Tri- and Pentacyclic Azaphenothiazine as Pro-Apoptotic Agents in Lung Carcinoma with a Protective Potential to Healthy Cell Lines
Abstract
:1. Introduction
2. Results and Discussion
2.1. Anticancer Activity
2.2. Cytostatic Potential of Modified Phenothiazines
2.3. Pro-Apoptotic and Pro-Necrotic Role of Phenothazines

2.4. Microscopic Long-Term Live Observations
2.5. ADME Analysis and Target Prediction of DPT-1 and DPT-2
3. Materials and Methods
3.1. Chemicals
3.2. Cell Culturing
3.3. MTT Viability Assay
3.4. Cell Cycle Analysis and Apoptosis/Necrosis Analysis via Flow Cytometry Using Annexin-V Assay
3.5. Microscopic Observation
3.6. Statistical Analyses
3.7. ADME Analysis and Target Prediction
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Bade, B.C.; Dela Cruz, C.S. Lung Cancer 2020 Epidemiology, Etiology, and Prevention. Clin. Chest Med. 2020, 41, 1–24. [Google Scholar] [CrossRef]
- Nasim, F.; Sabath, B.F.; George, A. Lung Cancer. Med. Clin. N. Am. 2019, 103, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Cordero, R.; Devine, W.P. Targeted Therapy and Checkpoint Immunotherapy in Lung Cancer. Surg. Pathol. 2020, 13, 17–33. [Google Scholar] [CrossRef] [PubMed]
- Schabath, M.B.; Cote, M.L. Cancer Progress and Priorities: Lung Cancer. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1563–1579. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Dela Cruz, C.S.; Tanoue, L.T.; Matthay, R.A. Lung cancer: Epidemiology, etiology, and prevention. Clin. Chest Med. 2011, 32, 605–644. [Google Scholar] [CrossRef]
- de Groot, P.M.; Wu, C.C.; Carter, B.W.; Munden, R.F. The epidemiology of lung cancer. Transl. Lung Cancer Res. 2018, 7, 220–233. [Google Scholar] [CrossRef]
- Li, Y.; Jiang, Y.; Yi, Y.; Liu, W.; Tang, Y.; Liu, Y.; Liu, Y. Application of auricular acupoints therapy in relieving the gastrointestinal side effects induced by chemotherapy: An integrative review. Chin. Nurs. Res. 2016, 3, 58–61. [Google Scholar] [CrossRef]
- Junmin, Z.; Dongzhu, D.; ZiLong, S.; Tianyu, L.; Yanan, H.; Jianguo, F. Small molecules regulating reactive oxygenspecies homeostasis for cancer therapy. Med. Res. Rev. 2021, 41, 342–394. [Google Scholar] [CrossRef]
- Mosnaim, A.D.; Ranade, V.V.; Wolf, M.E.; Puente, J.; Valenzuela, M.A. Phenothiazine molecule provides the basic chemical structure for various classes of pharmacotherapeutic agents. Am. J. Ther. 2006, 13, 261–273. [Google Scholar] [CrossRef]
- Huang, J.; Zhao, D.; Liu, Z.; Liu, F. Repurposing psychiatric drugs as anti-cancer agents. Cancer Lett. 2018, 419, 257–265. [Google Scholar] [CrossRef]
- Pluta, K.; Jeleń, M.; Morak-Młodawska, B. The Smiles rearrangement in the syntheses of azaphenothiazines. Part I. J. Mol. Struct. 2020, 1204, 127501. [Google Scholar] [CrossRef]
- Pluta, K.; Morak-Młodawska, B.; Jeleń, M. The Smiles rearrangement in the syntheses of azaphenothiazines. Part II. The review of the various types of phenyl azinyl and diazinyl sulfides undergoing this rearrangement. J. Mol. Struct. 2020, 1216, 128320. [Google Scholar] [CrossRef]
- Dasgupta, A.; Dastridara, S.G.; Shirataki, Y.; Motohashi, N. Antibacterial activity of artificial phenothiazines and isoflavones from plants. In Bioactive Heterocycles VI; Topics in Heterocyclic Chemistry Series; Springer: Berlin/Heidelberg, Germany, 2008; Volume 15, pp. 67–132. [Google Scholar]
- Pluta, K.; Morak-Młodawska, B.; Jeleń, M. Recent progress in biological activities of synthesized phenothiazines. Eur. J. Med. Chem. 2011, 46, 3179–3189. [Google Scholar] [CrossRef]
- Varga, B.; Csonka, Á.; Csonka, A.; Molnár, J.; Amaral, L.; Spengler, G. Possible biological and clinical applications of phenothiazines. Anticancer Res. 2017, 37, 5983–5993. [Google Scholar] [CrossRef]
- Morak-Młodawska, B.; Jeleń, M.; Pluta, K. Phenothiazines modified with the pyridine ring as promising anticancer agents. Life 2021, 11, 206. [Google Scholar] [CrossRef]
- Maciążek-Jurczyk, M.; Morak-Młodawska, B.; Jeleń, M.; Kopeć, W.; Szkudlarek, A.; Owczarzy, A.; Kulig, K.; Rogóż, W.; Pożycka, J. The influence of oxidative stress on serum albumin structure as a carrier of selected diazaphenothiazine with potential anticancer activity. Pharmaceuticals 2021, 14, 285. [Google Scholar] [CrossRef]
- Sochacka, J.; Pacholczyk, M.; Jeleń, M.; Morak-Młodawska, B.; Pluta, K. Interaction of new tri-, tetra-, and pentacyclic azaphenothiazine derivatives with calf thymus DNA: Spectroscopic and molecular docking studies. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2021, 262, 120105. [Google Scholar] [CrossRef]
- Morak-Młodawska, B.; Pluta, K.; Latocha, M.; Suwińska, K.; Jeleń, M.; Kuśmierz, D. 3,6-Diazaphenothiazines as potential lead molecules—Synthesis, characterization and anticancer activity. J. Enzym. Inhib. Med. Chem. 2016, 31, 1512–1519. [Google Scholar] [CrossRef]
- Jeleń, M.; Pluta, K.; Latocha, M.; Morak-Młodawska, B.; Suwińska, K.; Kuśmierz, D. Evaluation of angularly condensed diquinothiazines as potential anticancer agents. Bioorg. Chem. 2019, 87, 810–820. [Google Scholar] [CrossRef]
- Zhang, J.; Chen, M.; Wenzhi, Z.; Okechukwu, P.N.; Morak-Młodawska, B.; Pluta, K.; Jeleń, M.; Akim, A.M.; Ang, K.-P.; Ooi, K.K. 10H-3,6-Diazaphenothiazines Induce G2/M Phase Cell Cycle Arrest, Caspase-dependent Apoptosis and Inhibits Cell Invasion of A2780 Ovarian Carcinoma Cells through Regulation on NF-κB and [BIRC6-XIAP] Complexes. Drug Des. Dev. Ther. 2017, 11, 3045–3063. [Google Scholar] [CrossRef]
- Mielanczyk, A.; Mrowiec, K.; Kupczak, M.; Mielanczyk, Ł.; Scieglinska, D.; Gogler-Piglowska, A.; Michalski, M.; Gabriel, A.; Neugebauer, D.; Skonieczna, M. Synthesis and in vitro cytotoxicity evaluation of star-shaped polymethacrylic conjugates with methotrexate or acitretin as potential antipsoriatic prodrugs. Eur. J. Pharmacol. 2020, 866, 172804. [Google Scholar] [CrossRef] [PubMed]
- Nackiewicz, J.; Kliber-Jasik, M.; Skonieczna, M. A novel pro-apoptotic role of zinc octacarboxyphthalocyanine in melanoma Me45 cancer cell’s photodynamic therapy (PDT). J. Photochem. Photobiol. B Biol. 2019, 190, 146–153. [Google Scholar] [CrossRef]
- Skonieczna, M.; Hudy, D.; Poterala-Hejmo, A.; Hejmo, T.; Buldak, R.J.; Dziedzic, A. Effects of Resveratrol, Berberine, and Their Combinations on Reactive Oxygen Species, Survival, and Apoptosis in Human Squamous Carcinoma (SCC-25) Cells. Anticancer Agents Med. Chem. 2019, 19, 1161–1171. [Google Scholar] [CrossRef]
- Skonieczna, M.; Hudy, D.; Hejmo, T.; Buldak, R.J.; Adamiec, M.; Kukla, M. The adipokine vaspin reduces apoptosis in human hepatocellular carcinoma (Hep-3B) cells, associated with lower levels of NO and superoxide anion. BMC Pharmacol. Toxicol. 2019, 20, 58. [Google Scholar] [CrossRef] [PubMed]
- Krawczyk, M.; Pastuch-Gawołek, G.; Mrozek-Wilczkiewicz, A.; Kuczak, M.; Skonieczna, M.; Musioł, R. Synthesis of 8-hydroxyquinoline glycoconjugates and preliminary assay of their β1,4-GalT inhibitory and anti-cancer properties. Bioorg. Chem. 2019, 84, 326–338. [Google Scholar] [CrossRef] [PubMed]
- Bielas, R.; Siewniak, A.; Skonieczna, M.; Adamiec, M.; Mielańczyk, Ł.; Neugebauer, D. Choline based polymethacrylate matrix with pharmaceutical cations as co-delivery system for antibacterial and anti-inflammatory combined therapy. J. Mol. Liq. 2019, 285, 114–122. [Google Scholar] [CrossRef]
- Altmann, S.; Choroba, K.; Skonieczna, M.; Zygadło, D.; Raczyńska-Szajgin, M.; Maroń, A.; Małecki, J.G.; Szłapa-Kula, A.; Tomczyk, M.; Ratuszna, A.; et al. Platinum(II) coordination compounds with 4′-pyridyl functionalized 2,2′: 6′, mort 2″-terpyridines as an alternative to enhanced chemotherapy efficacy and reduced side-effects. J. Inorg. Biochem. 2019, 201, 110809. [Google Scholar] [CrossRef]
- Skonieczna, M.; Adamiec, M.; Hudy, D.; Nieslon, P.; Fochtman, D.; Bil, P. Live Impedance Measurements and Time-lapse Microscopy Observations of Cellular Adhesion, Proliferation and Migration after Ionizing Radiation. Curr. Pharm. Biotechnol. 2020, 21, 642–652. [Google Scholar] [CrossRef]
- Skonieczna, M.; Hudy, D.; Bil, P.; Adamiec, M.; Stachowska, M.; Biernacki, K. Role of Let-7 Family miRNAs in Migration of Colorectal Cancer HCT 116 and Caco-2 Cells After Stimulation by the Adipokine Vaspin. Time-Lapse Live-Cell Microscopic Observations. In Current Trends in Biomedical Engineering and Bioimages Analysis; Korbicz, J., Maniewski, R., Patan, K., Kowal, M., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 47–61. [Google Scholar] [CrossRef]
- SwissADME. Available online: http://www.swissadme.ch/index.php (accessed on 14 June 2022).
- Way2drug. Available online: http://way2drug.com (accessed on 14 June 2022).

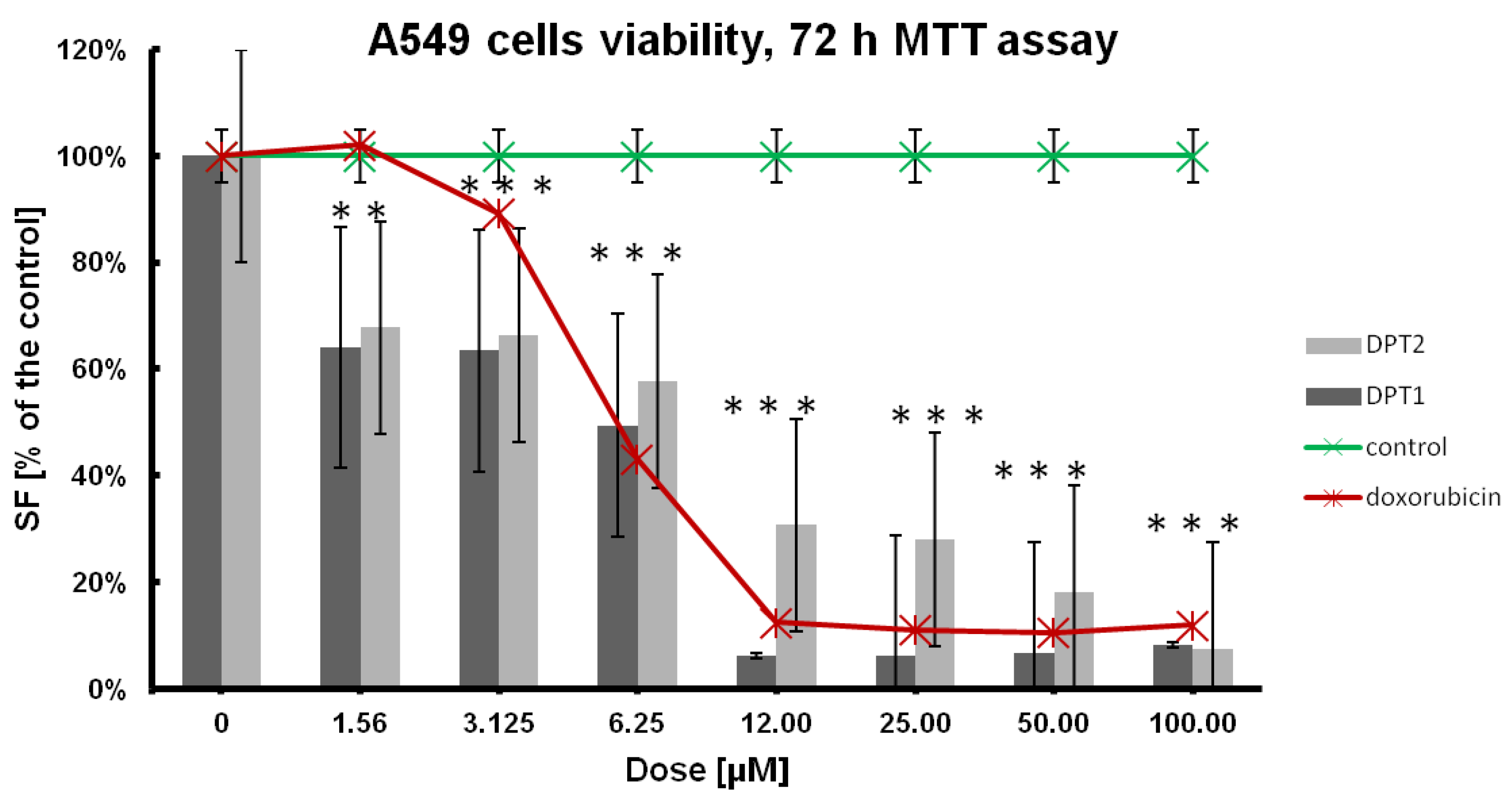







| IC50 [µM] | Cell Line | |||
|---|---|---|---|---|
| NHDF | BEAS-2B | A549 | H1299 | |
| DPT-1 | 2.246 ± 0.01 | 2.4679 ± 0.01 | 1.526 ± 0.004 | 2.515 ± 0.005 |
| DPT-2 | 18.77 ± 0.038 | 11.2648 ± 0.038 | 3.447 ± 0.054 | 12.895 ± 0.013 |
| doxorubicin | 116.061 ± 0.002 | 0.0651 ± 0.001 | 5.289 ± 0.004 | 7.749 ± 0.004 |
| No | Molecular Mass (M) | H-bond Acceptors | H-bond Donors | Rotatable Bonds | TPSA | Lipinski’s Rules | Ghose’s Rules | Veber’s Rules |
|---|---|---|---|---|---|---|---|---|
| DPT-1 | 201 | 2 | 1 | 0 | 63 | + | + | + |
| DPT-2 | 386 | 3 | 0 | 4 | 57 | + | + | + |
| No | LogPcalc. | GI Absorption | BBB Permeant | Pgp Substrate | CYP1A2 Inhibitor | CYP2C9 Inhibitor | CYP2D6 Inhibitor |
|---|---|---|---|---|---|---|---|
| DPT-1 | 1.78 | high | + | + | + | + | + |
| DPT-2 | 4.45 | high | + | + | + | + | + |
| DPT-1 Probability of Activity | DPT-2 Probability of Activity |
|---|---|
| Histone deacetylase SIRT1 stimulant Histone deacetylase stimulant Angiogenesis factor | X-methyl-His dipeptidase inhibitor Tumor necrosis factor alpha release inhibitor Immunomodulator |
| Anti-inflammatory | Angiogenesis factor |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skonieczna, M.; Kasprzycka, A.; Jeleń, M.; Morak-Młodawska, B. Tri- and Pentacyclic Azaphenothiazine as Pro-Apoptotic Agents in Lung Carcinoma with a Protective Potential to Healthy Cell Lines. Molecules 2022, 27, 5255. https://doi.org/10.3390/molecules27165255
Skonieczna M, Kasprzycka A, Jeleń M, Morak-Młodawska B. Tri- and Pentacyclic Azaphenothiazine as Pro-Apoptotic Agents in Lung Carcinoma with a Protective Potential to Healthy Cell Lines. Molecules. 2022; 27(16):5255. https://doi.org/10.3390/molecules27165255
Chicago/Turabian StyleSkonieczna, Magdalena, Anna Kasprzycka, Małgorzata Jeleń, and Beata Morak-Młodawska. 2022. "Tri- and Pentacyclic Azaphenothiazine as Pro-Apoptotic Agents in Lung Carcinoma with a Protective Potential to Healthy Cell Lines" Molecules 27, no. 16: 5255. https://doi.org/10.3390/molecules27165255








