Natural Reno-Protective Agents against Cyclosporine A-Induced Nephrotoxicity: An Overview
Abstract
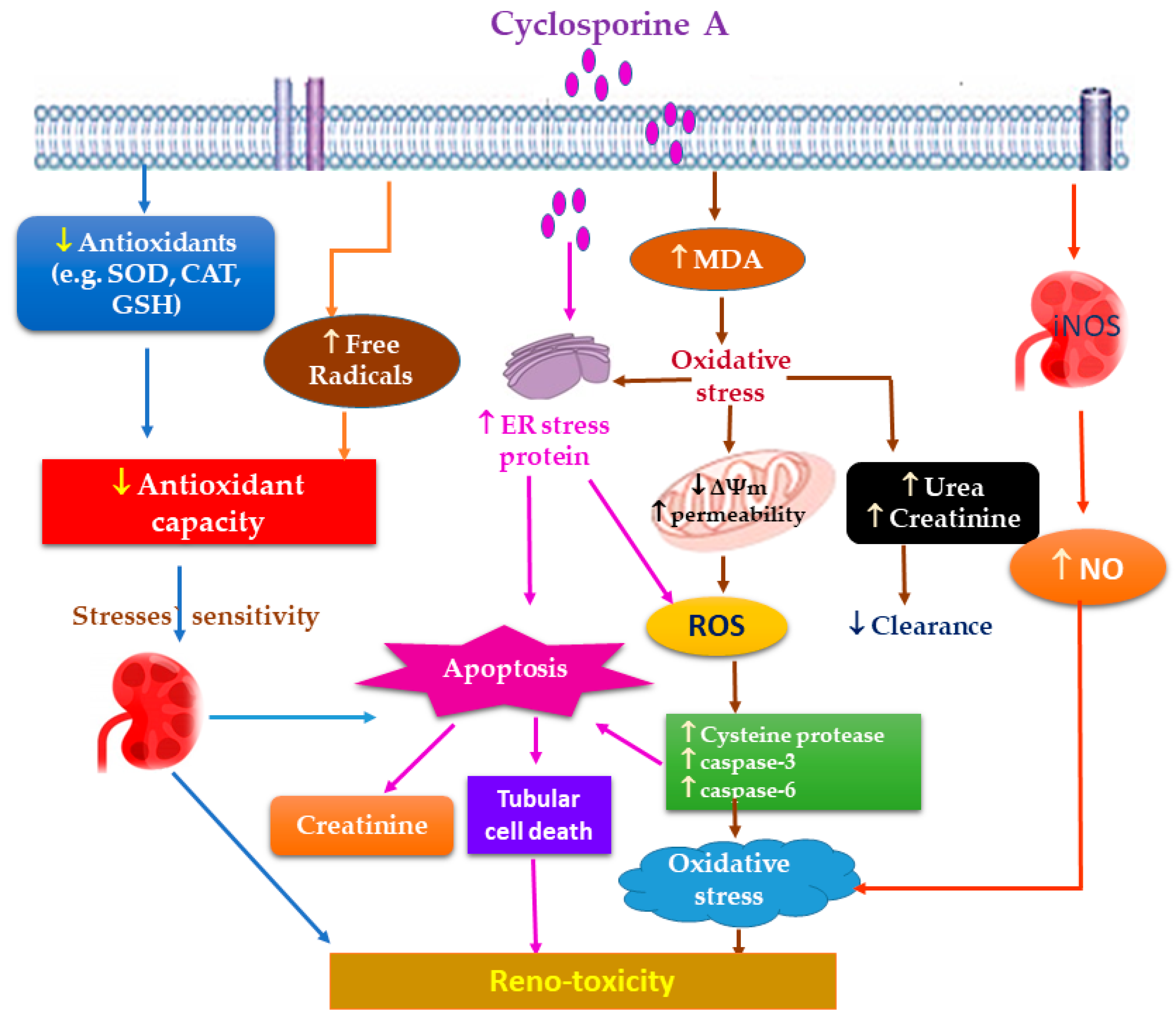
:1. Introduction
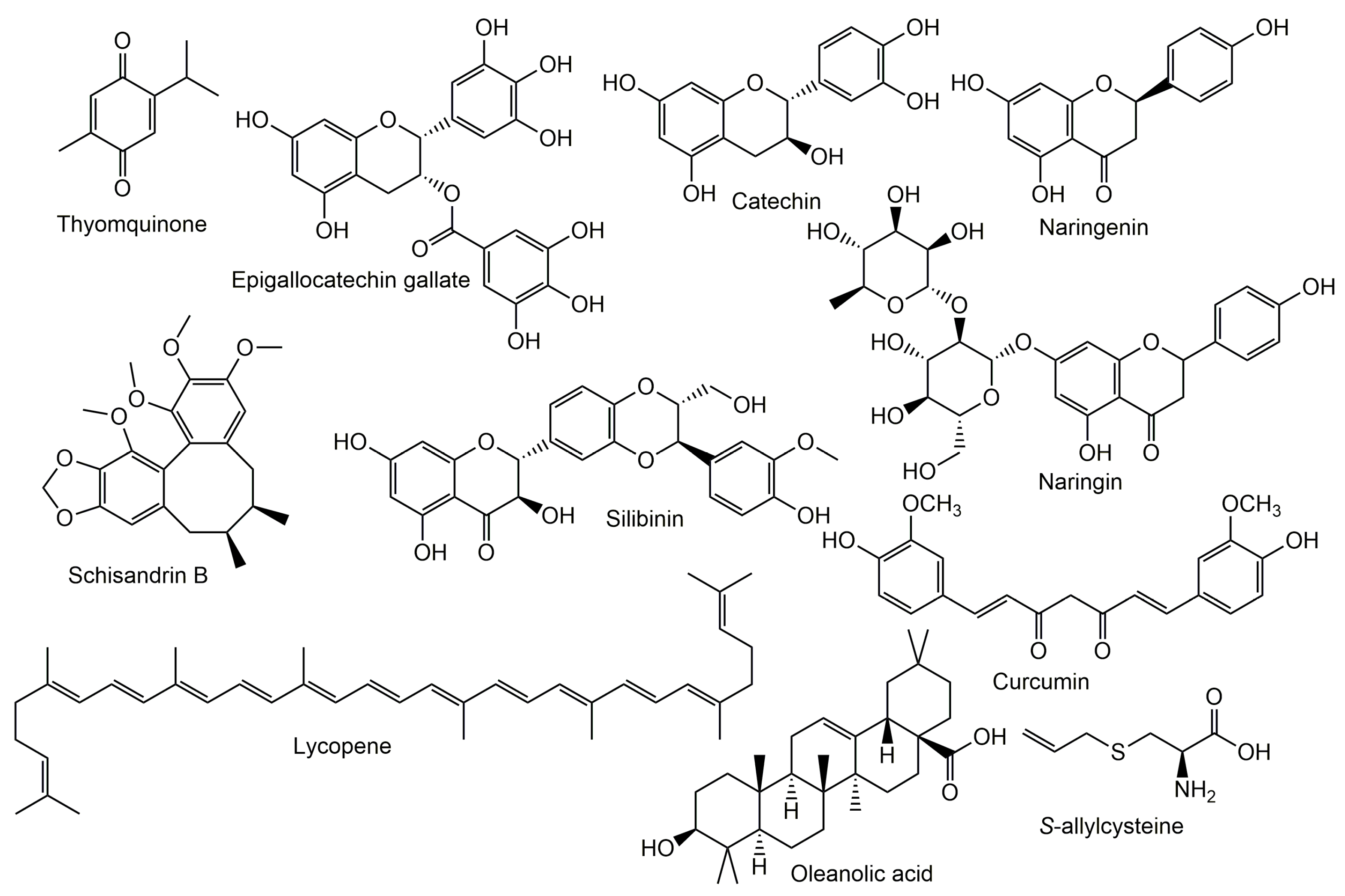
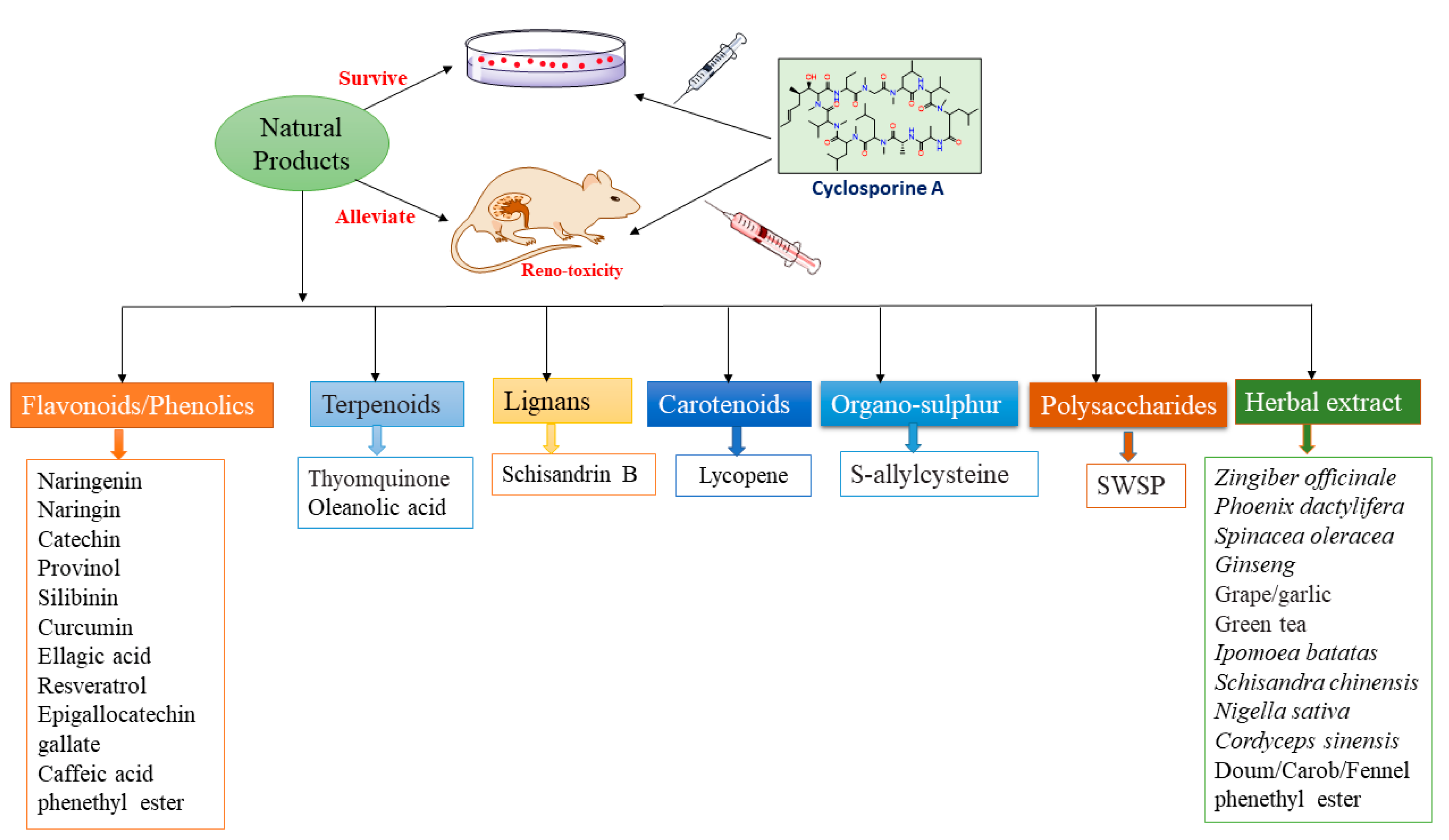
2. Phytoconstituents Prevent CA-Induced Nephrotoxicity
2.1. Phenolics and Polyphenols
2.1.1. Catechin
2.1.2. Epigallocatechin Gallate (EGCG)
2.1.3. Naringin
2.1.4. Silibinin
2.1.5. Ellagic Acid
2.1.6. Caffeic Acid Phenethyl Ester
2.1.7. Resveratrol
2.1.8. Provinol
2.1.9. Curcumin
2.2. Lignan Derivatives
2.3. Carotenoids
2.4. Organo-Sulfur Derivatives
2.5. Terpenoids
2.6. Polysaccharides
3. Herbal Extracts Prevent CA-Induced Nephrotoxicity
3.1. Zingiber officinale
3.2. Phoenix dactylifera
3.3. Spinacea oleracea
3.4. Ginseng
3.5. Grape and Garlic
3.6. Green Tea
3.7. Ipomoea batatas
3.8. Schisandra chinensis
3.9. Nigella sativa
3.10. Cordyceps sinensis
3.11. Doum, Carob, and Fennel
4. Miscellaneous Natural Products
4.1. Propolis
4.2. Spirulina
5. Diet Prevents CA-Induced Nephrotoxicity
6. Natural Products’ Stability and Adverse Effects
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Jivishov, E.; Nahar, L.; Sarker, S.D. Nephroprotective natural products. In Annual Reports in Medicinal Chemistry; Elsevier: Amsterdam, The Netherlands, 2020; Volume 55, pp. 251–271. [Google Scholar]
- Touiti, N.; Houssaini, T.S.; Achour, S. Overview on pharmacovigilance of nephrotoxic herbal medicines used worldwide. Clin. Phytoscience 2021, 7, 1–8. [Google Scholar] [CrossRef]
- Kolangi, F.; Memariani, Z.; Bozorgi, M.; Mozaffarpur, S.A.; Mirzapour, M. Herbs with potential nephrotoxic effects according to the traditional Persian medicine: Review and assessment of scientific evidence. Curr. Drug Metab. 2018, 19, 628–637. [Google Scholar] [CrossRef]
- Wu, H.; Huang, J. Drug-induced nephrotoxicity: Pathogenic mechanisms, biomarkers and prevention strategies. Curr. Drug Metab. 2018, 19, 559–567. [Google Scholar] [CrossRef]
- Faria, J.; Ahmed, S.; Gerritsen, K.G.; Mihaila, S.M.; Masereeuw, R. Kidney-based in vitro models for drug-induced toxicity testing. Arch. Toxicol. 2019, 93, 3397–3418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.Y.; Moon, A. Drug-induced nephrotoxicity and its biomarkers. Biomol. Ther. 2012, 20, 268–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mostafavi-Pour, Z.; Khademi, F.; Zal, F.; Sardarian, A.R.; Amini, F. In vitro analysis of CsA-induced hepatotoxicity in HepG2 cell line: Oxidative stress and α2 and β1 integrin subunits expression. Hepat. Mon. 2013, 13, e11447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ciresi, D.L.; Lloyd, M.A.; Sandberg, S.M.; Heublein, D.M.; Edwards, B.S. The sodium retaining effects of cyclosporine. Kidney Int. 1992, 41, 1599–1605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colombo, D.; Lunardon, L.; Bellia, G. Cyclosporine and herbal supplement interactions. J. Toxicol. 2014, 2014, 145325. [Google Scholar] [CrossRef]
- Colombo, M.D.; Perego, R.; Bellia, G. Drug interaction and potential side effects of cyclosporine. Adv. Exp. Med. Biol. 2013, 74, 1–24. [Google Scholar]
- Wu, Q.; Wang, X.; Nepovimova, E.; Wang, Y.; Yang, H.; Kuca, K. Mechanism of cyclosporine A nephrotoxicity: Oxidative stress, autophagy, and signalings. Food Chem. Toxicol. 2018, 118, 889–907. [Google Scholar] [CrossRef]
- Tedesco, D.; Haragsim, L. Cyclosporine: A Review. J. Transplant. 2012, 2012, 230386. [Google Scholar] [CrossRef] [PubMed]
- Lai, Q.; Luo, Z.; Wu, C.; Lai, S.; Wei, H.; Li, T.; Wang, Q.; Yu, Y. Attenuation of cyclosporine A induced nephrotoxicity by schisandrin B through suppression of oxidative stress, apoptosis and autophagy. Int. Immunopharmacol. 2017, 52, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Damiano, S.; Ciarcia, R.; Montagnaro, S.; Pagnini, U.; Garofano, T.; Capasso, G.; Florio, S.; Giordano, A. Prevention of nephrotoxicity induced by cyclosporine-A: Role of antioxidants. J. Cell. Biochem. 2015, 116, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Ciarcia, R.; Damiano, S.; Florio, A.; Spagnuolo, M.; Zacchia, E.; Squillacioti, C.; Mirabella, N.; Florio, S.; Pagnini, U.; Garofano, T. The protective effect of apocynin on cyclosporine A-induced hypertension and nephrotoxicity in rats. J. Cell. Biochem. 2015, 116, 1848–1856. [Google Scholar] [CrossRef] [PubMed]
- Hamon, J.; Jennings, P.; Bois, F.Y. Systems biology modeling of omics data: Effect of cyclosporine a on the Nrf2 pathway in human renal cells. BMC Syst. Biol. 2014, 8, 76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Q.-f.; Ye, J.-m.; Yu, L.-x.; Dong, X.-h.; Feng, J.-h.; Xiong, Y.; Gu, X.-x.; Li, S.-s. Klotho mitigates cyclosporine A (CsA)-induced epithelial–mesenchymal transition (EMT) and renal fibrosis in rats. Int. Urol. Nephrol. 2017, 49, 345–352. [Google Scholar] [CrossRef]
- McMorrow, T.; Gaffney, M.M.; Slattery, C.; Campbell, E.; Ryan, M.P. Cyclosporine A induced epithelial–mesenchymal transition in human renal proximal tubular epithelial cells. Nephrol. Dial. Transplant. 2005, 20, 2215–2225. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.S.; Choi, S.-I.; Jeung, E.-B.; Yoo, Y.-M. Cyclosporine A induces apoptotic and autophagic cell death in rat pituitary GH3 cells. PLoS ONE 2014, 9, e108981. [Google Scholar] [CrossRef]
- Shi, S.-H.; Zheng, S.-S.; Jia, C.-K.; Zhu, Y.-F.; Xie, H.-Y. Inhibitory effect of tea polyphenols on transforming growth factor-beta1 expression in rat with cyclosporine A-induced chronic nephrotoxicity. Acta Pharmacol. Sin. 2004, 25, 98–103. [Google Scholar]
- Wirestam, L.; Frodlund, M.; Enocsson, H.; Skogh, T.; Wetterö, J.; Sjöwall, C. Osteopontin is associated with disease severity and antiphospholipid syndrome in well characterised Swedish cases of SLE. Lupus Sci. Med. 2017, 4, e000225. [Google Scholar] [CrossRef] [Green Version]
- Anjaneyulu, M.; Tirkey, N.; Chopra, K. Attenuation of cyclosporine-induced renal dysfunction by catechin: Possible antioxidant mechanism. Ren. Fail. 2003, 25, 691–707. [Google Scholar] [CrossRef] [PubMed]
- Alrashedi, M.G.; Ali, A.S.; Ali, S.S.; Khan, L.M. Impact of thymoquinone on cyclosporine A pharmacokinetics and toxicity in rodents. J. Pharm. Pharmacol. 2018, 70, 1332–1339. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.A.; Lim, J.H.; Kim, M.Y.; Kim, E.N.; Koh, E.S.; Shin, S.J.; Choi, B.S.; Park, C.W.; Chang, Y.S.; Chung, S. Delayed treatment with oleanolic acid attenuates tubulointerstitial fibrosis in chronic cyclosporine nephropathy through Nrf2/HO-1 signaling. J. Transl. Med. 2014, 12, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Lai, Q.; Wei, J.; Mahmoodurrahman, M.; Zhang, C.; Quan, S.; Li, T.; Yu, Y. Pharmacokinetic and nephroprotective benefits of using Schisandra chinensis extracts in a cyclosporine A-based immune-suppressive regime. Drug Des. Dev. Ther. 2015, 9, 4997–5018. [Google Scholar]
- Gado, A.M.; Adam, A.N.I.; Aldahmash, B.A. Protective effect of lycopene against nephrotoxicity induced by cyclosporine in rats. Life Sci. J. 2013, 10, 1850–1856. [Google Scholar]
- Magendiramani, V.; Umesalma, S.; Kalayarasan, S.; Nagendraprabhu, P.; Arunkumar, J.; Sudhandiran, G. S-allylcysteine attenuates renal injury by altering the expressions of iNOS and matrix metallo proteinase-2 during cyclosporine-induced nephrotoxicity in Wistar rats. J. Appl. Toxicol. 2009, 29, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Said Elshama, S.; Osman, H.-E.H.; El-Kenawy, A.E.-M. Renoprotective effects of naringenin and olive oil against cyclosporine-induced nephrotoxicity in rats. Iranian J. Toxicol. 2016, 10, 27–37. [Google Scholar] [CrossRef] [Green Version]
- Chandramohan, Y.; Parameswari, C.S. Therapeutic efficacy of naringin on cyclosporine (A) induced nephrotoxicity in rats: Involvement of hemeoxygenase-1. Pharmacol. Rep. 2013, 65, 1336–1344. [Google Scholar] [CrossRef] [Green Version]
- Fan, F.-Y.; Sang, L.-X.; Jiang, M. Catechins and their therapeutic benefits to inflammatory bowel disease. Molecules 2017, 22, 484. [Google Scholar] [CrossRef] [Green Version]
- Almatroodi, S.A.; Almatroudi, A.; Khan, A.A.; Alhumaydhi, F.A.; Alsahli, M.A.; Rahmani, A.H. Potential therapeutic targets of epigallocatechin gallate (EGCG), the most abundant catechin in green tea, and its role in the therapy of various types of cancer. Molecules 2020, 25, 3146. [Google Scholar] [CrossRef]
- Bai, Z.-L.; Tay, V.; Guo, S.-Z.; Ren, J.; Shu, M.-G. Silibinin induced human glioblastoma cell apoptosis concomitant with autophagy through simultaneous inhibition of mTOR and YAP. BioMed Res. Int. 2018, 2018, 6165192. [Google Scholar] [CrossRef] [PubMed]
- Fattah, E.A.; Hashem, H.E.; Ahmed, F.A.; Ghallab, M.A.; Varga, I.; Polak, S. Prophylactic role of curcumin against cyclosporine-induced nephrotoxicity: Histological and immunohistological study. Gen. Physiol. Biophys. 2010, 29, 85–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- BenSaad, L.A.; Kim, K.H.; Quah, C.C.; Kim, W.R.; Shahimi, M. Anti-inflammatory potential of ellagic acid, gallic acid and punicalagin A&B isolated from Punica granatum. BMC Complement. Altern. Med. 2017, 17, 47. [Google Scholar]
- Abdul-Hamid, M.; Abdella, E.M.; Galaly, S.R.; Ahmed, R.H. Protective effect of ellagic acid against cyclosporine A-induced histopathological, ultrastructural changes, oxidative stress, and cytogenotoxicity in albino rats. Ultrastruct. Pathol. 2016, 40, 205–221. [Google Scholar] [CrossRef] [PubMed]
- Gökçe, A.; Oktar, S.; Yönden, Z.; Aydın, M.; İlhan, S.; Özkan, O.V.; Davarcı, M.; Yalçınkaya, F.R. Protective effect of caffeic acid phenethyl ester on cyclosporine A-induced nephrotoxicity in rats. Ren. Fail. 2009, 31, 843–847. [Google Scholar] [CrossRef]
- Chander, V.; Tirkey, N.; Chopra, K. Resveratrol, a polyphenolic phytoalexin protects against cyclosporine-induced nephrotoxicity through nitric oxide dependent mechanism. Toxicology 2005, 210, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Italia, J.; Datta, P.; Ankola, D.; Kumar, M. Nanoparticles enhance per oral bioavailability of poorly available molecules: Epigallocatechin gallate nanoparticles ameliorates cyclosporine induced nephrotoxicity in rats at three times lower dose than oral solution. J. Biomed. Nanotechnol. 2008, 4, 304–312. [Google Scholar] [CrossRef]
- Mun, K. Effect of epigallocatechin gallate on renal function in cyclosporine-induced nephrotoxicity. Transplant. Proc. 2004, 36, 2133–2134. [Google Scholar] [CrossRef]
- Hussein, S.A.; Ragab, O.A.; El-Eshmawy, M.A. Renoprotective effect of dietary fish oil on cyclosporine A: Induced nephrotoxicity in rats. Asian J. Biochem. 2014, 9, 71–85. [Google Scholar] [CrossRef] [Green Version]
- Zhu, S.; Wang, Y.; Chen, M.; Jin, J.; Qiu, Y.; Huang, M.; Huang, Z. Protective effect of schisandrin B against cyclosporine A-induced nephrotoxicity in vitro and in vivo. Am. J. Chin. Med. 2012, 40, 551–566. [Google Scholar] [CrossRef]
- Ateşşahin, A.; Çeribaşı, A.O.; Yılmaz, S. Lycopene, a carotenoid, attenuates cyclosporine-induced renal dysfunction and oxidative stress in rats. Basic Clin. Pharmacol. Toxicol. 2007, 100, 372–376. [Google Scholar] [CrossRef] [PubMed]
- Aiman, A.-Q.; Nesrin, M.; Amal, A.; Said, A.-D. The possible Ameliorating and Antioxidant Effects of Curcumin against Cyclosporine-Induced renal Impairment in Rats Kidney. Bull. Environ. Pharmacol. Life Sci. 2020, 9, 87–93. [Google Scholar]
- Huang, J.; Yao, X.; Weng, G.; Qi, H.; Ye, X. Protective effect of curcumin against cyclosporine A-induced rat nephrotoxicity. Mol. Med. Rep. 2018, 17, 6038–6044. [Google Scholar] [CrossRef] [Green Version]
- Tirkey, N.; Pilkhwal, S.; Kuhad, A.; Chopra, K. Hesperidin, a citrus bioflavonoid, decreases the oxidative stress produced by carbon tetrachloride in rat liver and kidney. BMC Pharmacol. 2005, 5, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yüce, A.; Ateşşahin, A.; Çeribaşı, A.O. Amelioration of cyclosporine A-induced renal, hepatic and cardiac damages by ellagic acid in rats. Basic Clin. Pharmacol. Toxicol. 2008, 103, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Zima, T.; Kamenikova, L.; Janebova, M.; Buchar, E.; Crkovska, J.; Tesar, V. The effect of silibinin on experimental cyclosporine nephrotoxicity. Ren. Fail. 1998, 20, 471–479. [Google Scholar] [CrossRef]
- Buffoli, B.; Pechánová, O.; Kojšová, S.; Andriantsitohaina, R.; Giugno, L.; Bianchi, R.; Rezzani, R. Provinol prevents CsA-induced nephrotoxicity by reducing reactive oxygen species, iNOS, and NF-kB expression. J. Histochem. Cytochem. 2005, 53, 1459–1468. [Google Scholar] [CrossRef] [Green Version]
- Rezzani, R.; Rodella, L.F.; Tengattini, S.; Bonomini, F.; Pechanova, O.; Kojšová, S.; Andriantsitohaina, R.; Bianchi, R. Protective role of polyphenols in cyclosporine A-induced nephrotoxicity during rat pregnancy. J. Histochem. Cytochem. 2006, 54, 923–932. [Google Scholar] [CrossRef]
- Rezzani, R.; Tengattini, S.; Bonomini, F.; Filippini, F.; Pechánová, O.; Bianchi, R.; Andriantsitohaina, R. Red wine polyphenols prevent cyclosporine-induced nephrotoxicity at the level of the intrinsic apoptotic pathway. Physiol. Res. 2009, 58, 511–519. [Google Scholar] [CrossRef]
- Khan, N.; Afaq, F.; Mukhtar, H. Cancer chemoprevention through dietary antioxidants: Progress and promise. Antioxid. Redox Signal. 2008, 10, 475–510. [Google Scholar] [CrossRef]
- Bingul, I.; Olgac, V.; Bekpinar, S.; Uysal, M. The protective effect of resveratrol against cyclosporine A-induced oxidative stress and hepatotoxicity. Arch. Physiol. Biochem. 2021, 127, 551–556. [Google Scholar] [CrossRef]
- Lee, J.-H.; Seo, Y.-S.; Lim, D.-Y. Provinol inhibits catecholamine secretion from the rat adrenal medulla. Korean J. Physiol. Pharmacol. 2009, 13, 229–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pechanova, O.; Rezzani, R.; Babál, P.; Bernatova, I.; Andriantsitohaina, R. Beneficial effects of Provinols: Cardiovascular system and kidney. Physiol. Res. 2006, 55, S17–S30. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.J.; Prasanth Kumar, S.; Rao, M.V.; Pandya, H.A. Ameliorative effects of curcumin towards cyclosporine-induced genotoxic potential: An in vitro and in silico study. Drug Chem. Toxicol. 2018, 41, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Bunel, V.; Antoine, M.H.; Nortier, J.; Duez, P.; Stévigny, C. Protective effects of schizandrin and schizandrin B towards cisplatin nephrotoxicity in vitro. J. Appl. Toxicol. 2014, 34, 1311–1319. [Google Scholar] [CrossRef] [Green Version]
- Stacchiotti, A.; Volti, G.L.; Lavazza, A.; Schena, I.; Aleo, M.F.; Rodella, L.F.; Rezzani, R. Different role of Schisandrin B on mercury-induced renal damage in vivo and in vitro. Toxicology 2011, 286, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Chiu, P.Y.; Leung, H.Y.; Ko, K.M. Schisandrin B enhances renal mitochondrial antioxidant status, functional and structural integrity, and protects against gentamicin-induced nephrotoxicity in rats. Biol. Pharm. Bull. 2008, 31, 602–605. [Google Scholar] [CrossRef] [Green Version]
- Amorim, A.G.; Souza, J.M.; Santos, R.C.; Gullon, B.; Oliveira, A.; Santos, L.F.; Virgino, A.L.; Mafud, A.C.; Petrilli, H.M.; Mascarenhas, Y.P. HPLC-DAD, ESI–MS/MS, and NMR of Lycopene Isolated From P. guajava L. and Its Biotechnological Applications. Eur. J. Lipid Sci. Technol. 2018, 120, 1700330. [Google Scholar] [CrossRef] [Green Version]
- Tapiero, H.; Townsend, D.M.; Tew, K.D. The role of carotenoids in the prevention of human pathologies. Biomed. Pharmacother. 2004, 58, 100–110. [Google Scholar] [CrossRef]
- Matos, H.R.; Di Mascio, P.; Medeiros, M.H. Protective effect of lycopene on lipid peroxidation and oxidative DNA damage in cell culture. Arch. Biochem. Biophys. 2000, 383, 56–59. [Google Scholar] [CrossRef]
- Karahan, İ.; Ateşşahin, A.; Yılmaz, S.; Çeribaşı, A.; Sakin, F. Protective effect of lycopene on gentamicin-induced oxidative stress and nephrotoxicity in rats. Toxicology 2005, 215, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Avula, P.R.; Asdaq, S.M.; Asad, M. Effect of aged garlic extract and s-allyl cysteine and their interaction with atenolol during isoproterenol induced myocardial toxicity in rats. Indian J. Pharmacol. 2014, 46, 94–99. [Google Scholar] [PubMed] [Green Version]
- Farag, M.M.; Ahmed, G.O.; Shehata, R.R.; Kazem, A.H. Thymoquinone improves the kidney and liver changes induced by chronic cyclosporine A treatment and acute renal ischaemia/reperfusion in rats. J. Pharm. Pharmacol. 2015, 67, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Hussein, S.A.; Elsenosi, Y.; Esmael, T.E.A.; Amin, A.; Sarhan, E.A.M. Thymoquinone suppressed Cyclosporine A-induced Nephrotoxicity in rats via antioxidant activation and inhibition of inflammatory and apoptotic signaling pathway. Benha Vet. Med. J. 2020, 39, 40–46. [Google Scholar]
- Zaporozhets, T.; Besednova, N. Prospects for the therapeutic application of sulfated polysaccharides of brown algae in diseases of the cardiovascular system. Pharm. Biol. 2016, 54, 3126–3135. [Google Scholar] [CrossRef]
- Patel, S. Therapeutic importance of sulfated polysaccharides from seaweeds: Updating the recent findings. 3 Biotech 2012, 2, 171–185. [Google Scholar] [CrossRef] [Green Version]
- Josephine, A.; Amudha, G.; Veena, C.K.; Preetha, S.P.; Rajeswari, A.; Varalakshmi, P. Beneficial effects of sulfated polysaccharides from Sargassum wightii against mitochondrial alterations induced by Cyclosporine A in rat kidney. Mol. Nutr. Food Res. 2007, 51, 1413–1422. [Google Scholar] [CrossRef]
- Josephine, A.; Veena, C.K.; Amudha, G.; Preetha, S.P.; Sundarapandian, R.; Varalakshmi, P. Sulphated Polysaccharides: New Insight in the Prevention of Cyclosporine A-Induced Glomerular Injury. Basic Clin. Pharmacol. Toxicol. 2007, 101, 9–15. [Google Scholar] [CrossRef]
- Miao, B.; Li, J.; Fu, X.; Gan, L.; Xin, X.; Geng, M. Sulfated polymannuroguluronate, a novel anti-AIDS drug candidate, inhibits T cell apoptosis by combating oxidative damage of mitochondria. Mol. Pharmacol. 2005, 68, 1716–1727. [Google Scholar] [CrossRef] [Green Version]
- Maneesh, A.; Chakraborty, K.; Makkar, F. Pharmacological activities of brown seaweed Sargassum wightii (Family Sargassaceae) using different in vitro models. Int. J. Food Prop. 2017, 20, 931–945. [Google Scholar] [CrossRef] [Green Version]
- Josephine, A.; Veena, C.K.; Amudha, G.; Preetha, S.P.; Varalakshmi, P. Protective role of sulphated polysaccharides in abating the hyperlipidemic nephropathy provoked by cyclosporine A. Arch. Toxicol. 2007, 81, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Ernst, E.; Pittler, M. Efficacy of ginger for nausea and vomiting: A systematic review of randomized clinical trials. Br. J. Anaesth. 2000, 84, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Kazeem, M.I.; Akanji, M.A.; Yakubu, M.T.; Ashafa, A.O.T. Protective effect of free and bound polyphenol extracts from ginger (Zingiber officinale Roscoe) on the hepatic antioxidant and some carbohydrate metabolizing enzymes of streptozotocin-induced diabetic rats. Evid.-Based Complement. Altern. Med. 2013, 2013, 935486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laight, D.; Carrier, M.; Änggård, E. Antioxidants, diabetes and endothelial dysfunction. CardiovaSC Res. 2000, 47, 457–464. [Google Scholar] [CrossRef] [Green Version]
- Adekunle, I.A.; Imafidon, C.E.; Oladele, A.A.; Ayoka, A.O. Ginger polyphenols attenuate cyclosporine-induced disturbances in kidney function: Potential application in adjuvant transplant therapy. Pathophysiology 2018, 25, 101–115. [Google Scholar] [CrossRef]
- Abduljawad, E.A. Potential Antioxidant Effect of Date Pits Extract on Nephrotoxicity induced by Cyclosporine-A in Male Rats. Int. J. Pharm. Phytopharmacol. Res. 2019, 9, 21–27. [Google Scholar]
- Lone, K.P. Protective Effect of Sponacea Oleracea Extract on cyclosporine-A induced nephrotoxixicty in male albino rats. Biomedica 2016, 32, 935486. [Google Scholar]
- Doh, K.C.; Lim, S.W.; Piao, S.G.; Jin, L.; Heo, S.B.; Zheng, Y.F.; Bae, S.K.; Hwang, G.H.; Min, K.I.; Chung, B.H. Ginseng treatment attenuates chronic cyclosporine nephropathy via reducing oxidative stress in an experimental mouse model. Am. J. Nephrol. 2013, 37, 421–433. [Google Scholar] [CrossRef]
- Venkateswarlu, K.; Heerasingh, T.; Babu, C.N.; Triveni, S.; Manasa, S.; Babu, T.N.B. Preclinical evaluation of nephroprotective potential of a probiotic formulation LOBUN on Cyclosporine-A induced renal dysfunction in Wistar rats. Braz. J. Pharm. Sci. 2017, 53, e16042. [Google Scholar] [CrossRef]
- Durak, I.; Çetin, R.; Çandır, Ö.; Devrim, E.; Kılıçoğlu, B.; Avcı, A. Black grape and garlic extracts protect against cyclosporine a nephrotoxicity. Immunol. Investig. 2007, 36, 105–114. [Google Scholar] [CrossRef]
- Hussein, S.A.; Ragab, O.A.; El-Eshmawy, M.A. Protective effect of green tea extract on cyclosporine A: Induced nephrotoxicity in rats. J. Biol. Sci. 2014, 14, 248–257. [Google Scholar] [CrossRef]
- Mohamadin, A.; El-Beshbishy, H.; El-Mahdy, M. Green tea extract attenuates cyclosporine A-induced oxidative stress in rats. Pharmacol. Res. 2005, 51, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Seven, I.; Baykalir, B.G.; Seven, P.T.; Dağoğlu, G. The ameliorative effects of propolis against cyclosporine A induced hepatotoxicity and nephrotoxicity in rats. System 2014, 10, 15. [Google Scholar]
- Aziz, M.M.; Eid, N.I.; Nada, A.S.; Amin, N.E.-D.; Ain-Shoka, A.A. Possible protective effect of the algae spirulina against nephrotoxicity induced by cyclosporine A and/or gamma radiation in rats. Environ. Sci. Pollut. Res. 2018, 25, 9060–9070. [Google Scholar] [CrossRef]
- Xu, F.; Huang, J.; Jiang, L.; Xu, J.; Mi, J. Amelioration of cyclosporin nephrotoxicity by Cordyceps sinensis in kidney-transplanted recipients. Nephrol. Dial. Transplant. 1995, 10, 142–143. [Google Scholar]
- Shalby, A.; Hamza, A.; Ahmed, H. New insight on the anti-inflammatory effect of some Egyptian plants against renal dysfunction induced by cyclosporine. Eur. Rev. Med. Pharmacol. Sci. 2012, 16, 455–461. [Google Scholar]
- Shatwan, I.M. Renoprotective Effect Of Ipomoea Batatas Aqueous Leaf Extract On Cyclosporine-Induced Renal Toxicity In Male Rats. Pharmacophores 2019, 10, 85–92. [Google Scholar]
- Uz, E.; Bayrak, O.; Uz, E.; Kaya, A.; Bayrak, R.; Uz, B.; Turgut, F.H.; Bavbek, N.; Kanbay, M.; Akcay, A. Nigella sativa oil for prevention of chronic cyclosporine nephrotoxicity: An experimental model. Am. J. Nephrol. 2008, 28, 517–522. [Google Scholar] [CrossRef]
- Wei, Y.; Luo, Z.; Zhou, K.; Wu, Q.; Xiao, W.; Yu, Y.; Li, T. Schisandrae chinensis fructus extract protects against hepatorenal toxicity and changes metabolic ions in cyclosporine A rats. Nat. Prod. Res. 2019, 35, 2915–2920. [Google Scholar] [CrossRef]
- Ergüder, İ.B.; Çetin, R.; Devrim, E.; Kılıçoğlu, B.; Avcı, A.; Durak, İ. Effects of cyclosporine on oxidant/antioxidant status in rat ovary tissues: Protective role of black grape extract. Int. Immunopharmacol. 2005, 5, 1311–1315. [Google Scholar] [CrossRef]
- Hussein, S.A.; Elsenosi, Y.; Esmael, T.E.A.; Amin, A.; Sarhan, E.A.M. Evaluation of renoprotective effect of grape seed proanthocyanidin extract on Cyclosporine A-induced Nephrotoxicity by mitigating inflammatory response, oxidative stress and apoptosis in rats. Benha Vet. Med. J. 2020, 39, 167–172. [Google Scholar] [CrossRef]
- Ulusoy, S.; Ozkan, G.; Yucesan, F.B.; Ersöz, Ş.; Orem, A.; Alkanat, M.; Yuluğ, E.; Kaynar, K.; Al, S. Anti-apoptotic and anti-oxidant effects of grape seed proanthocyanidin extract in preventing cyclosporine A-induced nephropathy. Nephrology 2012, 17, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Wongmekiat, O.; Thamprasert, K. Investigating the protective effects of aged garlic extract on cyclosporin-induced nephrotoxicity in rats. Fundam. Clin. Pharmacol. 2005, 19, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Wu, C.; Wang, S.; Gao, S.; Liu, J.; Dong, Z.; Zhang, B.; Liu, M.; Sun, X.; Guo, P. Extracts and lignans of Schisandra chinensis fruit alter lipid and glucose metabolism in vivo and in vitro. J. Funct. Foods 2015, 19, 296–307. [Google Scholar] [CrossRef]
- El Daly, E.S. Protective effect of cysteine and vitamin E, Crocus sativus and Nigella sativa extracts on cisplatin-induced toxicity in rats. J. Pharm. Belg. 1998, 53, 87–93, discussion 93. [Google Scholar] [PubMed]
- Badary, O.A.; Nagi, M.N.; Al-Shabanah, O.A.; Al-Sawaf, H.A.; Al-Sohaibani, M.O.; Al-Bekairi, A.M. Thymoquinone ameliorates the nephrotoxicity induced by cisplatin in rodents and potentiates its antitumor activity. Can. J. Physiol. Pharmacol. 1997, 75, 1356–1361. [Google Scholar] [CrossRef]
- Muckensturm, B.; Foechterlen, D.; Reduron, J.-P.; Danton, P.; Hildenbrand, M. Phytochemical and chemotaxonomic studies of Foeniculum vulgare. Biochem. Syst. Ecol. 1997, 25, 353–358. [Google Scholar] [CrossRef]
- Owen, R.; Haubner, R.; Hull, W.; Erben, G.; Spiegelhalder, B.; Bartsch, H.; Haber, B. Isolation and structure elucidation of the major individual polyphenols in carob fibre. Food Chem. Toxicol. 2003, 41, 1727–1738. [Google Scholar] [CrossRef]
- Cook, J.A.; VanderJagt, D.J.; Pastuszyn, A.; Mounkaila, G.; Glew, R.S.; Millson, M.; Glew, R.H. Nutrient and chemical composition of 13 wild plant foods of Niger. J. Food Compos. Anal. 2000, 13, 83–92. [Google Scholar] [CrossRef]
- Hsu, B.; Coupar, I.M.; Ng, K. Antioxidant activity of hot water extract from the fruit of the Doum palm, Hyphaene thebaica. Food Chem. 2006, 98, 317–328. [Google Scholar] [CrossRef]
- Calder, P.C. Omega-3 fatty acids and inflammatory processes: From molecules to man. Biochem. Soc. Trans. 2017, 45, 1105–1115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Méndez, L.; Medina, I. Polyphenols and fish oils for improving metabolic health: A revision of the recent evidence for their combined nutraceutical effects. Molecules 2021, 26, 2438. [Google Scholar] [CrossRef] [PubMed]
- Priyamvada, S.; Priyadarshini, M.; Arivarasu, N.; Farooq, N.; Khan, S.; Khan, S.A.; Khan, M.W.; Yusufi, A. Studies on the protective effect of dietary fish oil on gentamicin-induced nephrotoxicity and oxidative damage in rat kidney. Prostaglandins Leukot. Essent. Fatty Acids 2008, 78, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Ali, B.; Bashir, A. Effect of fish oil treatment on gentamicin nephrotoxicity in rats. Ann. Nutr. Metab. 1994, 38, 336–339. [Google Scholar] [CrossRef]
- Cid, T.P.; Garcıa, J.C.; Alvarez, F.C.; De Arriba, G. Antioxidant nutrients protect against cyclosporine A nephrotoxicity. Toxicology 2003, 189, 99–111. [Google Scholar]
- Klawitter, J.; Klawitter, J.; Schmitz, V.; Brunner, N.; Crunk, A.; Corby, K.; Bendrick-Peart, J.; Leibfritz, D.; Edelstein, C.L.; Thurman, J.M. Low-salt diet and cyclosporine nephrotoxicity: Changes in kidney cell metabolism. J. Proteome Res. 2012, 11, 5135–5144. [Google Scholar] [CrossRef]
- Martin, W.F.; Armstrong, L.E.; Rodriguez, N.R. Dietary protein intake and renal function. Nutr. Metab. 2005, 2, 25. [Google Scholar] [CrossRef] [Green Version]
- Pons, M.; Plante, I.; LeBrun, M.; Gourde, P.; Simard, M.; Grenier, L.; Thibault, L.; Labrecque, G.; Beauchamp, D. Protein-rich diet attenuates cyclosporin A-induced renal tubular damage in rats. J. Ren. Nutr. 2003, 13, 84–92. [Google Scholar] [CrossRef]
- Musumeci, G.; Trovato, F.M.; Pichler, K.; Weinberg, A.M.; Loreto, C.; Castrogiovanni, P. Extra-virgin olive oil diet and mild physical activity prevent cartilage degeneration in an osteoarthritis model: An in vivo and in vitro study on lubricin expression. J. Nutr. Biochem. 2013, 24, 2064–2075. [Google Scholar] [CrossRef]
- Thakur, L.; Ghodasra, U.; Patel, N.; Dabhi, M. Novel approaches for stability improvement in natural medicines. Pharmacogn. Rev. 2011, 5, 48–54. [Google Scholar] [CrossRef] [Green Version]
- Seeff, L.B.; Bonkovsky, H.L.; Navarro, V.J.; Wang, G. Herbal products and the liver: A review of adverse effects and mechanisms. Gastroenterology 2015, 148, 517–532.e3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bunchorntavakul, C.; Reddy, K. Herbal and dietary supplement hepatotoxicity. Aliment. Pharmacol. Ther. 2013, 37, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Sparks, E.; Zorzela, L.; Necyk, C.; Khamba, B.; Urichuk, L.; Barnes, J.; Vohra, S. Study of Natural products Adverse Reactions (SONAR) in children seen in mental health clinics: A cross-sectional study. BMJ Paediatr. Open 2020, 4, e000674. [Google Scholar] [CrossRef] [PubMed]
| Compound Name/Class | M.F. | M.W. | Plant/Name (Organ, Family) | Ref. |
|---|---|---|---|---|
| Terpenoids | ||||
| Thyomquinone | C10H12O2 | 164 | Nigella sativa (Ranunculaceae) | [23] |
| Oleanolic acid | C30H48O3 | 456 | Olea europaea (Oleaceae) | [24] |
| Lignans | ||||
| Schisandrin B | C23H28O6 | 400 | Schisandra chinensis (Schisandraceae) | [25] |
| Carotenoids | ||||
| Lycopene | C40H56 | 536 | Psidium guajava (Myrtaceae) Solanum lycopersicum (Solanaceae) | [26] |
| Organo-sulphur | ||||
| S-allylcysteine | C6H11NO2S | 161 | Allium sativum (Amaryllidaceae) | [27] |
| Flavonoids | ||||
| Naringenin | C15H12O5 | 272 | Citrus fruits (Rutaceae) | [28] |
| Naringin | C27H32O14 | 580 | Citrus fruits (Rutaceae) | [29] |
| Catechin | C15H14O6 | 290 | Camellia sinensis (Theaceae) | [30] |
| Epigallocatechin gallate | C22H18O11 | 458 | Camellia sinensis (Theaceae) | [31] |
| Silibinin | C25H22O10 | 482 | Silybum marianum L. (Asteraceae) | [32] |
| Phenolics | ||||
| Curcumin | C21H20O6 | 368 | Curcuma longa (Zingiberaceae) | [33] |
| Ellagic acid | C14H6O8 | 302 | Punica granatum (Punicaceae) | [34,35] |
| Caffeic acid phenethyl ester | C17H16O4 | 284 | Propolis | [36] |
| Resveratrol | C14H12O3 | 228 | Vitis vinifera (Vitaceae) | [37] |
| Compound | Experimental Model | Intervention (Dose, Route/Duration of Administration) | Studied Parameter | Pharmacological Outcomes/Effects | References |
|---|---|---|---|---|---|
| Thymoquinone | Male Wister rats | Four groups Control: vehicle TQ: TQ 10 mg/kg, orally TQ+CA: TQ (10 mg/kg, orally)/1 week then CA (10 mg/kg, I.P.)/5 days with continuing TQ CA: 10 mg/kg, I.P./5 days Treatment duration: 28 days |
Serum creatinine Serum cystatin C Blood glucose |
Concomitant administration of TQ with CA ↓ serum cystatin and blood glucose levels TQ prevented the major structural changes in both glomerular and tubular components induced by CA | [23] |
| White male albino rats | Three groups Control (no drugs) CA: CA 25 mg/kg/day/orally/21 days TQ protected + CA: TQ (10 mg/kg/day, orally) for 7 days before and during CA (25 mg/kg/day/orally) treatment Treatment duration: 21 days |
Serum urea and creatinine L-MDA and GSH levels CAT activity NF-kB and PAI-1 expression levels Caspase-3 p53 Bcl-2 |
TQ ↓ caspase-3 and p53 and ↑ Bcl-2 gene expressions TQ ↓ NF-κB and PAI-1 gene expressions TQ ↓ L-MDA level and ↑ GSH level and CAT activity TQ ↓ urea and creatinine values | [40] | |
| Oleanolic acid (OA) | Five-week-old male ICR mice | Four groups Control: 1 mL olive oil/kg/daily, SC VH + OA: 1 mL olive oil/kg/daily, SC then OA (25 mg/kg/daily I.P. for one week) CA: CA 30 mg/kg/ daily, SC CA + OA: CA (30 mg/kg/ daily, SC) + OA (25 mg/kg/daily I.P.) Treatment duration: 28 days | Renal functional parameters Morphological changes Nrf-2, Keap1, and antioxidant defense system Renal apoptosis | OA ↓ tubulointerstitial fibrosis and inflammation OA ↓ urinary 8-OHdG and 8-iso-PGF2α levels OA ↑ ratio of nuclear/total Nrf2 and enhanced HO-1 expression OA ↓ expression of Bcl-2 and ↑ Bax and cleaved caspase-3 | [24] |
| Schisandrin B (ScB) | HK-2 cell line | Pretreatment with ScB (2.5, 5.0, and 10.0 μM) for 12 h, then CA (10 μM) for 24 h | ROS, Nrf2, Bax, Bcl-2, LC3, Beclin1, and p62 |
ScB ↓ ROS and LDH levels ScB ↑ ΔΨm and GSH levels ScB activated Nrf2 ScB ameliorated apoptosis induced by CA ScB abrogated autophagy activation stimulated by CA | [13] |
| ScB (2.5, 5, and 10 M) for 30 min and then exposed to CA (10 M) for 24 h |
LDH release Cell viability Cellular apoptosis GSH and ATP levels ROS levels |
ScB ↓ LDH release and ↑ cell viability ScB ↓ number of early apoptotic cells ScB ↑ GSH and ATP levels | [41] | ||
| KM adult male mice | Four groups Control: olive oil (10 mL/kg, gavage) and then olive oil (2 mL/kg, SC) ScB: 20 mg/kg, gavage, and then olive oil (2 mL/kg, SC) CA: olive oil (10 mL/kg, gavage), and then CA (30 mg/kg, SC) CA+ScB: ScB (20 mg/kg, gavage), and then CA (30 mg/kg, SC) Treatment duration: 28 days |
LDH release Cellular apoptosis GSH and ATP levels ROS levels GSH level MDA level |
↓ BUN and creatinine levels ↑ GSH and ↓ MDA levels ScB markedly improved the structural changes induced by CA | [41] | |
| Lycopene | Male Swiss albino rats | Four groups Control: saline solution, I.P. Lyc: 40 mg/kg/day, oral gavage CA: 15 mg/kg/day, I.P. for 10 days LYC + CA: LYC (40 mg/kg/day, oral gavage for 5 days then CA (15 mg/kg/day, I.P. for 10 days) concomitantly with LYC Treatment duration: 15 days | Serum creatinine and urea levels MDA level GSH-Px activity SOD activity | LYC ↓ urea and creatinine levels LYC restored GSH and ↓ MDA levels LYC ↑ Gpx and SOD activities LYC markedly improved CA-induced structural changes | [26] |
| Adult male Sprague Dawley rats | Four groups Control: 0.5 mL isotonic saline + 0.5 mL corn oil, SC for 21 days CA: 15 mg/kg/day CA + 0.5 mL corn oil, SC for 21 days LYC: 10 mg/kg/day LYC + 0.5 mL corn oil, SC for 21 days CA+LYC: 10 mg/kg/day LYC + 15 mg/kg/day CA, SC for 21 days Treatment duration: 21 days |
TBARs level GSH level GSH-Px activity CAT activity Plasma creatinine, urea, Na+ and Ca++ |
LYC ↓ plasma creatinine and urea levels LYC normalized TBARs LYC ↑ GSH-Px and CAT activity LYC alleviated CA-induced histological changes | [42] | |
| S-Allylcysteine (SAC) | Wistar male albino rats | Five groups Control: oral saline CA: 25 mg/kg/day, orally CA+SAC: CA 25 mg/kg b.w./day with SAC 100 mg/kg/day, I.P. CA+ Vit. C: 25 mg/kg/day with vitamin C 100 mg/kg/day, orally SAC: 100 mg/kg/day I.P. Treatment duration: 21 days |
Serum renal markers urea, uric acid, creatinine, and BUN Renal enzymes (ALP, ACP, AST, ALT, and LDH) Antioxidants enzymic (SOD, CAT, GPx, and GR) non-enzymic (GSH, vits C and E) Expressions of NF-kB, iNOS, and MMP-2 |
SAC prevented alteration in urea, uric acid, creatinine, and BUN induced by CA the same as vit C SAC ↓ the rise in LPO induced by CA compared with vit. C SAC ↑ antioxidants levels compared with vit. C SAC ↓ renal injury and inflammation SAC suppressed the expressions of NF-kB, MMP-2, and iNOS | [27] |
| Curcumin | Adult male rats | Three groups Control Curcumin+CA (15 mg/kg with CA) CA: 20 mg/kg, SC/5 days Treatment duration: 21 days | Morphological changes Glutathione S-transferase (GST) immune expression Serum urea and creatinine | Curcumin showed promising protective effect against CA-induced nephrotoxicity in rats through improving histological parameters, antioxidant effect, and renal dysfunction | [33,43,44] |
| Five groups Vehicle: olive oil SC + 0.5% CMC orally for 21 days CA: 20 mg/kg/day, SC in olive oil for 21 days CA+ Curcumin: CA (20 mg/kg/day SC) + Curcumin (5, 10, or 15 mg/kg for 21 days Treatment duration: 21 days | Oxidative stress in kidney tissues (TBARS, GSH, SOD, and CAT) | Curcumin ameliorated renal dysfunction through decreasing TBARS and increasing levels of antioxidant enzymes (GSH, SOD, and CAT) | [45] | ||
| Resveratrol (RES) | Male albino Wistar rats | Eight groups Control Vehicle: olive oil (SC) + saline (p.o.) for 21 days CA: CA (20 mg/kg, SC) in olive oil for 21 days RES 2 mg+CA: RES (2 mg/kg, p.o.) 24 h before CA and continued along with CA for 21 days RES 5 mg+CA: RES (5 mg/kg, p.o.) 24 h before CA and continued along with CA for 21 days RES 10 mg+CA: RES (5 mg/kg, p.o.) 24 h before CA and continued along with CA for 21 days RES+ L-NAME: RES (5 mg/kg, p.o.) and L-NAME (10 mg/kg, I.P.) 24 h before CA and continued along with CsA for 21 days L-NAME: L-NAME (10 mg/kg, I.P.) 24 h before CA and continued along with CA for 21 days Treatment duration: 21 days | Renal oxidative stress Renal functions Tissue and urine nitrite and nitrate levels Renal lipid peroxides and antioxidant enzymes Renal histology | RES (5, 10 mg/kg) improved renal dysfunction, renal and tissue NO levels, and oxidative stress Co-administration of L-NAME blocked RES protective effect indicating that RES effect is NO-dependent | [37] |
| Naringin (NG) | Male albino Wistar rats | Four groups Control: olive oil CA: CA 25 mg/kg for 21 days NG: NG 40 mg/kg/orally CA+NG: CA-treated group concurrently with NG daily (oral dose 40 mg/kg) Treatment duration: 21 days | Lipid peroxides (TBARS) and hydroxyl radical (OH) SOD, CAT, GSH, and vitamins C, E, and A | NG significantly ↓ oxidative stress and restored the levels of enzymic and non-enzymic antioxidants in renal tissues | [29] |
| Caffeic acid phenethyl ester (CAPE) | Wistar albino female rats | Four groups Control: 0.5 mL normal saline CA: CA (15 mg/kg/day SC in saline for 10 days) CAPE: CAPE 10 µM/kg/day, I.P. in saline for 11 days CAPE+CA: CAPE 10 µM/kg/day, I.P. for 11 days, while CA was administered concurrently for 10 days Treatment duration: 11 days | MPO activity Lipid peroxidation SOD and CAT | CAPE prevented increase in MDA CAPE ↑ CAT, but did not affect MPO and SOD | [36] |
| Catechin (CATC) | Wistar rats (both sexes) | Five groups Control: olive oil (S.C) and 0.5% sodium CMC orally CA: CA (20 mg/Kg/day/SC, for 21 days) CA+50mg CATC: CA (20 mg/Kg/day, SC)+ CATC (50 mg/kg/day P.O) for 21 days CA+100mg catechin: CA (20 mg/Kg/day, SC)+ CATC (100 mg/kg/day, P.O) CATC: CATC (100 mg/kg/day, P.O.) Treatment duration: 11 days | Body weight, water intake, food intake, urine output and kidney weight, oxidative stress markers (renal MDA, glutathione, renal antioxidant enzymes, such as SOD, catalase) | CATC ↑ body weight by administration of CATC (100 mg/kg/day) with CA for 21 days CATC ↑ renal function by ↓ serum creatinine, blood urea nitrogen, and ↑ creatinine and urea clearance CATC (50 mg/kg/day) restored only increased serum creatinine levels | [22] |
| Epigallocatechin gallate PLGA NPs | Male Sprague Dawley rats | Six groups All receiving CA (15 mg/kg/day orally) and EGCG (50 mg/kg) Control Sandimmune neural (CA) SN+EGCG (I.P.) daily SN+EGCG (oral) daily SN+EGCG (I.P.) once in three days SN+EGCG (I.P.) once in three days (blank particles) Treatment duration: 30 days | BUN, PC, MDA, GSH, and total proteins Histological studies | ↓ BUN and PC levels (I.P. injection of EGCG along with SN) Co-treatment of EGCG NPs as equally effective as I.P. administration EGCG solution prevented histological damage induced by SN treatment EGCG NPs prevented renal damage, artial glomerular collapse, and tubular damage | [38] |
| Ellagic acid | Adult male Sprague Dawley rats | Four groups Control: 0.5 mL isotonic saline+ 0.5 mL slightly alkaline solution, SC for 21 days CA: 15 mg/kg+0.5 mL slightly alkaline solution S.C for 21 days Ellagic acid: 0.5 mL isotonic saline+10 mg/kg ellagic acid SC for 21 days CA+ellagic acid, SC for 21 days Treatment duration: 21 days | MDA, GSH, GSH-Px, and CAT activities Histopathological examination | No significant change in GSH level Slight decrease in MDA level Ellagic acid ↑ decreased GSH-Px activity and CAT activity due to CA intake Ameliorated tubular necrosis, tubular degeneration, and desquamation, thickening basement membrane, inter-tubular haemorrhagia, and tubular dilatation | [46] |
| Silibinin | Female Wistar rats | Four groups Control: standard chow and I.P. injection of placebo solution Silibinin: standard chow and I.P. silibinin 5 mg/kg CA: 30 mg/kg I.P. CA+Silibinin: I.P. silibinin and CA Treatment duration: 15 days | Urea, creatinine, total protein, and GFR Lipid peroxidation Histopathological examination Total MDA | Silibinin ↓ CA-induced LPO without protective effect on GFR | [47] |
| Naringenin (NGA) and VOO | Four groups Control: saline CA: 25 mg/kg/day for 45 days CA+NGA: NGA 100 mg/kg/day+ CA 25 mg/kg/day for 45 days CA+VOO: VOO 1.25 mL/kg/day + CA 25 mg/kg/day for 45 days Treatment duration: 45 days | Body and kidney weights Cyclosporine blood level Renal biochemical markers Redox status | VOO and NGA ↑ body and kidney weights VOO and NGA ↓ CA blood level VOO and NAR ↓ serum creatinine and urea levels VOO and NGA ↑ CAT, peroxidase, GSH, and SOD VOO and NGA ↓ MDA and NO | [28] | |
| Provinol (PV) mixture of polyphenolics: proanthocyanidins, total anthocyanins, free anthocyanins, catechin, hydroxycinnamic acid, and flavonols | Adult male Wistar rats | Four groups Control: olive oil, SC PV: PV (40 mg/kg/day orally) CA: CA (15 mg/kg/day/SC) PV+CA: PV and CA simultaneously Treatment duration: 21 days | Systolic blood pressure Creatinine clearance Oxidative stress NF-kB NO-synthase | PV ↓ oxidative stress and ↑ iNOS and NF-kB expression induced by CA | [48] |
| Ninety-day-old virgin female and male Wistar rats | Four groups Control: olive oil, SC PV: PV (40 mg/kg/day/orally) CA: CA (15 mg/kg/day/SC) CA+PV: CA and PV I.P. daily for 21 days of pregnancy Treatment duration: 21 days | Histopathological and immunohistochemical evaluations Stereological analysis for glomerular volume and size iNOS and MMP2 | PV ↓ oxidative stress and iNOS expression via NF-kB pathway PV protected on CA-induced structural and functional alterations of the kidney | [49] | |
| Adult male Wistar rats | Four groups Control: olive oil (SC) CA: CA (15 mg/kg/day/ SC) for 21 days PV: (40 mg/kg/day, orally) PV+CA: PV concurrently during CA injections for 21 days Treatment duration: 21 days | Body weight, SBP, serum creatinine, urinary protein concentration, GFR, creatinine clearance, renal GSH content | PV prevented CA-induced decrease in body weight and increase in SBP PV ↓ CA-induced depletion of GSH PV restored morphological and biochemical alterations | [50] |
| Name of Plant (Organ, Family)/Diet | Extract/Fraction (Major Constituents) | Intervention (Dose, Route/Administration Duration) | Studied Parameter | Pharmacological Outcomes/Effects | Reference |
|---|---|---|---|---|---|
| Sargassum wightii (Sargassaceae) | Sulphated polysaccharides (SWSPs) | Male albino Wistar rats Four groups Control: olive oil SWSP: SWSP (5 mg/kg/b.w., S.C.) SWSP+CA: SWSP (5 mg/Kg/b.w., SC)/3 weeks then CA (25 mg/kg/b.w., orally)/21 days CA: CA (25 mg/kg/b.w., orally/21 days) Treatment duration: 28 days |
Glycosaminoglycans Protein content Creatinine clearance Lysosomal enzymes Serum and urinary creatinine Protein-bound carbohydrates | SWSP ↑ creatinine clearance SWSP ↓ lysosomal enzyme activity SWSP ↓ glycoproteins levels SWSP ↓ glycosaminoglycanuria SWSP ↓ proteinuria SWSP attenuated CA-induced histological changes | [69] |
| Male albino Wistar rats Four groups Control: olive oil alone CA: 25 mg/kg/b.w., orally/21 days SWSP: 5 mg/Kg/b.w., SC SWSP+CA: SWSP (5 mg/Kg/b.w., SC)/3 week then CA (25 mg/kg/b.w., orally)/21 days. Treatment duration: 28 days |
Enzymes (ALP, NAG, LDH, and c-GT) Mitochondrial oxidative stress (ROS, SOD, GPx, and GSH) Lipid peroxidation (MDA) TCA cycle enzymes Enzyme complexes of electron transport chain | SWSP ↓ ROS level and lipid peroxidation SWSP ↑ antioxidant defense system SWSP ↑ activities of tricarboxylic acid cycle and electron transport chain enzymes and ↓ urinary enzymes SWSP ameliorated mitochondrial swelling | [68] | ||
| Dietary fish oil (DFO) | White male albino rats Four groups Control: no drugs DFO: DFO (270 mg/kg/day, orally) CA: CA (25 mg/kg/day orally for 21 days) DFO+CA: DFO for 21 days before, 21 days concurrently during CA and 21 days later Treatment duration: 63 days |
Serum glucose, TP, albumin, and lipid profile (TC, TAGs, and PLs) Renal function (urea, UA and Cr, and electrolytes (Na and K)) Inorganic phosphorus and haptoglobin levels LDH and GGT activities MDA, GSH, NO, and TOA levels CAT, SOD, and Gpx activities | DFO restored urea, uric acid, creatinine, and haptoglobin levels DFO normalized lipid profile, LDH, CGT, serum protein, and electrolytes DFO ↓ peroxidative levels and ↑ CAT, SOD, and GPx activities DFO ↑ GSH and TAC levels | [40] | |
| Probiotic formulation LOBUN | Male Wistar rats Four groups Normal: olive oil Control: CA (20 mg/kg/day, SC) for 15 days CA+LOBUN: CA (20 mg/kg/day, SC) for 15 days; LOBUN (500 mg/kg/p.o./twice daily) from 15th to 28th day CA+LOBUN: CA (20 mg/kg/day, SC) for 15 days; LOBUN (500 mg/kg p.o./thrice daily) from 15th to 28th day Treatment duration: 28 days |
BUN, serum Cr, serum UA, total serum and urine proteins, and urine K and Na | LOBUN ↓ serum BUN, serum Cr, serum UA and ↑ total serum protein LOBUN ↓ urine protein concentration and ↑ Na and K LOBUN ↓ inflammatory infiltration and vacuolization | [80] | |
| Zingiber officinale (Zingebraceae) | 80% rhizome acetone extract rich in polyphenols (GP) | Male Wistar rats Five groups Control: distilled H2O CA: CA (50 mg/kg, p.o.) for 10 consecutive days CA+GP: CA (50 mg/kg, p.o.) + GP (100 mg/kg, p.o.) for 21 days CA+GP: CA (50 mg/kg, p.o.) +GP (200 mg/kg, p.o.) for 21 days CA+GP: CA (50 mg/kg, p.o.) + GP (400 mg/kg, p.o.) for 21 days Treatment duration: 21 days |
Percentage of body weight Kidney weight changes Food consumption, water intake, and urine volume Creatinine clearance Electrolyte assays Oxidative stress | GP attenuated kidney injury caused by CA through improvement of plasma and urine levels of creatinine, urea, Na+ and K+ electrolyte balance, as well as creatinine clearance GP improved feeding pattern, relative kidney weight, and oxidative stress | [76] |
| Date pits (DPEs) | Aqueous extract | Male Wister albino rats Four groups Control: 0.5 mL of NaCl/ day for 28 days CA: CA (15 mg/kg/day, SC) for 28 days DPE+CA: DPE (4 mL/ kg/ day)+CA (15 mg/kg/d) for 28 days DPE+CA: DPE (6 mL/ kg/ day, orally)+CA (15 mg/kg/ day) for 28 days Treatment duration: 28 days | Serum Cr, BUN, UA, sodium, potassium, total protein, and albumin levels MDA, GSH, and CAT activities Histological changes | DPE ameliorated all measured parameters DPE protected against CA-induced histopathological changes DPE ↓ MDA and ↑ GSH and CAT activities | [77] |
| Spinacea oleracea | 1%n-hexane extract (SOH) | Rats Four groups Control: olive oil (2 mL/kg, I.P., 7 days) CA: CA (20 mg/kg in 2 mL olive oil I.P., 7 days) SOH+CA: SOH (0.5 mL concomitantly with CA (20 mg/kg in 2 mL olive oil, I.P.) from days 7 to 14 SOH: SOH (0.5 mL orally for 14 days) Treatment duration: 14 days | Histological changes | SOH significantly restored all disturbed histologic parameters SOH ↓ glomerular diameter | [78] |
| Ginseng | Korean red ginseng extract (KRG) |
Mice Eight groups VH: olive oil (5 mL/kg, SC daily) and oral sterile water for 4 weeks VH+KRG 0.2: Olive oil (5 mL/kg, SC) + KRG (0.2 g/kg, orally) for 4 weeks VH+KRG 0.4: Olive oil (5 mL/kg, SC) + KRG (0.4 g/kg, orally) for 4 weeks VH+KRG 0.8: Olive oil (5 mL/kg, SC) + KRG (0.8 g/kg, orally) for 4 weeks CA: CA (30 mg/kg, SC) and oral sterile water for 4 weeks CA+KRG 0.2: CA (30 mg/kg, SC) + KRG (0.2 g/kg, orally) for 4 weeks CA+KRG 0.4: CA (30 mg/kg, SC) + KRG (0.4 g/kg, orally) for 4 weeks CA+KRG 0.8: CA (30 mg/kg, SC) + KRG (0.8 g/kg, orally) for 4 weeks Treatment duration: 28 days |
Assessing renal function and pathology, mediators of inflammation, tubulointerstitial fibrosis, and apoptotic cell death Effect on proximal tubular cells (HK-2) by in vitro model Assessing 8-OHdG levels in 24 h urine, tissue sections, and culture media | KRG ↓ serum Cr and BUN KRG ↑Cr clearance KRG ↓ proinflammatory and profibrotic molecules as iNOs, cytokines, TGF-β1, and TGF-β1-inducible gene h3 and apoptotic cell death In vitro studies, KRG ↑ protection against CA-induced morphological changes, cytotoxicity, inflammation, and apoptotic cell death KRG ↓ 8-OHdG level in urine and culture supernatant | [79] |
| Black grape/garlic extract | Dried fruit (BG)/aqueous extract (GAE) | Sprague Dawley rats Six groups CA: CA (25 mg/kg/day, orally) for 10 days, with food supplementation (3 days before CA treatment and continued during the study period (13 days)) Control CA: CA (25 mg/kg/day, orally) for 10 days CA+ BG: BG (25 g/kg/day with diet) CA+GAE: GAE (20 mL/kg/day with drinking H2O) BG: BG (25 g/kg/day with diet) GAE: GAE (20 mL/kg/day with drinking H2O) Treatment duration: 13 days | Oxidant (XO and MDA) and antioxidant (SOD, GSH-Px, and CAT) enzymes Histopathological changes | BG and GAE produced no changes in XO, SOD, and GSH-Px activities BG and GAE ↓ MDA level and CAT activity BG and GAE ameliorated glomerular sclerosis tubular necrosis and interstitial fibrosis | [81] |
| Green tea | Lyophilized aqueous extract (GTE) | White male albino rats Four groups Control GTE: GTE (3 %W/V) for 9 weeks CA: CA (25 mg/kg/orally/day) for 21 days GTE+CA: GTAE (3% W/V) for 21 days before CA, then for 21 days concomitant with CA followed by 21 days later Treatment duration: 63 days | Serum glucose, TP, albumin, TC, TAGs, PLs, urea, UA, Cr, Na, K, inorganic phosphorus, LDH, GGT. MDA, GSH, NO, TAO, CAT, SOD, and GPX | GTE improve renal function and ↓ peroxidative levels GTE ↑ renal tissues antioxidant by enhancing CAT, SOD, GPX, and TAC activities GTE restored elevated glucose, lipid profile, urea, UA, Cr, LDH, and GGT. GTE reversed ↑ in serum proteins and electrolyte to normal range | [82] |
| Lyophilized aqueous extract | Sprague Dawley rats Six groups Control CA: CA (20 mg/kg/day, I.P.) for 21 days GTE0.5+CA: GTE (0.5% with drinking water, 4 days before and 21 days concurrently with CA GTE0.5+CA: GTE (1% with drinking water, 4 days before and 21 days concurrently with CA GTE0.5+CA: GTE (1.5% with drinking water, 4 days before and 21 days concurrently with CA GTE: GTE (1.5% with water) for 25 days Treatment duration: 21 days | Glucose, Cr, BUN, serum UA, and Cr levels GSH and TBARS Enzyme activities: CAT, SOD, GPx, GR, GST, NAG, β-GU, and AP | GTE prevented TBARS regeneration GTE ↓ CA-induced renal dysfunction as indicated by ↓ serum Cr, BUN, UA, and urinary excretion of glucose GTE ↑ reduced glutathione content and activity of antioxidant enzymes in the kidney homogenate GTE ↓ activity of lysosomal enzymes; NAG and AP | [83] | |
| Propolis | Ethanol extract | Sprague Dawley rats Four groups Control: no supplement CA: CA (15 mg/kg/day SC) Propolis (100 mg/kg/day, gavage) CA+Propolis: CA (15 mg/kg/day SC) + Propolis (100 mg/kg/day, gavage) Treatment duration: 21 days | Serum cortisol, glucose, albumin, globulin, TP, urea, TAGs, HDL, VLDL, LDL, TC, Cr, AST, and ALT values | Propolis ↓ improved CA-induced BW reduction Propolis ↓ cortisol, AST, ALT, urea, and MDA levels in kidney Propolis ↑ CAT and GSH activities | [84] |
| Spirulina (algae, Arthrospira platensis) | Male Sprague Dawley rats Eight groups Control R: single dose of whole-body gamma irradiation (6.5 Gy) CA: CA (25 mg/kg, I.P.) for 10 days CA+R: CA for 10 days, then exposed to gamma radiation on the last day Sp: Sp (1 g/kg, intragastric gavages for 15 consecutive days) Sp+R: Sp for 15 days before irradiation Sp+CA: Sp for 5 days before and 10 days concomitant with CA Sp+CA+R: Sp for 5 days before and 10 days concomitant with CA injection and exposed to gamma radiation Treatment duration: 15 days | Serum creatinine, urea, glucose, albumin, protein, and lipid profile as well as GSH, TBARS, nitrite, and SOD activities Trace elements (Zn and Mg) Caspase-3 expression Histopathological changes | Sp ↓ serum creatinine, urea, and glucose levels of CA-administrated rats Treatment of irradiated CA- administrated rats with Sp ↓ serum creatinine and urea Sp ↓ serum albumin and protein levels of R group (20 and 17%, respectively), CA group (20 and 13%, respectively), and CA + R group (28 and 21%, respectively) Sp ↓ Zn and ↑ Mg content of kidney | [85] | |
| Cordyceps cynensis (CS) | Pharmaceutical product | Concurrent administration of Cordyceps sinensis in CA-treated kidney-transplanted recipients. Each recipient was given CA (5 mg/kg/day for 15 days) Control: placebo (glucose) 3 g CS: Cordyceps sinensis 3g simultaneously Treatment duration: 15 days | Blood creatinine, urea, and NAG | SC ↓ creatinine, urea, and NAG SC protected the proximal tubular function and ameliorated renal hemodynamics | [86] |
| Fennel, carob, doum (FE, CA, DO) | Powdered FE seeds, CA pods, and DO fruit (17, 18, and 21 g/kg, respectively) were added to the experimental animal’s diet | Female Sprague Dawley rats Six groups Control: injected with corn oil daily for 7 days CA: CA (50 mg/kg/day in corn oil for 1 week) CA+FE, CA, and DO: injected CA for 7 days then FE, CA, and DO and mixture of them was added to the diet of these groups, respectively Treatment duration: 45 days | Creatinine levels in serum and urinary samples, serum ammonia, TGF-β, TNFα, NAG, and β2MG Histopathological examination | FE, CA, and DO mixture ↓ serum creatinine, urinary creatinine, and serum ammonia levels They ↑ creatinine clearance They ↓ urinary β2MG and NAG activity and ↓ levels of serum TNF-α and TGF-β They significantly ameliorated functions and morphological structure of the kidney | [87] |
| Ipomea batates (LB) | Aqueous extract | Male rats Four groups Control: distilled water for 2 weeks, then olive oil, I.P. for 21 days CA: distilled water for 2 weeks, then CA (25 mg/kg, I.P. in olive oil/21 days) LB200 + CA: LB 200 mg/kg, orally) for 21 days, then CA LB400 + CA: LB 400 mg/kg, orally) for 21 days, then CA Treatment duration: 21 days | Oxidative stress biomarkers (MDA and SOD) Cytokines (IL-1β and TNF-α) Kidney function (BUN, UA, Cr) Na+ and K+serum levels Histopathological studies | LB ↓MDA and ↑SOD activity LB ↓ TNF-α and IL1-β LB ↓ BUN, UA, and Cr LB ↑ ionic Na+ level and ↑ ionic K+ level | [88] |
| Nigella sativa oil (NSO) | Fixed oil | Male Wistar albino rats Four groups Control: sunflower oil (2 mL/kg/day, orally) NSO: NSO (2 mL/kg orally/21 days) CA: CA (25 mg/kg, orally/21 days) CA + NSO: NSO (2 mL/kg orally) since the first day, while CA (25 mg/kg orally) for the last 21 days Treatment duration: 21 days | Urine and serum Cr levels Total (Cu-Zn, Mn) SOD activities CAT, GSH-Px, and MDA Kidney nitrite and nitrate levels | No significant amelioration of Cr levels and SOD activities for groups CA with NSO NSO ↑ GSH-Px level NSO ↓ MDA and NO levels | [89] |
| Schisandrae chinensis (SCE) | Fruit 95% alcohol extract | Male Sprague Dawley rats Seven groups Vehicle: olive oil (10 mL/kg) for 14 days CA: CA (50 mg/kg) for 3 days CA + SCE: 50 mg/kg CA + 216 mg/kg SCE for 3 days CA group: 50 mg/kg CA for 7 days CA + SCE: 50 mg/kg CA + 216 mg/kg SCE for 7 days CA: 50 mg/kg CA for 14 days CA + SCE: 50 mg/kg CA + 216 mg/kg SCE for 14 days Treatment duration: 14 days | Cre and BUN GSH, CAT, MDA, and SOD Pathologic manifestations | SCE ↓ CRE and BUN levels SCE ↑ GSH, CAT, and SOD and ↓ MDA In the 14-day group, no glomerular balloon occlusions or vacuolar lesions were observed, and the tissues presented good renal characteristics | [90] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibrahim, S.R.M.; Abdallah, H.M.; El-Halawany, A.M.; Mohamed, G.A.; Alhaddad, A.A.; Samman, W.A.; Alqarni, A.A.; Rizq, A.T.; Ghazawi, K.F.; El-Dine, R.S. Natural Reno-Protective Agents against Cyclosporine A-Induced Nephrotoxicity: An Overview. Molecules 2022, 27, 7771. https://doi.org/10.3390/molecules27227771
Ibrahim SRM, Abdallah HM, El-Halawany AM, Mohamed GA, Alhaddad AA, Samman WA, Alqarni AA, Rizq AT, Ghazawi KF, El-Dine RS. Natural Reno-Protective Agents against Cyclosporine A-Induced Nephrotoxicity: An Overview. Molecules. 2022; 27(22):7771. https://doi.org/10.3390/molecules27227771
Chicago/Turabian StyleIbrahim, Sabrin R. M., Hossam M. Abdallah, Ali M. El-Halawany, Gamal A. Mohamed, Aisha A. Alhaddad, Waad A. Samman, Ali A. Alqarni, Akaber T. Rizq, Kholoud F. Ghazawi, and Riham Salah El-Dine. 2022. "Natural Reno-Protective Agents against Cyclosporine A-Induced Nephrotoxicity: An Overview" Molecules 27, no. 22: 7771. https://doi.org/10.3390/molecules27227771









