Design of pH/Redox Co-Triggered Degradable Diselenide-Containing Polyprodrug via a Facile One-Pot Two-Step Approach for Tumor-Specific Chemotherapy
Abstract
1. Introduction
2. Results
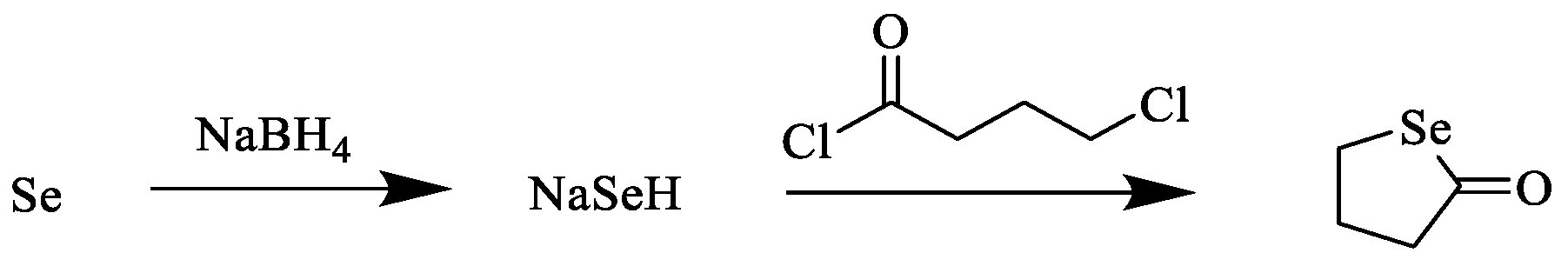
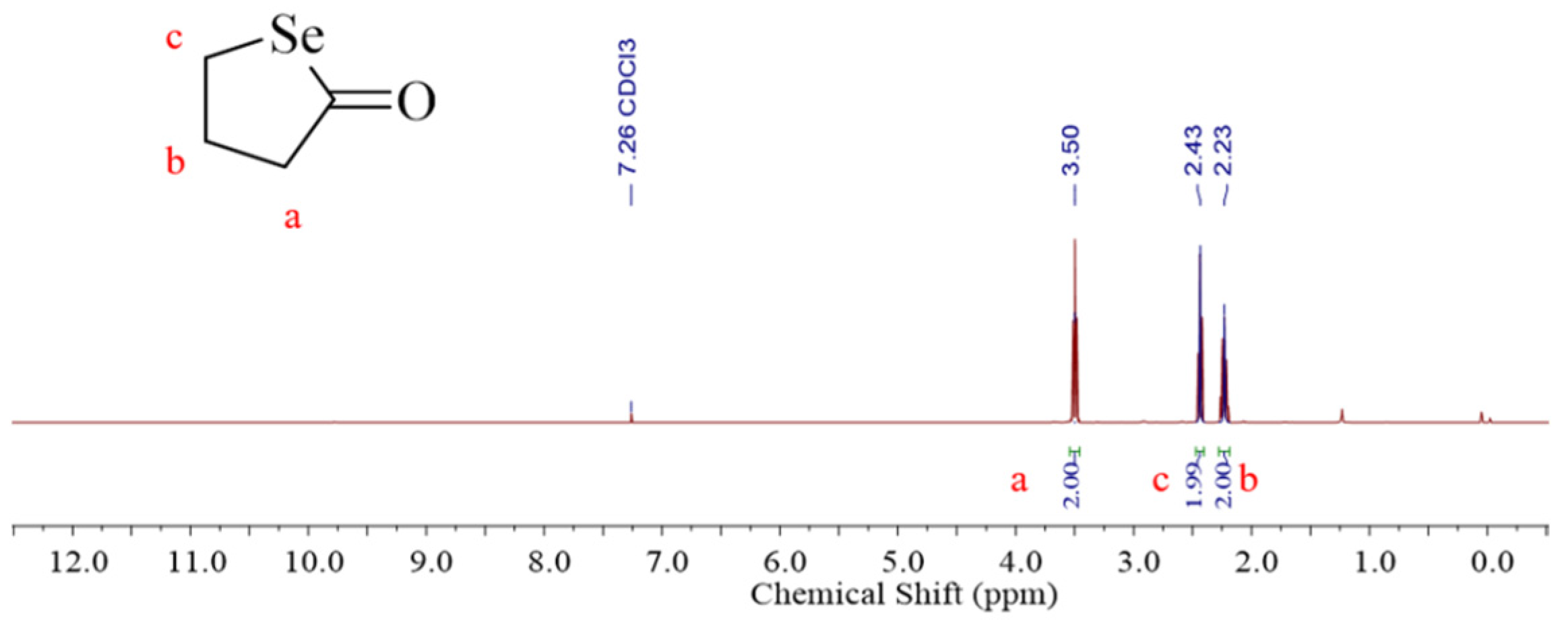
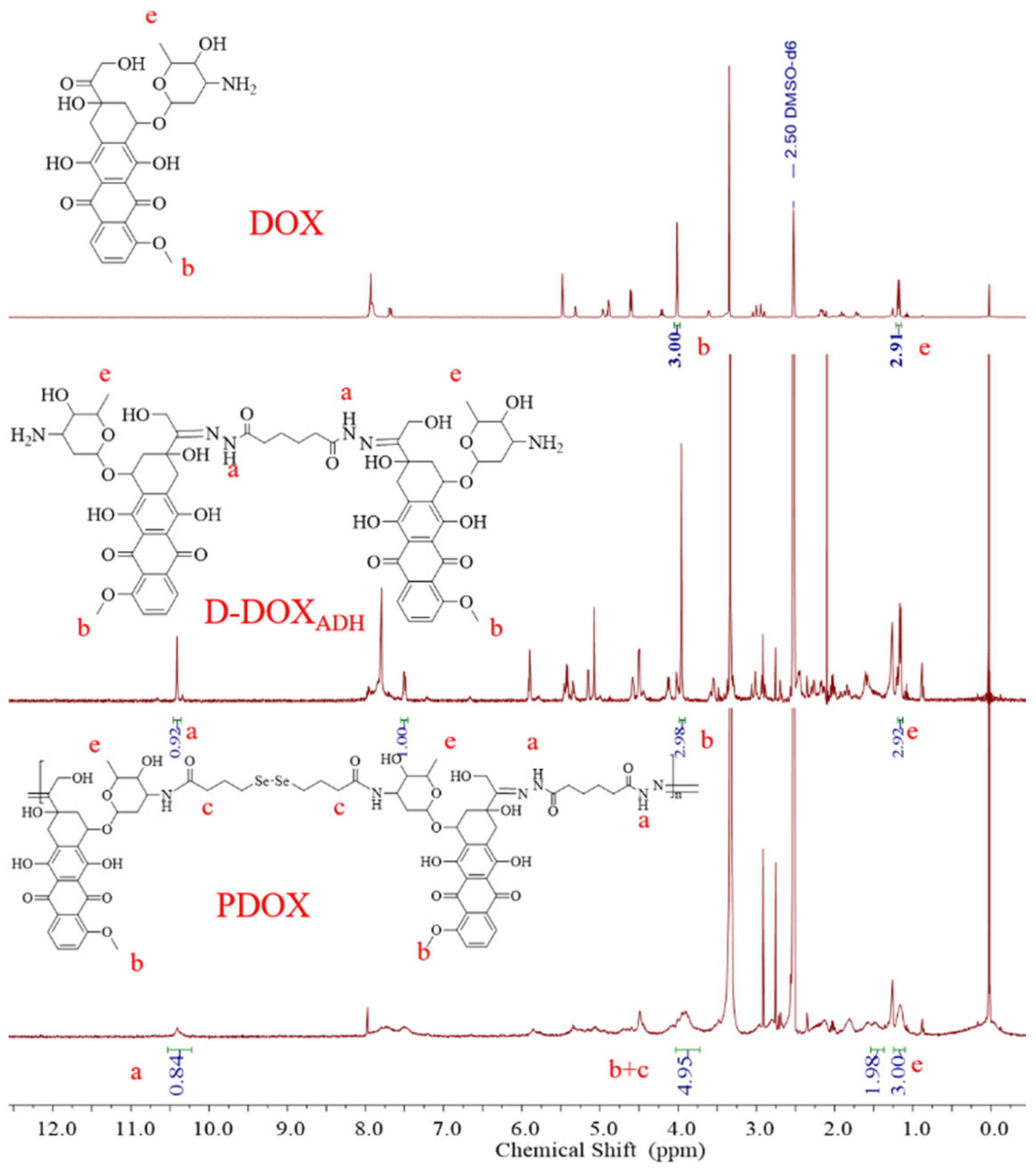
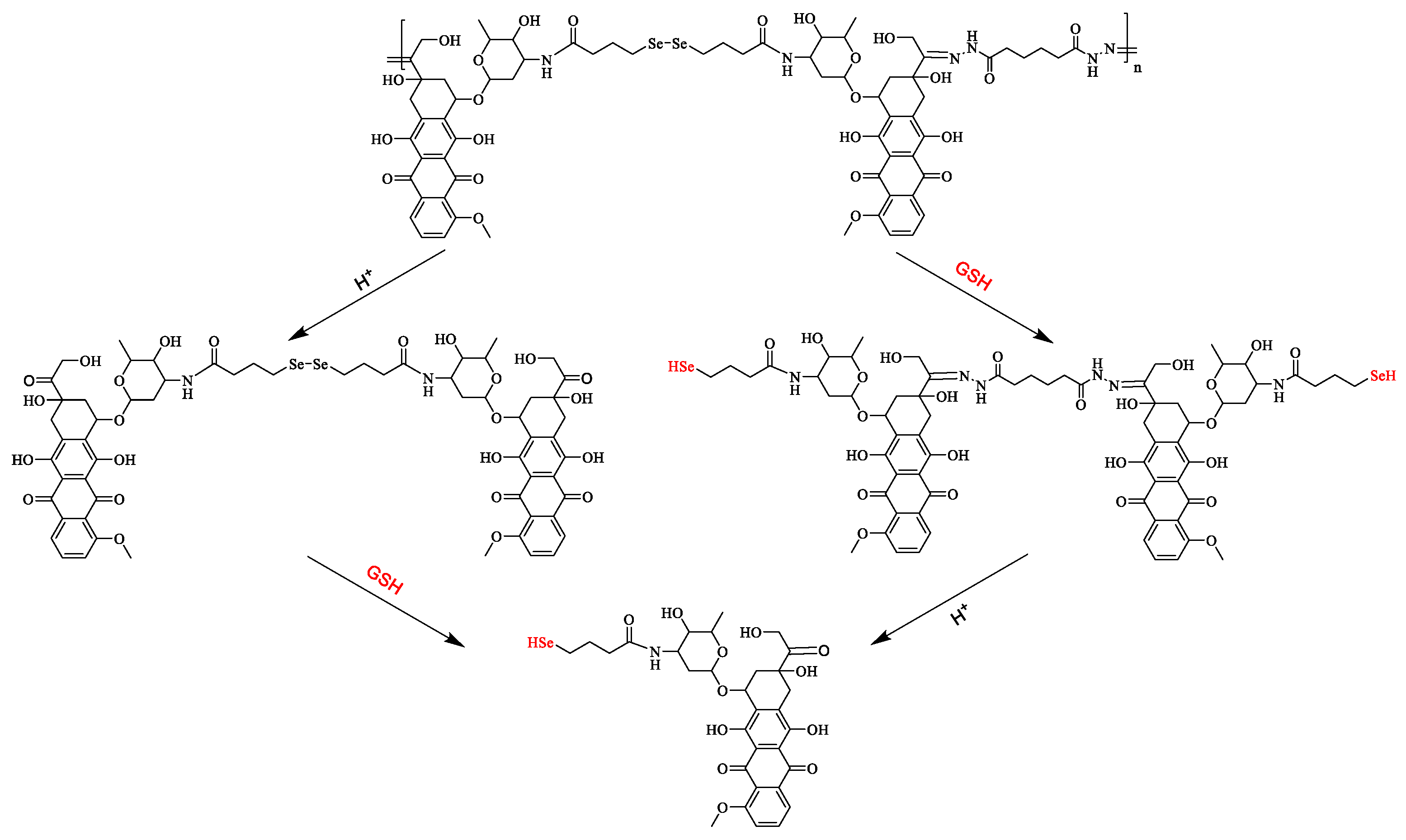
2.1. Synthesis and Characterization of PDOX
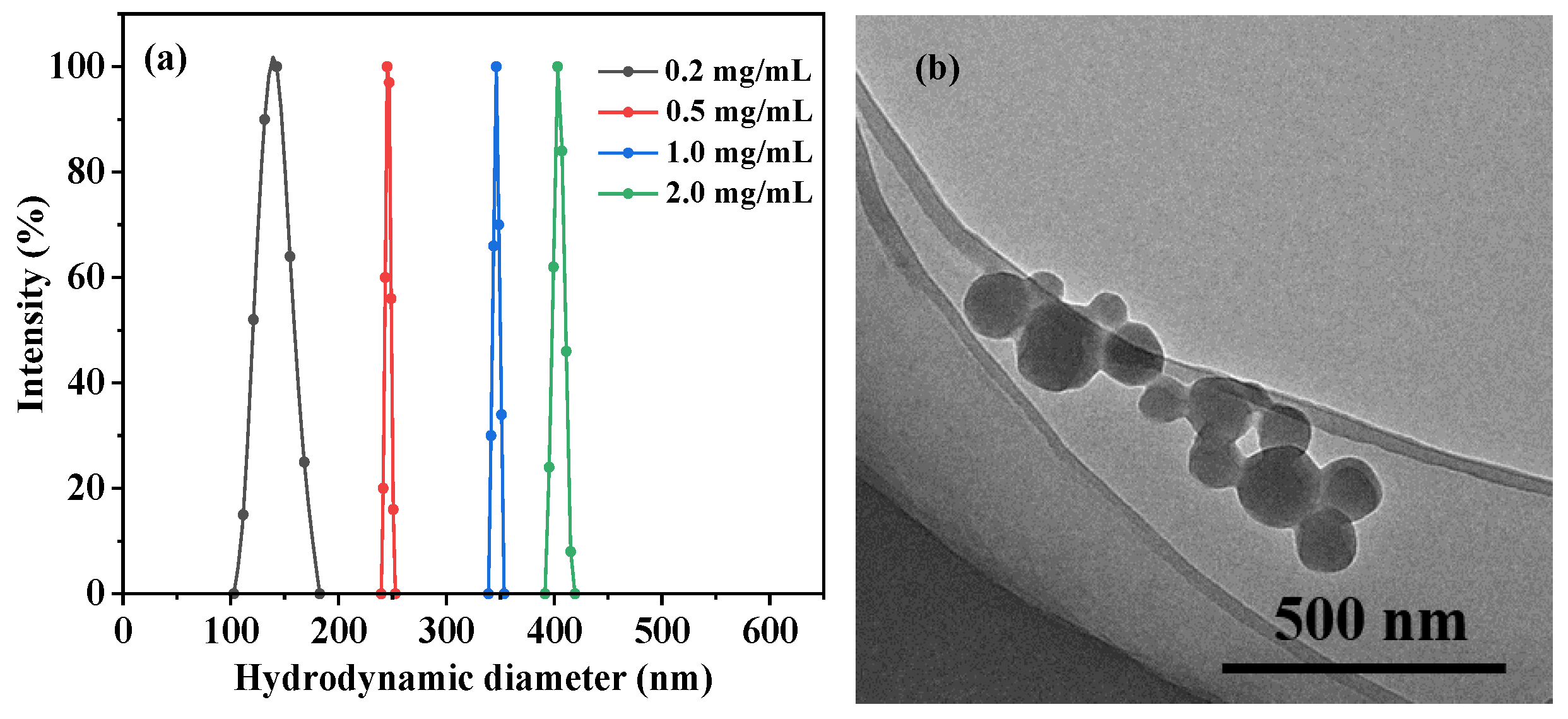
2.2. Fabrication and Characterization of PDOX Nanoparticles
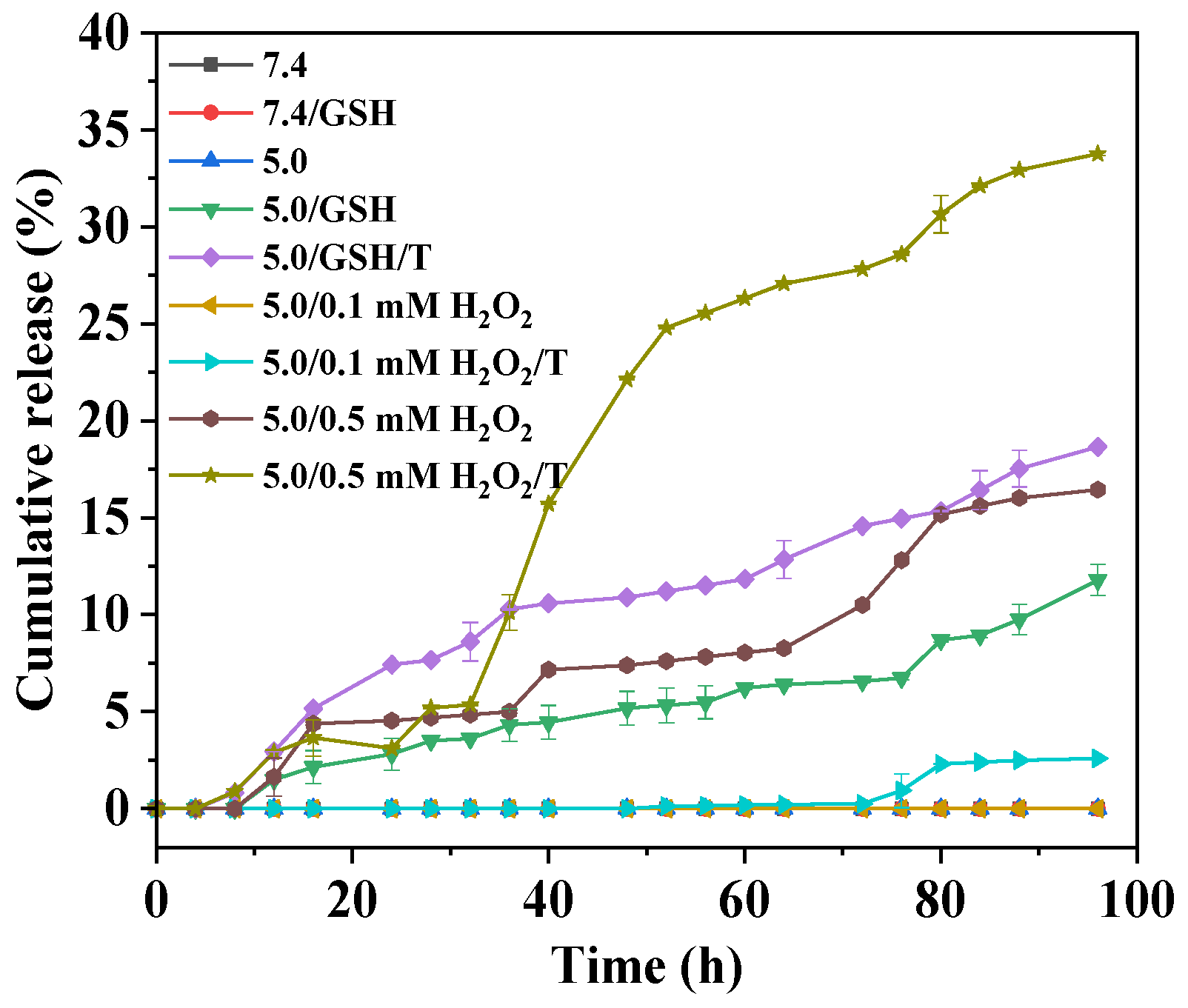
2.3. In Vitro Drug Release
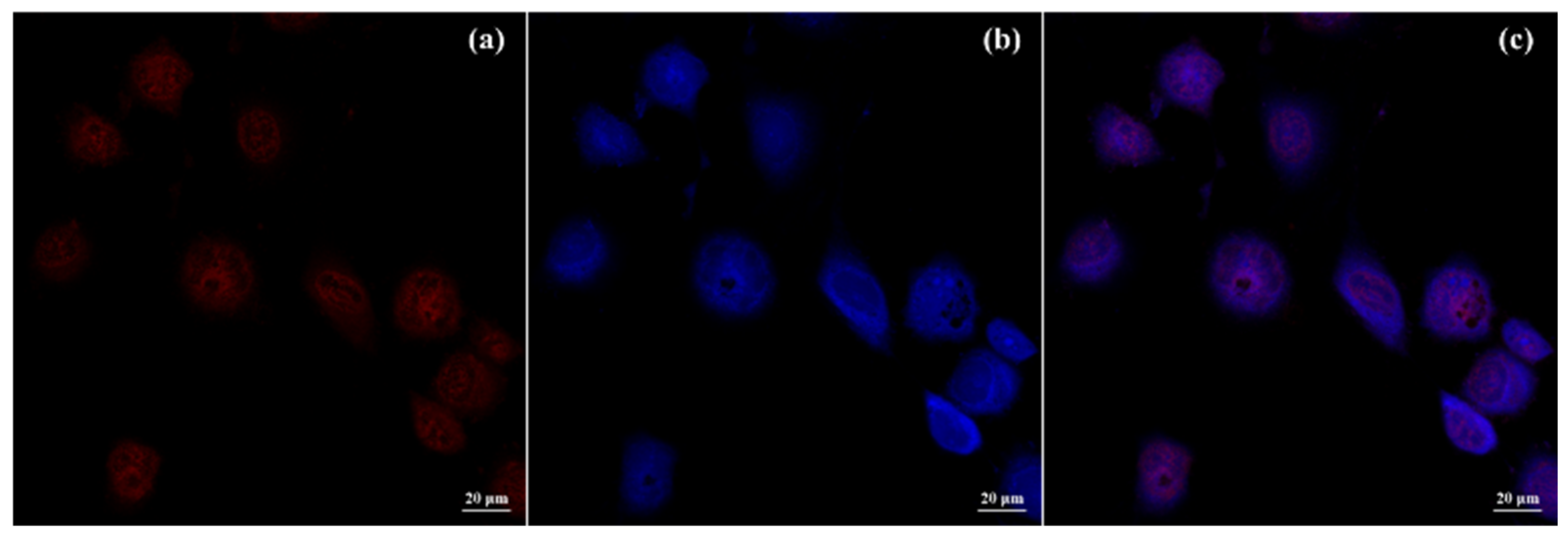
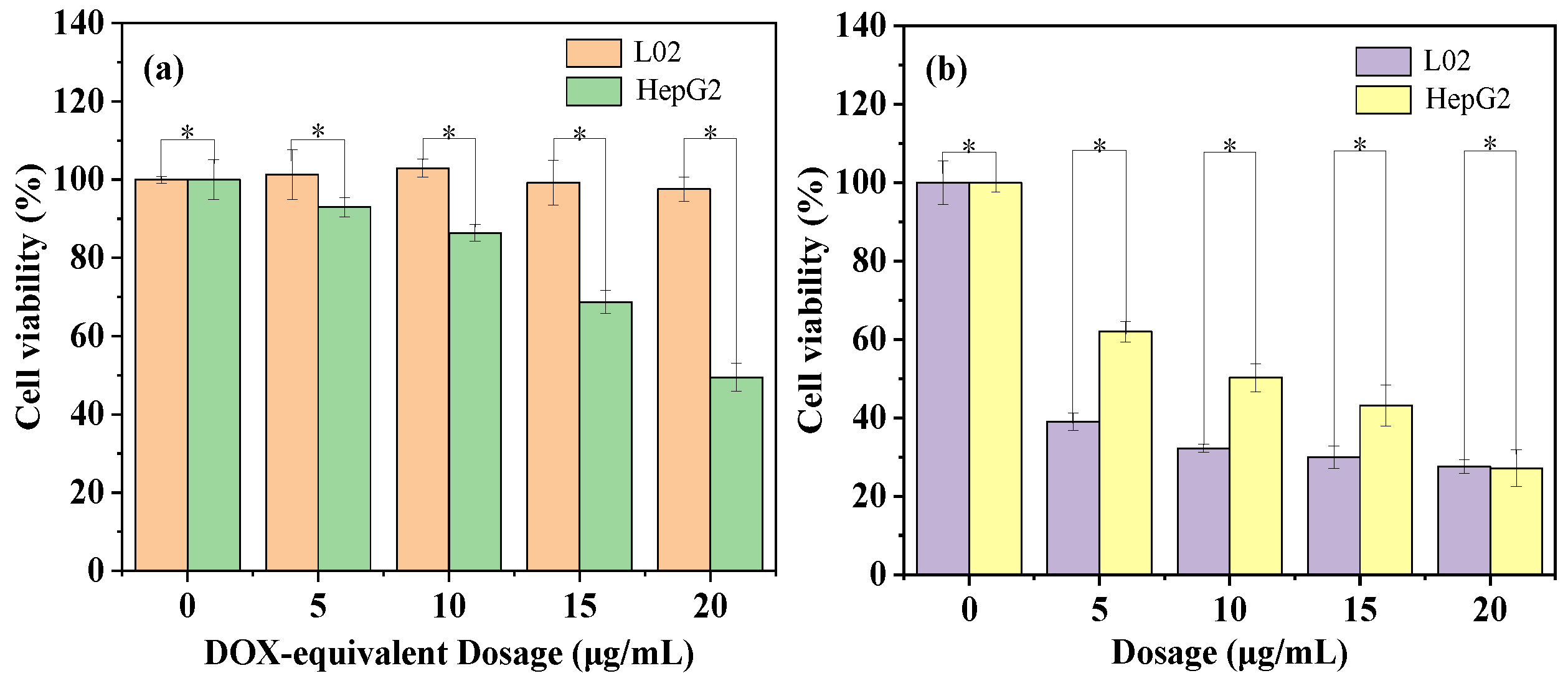
2.4. Cellular Uptake and Cytotoxicity
3. Discussion
4. Materials and Methods
4.1. Materials and Reagents
4.2. Analysis and Characterization
4.3. Synthesis Procedure
4.4. Redox-Triggered Drug Release
4.5. In Vitro Cellular Experiments
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Mirhadi, E.; Mashreghi, M.; Maleki, M.F.; Alavizadeh, S.H.; Arabi, L.; Badiee, A.; Jaafari, M.R. Redox-sensitive nanoscale drug delivery systems for cancer treatment. Int. J. Pharm. 2020, 589, 119882. [Google Scholar] [CrossRef]
- Mollazadeh, S.; Mackiewicz, M.; Yazdimamaghani, M. Recent advances in the redox-responsive drug delivery nanoplatforms: A chemical structure and physical property perspective. Mater. Sci. Eng. C 2021, 118, 111536. [Google Scholar] [CrossRef]
- Deng, Z.Y.; Liu, S.Y. Controlled drug delivery with nanoassemblies of redox-responsive prodrug and polyprodrug amphiphiles. J. Control Release 2020, 326, 276–296. [Google Scholar] [CrossRef]
- Wang, Q.; Guan, J.K.; Wan, J.L.; Li, Z.F. Disulfide based prodrugs for cancer therapy. RSC Adv. 2020, 10, 24397–24409. [Google Scholar] [CrossRef]
- Yang, K.K.; Yang, Z.Q.; Yu, G.C.; Nie, Z.H.; Wang, R.B.; Chen, X.Y. Polyprodrug Nanomedicines: An Emerging Paradigm for Cancer Therapy. Adv. Mater. 2022, 34, 2107434. [Google Scholar] [CrossRef]
- Seidi, F.; Zhong, Y.J.; Xiao, H.N.; Jin, Y.C.; Crespy, D. Degradable polyprodrugs: Design and therapeutic efficiency. Chem. Soc. Rev. 2022, 51, 6652–6703. [Google Scholar] [CrossRef]
- Liu, P. Polyprodrugs for tumor chemotherapy: From molecular structure to drug release performance. J. Mater. Chem. B 2023, 11, 9565–9571. [Google Scholar] [CrossRef]
- Wang, D.Q.; Zhou, N.; Zhang, N.; Zhi, Z.; Shao, Y.P.; Meng, L.J.; Yu, D.M. Facile preparation of pH/redox dual-responsive biodegradable polyphosphazene prodrugs for effective cancer chemotherapy. Colloids Surf. B-Biointerfaces 2021, 200, 111573. [Google Scholar] [CrossRef]
- Li, J.G.; Liu, P. pH/Reduction Dual-Triggered Degradable Poly(doxorubicin) Prodrug Nanoparticles for Leakage-Free Tumor-Specific Self-Delivery. Macromol. Rapid Commun. 2018, 39, 1800381. [Google Scholar] [CrossRef] [PubMed]
- Li, X.M.; Zhang, J.; Liu, P. Facile one-pot synthesis of amphiphilic acid/hypoxia co-triggered degradable diblock polyprodrug for tumor selective drug delivery. Int. J. Pharm. 2021, 606, 120941. [Google Scholar] [CrossRef] [PubMed]
- Li, X.M.; Liu, P. Synthesis and self-assembly of an acid/reduction co-triggered degradable amphiphilic copolyprodrug as a tumor-selective drug self-delivery system. J. Mater. Chem. B 2022, 10, 2926–2932. [Google Scholar] [CrossRef]
- Shi, Z.F.; Liu, J.F.; Tian, L.; Li, J.Y.; Gao, Y.; Xing, Y.; Yan, W.J.; Hua, C.Y.; Xie, X.L.; Liu, C.; et al. Insights into stimuli-responsive diselenide bonds utilized in drug delivery systems for cancer therapy. Biomed. Pharmacother. 2022, 155, 113707. [Google Scholar] [CrossRef]
- Deepagan, V.G.; Kown, S.; You, D.G.; Nguyen, V.Q.; Um, W.; Ko, H.; Lee, H.; Jo, D.-G.; Kang, Y.M.; Park, J.H. In situ diselenide-crosslinked polymeric micelles for ROS-mediated anticancer drug delivery. Biomaterials 2016, 103, 56–66. [Google Scholar] [CrossRef]
- Zhai, S.D.; Hu, X.L.; Hu, Y.J.; Wu, B.Y.; Xing, D. Visible light-induced crosslinking and physiological stabilization of diselenide-rich nanoparticles for redox-responsive drug release and combination chemotherapy. Biomaterials 2017, 121, 41–54. [Google Scholar] [CrossRef]
- Shao, D.; Li, M.Q.; Wang, Z.; Zheng, X.; Lao, Y.-H.; Chang, Z.M.; Zhang, F.; Lu, M.M.; Yue, J.; Hu, H.Z.; et al. Bioinspired Diselenide-Bridged Mesoporous Silica Nanoparticles for Dual-Responsive Protein Delivery. Adv. Mater. 2018, 30, 1801198. [Google Scholar] [CrossRef]
- Lin, W.J.; Xue, Z.L.; Wen, L.Y.; Li, Y.Z.; Liang, Z.P.; Xu, J.C.; Yang, C.F.; Gu, Y.X.; Zhang, J.; Xu, X.H.; et al. Mesoscopic simulations of drug-loaded diselenide crosslinked micelles: Stability, drug loading and release properties. Colloid Surf. B-Biointerfaces 2019, 182, 110313. [Google Scholar] [CrossRef]
- Tian, Y.F.; Lei, M.; Yan, L.K.; An, F.F. Diselenide-crosslinked zwitterionic nanogels with dual redox-labile properties for controlled drug release. Polym. Chem. 2020, 11, 2360–2369. [Google Scholar] [CrossRef]
- Wang, J.; Liu, J.; Lu, D.Q.; Chen, L.J.; Yang, R.J.; Liu, D.H.; Zhang, B. Diselenide-crosslinked carboxymethyl chitosan nanoparticles for doxorubicin delivery: Preparation and in vivo evaluation. Carbohydr. Polym. 2022, 292, 119699. [Google Scholar] [CrossRef]
- Tan, R.H.; Ge, J.; Wang, C.C.; Wan, Y.; Yang, X.L. Diselenide-triggered hydroxyethyl starch conjugate nanoparticles with cascade drug release properties for potentiating chemo-photodynamic therapy. Carbohydr. Polym. 2023, 311, 120748. [Google Scholar] [CrossRef] [PubMed]
- Shao, D.; Zhang, F.; Chen, F.M.; Zheng, X.; Hu, H.Z.; Yang, C.; Tu, Z.X.; Wang, Z.; Chang, Z.M.; Lu, J.N.; et al. Biomimetic Diselenide-Bridged Mesoporous Organosilica Nanoparticles as an X-ray-Responsive Biodegradable Carrier for Chemo-Immunotherapy. Adv. Mater. 2020, 32, 202004385. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.X.; Zhang, S.T.; Xu, J.Y.; Li, Y.Y.; He, J.L.; Yang, Y.; Huynh, T.; Ni, P.H.; Duan, G.X.; Yang, Z.X.; et al. Low-Dose X-ray-Responsive Diselenide Nanocarriers for Effective Delivery of Anticancer Agents. ACS Appl. Mater. Interfaces 2020, 12, 43398–43407. [Google Scholar] [CrossRef]
- Cao, W.; Zhang, X.L.; Miao, X.M.; Yang, Z.M.; Xu, H.P. γ-Ray-responsive supramolecular hydrogel based on a diselenide-containing polymer and a peptide. Angew. Chem. Int. Ed. 2013, 52, 6233–6237. [Google Scholar] [CrossRef]
- Zhu, R.; He, Q.; Li, Z.L.; Ren, Y.H.; Liao, Y.X.; Zhang, Z.J.; Dai, Q.; Wan, C.Y.; Long, S.H.; Kong, L.Y.; et al. ROS-cleavable diselenide nanomedicine for NIR-controlled drug release and on-demand synergistic chemo-photodynamic therapy. Acta Biomater. 2022, 153, 442–452. [Google Scholar] [CrossRef]
- Salma, S.A.; Patil, M.P.; Kim, D.W.; Le, C.M.Q.; Ahn, B.-H.; Kim, G.-D.; Lim, K.T. Near-infrared light-responsive, diselenide containing core-cross-linked micelles prepared by the Diels–Alder click reaction for photocontrollable drug release application. Polym. Chem. 2018, 9, 4813–4823. [Google Scholar] [CrossRef]
- Sun, C.X.; Tan, Y.Z.; Xu, H.P. From Selenite to Diselenide-Containing Drug Delivery Systems. ACS Mater. Lett. 2020, 2, 1173–1177. [Google Scholar] [CrossRef]
- Sun, C.X.; Gao, S.Q.; Tan, Y.Z.; Zhang, Z.H.; Xu, H.P. Side-Chain Selenium-Grafted Polymers Combining Antiangiogenesis Treatment with Photodynamic Therapy and Chemotherapy. ACS Biomater. Sci. Eng. 2021, 7, 3201–3208. [Google Scholar] [CrossRef]
- Wei, C.; Liang, B.Y.; Li, Y.S.; Yan, B.K.; Zhou, Y.; Liu, Y.B.; Lang, M.D. A Drug-Free Therapeutic System for Cancer Therapy by Diselenide-Based Polymers Themselves. Adv. Healthcare Mater. 2020, 10, 2001471. [Google Scholar] [CrossRef]
- Pan, X.Q.; Driessen, F.; Zhu, X.L.; Du Prez, F.E. Selenolactone as a Building Block toward Dynamic Diselenide-Containing Polymer Architectures with Controllable Topology. ACS Macro Lett. 2017, 6, 89–92. [Google Scholar] [CrossRef]
- Li, J.G.; Liu, P. Self-Assembly of Drug–Drug Conjugates as Drug Self-Delivery System for Tumor-Specific pH-Triggered Release. Part. Part. Syst. Charact. 2019, 36, 1900113. [Google Scholar] [CrossRef]
- Zhuang, W.-R.; Wang, Y.; Cui, P.-F.; Xing, L.; Lee, J.; Kim, D.; Jiang, H.-L.; Oh, Y.-K. Applications of π-π stacking interactions in the design of drug-delivery systems. J. Control Release 2019, 294, 311–326. [Google Scholar] [CrossRef]
- Ma, G.Q.; Liu, J.; He, J.L.; Zhang, M.Z.; Ni, P.H. Dual-Responsive Polyphosphoester-Doxorubicin Prodrug Containing a Diselenide Bond: Synthesis, Characterization, and Drug Delivery. ACS Biomater. Sci. Eng. 2018, 4, 2443–2452. [Google Scholar] [CrossRef]
- Huang, Y.; Nahar, S.; Masud Alam, M.D.; Hu, S.; McVicar, D.W.; Yang, D. Reactive Oxygen Species-Sensitive Biodegradable Mesoporous Silica Nanoparticles Harboring TheraVac Elicit Tumor-Specific Immunity for Colon Tumor Treatment. ACS Nano 2023, 17, 19740–19752. [Google Scholar] [CrossRef]
- Song, Q.; Wang, X.; Wang, Y.Q.; Liang, Y.Q.; Zhou, Y.X.; Song, X.N.; He, B.; Zhang, H.; Dai, W.B.; Wang, X.Q.; et al. Reduction Responsive Self-Assembled Nanoparticles Based on Disulfide-Linked Drug-Drug Conjugate with High Drug Loading and Antitumor Efficacy. Mol. Pharm. 2016, 13, 190–201. [Google Scholar] [CrossRef]
- Hu, Y.R.; Liu, P. Diselenide-Bridged Doxorubicin Dimeric Prodrug: Synthesis and Redox-Triggered Drug Release. Molecules 2024, 29, 1709. [Google Scholar] [CrossRef]
- Hu, Y.R.; Liu, P. Design of diselenide-containing polyprodrug and its pH/redox co-triggered degradation and slow drug release for tumor-specific chemotherapy. Colloid Surf. A Physicochem. Eng. Aspects 2024, 695, 134308. [Google Scholar] [CrossRef]
- Yang, C.; Liu, P. Disulfide/α-Amide-Bridged Doxorubicin Dimeric Prodrug: Effect of Aggregation Structures on pH/GSH Dual-Triggered Drug Release. Langmuir 2024, 40, 11098–11105. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, Y.; Liu, P. Design of pH/Redox Co-Triggered Degradable Diselenide-Containing Polyprodrug via a Facile One-Pot Two-Step Approach for Tumor-Specific Chemotherapy. Molecules 2024, 29, 3837. https://doi.org/10.3390/molecules29163837
Hu Y, Liu P. Design of pH/Redox Co-Triggered Degradable Diselenide-Containing Polyprodrug via a Facile One-Pot Two-Step Approach for Tumor-Specific Chemotherapy. Molecules. 2024; 29(16):3837. https://doi.org/10.3390/molecules29163837
Chicago/Turabian StyleHu, Yanru, and Peng Liu. 2024. "Design of pH/Redox Co-Triggered Degradable Diselenide-Containing Polyprodrug via a Facile One-Pot Two-Step Approach for Tumor-Specific Chemotherapy" Molecules 29, no. 16: 3837. https://doi.org/10.3390/molecules29163837
APA StyleHu, Y., & Liu, P. (2024). Design of pH/Redox Co-Triggered Degradable Diselenide-Containing Polyprodrug via a Facile One-Pot Two-Step Approach for Tumor-Specific Chemotherapy. Molecules, 29(16), 3837. https://doi.org/10.3390/molecules29163837






