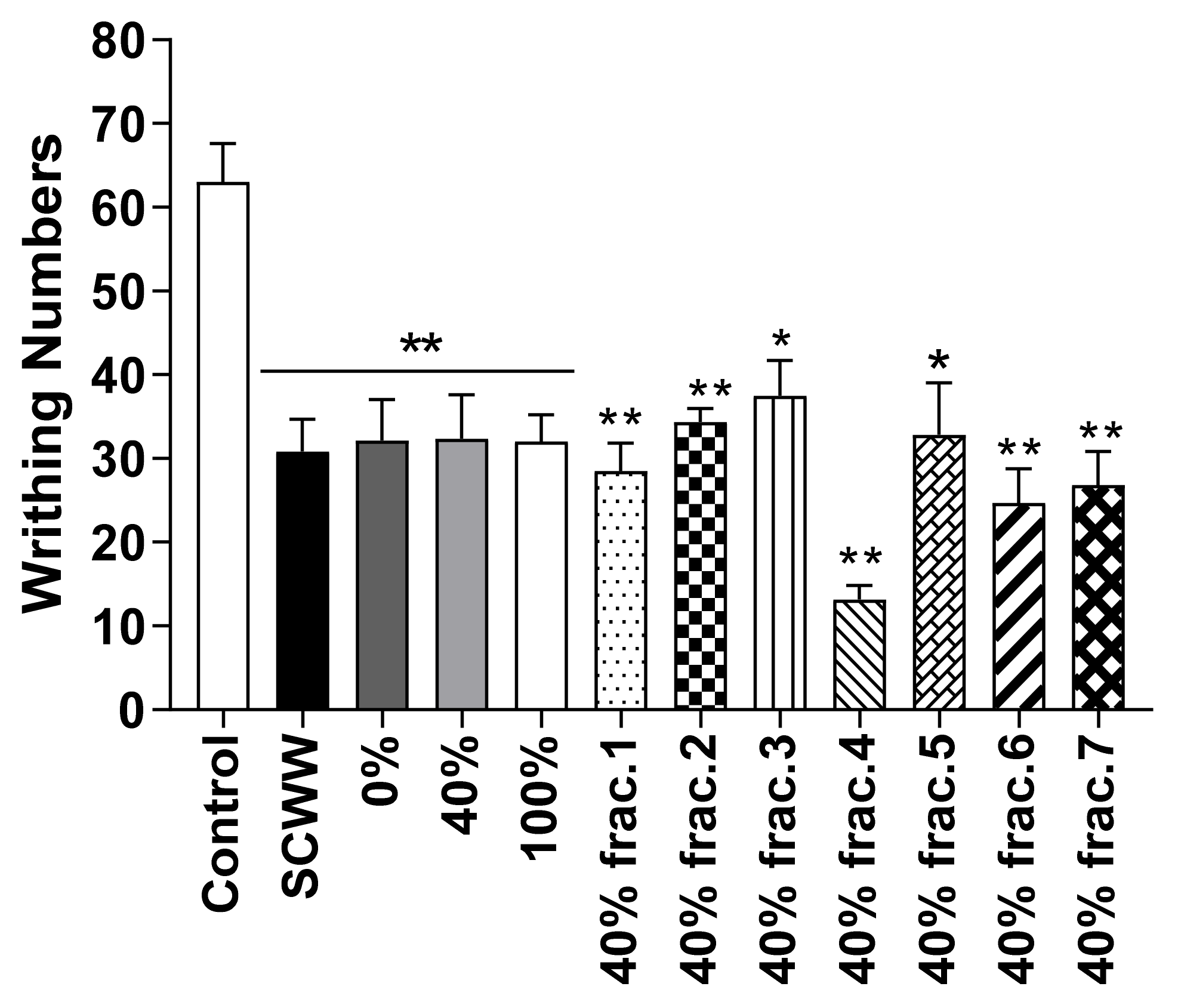
2.6. Antinociceptive Effect of SCW Fractions in Acetic Acid-Induced Writhing Test
2.7. Antinociceptive Effect of Isolated Sub-Fractions from SCWW in Acetic Acid-Induced Writhing Test
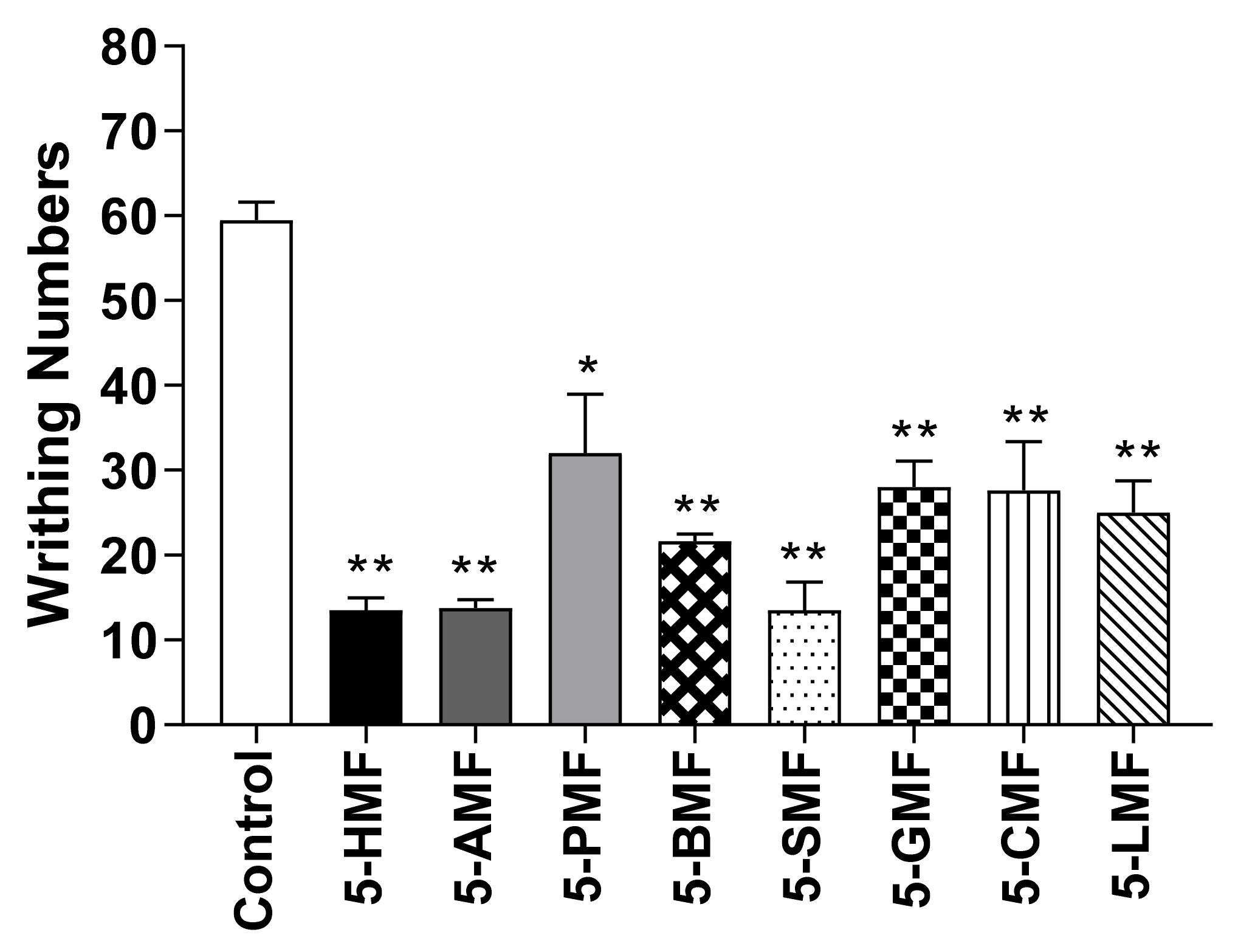
2.8. Antinociceptive Effect of Isolated 5-HMF and Derivatives in Acetic Acid-Induced Writhing Test and on 5% Formalin-Induced Nociception
2.9. Antinociceptive Effect of 5-SMF and Gabapentin in Acetic Acid-Induced Writhing Test
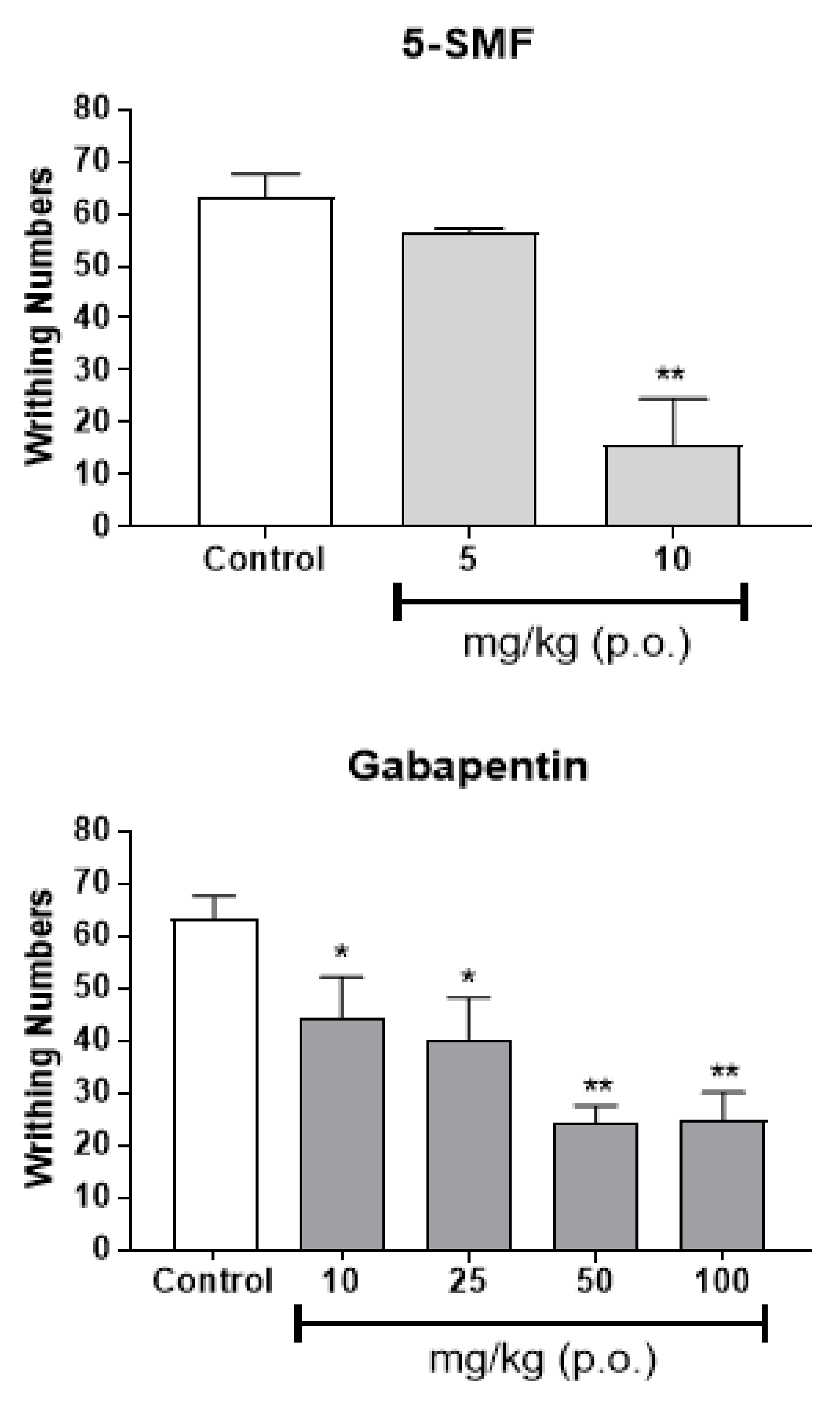
2.10. Antinociceptive Effect of 5-SMF and Gabapentin on 5% Formalin-Induced Nociception
2.11. Antinociceptive Effect of 5-SMF in Tail-Flick and Hot-Plate Tests
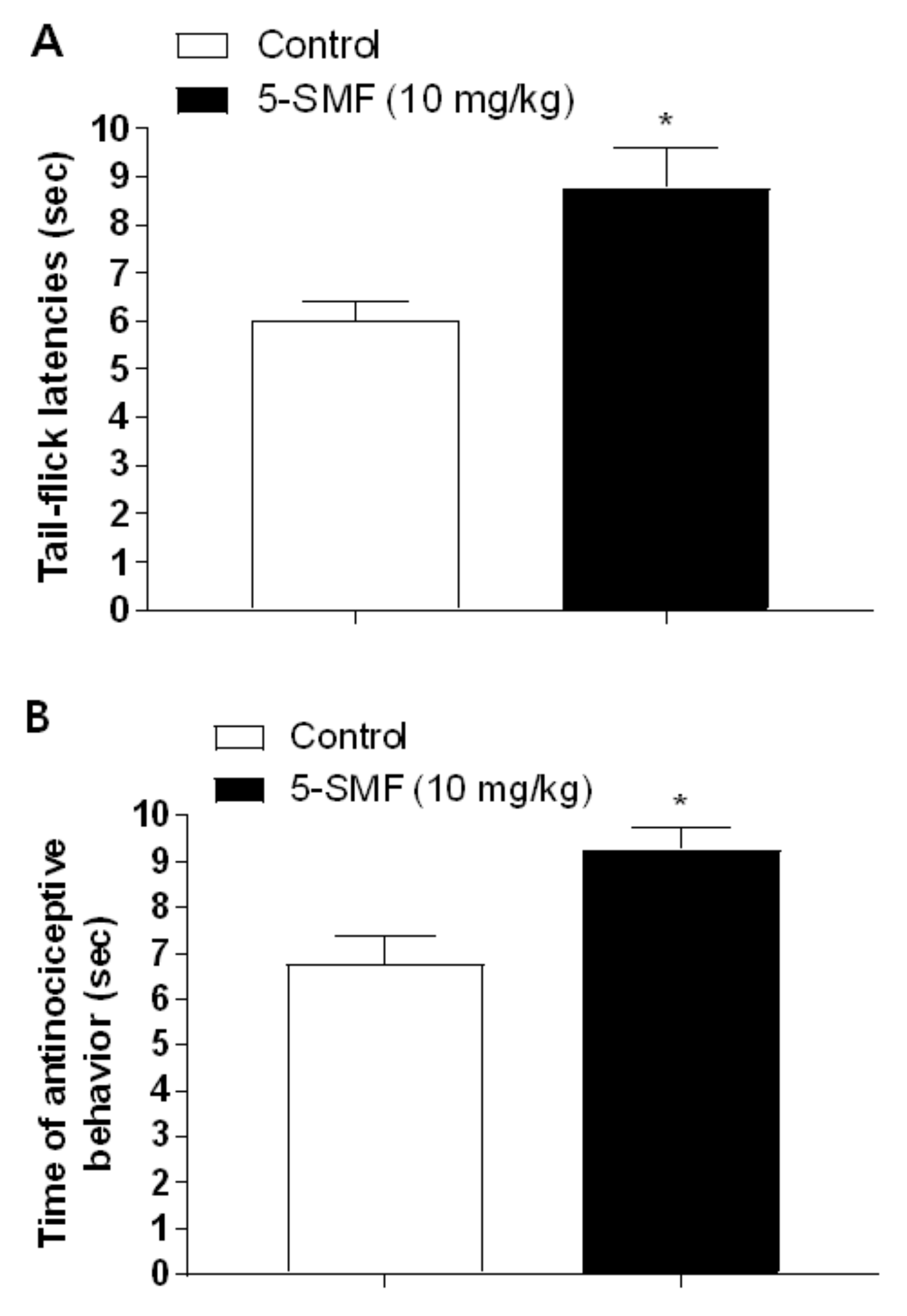
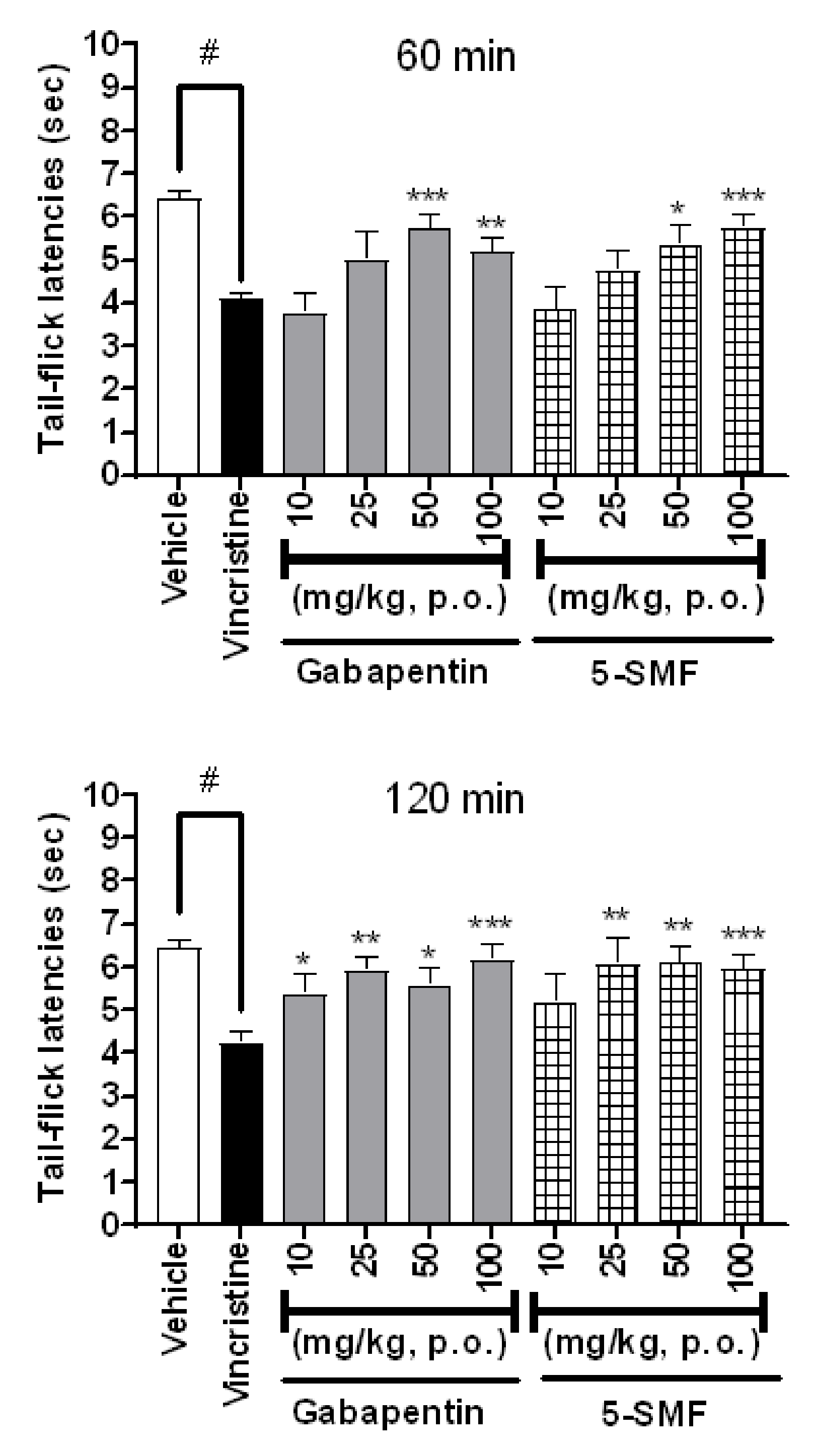
2.12. Antinociceptive Effect of 5-SMF and Gabapentin in the Tail-Flick Test in Vincristine-Induced Pain Model
3. Discussion
4. Materials and Methods
4.1. Chemicals and Reagents
4.2. Plant Materials
4.3. Preparation of Extraction and Isolation
4.4. Chemistry
4.4.1. Synthesis of 5-Acetoxy Methyl Furfural (5-AMF) (1)
4.4.2. Synthesis of 5-Propionoxy Methyl Furfural (5-PMF) (2)
4.4.3. Synthesis of 5-Butyroxy Methyl Furfural (5-BMF) (3)
4.4.4. Synthesis of 5-Succinoxy Methyl Furfural (5-SMF) (4)
4.4.5. Synthesis of 5-Glutaroxy Methyl Furfural (5-GMF) (5)
4.4.6. Synthesis of 5-Cinnamoxy Methyl Furfural (5-CMF) (6)
4.4.7. Synthesis of 5-Lauroxy Methyl Furfural (5-LMF) (7)
4.5. Animals
4.6. In Vivo Studies
4.6.1. Induction of Neuropathic Pain Model
Chronic Constriction Injury (CCI) Neuropathic Pain Model
Spared Nerve Injury (SNI) Neuropathic Pain Model
Vincristine Induced Neuropathic Pain Model
4.6.2. Writhing Test
4.6.3. Formalin (5%) Test
4.6.4. Tail-Flick Test
4.7. Von Frey Filament Tests
4.8. Bacterial Reverse Mutation (Ames) Test
4.9. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Rasul, A.; Millimouno, F.M.; Ali Eltayb, W.; Ali, M.; Li, J.; Li, X. Pinocembrin: A novel natural compound with versatile pharmacological and biological activities. BioMed. Res. Int. 2013, 2013, 379850. [Google Scholar] [CrossRef]
- Harvey, A.L. Natural products in drug discovery. Drug Discov. Today 2008, 13, 894–901. [Google Scholar] [CrossRef]
- Adami, C.; Spadavecchia, C. Use of nociceptive threshold testing in cats in experimental and clinical settings: A qualitative review. Vet. Anaesth. Analg. 2020, 47, 419–436. [Google Scholar] [CrossRef] [PubMed]
- Falk, S.; Dickenson, A.H. Pain and nociception: Mechanisms of cancer-induced bone pain. J. Clin. Oncol. 2014, 32, 1647–1654. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.N.; Meyer, R.A. Mechanisms of neuropathic pain. Neuron 2006, 52, 77–92. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M. Pathobiology of neuropathic pain. Eur. J. Pharmacol. 2001, 429, 23–37. [Google Scholar] [CrossRef]
- Comelli, F.; Giagnoni, G.; Bettoni, I.; Colleoni, M.; Costa, B. Antihyperalgesic effect of a Cannabis sativa extract in a rat model of neuropathic pain: Mechanisms involved. Phytother. Res. 2008, 22, 1017–1024. [Google Scholar] [CrossRef] [PubMed]
- Rahbardar, M.G.; Amin, B.; Mehri, S.; Mirnajafi-Zadeh, S.J.; Hosseinzadeh, H. Anti-inflammatory effects of ethanolic extract of Rosmarinus officinalis L. and rosmarinic acid in a rat model of neuropathic pain. Biomed. Pharmacother. 2017, 86, 441–449. [Google Scholar] [CrossRef]
- Kaeidi, A.; Esmaeili-Mahani, S.; Sheibani, V.; Abbasnejad, M.; Rasoulian, B.; Hajializadeh, Z.; Afrazi, S. Olive (Olea europaea L.) leaf extract attenuates early diabetic neuropathic pain through prevention of high glucose-induced apoptosis: In vitro and in vivo studies. J. Ethnopharmacol. 2011, 136, 188–196. [Google Scholar] [CrossRef]
- Jean, Y.H.; Chen, W.F.; Sung, C.S.; Duh, C.Y.; Huang, S.Y.; Lin, C.S.; Tai, M.H.; Tzeng, S.F.; Wen, Z.H. Capnellene, a natural marine compound derived from soft coral, attenuates chronic constriction injury induced neuropathic pain in rats. Br. J. Pharmacol. 2009, 158, 713–725. [Google Scholar] [CrossRef] [PubMed]
- Lim, E.Y.; Kim, Y.T. Food-derived natural compounds for pain relief in neuropathic pain. BioMed Res. Int. 2016, 2016, 7917528. [Google Scholar] [CrossRef]
- Sunil, C.; Ignacimuthu, S.; Kumarappan, C. Hypolipidemic activity of Symplocos cochinchinensis S. Moore leaves in hyperlipidemic rats. J. Nat. Med. 2012, 66, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Na, M.K.; Yang, S.; He, L.; Oh, H.; Kim, B.S.; Oh, W.K.; Kim, B.Y.; Ahn, J.S. Inhibition of protein tyrosine phosphatase 1B by ursane-type triterpenes isolated from Symplocos paniculata. Planta Med. 2006, 72, 261–263. [Google Scholar] [CrossRef]
- Huo, C.H.; Shen, L.R.; Zhao, Y.Y.; Liang, H. Chemical constituents of plants from the genus Symplocos. Chem. Biodivers. 2007, 4, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Li, X.-H.; Shen, D.-D.; Li, N.; Yu, S.-S. Bioactive triterpenoids from Symplocos chinensis. J. Asian Nat. Prod. Res. 2003, 5, 49–56. [Google Scholar] [CrossRef]
- Li, B.; Abliz, Z.; Fu, G.; Tang, M.; Yu, S. Characteristic fragmentation behavior of some glucuronide-type triterpenoid saponins using electrospray ionization tandem mass spectrometry. Rapid Commun. Mass Spectrom. 2005, 19, 381–390. [Google Scholar] [CrossRef]
- Schuller, Y.; Linthorst, G.; Hollak, C.; Van Schaik, I.; Biegstraaten, M. Pain management strategies for neuropathic pain in Fabry disease-a systematic review. BMC Neurol. 2016, 16, 25. [Google Scholar] [CrossRef]
- Wang, Y.; Brown, C.A.; Chen, R. Industrial production, application, microbial biosynthesis and degradation of furanic compound, hydroxymethylfurfural (HMF). AIMS Microbiol. 2018, 4, 261–273. [Google Scholar] [CrossRef] [PubMed]
- Velali, E.; Pantazaki, A.; Besis, A.; Choli-Papadopoulou, T.; Samara, C. Oxidative stress, DNA damage, and mutagenicity induced by the extractable organic matter of airborne particulates on bacterial models. Regul. Toxicol. Pharmacol. 2019, 104, 59–73. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, P.; Tang, C.; Li, Y.; Zhang, H. Antinociceptive and anti-inflammatory activities of extract and two isolated flavonoids of Carthamus tinctorius L. J. Ethnopharmacol. 2014, 151, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Tjølsen, A.; Berge, O.-G.; Hunskaar, S.; Rosland, J.H.; Hole, K. The formalin test: An evaluation of the method. Pain 1992, 51, 5–17. [Google Scholar] [CrossRef]
- Shields, S.D.; Eckert III, W.A.; Basbaum, A.I. Spared nerve injury model of neuropathic pain in the mouse: A behavioral and anatomic analysis. J. Pain 2003, 4, 465–470. [Google Scholar] [CrossRef]
- Bourquin, A.F.; Süveges, M.; Pertin, M.; Gilliard, N.; Sardy, S.; Davison, A.C.; Spahn, D.R.; Decosterd, I. Assessment and analysis of mechanical allodynia-like behavior induced by spared nerve injury (SNI) in the mouse. Pain 2006, 122, e11–e14. [Google Scholar] [CrossRef]
- De Vry, J.; Kuhl, E.; Franken-Kunkel, P.; Eckel, G. Pharmacological characterization of the chronic constriction injury model of neuropathic pain. Eur. J. Pharmacol. 2004, 491, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Karna, S.R.; Kongara, K.; Singh, P.M.; Chambers, P.; Lopez-Villalobos, N. Evaluation of analgesic interaction between morphine, dexmedetomidine and maropitant using hot-plate and tail-flick tests in rats. Vet. Anaesth. Analg. 2019, 46, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Lima Cavendish, R.; de Souza Santos, J.; Belo Neto, R.; Oliveira Paixao, A.; Valeria Oliveira, J.; Divino de Araujo, E.; Berretta, E.S.A.A.; Maria Thomazzi, S.; Cordeiro Cardoso, J.; Zanardo Gomes, M. Antinociceptive and anti-inflammatory effects of Brazilian red propolis extract and formononetin in rodents. J. Ethnopharmacol. 2015, 173, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Xu, Y. Suppressing BRD4 exhibits protective effects against vincristine-induced peripheral neuropathy by alleviating inflammation and oxidative stress. Biochem. Biophys. Res. Commun. 2020, 532, 271–279. [Google Scholar] [CrossRef]
- Bennett, G.J.; Xie, Y.K. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain 1988, 33, 87–107. [Google Scholar] [CrossRef]
- Saika, F.; Kiguchi, N.; Kobayashi, Y.; Fukazawa, Y.; Maeda, T.; Ozaki, M.; Kishioka, S. Suppressive effect of imipramine on vincristine-induced mechanical allodynia in mice. Biol. Pharm. Bull. 2009, 32, 1231–1234. [Google Scholar] [CrossRef] [PubMed]
- Koster, R.; Anderson, M.; De Beer, E.J. Acetic acid for analgesic screening. Fed. Proc. 1959, 18, 412–417. [Google Scholar]
- Hunskaar, S.; Fasmer, O.B.; Hole, K. Formalin test in mice, a useful technique for evaluating mild analgesics. J. Neurosci. Methods 1985, 14, 69–76. [Google Scholar] [CrossRef]
- Hunskaar, S.; Hole, K. The formalin test in mice: Dissociation between inflammatory and non-inflammatory pain. Pain 1987, 30, 103–114. [Google Scholar] [CrossRef]
- D’Amour, F.E.; Smith, D.L. A method for determining loss of pain sensation. J. Pharmacol. Exp. Ther. 1941, 72, 74–79. [Google Scholar]
- Chaplan, S.R.; Bach, F.; Pogrel, J.; Chung, J.; Yaksh, T. Quantitative assessment of tactile allodynia in the rat paw. J. Neurosci. Methods 1994, 53, 55–63. [Google Scholar] [CrossRef]
- Bonin, R.P.; Bories, C.; De Koninck, Y. A simplified up-down method (SUDO) for measuring mechanical nociception in rodents using von Frey filaments. Mol. Pain 2014, 10, 26. [Google Scholar] [CrossRef]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.-Y.; Park, S.-H.; Zuo, G.; Kim, K.H.; Hwang, S.H.; Suh, H.-W.; Lim, S.-S. Effect of Extract and Synthesized Derivatives of Isolated Compound from Symplocos chinensis f. Pilosa Ohwi on Neuropathic Pain in Mice. Molecules 2021, 26, 1639. https://doi.org/10.3390/molecules26061639
Kim H-Y, Park S-H, Zuo G, Kim KH, Hwang SH, Suh H-W, Lim S-S. Effect of Extract and Synthesized Derivatives of Isolated Compound from Symplocos chinensis f. Pilosa Ohwi on Neuropathic Pain in Mice. Molecules. 2021; 26(6):1639. https://doi.org/10.3390/molecules26061639
Chicago/Turabian StyleKim, Hyun-Yong, Soo-Hyun Park, Guanglei Zuo, Kang Hyuk Kim, Seung Hwan Hwang, Hong-Won Suh, and Soon-Sung Lim. 2021. "Effect of Extract and Synthesized Derivatives of Isolated Compound from Symplocos chinensis f. Pilosa Ohwi on Neuropathic Pain in Mice" Molecules 26, no. 6: 1639. https://doi.org/10.3390/molecules26061639
APA StyleKim, H.-Y., Park, S.-H., Zuo, G., Kim, K. H., Hwang, S. H., Suh, H.-W., & Lim, S.-S. (2021). Effect of Extract and Synthesized Derivatives of Isolated Compound from Symplocos chinensis f. Pilosa Ohwi on Neuropathic Pain in Mice. Molecules, 26(6), 1639. https://doi.org/10.3390/molecules26061639







