Long-Term Biodegradation of Polyacrylamide Gel Residues in Mammary Glands: Physico-Chemical Analysis, Chromatographic Detection, and Implications for Chronic Inflammation
Abstract
:1. Introduction
2. Results and Discussion
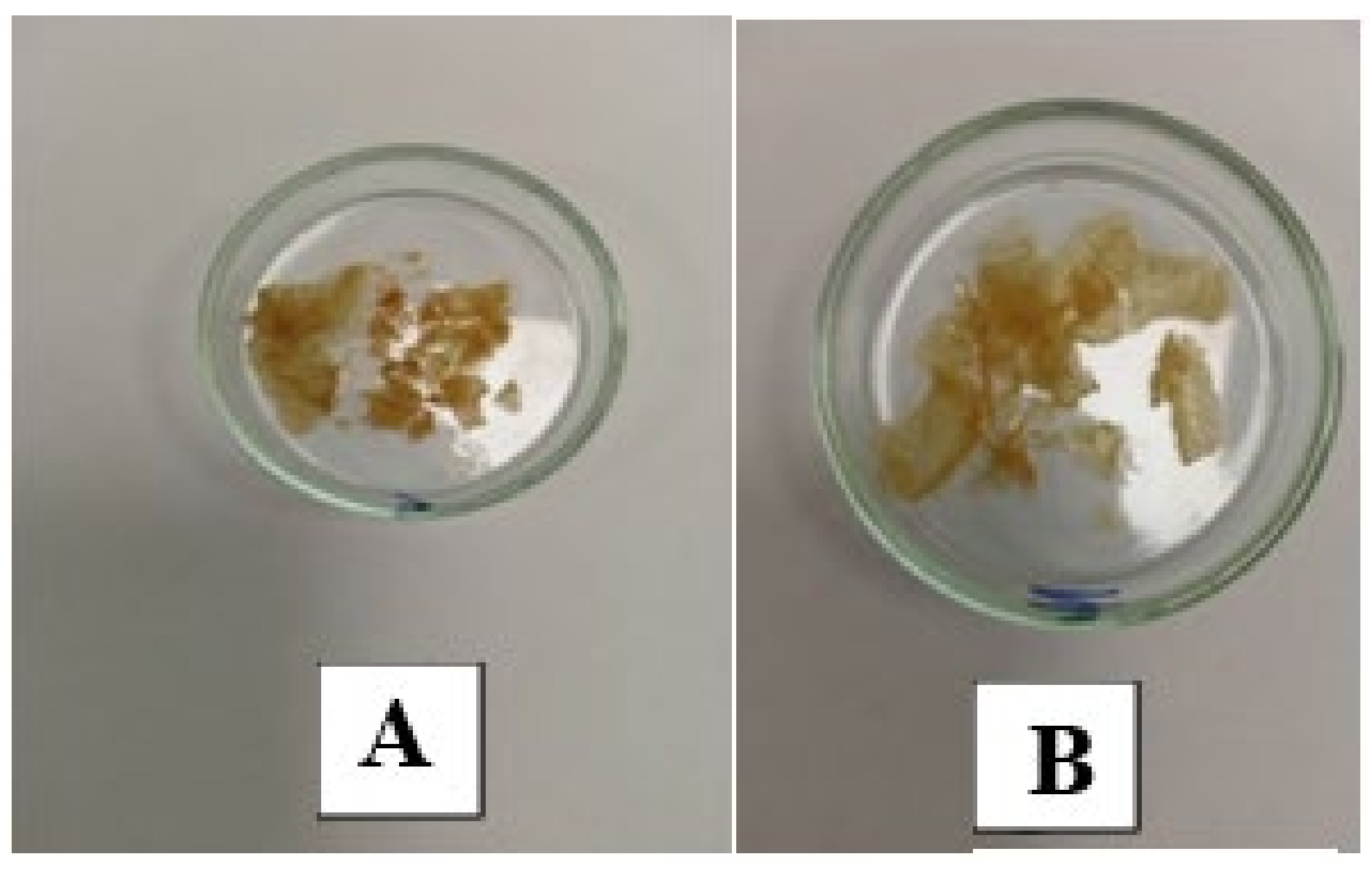
- MG-23: Gel implanted in the mammary glands for 23 years.
- LB-27: Gel from the left breast implanted for 27 years (contains dense infiltrate inclusions).
- RB-27: Gel from the right breast implanted for 27 years.
- -
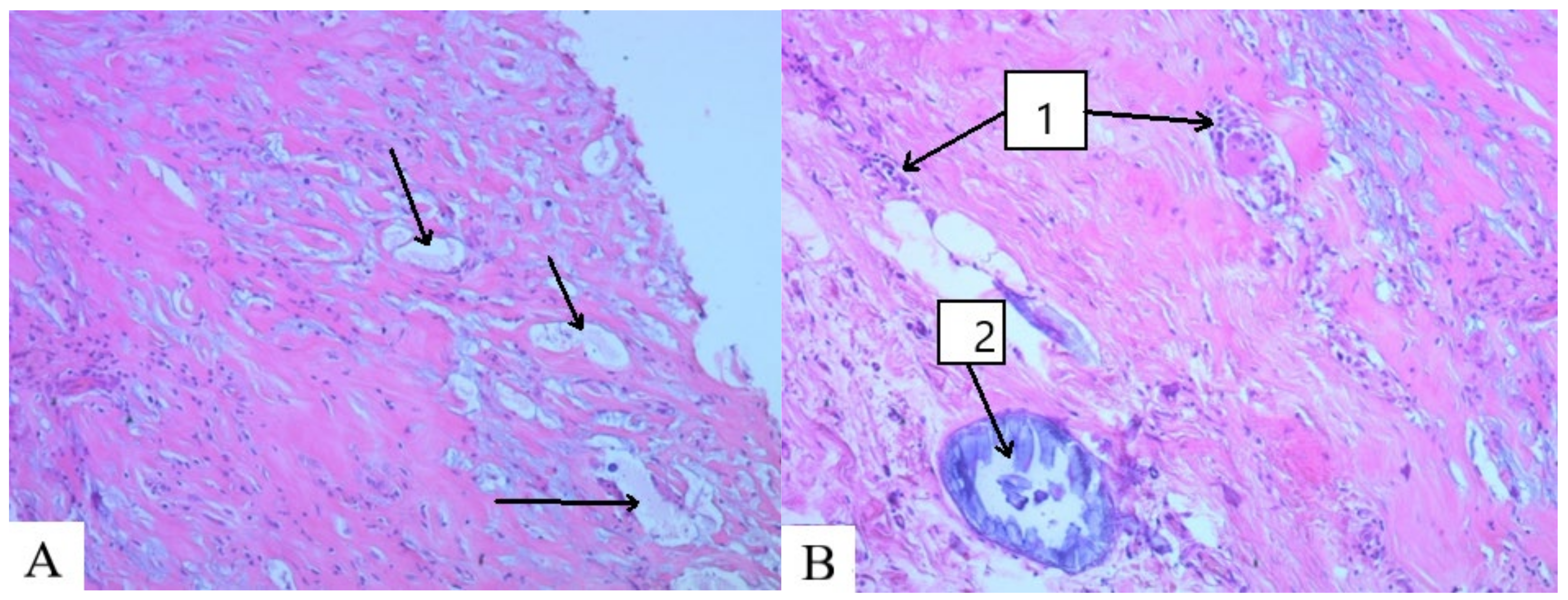
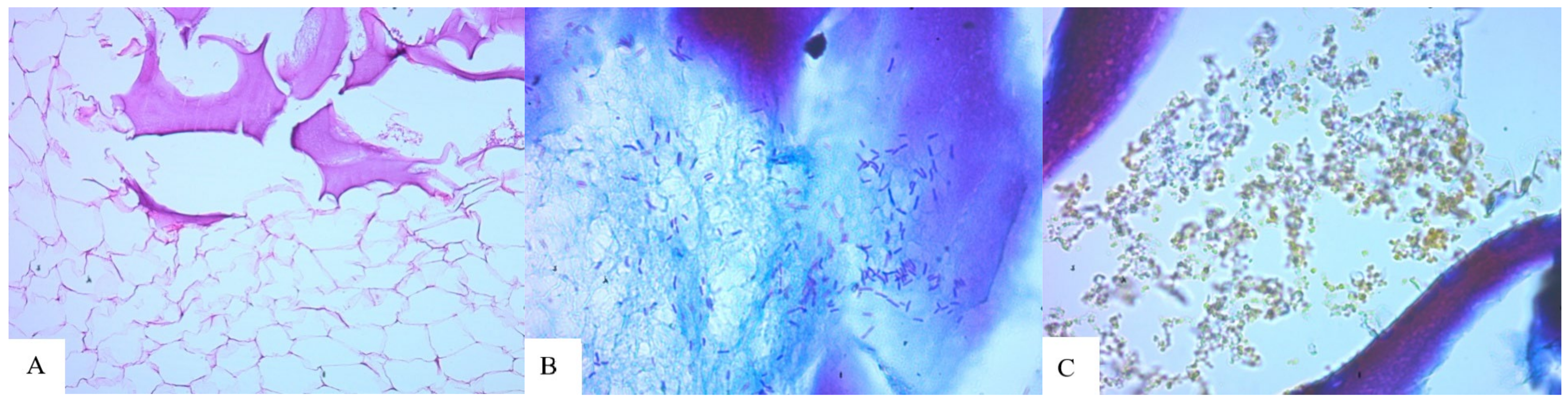
- Foreign substance (gel) migrated in the tissues, provoking the active growth of connective tissue;
- -
- Aseptic and septic inflammatory reactions;
- -
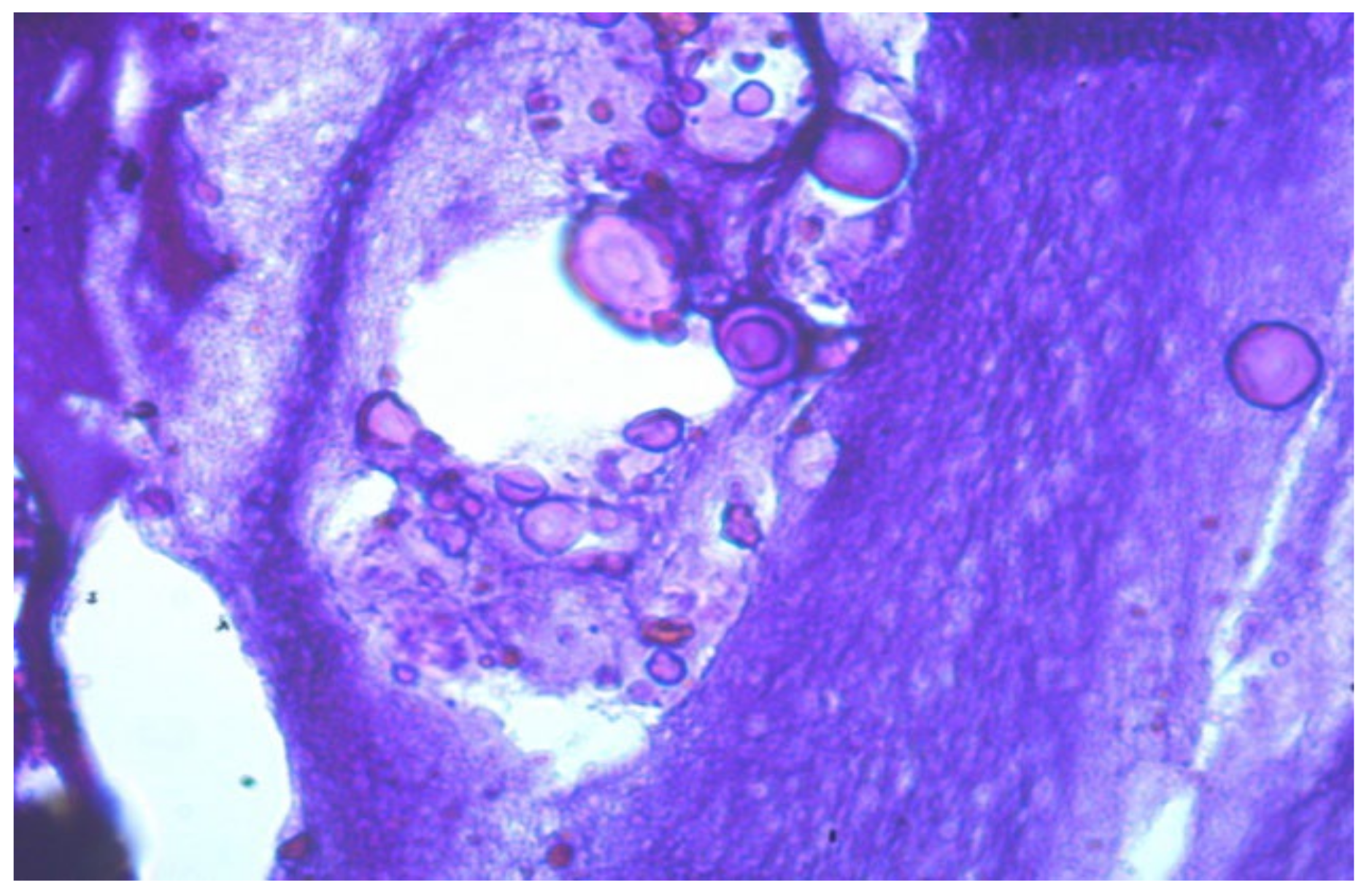
- Sections of round-shaped petrifications with clear contours;
- -
- Lymphoid cell reaction, the presence of voids and necrotic masses, and the formation of cystic cavities;
- -
- Pronounced deformation of adipocytes;
- -
- Muscle tissue with extensive necrosis and effusion of the protein component;
- -
- Numerous mast cells;
- -
- Isolated, giant Pirogov–Langhans cells surrounded by lymphocytes and macrophages.
- Rupture of cross-linked chains. Nucleophilic effect of protonated solvent on cross-linked sections of macromolecules:
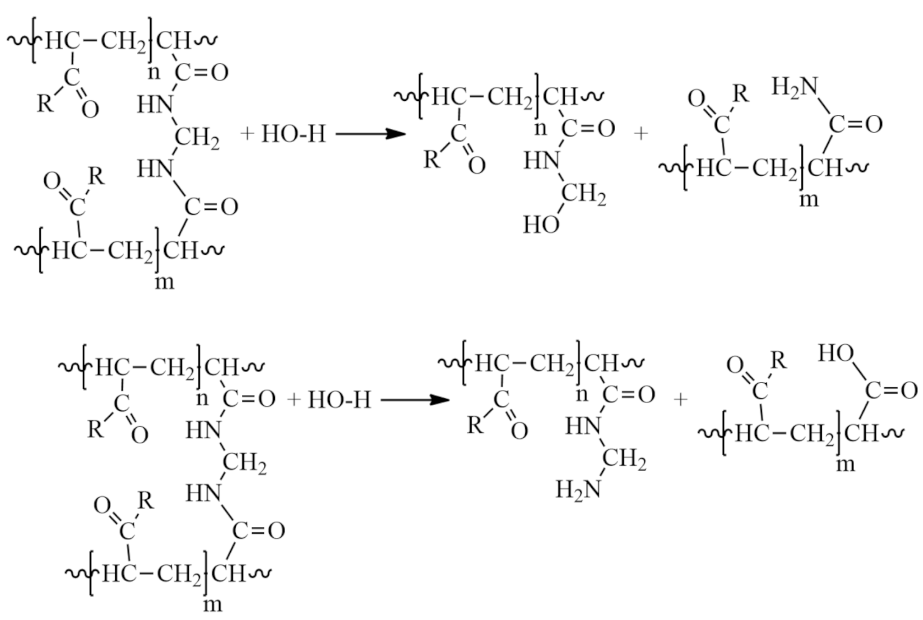
- 2
- Partial hydrolysis under slightly acidic conditions:
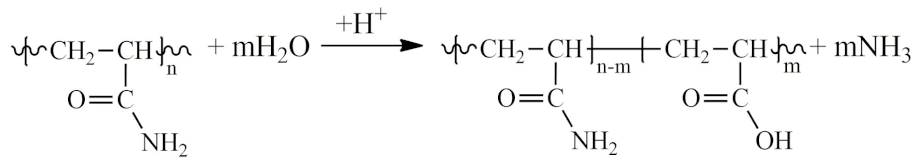
- The degree of partial hydrolysis under acidic conditions can reach a significant level. Moreover, when the degree of conversion reaches 3–5%, hydrolysis in an acidic medium is auto-catalytically accelerated.
- 3
- The formation of partially or completely insoluble products due to the imidization reaction in acidic and slightly acidic media, leading to the formation of cyclic and three-dimensional spatial structures:

- 4
- Hydrolysis of the amide group in a slightly alkaline medium under the action of hydroxides and carbonates:
- Alkaline hydrolysis of PAA results in the formation of macromolecules of acrylamide copolymers with acrylic acid salts, exhibiting a statistical distribution along the polymer chain without block structures. The maximum degree of hydrolysis of PAA in alkaline conditions does not exceed 70% due to the reduced reactivity of amide groups blocked by neighboring carboxylate groups, as shown in the scheme:

- 5
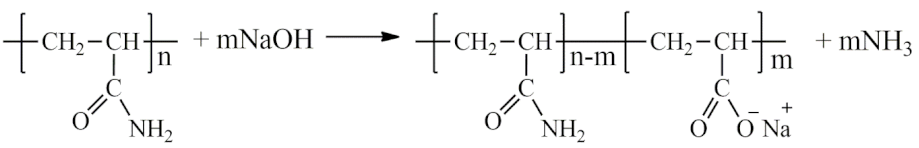
- Aminomethylation of PAA with aldehydes (formaldehyde, acetaldehyde, 5-hydroxymethylfurfural, malondialdehyde, fatty aldehydes, etc.) and primary and secondary amines in a slightly alkaline medium to form an aminomethylated polymer according to the scheme:

- 6
- The interaction of PAA with endogenous and exogenous aldehydes in acidic and slightly acidic media results in the formation of intramolecular cross-linking:
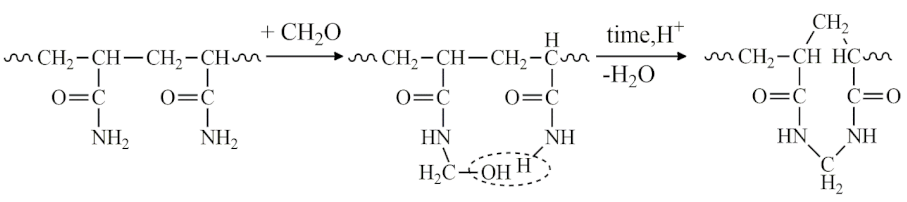
- In this case, intermolecular cross-linking can also occur, resulting in the formation of three-dimensional structures (-CONH-CH2-NHCO-):

- -
- PAAG degradation products: N,N-dimethylacetamide (a potentially carcinogenic substance) and acetamide (an aprotic solvent);
- -
- Eicosanoids—oxidized derivatives of polyunsaturated fatty acids are involved in a variety of processes, such as muscle tissue growth, irritation, and immune reactions to introduced toxins and pathogens, neurotransmitters and hormones: methyl ester 5,8,11,14-eicosatetraenoic acid, 2-methyleicosan, methyl ester 11,14-eicosadienoic acid;
- -
- Products of fatty acid metabolism: 2,4-decadienal, N,N-Dimethyldodecanamide, Tetradecanamide, 9-Octadecenamide, Linoleic acid ethyl ester, 2,4-Decadienal, Hexadecanoic acid, methyl ester, 9-Octadecenoic acid (Z)-, methyl ester, Methyl tetradecanoate, Pantolactone, Ethyl Oleate, 9,12-Octadecadienoic acid, methyl ester, Dodecanamide, Pentanoic acid, 2,2,4-trimethyl-3-carboxyisopropyl, isobutyl ester, Methyl 8-methyl-nonanoate, Tetradecanoic acid, 12-methyl-, methyl ester, 10-Octadecenoic acid, methyl ester, Citric acid, triethyl ester;
- -
- Squalene (characterized by antioxidant, cardioprotective, and anti-carcinogenic activity, as well as anti-inflammatory properties [27]);
- -
- Phosphates, which accompany an inflammatory reaction, can serve as a source of calcinate formation (calcium phosphate).
- -
- Cholesterol.
3. Materials and Methods
3.1. Materials
- MG-23: Gel implanted in the mammary glands for 23 years.
- LB-27: Gel from the left breast implanted for 27 years (contains dense infiltrate inclusions).
- RB-27: Gel from the right breast implanted for 27 years.
3.2. Characterization Methods
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- ISAPS (International Society of Aesthetic Plastic Surgery). Reports and Press Releases. Available online: https://www.isaps.org/discover/about-isaps/global-statistics/reports-and-press-releases/ (accessed on 26 April 2024).
- Knoedler, S.; Knoedler, L.; Geldner, B.; Ghanad, I.; Kim, B.S.; Alfertshofer, M.; Machens, H.G.; Broer, P.N.; Pomahac, B.; Kauke-Navarro, M.; et al. Isolated and combined breast augmentation in transgender patients: Multi-institutional insights into early outcomes and risk factors. J. Plast. Reconstr. Aesthetic Surg. 2024, 90, 149–160. [Google Scholar] [CrossRef]
- Asiri, M.N.; Shaheen, R.S.; Altamimi, O.M.I.; Alzahrani, M.M.A.; Alzhrani, A.A.; Alballaa, N.A.; Al Mazyad, Y.N.; ALzahrani, K. Understanding the Factors that Influence Woman’s Decision-Making regarding Breast Augmentation Surgery. Nat. Camp. 2024, 28, 2694–2716. [Google Scholar]
- Crerand, C.E.; Infield, A.L.; Sarwer, D.B. Psychological Considerations in Cosmetic Breast Augmentation. Plast. Aesthetic Nurs. 2009, 29, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Suri, K.; Billick, S. Breast Implant Illness Through a Psychiatric Lens. Aesthetic Plast. Surg. 2024, 48, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Unda, N.A.; McMains, C.J.; Doren, E.L. Long-Term Implications of Implant-Based Breast Reconstruction: What You Should Know About Breast Implant Illness and Breast Implant-Associated ALCL. Curr. Breast Cancer Rep. 2024, 16, 212–219. [Google Scholar] [CrossRef]
- Teo, S.Y.; Wang, S.-c. Radiologic features of polyacrylamide gel mammoplasty. Am. J. Roentgenol. 2008, 191, W89–W95. [Google Scholar] [CrossRef] [PubMed]
- Unukovych, D.; Khrapach, V.; Wickman, M.; Liljegren, A.; Mishalov, V.; Patlazhan, G.; Sandelin, K. Polyacrylamide gel injections for breast augmentation: Management of complications in 106 patients, a multicenter study. World J. Surg. 2012, 36, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Khedher, N.B.; David, J.; Trop, I.; Drouin, S.; Peloquin, L.; Lalonde, L. Imaging findings of breast augmentation with injected hydrophilic polyacrylamide gel: Patient reports and literature review. Eur. J. Radiol. 2011, 78, 104–111. [Google Scholar] [CrossRef]
- Lau, P.P.; Chan, A.C.; Tsui, M. Diagnostic cytological features of polyacrylamide gel injection augmentation mammoplasty. Pathology 2009, 41, 443–447. [Google Scholar] [CrossRef]
- Qian, B.; Xiong, L.; Guo, K.; Wang, R.; Yang, J.; Wang, Z.; Tong, J.; Sun, J. Comprehensive management of breast augmentation with polyacrylamide hydrogel injection based on 15 years of experience: A report on 325 cases. Ann. Transl. Med. 2020, 8, 475. [Google Scholar] [CrossRef]
- Qian, B.; Xiong, L.; Guo, K.; Wang, R.; Yang, J.; Wang, Z.; Tong, J.; Sun, J. Our strategy in complication management of augmentation mammaplasty with polyacrylamide hydrogel injection in 235 patients. J. Plast. Reconstr. Aesthetic Surg. 2011, 64, 731–737. [Google Scholar] [CrossRef]
- Ding, F.; Zhao, F.; Jin, R.; Rao, Y.; Yang, G.; Lu, L.; Wang, X.; Sun, D.; Zhou, X. Management of complications in 257 cases of breast augmentation with polyacrylamide hydrogel, using two different strategies: A retrospective study. Aesthetic Plast. Surg. 2022, 46, 2107–2121. [Google Scholar] [CrossRef] [PubMed]
- Hedström, K.; Falk-Delgado, A.; Sackey, H. Complications after breast augmentation with dermal fillers containing copolyamide: A systematic review. JPRAS Open 2024, 40, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Xiong, C.; Chen, Y.; Xu, Y.; Jiang, W.; Yin, X.; Chen, D.; Gong, X.; He, T.; An, Y.; Han, Y. A review of complications of polyacrylamide hydrogel injection. Chin. J. Plast. Reconstr. Surg. 2023, 5, 86–95. [Google Scholar] [CrossRef]
- Khan, N.; Pu, J.; Pu, C.; Xu, H.; Gu, X.; Lei, Z.; Huang, F.; Nasir, M.A.; Ullah, R. Experimental and mechanism study: Partially hydrolyzed polyacrylamide gel degradation and deplugging via ultrasonic waves and chemical agents. Ultrason. Sonochem. 2019, 56, 350–360. [Google Scholar] [CrossRef]
- Wan, Z.Y.; Xi, T.F.; Zhao, P.; Fan, C.X.; Sun, Y.; Feng, Z.G. In vitro degradation of medical polyacrylamide hydrogel I. Oxid. Key Eng. Mater. 2005, 288, 397–400. [Google Scholar] [CrossRef]
- Fernández-Cossío, S.; Castaño-Oreja, M.T. Biocompatibility of two novel dermal fillers: Histological evaluation of implants of a hyaluronic acid filler and a polyacrylamide filler. Plast. Reconstr. Surg. 2006, 117, 1789–1796. [Google Scholar] [CrossRef] [PubMed]
- Christensen, L.H.; Breiting, V.B.; Aasted, A.; Jørgensen, A.; Kebuladze, I. Long-Term Effects of Polyacrylamide Hydrogel on Human Breast Tissue. Plast. Reconstr. Surg. 2003, 111, 1883–1890. [Google Scholar] [CrossRef] [PubMed]
- Kushida-Contreras, B.H.; Gómez-Calva, B.; Mendoza-Ramírez, B.; Gaxiola-García, M.A. Autoimmune Autoinflammatory Syndrome Induced by Adjuvants (ASIA) After Injection of Foreign Materials for Cosmetic Purposes: Retrospective Analysis of 1027 Cases. Aesthetic Plast. Surg. 2024, 48, 491–500. [Google Scholar] [CrossRef]
- Lipatov, K.; Struchkov, Y.V.; Komarova, E.A.; Nasibov, B.S. Post-implantation polyacrylamide mammary syndrome: The actual problem of general surgical hospitals. Surg. News 2016, 24, 401–406. [Google Scholar]
- Lui, C.Y.; Ho, C.M.; Iu, P.P.; Cheung, W.Y.; Lam, H.S.; Cheng, M.S.; Liu, H.L.L. Evaluation of MRI findings after polyacrylamide gel injection for breast augmentation. Am. J. Roentgenol. 2008, 191, 677–688. [Google Scholar] [CrossRef] [PubMed]
- Caulfield, M.J.; Hao, X.; Qiao, G.G.; Solomon, D.H. Degradation on polyacrylamides. Part I. Linear Polyacryl. Polym. 2003, 44, 1331–1337. [Google Scholar] [CrossRef]
- Caulfield, M.J.; Hao, X.; Qiao, G.G.; Solomon, D.H. Degradation on polyacrylamides. Part II. Polyacryl. Gels. Polym. 2003, 44, 3817–3826. [Google Scholar] [CrossRef]
- Lopatin, V.V.; Askadskii, A.A.; Peregudov, A.S.; Vasil’ev, V.G. Structure and relaxation properties of medical-purposed polyacrylamide gels. J. Appl. Polym. Sci. 2005, 96, 1043–1058. [Google Scholar] [CrossRef]
- Kuptsov, A.; Zhizhin, G.N. Handbook of Fourier Transform Raman and Infrared Spectra of Polymers; Elsevier: Amsterdam, The Netherlands, 1998. [Google Scholar]
- Cárdeno, A.; Aparicio-Soto, M.; de la Paz, S.M.; Bermúdez, B.; Muriana, F.J.; de la Lastra, C.A. Squalene targets pro- and anti-inflammatory mediators and pathways to modulate over-activation of neutrophils, monocytes and macrophages. J. Funct. Foods 2015, 14, 779–790. [Google Scholar] [CrossRef]
- Shodex. Available online: https://www.shodex.com/en/dc/06/13/08.html (accessed on 26 April 2024).







| Types of Oscillation | The Wave Number ν, cm−1 |
|---|---|
| Intramolecular hydrogen bonding of polyatomic alcohols, amines, and valence vibrations N-H in amino acids | 3450 |
| Wide-band, intra-complex compounds, intramolecular hydrogen bonds | 3280 |
| -CH2-—valence vibrations | 2930–2800; 1440–1400 |
| -COOH—valence vibrations | 1760 |
| -CO-NHR—valence vibrations | 1640–1540 |
| -C=O—valence vibrations | 1640 |
| -CO-N=—valence vibrations in tertiary amines | 1650 |
| Secondary amines in imidization reactions | 1580 |
| C=O valence symmetric and asymmetric vibrations in RCOO-. Dimers –COOH: plane deformation vibrations -OH and valence vibrations of C-O dimers of carboxyl groups | 1405 |
| -CN | 1350–1210 |
| -C=O,-C-O- valence vibrations in RC(=O)-OH | 1262 |
| -C-O-C- | 1050 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Legonkova, O.A.; Sultanova, N.O.; Stafford, V.V.; Zavitaeva, A.A.; Kopitsyn, D.S.; Tolboeva, E.R.; Mahmydov, A.M.; Vinokurov, V.A.; Davydova, G.A.; Svishcheva, N.B.; et al. Long-Term Biodegradation of Polyacrylamide Gel Residues in Mammary Glands: Physico-Chemical Analysis, Chromatographic Detection, and Implications for Chronic Inflammation. Molecules 2024, 29, 3247. https://doi.org/10.3390/molecules29143247
Legonkova OA, Sultanova NO, Stafford VV, Zavitaeva AA, Kopitsyn DS, Tolboeva ER, Mahmydov AM, Vinokurov VA, Davydova GA, Svishcheva NB, et al. Long-Term Biodegradation of Polyacrylamide Gel Residues in Mammary Glands: Physico-Chemical Analysis, Chromatographic Detection, and Implications for Chronic Inflammation. Molecules. 2024; 29(14):3247. https://doi.org/10.3390/molecules29143247
Chicago/Turabian StyleLegonkova, Olga A., Naida O. Sultanova, Victoria V. Stafford, Anastasia A. Zavitaeva, Dmitry S. Kopitsyn, Elena R. Tolboeva, Abdul M. Mahmydov, Vladimir A. Vinokurov, Galina A. Davydova, Natalia B. Svishcheva, and et al. 2024. "Long-Term Biodegradation of Polyacrylamide Gel Residues in Mammary Glands: Physico-Chemical Analysis, Chromatographic Detection, and Implications for Chronic Inflammation" Molecules 29, no. 14: 3247. https://doi.org/10.3390/molecules29143247
APA StyleLegonkova, O. A., Sultanova, N. O., Stafford, V. V., Zavitaeva, A. A., Kopitsyn, D. S., Tolboeva, E. R., Mahmydov, A. M., Vinokurov, V. A., Davydova, G. A., Svishcheva, N. B., Barbaro, K., & Rau, J. V. (2024). Long-Term Biodegradation of Polyacrylamide Gel Residues in Mammary Glands: Physico-Chemical Analysis, Chromatographic Detection, and Implications for Chronic Inflammation. Molecules, 29(14), 3247. https://doi.org/10.3390/molecules29143247








