Potential Anti-Inflammatory Effect of Rosmarinus officinalis in Preclinical In Vivo Models of Inflammation
Abstract
:1. Introduction
2. Results and Discussion
2.1. Animal Model
2.2. Plant/Compound and Extraction
2.3. Dose and Route of Administration
2.3.1. Gavage
2.3.2. Intraperitoneal
2.3.3. Oral
2.4. Frequency and Duration
2.5. Biomarkers Evaluated
3. Materials and Methods
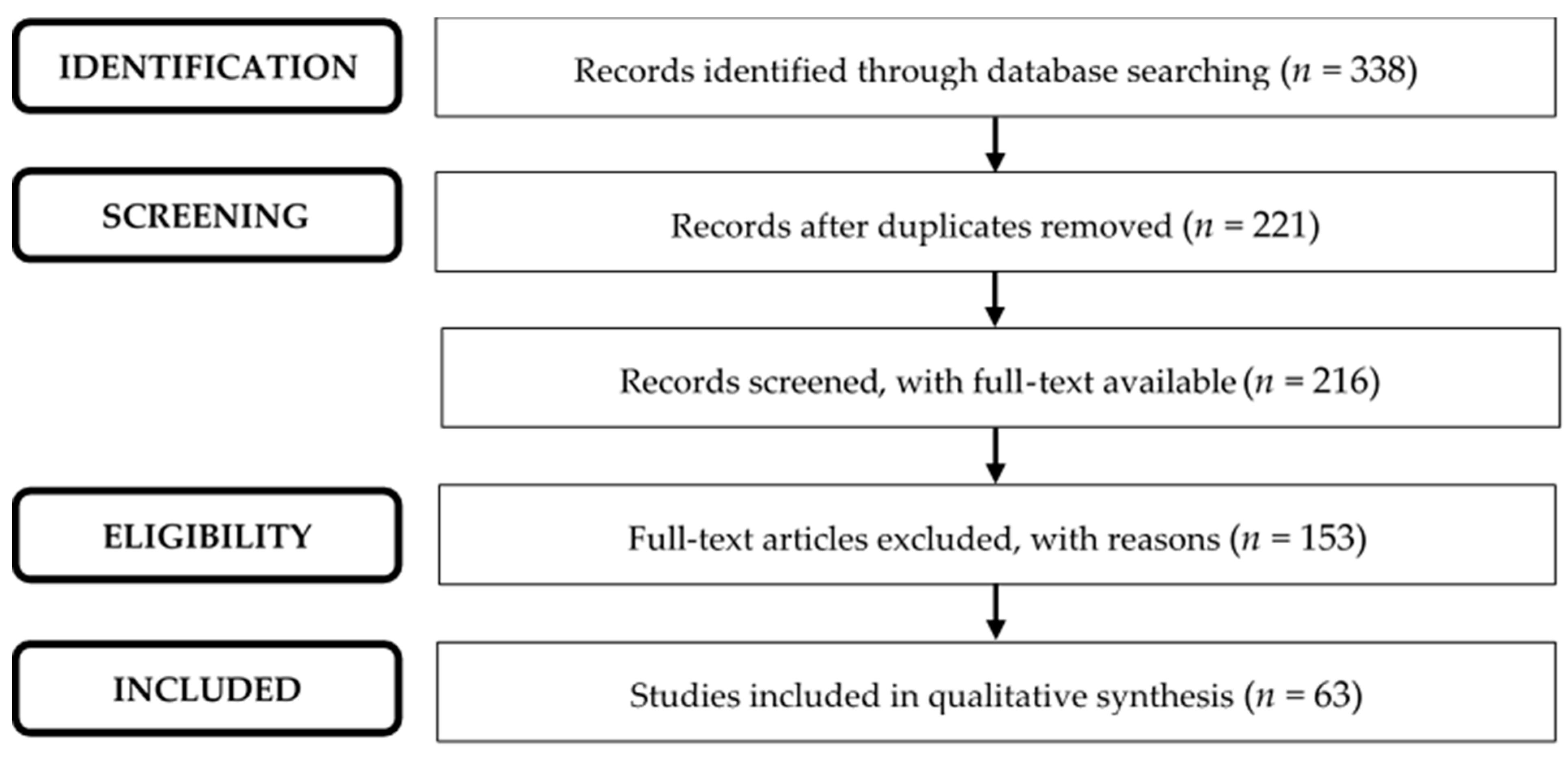
3.1. Search Strategy
3.2. Selection of Studies
3.3. Data Extraction
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Andrade, J.M.; Faustino, C.; Garcia, C.; Ladeiras, D.; Reis, C.P.; Rijo, P. Rosmarinus officinalis L.: An update review of its phytochemistry and biological activity. Future Sci. OA 2018, 4, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Farkhondeh, T.; Samarghandian, S.; Pourbagher-Shahri, A.M. Hypolipidemic effects of Rosmarinus officinalis L. J. Cell Physiol. 2019, 234, 14680–14688. [Google Scholar] [CrossRef]
- Ahmed, H.M.; Babakir-Mina, M. Investigation of rosemary herbal extracts (Rosmarinus officinalis) and their potential effects on immunity. Phyther. Res. 2020, 34, 1829–1837. [Google Scholar] [CrossRef]
- de Oliveira, J.R.; Camargo, S.E.A.; de Oliveira, L.D. Rosmarinus officinalis L. (rosemary) as therapeutic and prophylactic agent. J. Biomed. Sci. 2019, 26, 5. [Google Scholar] [CrossRef]
- Patil, K.R.; Mahajan, U.B.; Unger, B.S.; Goyal, S.N.; Belemkar, S.; Surana, S.J.; Ojha, S.; Patil, C.R. Animal models of inflammation for screening of anti-inflammatory drugs: Implications for the discovery and development of phytopharmaceuticals. Int. J. Mol. Sci. 2019, 20, 4367. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Sun, J.-J.; Chen, G.-Y.; Wang, W.-W.; Xie, Z.-T.; Tang, G.-F.; Wei, S.-D. Carnosic acid nanoparticles suppress liver ischemia/reperfusion injury by inhibition of ROS, Caspases and NF-κB signaling pathway in mice. Biomed. Pharmacother. 2016, 82, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Liu, L.; Sun, H.; Cao, K. Carnosic acid protects against lipopolysaccharide-induced acute lung injury in mice. Exp. Ther. Med. 2019, 18, 3707–3714. [Google Scholar] [CrossRef]
- Song, H.-M.; Li, X.; Liu, Y.-Y.; Lu, W.-P.; Cui, Z.-H.; Zhou, L.; Yao, D.; Zhang, H.-M. Carnosic acid protects mice from high-fat diet-induced NAFLD by regulating MARCKS. Int. J. Mol. Med. 2018, 42, 193–207. [Google Scholar] [CrossRef] [Green Version]
- Tang, B.; Tang, F.; Wang, Z.; Qi, G.; Liang, X.; Li, B.; Yuan, S.; Liu, J.; Yu, S.; He, S. Upregulation of Akt/Nf-κB-regulated inflammation and Akt/Bad-related apoptosis signaling pathway involved in hepatic carcinoma process: Suppression by carnosic acid nanoparticle. Int. J. Nanomed. 2016, 11, 6401–6420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, L.; Shan, W.; Zeng, W.; Hu, Y.; Wang, G.; Tian, X.; Zhang, N.; Shi, X.; Zhao, Y.; Ding, C.; et al. Carnosic acid alleviates chronic alcoholic liver injury by regulating the SIRT1/ChREBP and SIRT1/p66shc pathways in rats. Mol. Nutr. Food Res. 2016, 60, 1902–1911. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.-L.; Yang, J.-J.; Zhang, H.-S. Carvedilol (CAR) combined with carnosic acid (CAA) attenuates doxorubicin-induced cardiotoxicity by suppressing excessive oxidative stress, inflammation, apoptosis and autophagy. Biomed. Pharmacother. 2019, 109, 71–83. [Google Scholar] [CrossRef]
- Xia, G.; Wang, X.; Sun, H.; Qin, Y.; Fu, M. Carnosic acid (CA) attenuates collagen-induced arthritis in db/db mice via inflammation suppression by regulating ROS-dependent p38 pathway. Free Radic. Biol. Med. 2017, 108, 418–432. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Zhou, X.; Zhou, L.; Liu, Z.; Yuan, J.; Cheng, J.; Zhao, J.; Wu, L.; Li, H.; Qiu, H.; et al. Carnosic acid inhibits inflammation response and joint destruction on osteoclasts, fibroblast-like synoviocytes, and collagen-induced arthritis rats. J. Cell Physiol. 2018, 233, 6291–6303. [Google Scholar] [CrossRef]
- Park, M.-Y.; Sung, M.-K. Carnosic acid attenuates obesity-induced glucose intolerance and hepatic fat accumulation by modulating genes of lipid metabolism in C57BL/6J-ob/ob mice. J. Sci. Food Agric. 2015, 95, 828–835. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, Y.; Hu, M.; Li, Y.-H.; Cao, X.-H. Carnosic acid alleviates brain injury through NF-κB-regulated inflammation and Caspase-3-associated apoptosis in high fat-induced mouse models. Mol. Med. Rep. 2019, 20, 495–504. [Google Scholar] [CrossRef] [Green Version]
- Xiang, Q.; Liu, Z.; Wang, Y.; Xiao, H.; Wu, W.; Xiao, C.; Liu, X. Carnosic acid attenuates lipopolysaccharide-induced liver injury in rats via fortifying cellular antioxidant defense system. Food Chem. Toxicol. 2013, 53, 1–9. [Google Scholar] [CrossRef]
- Mengoni, E.S.; Vichera, G.; Rigano, L.A.; Rodriguez-Puebla, M.L.; Galliano, S.R.; Cafferata, E.E.; Pivetta, O.H.; Moreno, S.; Vojnov, A.A. Suppression of COX-2, IL-1β and TNF-α expression and leukocyte infiltration in inflamed skin by bioactive compounds from Rosmarinus officinalis L. Fitoterapia 2011, 82, 414–421. [Google Scholar] [CrossRef]
- Takaki, I.; Bersani-Amado, L.E.; Vendruscolo, A.; Sartoretto, S.M.; Diniz, S.P.; Bersani-Amado, C.A.; Cuman, R.K.N. Anti-inflammatory and antinociceptive effects of Rosmarinus officinalis L. essential oil in experimental animal models. J. Med. Food 2008, 11, 741–746. [Google Scholar] [CrossRef]
- de Oliveira E Silva, A.M.; Machado, I.D.; Santin, J.R.; Pereira de Melo, I.L.; Pedrosa, G.V.; Genovese, M.I.; Farsky, S.H.P.; Mancini-Filho, J. Aqueous extract of Rosmarinus officinalis L. inhibits neutrophil influx and cytokine secretion. Phyther. Res. 2015, 29, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Goncalves, G.A.; Sa-Nakanishi, A.B.D.; Comar, J.F.; Bracht, L.; Dias, M.I.; Barros, L.; Peralta, R.M.; Ferreira, I.C.F.R.; Bracht, A. Water soluble compounds of Rosmarinus officinalis L. improve the oxidative and inflammatory states of rats with adjuvant-induced arthritis. Food Funct. 2018, 9, 2328–2340. [Google Scholar] [CrossRef] [PubMed]
- Amaral, G.P.; Dobrachinski, F.; de Carvalho, N.R.; Barcelos, R.P.; da Silva, M.H.; Lugokenski, T.H.; Dias, G.R.M.; Portella, R.L.; Fachinetto, R.; Soares, F.A.A. Multiple mechanistic action of Rosmarinus officinalis L. extract against ethanol effects in an acute model of intestinal damage. Biomed. Pharmacother. 2018, 98, 454–459. [Google Scholar] [CrossRef] [PubMed]
- Amaral, G.P.; de Carvalho, N.R.; Barcelos, R.P.; Dobrachinski, F.; Portella, R.L.; da Silva, M.H.; Lugokenski, T.H.; Dias, G.R.M.; da Luz, S.C.A.; Boligon, A.A.; et al. Protective action of ethanolic extract of Rosmarinus officinalis L. in gastric ulcer prevention induced by ethanol in rats. Food Chem. Toxicol. 2013, 55, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.-H.; Chuang, L.-T.; Lien, T.-J.; Liing, Y.-R.; Chen, W.-Y.; Tsai, P.-J. Rosmarinus officinalis extract suppresses propionibacterium acnes-induced inflammatory responses. J. Med. Food 2013, 16, 324–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahbardar, M.G.; Amin, B.; Mehri, S.; Mirnajafi-Zadeh, S.J.; Hosseinzadeh, H. Effect of alcoholic extract of aerial parts of Rosmarinus officinalis L. on pain, inflammation and apoptosis induced by chronic constriction injury (CCI) model of neuropathic pain in rats. J. Ethnopharmacol. 2016, 194, 117–130. [Google Scholar] [CrossRef]
- Yang, L.; Liu, X.; Cheng, D.; Fang, X.; Mu, M.; Hu, X.; Nie, L. Inhibition of bleomycin-induced pulmonary fibrosis by extract from Rosmarinus officinalis in rats. Int. J. Clin. Exp. Med. 2016, 9, 6054–6061. [Google Scholar]
- Borges, R.S.; Lima, E.S.; Keita, H.; Ferreira, I.M.; Fernandes, C.P.; Cruz, R.A.S.; Duarte, J.L.; Vélázquez-Moyado, J.; Ortiz, B.L.S.; Castro, A.N.; et al. Anti-inflammatory and antialgic actions of a nanoemulsion of Rosmarinus officinalis L. essential oil and a molecular docking study of its major chemical constituents. Inflammopharmacology 2018, 26, 183–195. [Google Scholar] [CrossRef]
- Guo, Y.; Xie, J.; Li, X.; Yuan, Y.; Zhang, L.; Hu, W.; Luo, H.; Yu, H.; Zhang, R. Antidepressant Effects of Rosemary Extracts Associate with Anti-inflammatory Effect and Rebalance of Gut Microbiota. Front. Pharmacol. 2018, 9, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Draganova-Filipova, M.; Apostolova, E.; Zagorchev, P. Effects of Rosmarinus officinalis oil on histamine-induced acute inflammation. C. R. Acad. Bulg. Sci. 2018, 71, 261–270. [Google Scholar]
- Inoue, K.-I.; Takano, H.; Shiga, A.; Fujita, Y.; Makino, H.; Yanagisawa, R.; Ichinose, T.; Kato, Y.; Yamada, T.; Yoshikawa, T. Effects of volatile constituents of a rosemary extract on allergic airway inflammation related to house dust mite allergen in mice. Int. J. Mol. Med. 2005, 16, 315–319. [Google Scholar] [CrossRef]
- Juhás, Š.; Bukovská, A.; Čikoš, Š.; Czikková, S.; Fabian, D.; Koppel, J. Anti-inflammatory effects of Rosmarinus officinalis essential oil in mice. Acta Vet. Brno 2009, 78, 121–127. [Google Scholar] [CrossRef] [Green Version]
- Medicherla, K.; Ketkar, A.; Sahu, B.D.; Sudhakar, G.; Sistla, R. Rosmarinus officinalis L. extract ameliorates intestinal inflammation through MAPKs/NF-κB signaling in a murine model of acute experimental colitis. Food Funct. 2016, 7, 3233–3243. [Google Scholar] [CrossRef]
- Khezri, K.; Farahpour, M.R.; Rad, S.M. Accelerated infected wound healing by topical application of encapsulated Rosemary essential oil into nanostructured lipid carriers. Artif. Cells Nanomed. Biotechnol. 2019, 47, 980–988. [Google Scholar] [CrossRef] [Green Version]
- de Melo, G.A.N.; Grespan, R.; Fonseca, J.P.; Farinha, T.O.; Silva, E.L.; Romero, A.L.; Bersani-Amado, C.A.; Cuman, R.K.N. Rosmarinus officinalis L. Essential Oil Inhibits In Vivo and In Vitro Leukocyte Migration. J. Med. Food. 2011, 14, 944–949. [Google Scholar] [CrossRef]
- Elbahnasawy, A.S.; Valeeva, E.R.; El-Sayed, E.M.; Rakhimov, I.I. The Impact of Thyme and Rosemary on Prevention of Osteoporosis in Rats. J. Nutr. Metab. 2019, 2019, 1431384. [Google Scholar] [CrossRef] [Green Version]
- de Faria, L.R.D.; Lima, C.L.; Perazzo, F.F.; Carvalho, J.C.T. Anti-inflammatory and antinociceptive activities of the essential oil from Rosmarinus Officinalis L. (lamiaceae). Int. J. Pharm. Sci. Rev. Res. 2011, 7, 1–8. [Google Scholar]
- Grigore, A.; Pirvu, L.; Bubueanu, C.; Panteli, M.; Rasit, I. Influence of chemical composition on the antioxidant and anti-inflammatory activity of Rosmarinus officinalis extracts. Rom. Biotechnol. Lett. 2015, 20, 10047–10054. [Google Scholar]
- Roohbakhsh, Y.; Rahimi, V.B.; Silakhori, S.; Rajabi, H.; Rahmanian-Devin, P.; Samzadeh-Kermani, A.; Rakhshandeh, H.; Hasanpour, M.; Iranshahi, M.; Mousavi, S.H.; et al. Evaluation of the Effects of Peritoneal Lavage with Rosmarinus officinalis Extract against the Prevention of Postsurgical-Induced Peritoneal Adhesion. Planta Med. 2020, 86, 405–414. [Google Scholar] [CrossRef] [PubMed]
- Rocha, J.; Eduardo-Figueira, M.; Barateiro, A.; Fernandes, A.; Brites, D.; Bronze, R.; Duarte, C.M.M.; Serra, A.T.; Pinto, R.; Freitas, M.; et al. Anti-inflammatory effect of rosmarinic acid and an extract of Rosmarinus officinalis in rat models of local and systemic inflammation. Basic Clin. Pharmacol. Toxicol. 2015, 116, 398–413. [Google Scholar] [CrossRef] [PubMed]
- Lucarini, R.; Bernardes, W.A.; Ferreira, D.S.; Tozatti, M.G.; Furtado, R.; Bastos, J.K.; Pauletti, P.M.; Januário, A.H.; Silva, M.L.A.; Cunha, W.R. In vivo analgesic and anti-inflammatory activities of Rosmarinus officinalis aqueous extracts, rosmarinic acid and its acetyl ester derivative. Pharm. Biol. 2013, 51, 1087–1090. [Google Scholar] [CrossRef] [Green Version]
- Bacanlı, M.; Aydın, S.; Taner, G.; Göktaş, H.G.; Şahin, T.; Başaran, A.A.; Başaran, N. Does rosmarinic acid treatment have protective role against sepsis-induced oxidative damage in Wistar Albino rats? Hum. Exp. Toxicol. 2015, 35, 877–886. [Google Scholar] [CrossRef]
- Chu, X.; Ci, X.; He, J.; Jiang, L.; Wei, M.; Cao, Q.; Guan, M.; Xie, X.; Deng, X.; He, J. Effects of a Natural Prolyl Oligopeptidase Inhibitor, Rosmarinic Acid, on Lipopolysaccharide-Induced Acute Lung Injury in Mice. Molecules 2012, 17, 3586–3598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eftekhar, N.; Moghimi, A.; Boskabady, M.H. Prophylactic effect of rosmarinic acid on tracheal responsiveness, white blood cell count and oxidative stress markers in lung lavage of sensitized rats. Pharmacol. Rep. 2018, 70, 119–125. [Google Scholar] [CrossRef]
- Sotnikova, R.; Okruhlicova, L.; Vlkovicova, J.; Navarova, J.; Gajdacova, B.; Pivackova, L.; Fialova, S.; Krenek, P. Rosmarinic acid administration attenuates diabetes-induced vascular dysfunction of the rat aorta. J. Pharm. Pharmacol. 2013, 65, 713–723. [Google Scholar] [CrossRef]
- Shakeri, F.; Eftekhar, N.; Roshan, N.M.; Rezaee, R.; Moghimi, A.; Boskabady, M.H. Rosmarinic acid affects immunological and inflammatory mediator levels and restores lung pathological features in asthmatic rats. Allergol. Immunopathol. 2019, 47, 16–23. [Google Scholar] [CrossRef]
- Domitrović, R.; Škoda, M.; Marchesi, V.V.; Cvijanović, O.; Pugel, E.P.; Štefan, M.B. Rosmarinic acid ameliorates acute liver damage and fibrogenesis in carbon tetrachloride-intoxicated mice. Food Chem. Toxicol. 2013, 51, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Hashiesh, H.M.; Elkhoely, A.A.; Eissa, A.A.; Youns, M.M. Rosmarinic acid enhances cisplatin cytotoxicity in hepg2 cell line and attenuates its nephrotoxicity in mice. Int. J. Pharm. Sci. Res. 2018, 9, 2731–2743. [Google Scholar] [CrossRef]
- Cao, W.; Hu, C.; Wu, L.; Xu, L.; Jiang, W. Rosmarinic acid inhibits inflammation and angiogenesis of hepatocellular carcinoma by suppression of NF-κB signaling in H22 tumor-bearing mice. J. Pharmacol. Sci. 2016, 132, 131–137. [Google Scholar] [CrossRef] [Green Version]
- Yao, Y.; Mao, J.; Xu, S.; Zhao, L.; Long, L.; Chen, L.; Li, D.; Lu, S. Rosmarinic acid inhibits nicotine-induced C-reactive protein generation by inhibiting NLRP3 inflammasome activation in smooth muscle cells. J. Cell Physiol. 2019, 234, 1758–1767. [Google Scholar] [CrossRef]
- Cao, W.; Mo, K.; Wei, S.; Lan, X.; Zhang, W.; Jiang, W. Effects of rosmarinic acid on immunoregulatory activity and hepatocellular carcinoma cell apoptosis in H22 tumor-bearing mice. Korean J. Physiol. Pharmacol. 2019, 23, 501–508. [Google Scholar] [CrossRef] [Green Version]
- Jin, B.-R.; Chung, K.-S.; Cheon, S.-Y.; Lee, M.; Hwang, S.; Hwang, S.N.; Rhee, K.-J.; An, H.-J. Rosmarinic acid suppresses colonic inflammation in dextran sulphate sodium (DSS)-induced mice via dual inhibition of NF-κB and STAT3 activation. Sci. Rep. 2017, 7, 46252. [Google Scholar] [CrossRef] [PubMed]
- Shang, A.-J.; Yang, Y.; Wang, H.-Y.; Tao, B.-Z.; Wang, J.; Wang, Z.-F.; Zhou, D.-B. Spinal cord injury effectively ameliorated by neuroprotective effects of rosmarinic acid. Nutr. Neurosci. 2017, 20, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Nie, H.; Xu, Y.; Peng, J.; Zeng, Y.; Wei, Y.; Wen, X.; Qiu, J.; Zhong, W.; Deng, X.; et al. Therapeutic effects of rosmarinic acid on airway responses in a murine model of asthma. Int. Immunopharmacol. 2016, 41, 90–97. [Google Scholar] [CrossRef]
- Jiang, K.; Ma, X.; Guo, S.; Zhang, T.; Zhao, G.; Wu, H.; Wang, X.; Deng, G. Anti-inflammatory Effects of Rosmarinic Acid in Lipopolysaccharide-Induced Mastitis in Mice. Inflammation 2018, 41, 437–448. [Google Scholar] [CrossRef] [PubMed]
- Budhiraja, A.; Dhingra, G. Development and characterization of a novel antiacne niosomal gel of rosmarinic acid. Drug Deliv. 2015, 22, 723–730. [Google Scholar] [CrossRef] [Green Version]
- Cin, B.; Ciloglu, N.S.; Omar, S.; Terzi, N.K. Effect of Rosmarinic Acid and Alcohol on Fat Graft Survival in Rat Model. Aesth. Plast. Surg. 2020, 44, 177–185. [Google Scholar] [CrossRef]
- Zych, M.; Kaczmarczyk-Sedlak, I.; Wojnar, W.; Folwarczna, J. Effect of Rosmarinic Acid on the Serum Parameters of Glucose and Lipid Metabolism and Oxidative Stress in Estrogen-Deficient Rats. Nutrients 2019, 11, 267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hasanein, P.; Seifi, R. Beneficial effects of rosmarinic acid against alcohol-induced hepatotoxicity in rats. Can. J. Physiol. Pharmacol. 2018, 96, 32–37. [Google Scholar] [CrossRef]
- Joardar, S.; Dewanjee, S.; Bhowmick, S.; Dua, T.K.; Das, S.; Saha, A.; de Feo, V. Rosmarinic acid attenuates cadmium-induced nephrotoxicity via inhibition of oxidative stress, apoptosis, inflammation and fibrosis. Int. J. Mol. Sci. 2019, 20, 2027. [Google Scholar] [CrossRef] [Green Version]
- Areti, A.; Komirishetty, P.; Kalvala, A.K.; Nellaiappan, K.; Kumar, A. Rosmarinic Acid Mitigates Mitochondrial Dysfunction and Spinal Glial Activation in Oxaliplatin-induced Peripheral Neuropathy. Mol. Neurobiol. 2018, 55, 7463–7475. [Google Scholar] [CrossRef]
- Ozdemir, D.; Agri, I.; Bakirtas, M.; Agri, A.; Mehel, D.M.; Celebi, M.; Ozgur, A. The effect of rosmarinic acid on the prevention of myringosclerosis. Int. J. Pediatr. Otorhinolaryngol. 2019, 126, 109597. [Google Scholar] [CrossRef]
- Rahbardar, M.G.; Amin, B.; Mehri, S.; Mirnajafi-Zadeh, S.J.; Hosseinzadeh, H. Anti-inflammatory effects of ethanolic extract of Rosmarinus officinalis L. and rosmarinic acid in a rat model of neuropathic pain. Biomed. Pharmacother. 2017, 86, 441–449. [Google Scholar] [CrossRef]
- Emami, F.; Ali-Beig, H.; Farahbakhsh, S.; Mojabi, N.; Rastegar-Moghadam, B.; Arbabian, S.; Kazemi, M.; Tekieh, E.; Golmanesh, L.; Ranjbaran, M.; et al. Hydroalcoholic extract of rosemary (Rosmarinus officinalis L.) and its constituent carnosol inhibit formalin-induced pain and Inflammation in mice. Pakistan J. Biol. Sci. 2013, 16, 309–316. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.Y.; Hwang, C.J.; Choi, J.Y.; Park, M.H.; Song, M.J.; Oh, K.W.; Son, D.J.; Lee, S.H.; Han, S.B.; Hong, J.T. Inhibitory Effect of Carnosol on Phthalic Anhydride-Induced Atopic Dermatitis via Inhibition of STAT3. Biomol. Ther. 2017, 25, 535–544. [Google Scholar] [CrossRef] [Green Version]
- Li, X.; Zhao, L.; Han, J.-J.; Zhang, F.; Liu, S.; Zhu, L.; Wang, Z.-Z.; Zhang, G.-X.; Zhang, Y. Carnosol modulates Th17 cell differentiation and microglial switch in experimental autoimmune encephalomyelitis. Front. Immunol. 2018, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Z.-H.; Xie, Y.-X.; Zhang, J.-W.; Qiu, X.-H.; Cheng, A.-B.; Tian, L.; Ma, B.-Y.; Hou, Y.-B. Carnosol protects against spinal cord injury through Nrf-2 upregulation. J. Recept. Signal Transduct. 2016, 36, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Zhang, Y.; Zheng, Y.; Zhang, N. Carnosol protects against renal ischemia-reperfusion injury in rats. Exp. Anim. 2018, 67, 545–553. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeo, I.J.; Park, J.H.; Jang, J.S.; Lee, D.Y.; Park, J.E.; Choi, Y.E.; Joo, J.H.; Song, J.K.; Jeon, H.O.; Hong, J.T. Inhibitory effect of Carnosol on UVB-induced inflammation via inhibition of STAT3. Arch. Pharm. Res. 2019, 42, 274–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- da Rosa, J.S.; Facchin, B.M.; Bastos, J.; Siqueira, M.A.; Micke, G.A.; Dalmarco, E.M.; Pizzolatti, M.G.; Frode, T.S. Systemic administration of Rosmarinus officinalis attenuates the inflammatory response induced by carrageenan in the mouse model of pleurisy. Planta Med. 2013, 79, 1605–1614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Babu, N.P.; Pandikumar, P.; Ignacimuthu, S. Anti-inflammatory activity of Albizia lebbeck Benth, an ethnomedicinal plant, in acute and chronic animal models of inflammation. J. Ethnopharmacol. 2009, 125, 356–360. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, H.; Shimizu, M. Early and delayed phases of hind paw edema in rats. Jpn. J. Pharmacol. 1974, 24, 393–405. [Google Scholar] [CrossRef] [Green Version]
- Moreno, J.J. Effect of aristolochic acid on arachidonic acid cascade and in vivo models of inflammation. Immunopharmacology 1993, 26, 1–9. [Google Scholar] [CrossRef]
- Gupta, M.; Mazumder, U.K.; Kumar, R.S.; Gomathi, P.; Rajeshwar, Y.; Kakoti, B.B.; Selven, V.T. Anti-inflammatory, analgesic and antipyretic effects of methanol extract from Bauhinia racemosa stem bark in animal models. J. Ethnopharmacol. 2005, 98, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Boominathan, R.; Parimaladevi, B.; Mandal, S.C.; Ghoshal, S.K. Anti-inflammatory evaluation of Ionidium suffruticosam Ging. in rats. J. Ethnopharmacol. 2004, 91, 367–370. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Bani, S.; Gupta, D.K.; Chandan, B.K.; Kaul, A. Anti-inflammatory activity of “TAF” an active fraction from the plant Barleria prionitis Linn. J. Ethnopharmacol. 2003, 85, 187–193. [Google Scholar] [CrossRef]
- Panthong, A.; Norkaew, P.; Kanjanapothi, D.; Taesotikul, T.; Anantachoke, N.; Reutrakul, V. Anti-inflammatory, analgesic and antipyretic activities of the extract of gamboge from Garcinia hanburyi Hook f. J. Ethnopharmacol. 2007, 111, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Bas, E.; Recio, M.C.; Máñez, S.; Giner, R.M.; Escandell, J.M.; López-Ginés, C.; Rios, J.-L. New insight into the inhibition of the inflammatory response to experimental delayed-type hypersensitivity reactions in mice by scropolioside A. Eur. J. Pharmacol. 2007, 555, 199–210. [Google Scholar] [CrossRef]
- Bas, E.; Recio, M.C.; Abdallah, M.; Máñez, S.; Giner, R.M.; Cerdá-Nicolás, M.; Rios, J.-L. Inhibition of the pro-inflammatory mediators’ production and anti-inflammatory effect of the iridoid scrovalentinoside. J. Ethnopharmacol. 2007, 110, 419–427. [Google Scholar] [CrossRef]
- Boller, S.; Soldi, C.; Marques, M.C.A.; Santos, E.P.; Cabrini, D.A.; Pizzolatti, M.G.; Zampronio, A.R.; Otuki, M.F. Anti-inflammatory effect of crude extract and isolated compounds from Baccharis illinita DC in acute skin inflammation. J. Ethnopharmacol. 2010, 130, 262–266. [Google Scholar] [CrossRef]
- Inoue, H.; Mori, T.; Shibata, S.; Koshihara, Y. Modulation by glycyrrhetinic acid derivatives of TPA-induced mouse ear oedema. Br. J. Pharmacol. 1989, 96, 204–210. [Google Scholar] [CrossRef] [Green Version]
- Vasudevan, M.; Gunnam, K.K.; Parle, M. Antinociceptive and anti-inflammatory effects of Thespesia populnea bark extract. J. Ethnopharmacol. 2007, 109, 264–270. [Google Scholar] [CrossRef]
- Morris, C.J. Carrageenan-induced paw edema in the rat and mouse. In Methods in Molecular Biology; Springer: Berlin/Heidelberg, Germany, 2003; pp. 115–121. [Google Scholar]
- Sadeghi, H.; Parishani, M.; Touri, M.A.; Ghavamzadeh, M.; Barmak, M.J.; Zarezade, V.; Delaviz, H.; Sadeghi, H. Pramipexole reduces inflammation in the experimental animal models of inflammation. Immunopharmacol. Immunotoxicol. 2017, 39, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Panthong, A.; Kanjanapothi, D.; Taesotikul, T.; Wongcome, T.; Reutrakul, V. Anti-inflammatory and antipyretic properties of Clerodendrum petasites S. Moore. J. Ethnopharmacol. 2003, 85, 151–156. [Google Scholar] [CrossRef]
- Turner, P.V.; Brabb, T.; Pekow, C.; Vasbinder, M.A. Administration of substances to laboratory animals: Routes of administration and factors to consider. J. Am. Assoc. Lab Anim. Sci. 2011, 50, 600–613. [Google Scholar] [PubMed]
- Pahwa, R.; Goyal, A.; Bansal, P.; Jialal, I. Chronic Inflammation. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Cash, J.L.; White, G.E.; Greaves, D.R. Chapter 17—Zymosan-Induced Peritonitis as a Simple Experimental System for the Study of Inflammation. Methods Enzymol. 2009, 461, 379–396. [Google Scholar] [CrossRef]
- Yu, M.-H.; Choi, J.-H.; Chae, I.-G.; Im, H.-G.; Yang, S.-A.; More, K.; See, I.-S.; Lee, J. Suppression of LPS-induced inflammatory activities by Rosmarinus officinalis L. Food Chem. 2013, 136, 1047–1054. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Zou, L.; Sun, H.; Peng, J.; Gao, C.; Bao, L.; Ji, R.; Jin, Y.; Sun, S. A Review of the Anti-Inflammatory Effects of Rosmarinic Acid on Inflammatory Diseases. Front. Pharmacol. 2020, 11, 153. [Google Scholar] [CrossRef] [PubMed]
- Kunnumakkara, A.B.; Sailo, B.L.; Banik, K.; Harsha, C.; Prasad, S.; Gupta, S.C.; Bharti, A.C.; Aggarwal, B.B. Chronic diseases, inflammation, and spices: How are they linked? J. Transl. Med. 2018, 16, 14. [Google Scholar] [CrossRef] [Green Version]
| Plant/Compound | Extraction | Dose (mg/kg) | Animal Model | Route | Frequency/Duration | Biomarkers Evaluated | Reference |
|---|---|---|---|---|---|---|---|
| Carnosic acid | n.m. | 10, 20 | Acute liver injury | Injected | Daily, 5 d | TNF-α, IL-1β, IL-6, IL-18, IFN-γ, TGF-β, CAT, GPx, GSH, MDA, SOD | [6] |
| n.a. | 10–40 | Acute lung injury | IP | Single-dose | TNF-α, IL-1β, IL-6 | [7] | |
| 15, 30 | Non-alcoholic fatty liver disease | Oral | Daily, 8 wks | TNF-α, IL-1β, IL-2, IL-4, IL-6, IL-12, IL-18, IFN-γ | [8] | ||
| n.m. | 10, 20 | Hepatocarcinoma | IP | Daily, 4 wks | TNF-α, IL-1β, IL-2, IL-6, IL-10, IL-18, IFN-γ | [9] | |
| n.a. | 15, 30 | Cirrhosis | Gavage | Daily, 8 wks | TNF-α | [10] | |
| 5 | Cardiotoxicity | Daily, 6 d | TNF-α, IL-6, COX-2, CAT, GSH, MDA, SOD | [11] | |||
| 30, 60 | Arthritis | IP | Daily, 4 wks | TNF-α, IL-1β, IL-6, IL-17, IFN-γ, RANKL, MIP-1, GPx, MDA, SOD, ROS | [12] | ||
| 5 | Arthritis | 4 wk, 14 d | TNF-α, IL-1β, RANKL | [13] | |||
| 100, 200 | Diabetes and hepatic fat accumulation | Oral | Daily, 4 wks | TNF-α, IL-6 | [14] | ||
| 10, 20 | Brain injury | Gavage | Daily, 9 wks | TNF-α, IL-1β, IL-6, IL-18 | [15] | ||
| 15–60 | Acute liver injury | Daily, 35 d | TNF-α, IL-6, GPx, GSH, MDA, SOD, NO, iNOS | [16] | |||
| n.m. | Ear edema | Topical | Single-dose | TNF-α, IL-1β, COX-1, COX-2 | [17] | ||
| Rosmarinusofficinalis | Steam distillation | n.m. | Single-dose | Edema, leukocyte infiltration | |||
| 0.6 | Paw edema | Topical/Injected | Single-dose | Edema, leukocyte infiltration | |||
| 250–750 | Paw edema | Gavage | Single-dose | Edema | [18] | ||
| 125–500 | Pleurisy | Single-dose | Volume of exudate, migrated cells | ||||
| Aqueous maceration | 100–400 | Subcutaneous edema | Single-dose | Neutrophil infiltration, TNF-α, IL-6, PGE-2, GPx, SOD | [19] | ||
| Aqueous maceration | 150 | Arthritis | Daily, 23 d | Edema, leukocyte infiltration, MPO, CAT, GPx, GSH, GSSG, GR, SOD, ROS | [20] | ||
| Rosmarinus officinalis | Ethanolic Soxhlet extraction | 500, 1000 | Acute intestinal injury | Gavage | Daily, 3 d | MPO, CAT, GSH, GSSG, MDA, SOD | [21] |
| 500, 1000 | Gastric ulcer | Daily, 3 d | MPO, CAT, GSH/GSSG ratio, MDA, NOx, SOD | [22] | |||
| Ethanolic maceration | 50 | Ear edema | ID | Single-dose | Edema, neutrophil infiltration | [23] | |
| 100–400 | Neuropathic pain | IP | Daily, 14 d | TNF-α, Iba-1, iNOS | [24] | ||
| n.a. | 50–200 | Pulmonary fibrosis | Gavage | Daily, 28 d | TGF-β | [25] | |
| 100, 300 | Paw edema | Single-dose | Edema | [26] | |||
| 100 | Inflammation in hippocampus | Daily, 21 d | TNF-α, IL-1β, Iba-1, NF-κB | [27] | |||
| 35, 70 | Paw edema | IP | Single-dose | Edema | [28] | ||
| 0.46, 2.3 | Asthma | IT | Daily | IL-5, IL-13, MIP-1 | [29] | ||
| 1250–5000 | Paw edema | Oral | Daily, 15 d | Edema, MPO | [30] | ||
| 1250–5000 | Colitis | Daily, 18 d | IL-1β, IL-6, MPO | ||||
| 50, 100 | Colitis | Gavage | Daily, 10 d | TNF-α, IL-6, MPO, NF-κB | [31] | ||
| n.m | n.m. | Infected cutaneous wounds | Topical | Daily, 13 d | IL-3, IL-10 | [32] | |
| Hydrodistillation | 125–500 | Internal spermatic fascia edema | Gavage | Single-dose | Leukocyte infiltration | [33] | |
| n.m. | Osteoporosis | Oral | n.m. | TNF-α, CRP, MDA | [34] | ||
| 300 | Ear edema | Gavage | Single-dose | Edema | [35] | ||
| 300 | Paw edema | Single-dose | Edema | ||||
| 300 | Vascular permeability | Single-dose | Volume of exudate | ||||
| 300 | Granulomatous | Daily, 6 d | Granulomatous tissue | ||||
| Acetone maceration | 2500 | Paw edema | Single-dose | Edema | [36] | ||
| Ethanolic maceration | 2500 | Paw edema | Single-dose | Edema | |||
| Rosmarinus officinalis | Hydro-ethanolic maceration | 10–40 | Peritoneal adhesion | IP | Single-dose | TNF-α, IL-1β, IL-6, TGF-β, GSH, MDA, NO | [37] |
| Methanolic Soxhlet extraction | 10, 50 | Paw edema | Gavage | Single-dose | Edema | [38] | |
| Rosmarinic acid | n.a. | 10–50 | Single-dose | Edema | |||
| 25 | Thermal injury | IV | Single-dose | TNF-α, IL-1β, IL-6 | |||
| Chromatography extraction | 10–40 | Paw edema | Gavage | Single-dose | Edema | [39] | |
| n.a. | 100 | Sepsis | IP | Single-dose | TNF-α, CAT, GPx, GSH, SOD | [40] | |
| 5–20 | Acute lung injury | Single-dose | TNF-α, IL-1β, IL-6, SOD | [41] | |||
| 5–20 | Asthma | Oral | Daily, 22 d | Eosinophils/neutrophils/monocytes/lymphocytes infiltration, CAT, MDA, SOD | [42] | ||
| 50 | Vascular impairment | Gavage | Daily, 10 wks | TNF-α, IL-1β, IL-6 | [43] | ||
| n.m. | 5–20 | Asthma | Oral | Daily, 22 d | IL-4, IFN-γ, IgE, PLA2 | [44] | |
| n.a. | 10–50 | Acute liver injury | Gavage | Daily, 2 d | TNF-α, COX-2, TGF-β, SOD | [45] | |
| n.a. | 200 | Nephrotoxicity | Daily, 7 d | TNF-α, GSH, MDA | [46] | ||
| 75–300 | Hepatocarcinoma | Daily, 10 d | TNF-α, IL-1β, IL-6, TGF-β | [47] | |||
| n.m. | 40, 80 | Elevation of C-reactive protein | Daily, 8 wks | IL-1β, IL-18 | [48] | ||
| n.a. | 75–300 | Hepatocarcinoma | Daily, 10 d | IL-2, IL-6, IL-10, IFN-γ | [49] | ||
| 30, 60 | Colitis | Daily, 7 d | IL-1β, IL-6, IL-22, COX-2, MPO, iNOS | [50] | |||
| n.m. | 10 | Spinal cord injury | IP | Daily, 7 d | TNF-α, IL-1β, IL-6, CAT, GPx, GSH, GST, MDA, SOD, ROS | [51] | |
| n.a. | 20 | Asthma | Daily, 3 d | IL-4, IL-5, IL-13 | [52] | ||
| n.a. | 5–20 | Mastitis | IP | Single-dose | TNF-α, IL-1β, IL-6, MPO | [53] | |
| n.m. | Skin irritation | Topical | 3 d | Edema | [54] | ||
| n.m. | 20 | Fat graft | IP | Daily, 8 wks | TNF-α, TGF-β1, MDA | [55] | |
| Rosmarinic acid | n.a. | 10, 50 | Estrogen deficiency | Gavage | Daily, 28 d | IL-18, CAT, GSH, GSSG, GSH/GSSG ratio, SOD | [56] |
| 10 | Acute liver injury | Daily, 30 d | TNF-α, IL-6, CAT, GSH, MDA, SOD | [57] | |||
| n.m. | 50 | Nephrotoxicity | Daily, 14 d | TNF-α, IL-1β, IL-6, CAT, GPx, GR, GSH, GSSH, GST, NO, SOD | [58] | ||
| n.a. | 25, 50 | Neuropathic pain | Daily, 28 d | TNF-α, IL-6, MDA | [59] | ||
| n.m. | 10 | Myringosclerosis | 5 wk, 7 d | Edema | [60] | ||
| n.a. | 10–50 | Neuropathic pain | Single-dose | IL-1β, COX2, PGE-2, NO | [61] | ||
| Rosmarinusofficinalis | Ethanolic Soxhlet extraction | 400 | IP | Daily, 14 d | IL-1β, COX2, PGE-2, NO | ||
| Hydro-ethanolic maceration | 10–50 | Paw edema | Single-dose | COX-1, COX-2 | [62] | ||
| Carnosol | n.a. | 0.5, 1, 2 | Single-dose | COX-1, COX-2 | |||
| n.m. | Atopic dermatitis | n.m. | Twice | Edema, TNF-α, IL-1β, COX-2, iNOS | [63] | ||
| 50 | Autoimmune encephalomyelitis | IP | Daily | IL-5, IL-10, IL-17, FN-γ | [64] | ||
| n.m. | 5 | Spinal cord injury | Daily, 5 d | TNF-α, IL-1β, IL-6, CAT, GPx, GSH, GST | [65] | ||
| n.a. | 3 | Acute kidney injury | IV | Single-dose | TNF-α, IL-1β, MPO | [66] | |
| 0.0125 | Atopic dermatitis | Topical | 3 wk, 4 wks | Edema, TNF-α, IL-1β, COX-2, JAK, iNOS | [67] | ||
| Chromatography extraction | 2.5 | Pleurisy | IP | Single-dose | Leukocyte infiltration, volume of exudate, IL-10, IL-17, MPO, NOx | [68] | |
| Rosmarinusofficinalis | Hydrodistillation | 25, 50 | Single-dose | Leukocyte infiltration, volume of exudate, IL-10, IL-17, MPO, NOx | |||
| Rosmarinic acid | Chromatography extraction | 5 | Single-dose | Leukocyte infiltration, volume of exudate, IL-10, IL-17, MPO, NOx |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonçalves, C.; Fernandes, D.; Silva, I.; Mateus, V. Potential Anti-Inflammatory Effect of Rosmarinus officinalis in Preclinical In Vivo Models of Inflammation. Molecules 2022, 27, 609. https://doi.org/10.3390/molecules27030609
Gonçalves C, Fernandes D, Silva I, Mateus V. Potential Anti-Inflammatory Effect of Rosmarinus officinalis in Preclinical In Vivo Models of Inflammation. Molecules. 2022; 27(3):609. https://doi.org/10.3390/molecules27030609
Chicago/Turabian StyleGonçalves, Catarina, Daniela Fernandes, Inês Silva, and Vanessa Mateus. 2022. "Potential Anti-Inflammatory Effect of Rosmarinus officinalis in Preclinical In Vivo Models of Inflammation" Molecules 27, no. 3: 609. https://doi.org/10.3390/molecules27030609
APA StyleGonçalves, C., Fernandes, D., Silva, I., & Mateus, V. (2022). Potential Anti-Inflammatory Effect of Rosmarinus officinalis in Preclinical In Vivo Models of Inflammation. Molecules, 27(3), 609. https://doi.org/10.3390/molecules27030609







