Effect of Apis mellifera syriaca Bee Venom on Glioblastoma Cancer: In Vitro and In Vivo Studies
Abstract
1. Introduction
2. Results
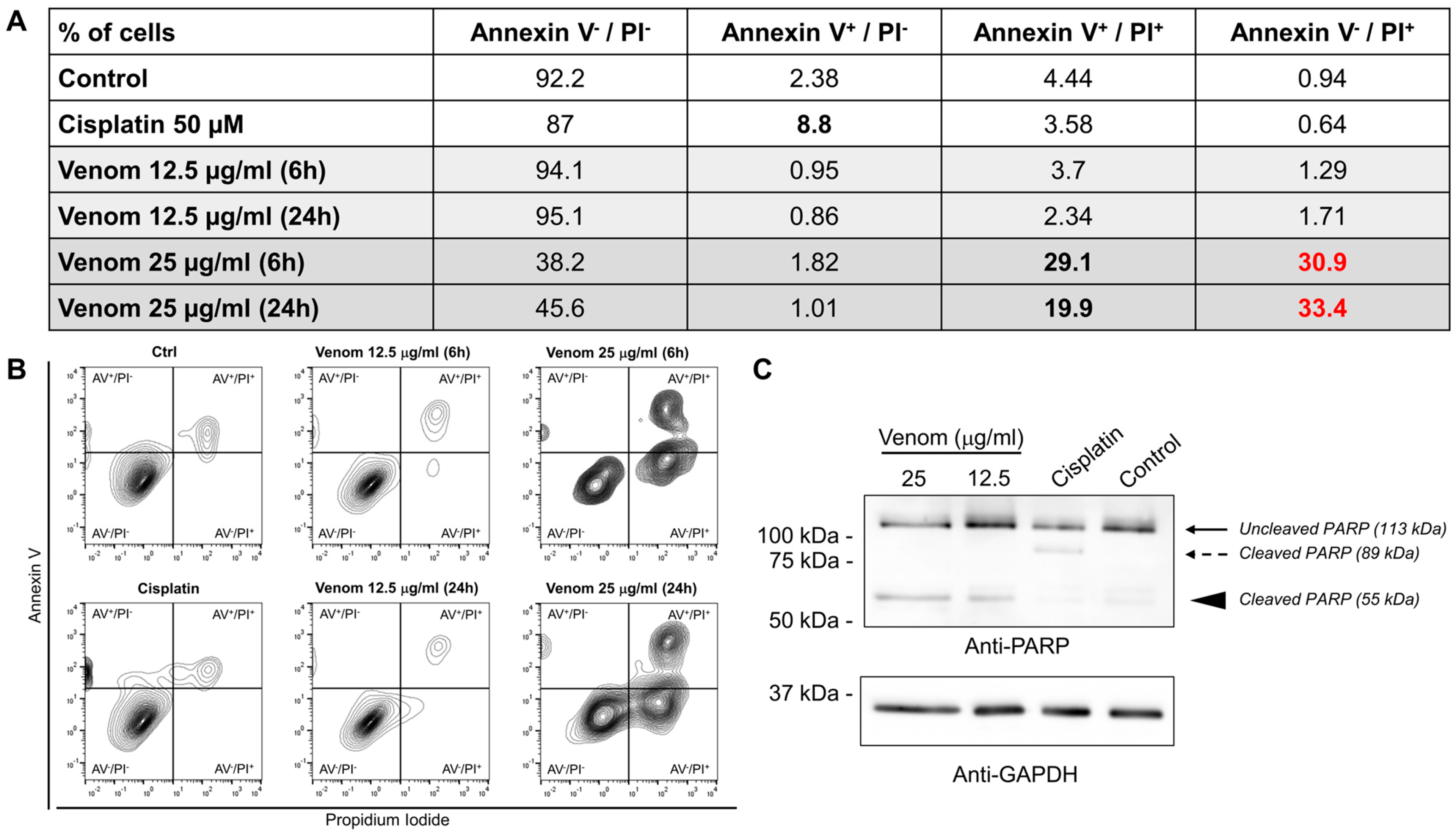
2.1. In Vitro Effect of A. mellifera syriaca Venom on Glioblastoma Cancer Cell Lines
2.2. In Vivo Effect of A. mellifera syriaca Venom in Human Glioblastoma Mouse Model
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Materials
5.2. Venom Collection
5.3. Cell Culture and Spheroid Formation
5.4. Glioblastoma Cell Proliferation
5.5. Annexin V/Propidium Iodide Staining
5.6. Cytotoxicity
5.7. C57BL/6 Mouse Handling, Tumor Injection, and Treatment Procedures
5.8. Immunohistochemistry
5.9. Hematoxylin and Eosin Staining
5.10. Confocal Microscopy Analysis
5.11. Protein Extraction and Western Blot
5.12. Statistical Analyses
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guerra, D.A.P.; Paiva, A.E.; Sena, I.F.G.; Azevedo, P.O.; Silva, W.N.; Mintz, A.; Birbrair, A. Glioblastoma-derived pericytes improves chemotherapeutic outcome. Angiogenesis 2018, 21, 667–675. [Google Scholar] [CrossRef]
- Weller, M.; Wick, W.; Aldape, K.; Brada, M.; Berger, M.; Pfister, S.M.; Nishikawa, R.; Rosenthal, M.; Wen, P.Y.; Stupp, R.; et al. Glioma. Nat. Rev. Dis. Primers 2015, 1, 15017. [Google Scholar] [CrossRef]
- Hanif, F.; Muzaffar, K.; Perveen, K.; Malhi, S.M.; Simjee, S.U. Glioblastoma Multiforme: A Review of its Epidemiology and Pathogenesis through Clinical Presentation and Treatment. Asian Pac. J. Cancer Prev. APJCP 2017, 18, 3–9. [Google Scholar]
- Jacob, F.; Salinas, R.D.; Zhang, D.Y.; Nguyen, P.T.; Schnoll, J.G.; Wong, S.Z.H.; Thokala, R.; Sheikh, S.; Saxena, D.; Prokop, S.; et al. A Patient-Derived Glioblastoma Organoid Model and Biobank Recapitulates Inter- and Intra-tumoral Heterogeneity. Cell 2020, 180, 188–204.e22. [Google Scholar] [CrossRef] [PubMed]
- Dymova, M.A.; Kuligina, E.V.; Richter, V.A. Molecular Mechanisms of Drug Resistance in Glioblastoma. Int. J. Mol. Sci. 2021, 22, 6385. [Google Scholar] [CrossRef]
- Mohammed, S.; Dinesan, M.; Ajayakumar, T. Survival and quality of life analysis in glioblastoma multiforme with adjuvant chemoradiotherapy: A retrospective study. Rep. Pract. Oncol. Radiother. 2022, 27, 1026–1036. [Google Scholar] [CrossRef]
- Jiang, H.; Yu, K.; Li, M.; Cui, Y.; Ren, X.; Yang, C.; Zhao, X.; Lin, S. Classification of Progression Patterns in Glioblastoma: Analysis of Predictive Factors and Clinical Implications. Front. Oncol. 2020, 10, 590648. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.C.; Ashley, D.M.; López, G.Y.; Malinzak, M.; Friedman, H.S.; Khasraw, M. Management of glioblastoma: State of the art and future directions. CA Cancer J. Clin. 2020, 70, 299–312. [Google Scholar] [CrossRef] [PubMed]
- McAleavey, P.G.; Walls, G.M.; Chalmers, A.J. Radiotherapy-drug combinations in the treatment of glioblastoma: A brief review. CNS Oncol. 2022, 11, CNS86. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Klockow, J.L.; Zhang, M.; Lafortune, F.; Chang, E.; Jin, L.; Wu, Y.; Daldrup-Link, H.E. Glioblastoma multiforme (GBM): An overview of current therapies and mechanisms of resistance. Pharmacol. Res. 2021, 171, 105780. [Google Scholar] [CrossRef]
- Mo, F.; Pellerino, A.; Soffietti, R.; Rudà, R. Blood–Brain Barrier in Brain Tumors: Biology and Clinical Relevance. Int. J. Mol. Sci. 2021, 22, 12654. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.-M.; Guz-Montgomery, K.; Lowe, D.B.; Saha, D. Pathogenetic Features and Current Management of Glioblastoma. Cancers 2021, 13, 856. [Google Scholar] [CrossRef] [PubMed]
- Ou, A.; Yung, W.K.A.; Majd, N. Molecular Mechanisms of Treatment Resistance in Glioblastoma. Int. J. Mol. Sci. 2020, 22, 351. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Li, K.; Qi, L. Cancer stem cells in brain tumors: From origin to clinical implications. Medcomm 2023, 4, e341. [Google Scholar] [CrossRef] [PubMed]
- Baumann, F.; Bjeljac, M.; Kollias, S.S.; Baumert, B.G.; Brandner, S.; Rousson, V.; Yonekawa, Y.; Bernays, R.L. Combined Thalidomide and Temozolomide Treatment in Patients with Glioblastoma Multiforme. J. Neuro-Oncol. 2004, 67, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Riva, M.; Imbesi, F.; Beghi, E.; Galli, C.; Citterio, A.; Trapani, P.; Sterzi, R.; Collice, M. Temozolomide and thalidomide in the treatment of glioblastoma multiforme. Anticancer Res. 2007, 27, 1067–1071. [Google Scholar] [PubMed]
- Rominiyi, O.; Vanderlinden, A.; Clenton, S.J.; Bridgewater, C.; Al-Tamimi, Y.; Collis, S.J. Tumour treating fields therapy for glioblastoma: Current advances and future directions. Br. J. Cancer 2021, 124, 697–709. [Google Scholar] [CrossRef] [PubMed]
- Shergalis, A.; Bankhead, A.; Luesakul, U.; Muangsin, N.; Neamati, N. Current Challenges and Opportunities in Treating Glioblastoma. Pharmacol. Rev. 2018, 70, 412–445. [Google Scholar] [CrossRef] [PubMed]
- Yalamarty, S.S.K.; Filipczak, N.; Li, X.; Subhan, A.; Parveen, F.; Ataide, J.A.; Rajmalani, B.A.; Torchilin, V.P. Mechanisms of Resistance and Current Treatment Options for Glioblastoma Multiforme (GBM). Cancers 2023, 15, 2116. [Google Scholar] [CrossRef]
- Park, S.-H.; Kim, M.; Lee, S.; Jung, W.; Kim, B. Therapeutic Potential of Natural Products in Treatment of Cervical Cancer: A Review. Nutrients 2021, 13, 154. [Google Scholar] [CrossRef]
- Prakash, M.D.; Stojanovska, L.; Feehan, J.; Nurgali, K.; Donald, E.L.; Plebanski, M.; Flavel, M.; Kitchen, B.; Apostolopoulos, V. Anti-cancer effects of polyphenol-rich sugarcane extract. PLoS ONE 2021, 16, e0247492. [Google Scholar] [CrossRef]
- Morjen, M.; Moslah, W.; Touihri-Baraketi, I.; Srairi-Abid, N.; Luis, J.; Marrakchi, N.; Jebali, J. Expression of the First Recombinant Anti-Tumoral Snake Venom Kunitz-Type Serine Protease Inhibitor. Toxins 2022, 14, 170. [Google Scholar] [CrossRef] [PubMed]
- Rajabi, S.; Maresca, M.; Yumashev, A.V.; Choopani, R.; Hajimehdipoor, H. The Most Competent Plant-Derived Natural Products for Targeting Apoptosis in Cancer Therapy. Biomolecules 2021, 11, 534. [Google Scholar] [CrossRef]
- Rifi, M.; Radwan, Z.; AlMonla, R.; Fajloun, Z.; Sabatier, J.M.; Kouzayha, A.; El-Sabban, M.; Mawlawi, H.; Dassouki, Z. The Lebanese Red Algae Jania rubens: Promising Biomolecules against Colon Cancer Cells. Molecules 2022, 27, 6617. [Google Scholar] [CrossRef] [PubMed]
- Touihri-Barakati, I.; Kallech-Ziri, O.; Morjen, M.; Marrakchi, N.; Luis, J.; Hosni, K. Inhibitory effect of phenolic extract from squirting cucumber (Ecballium elaterium (L.) A. Rich) seed oil on integrin-mediated cell adhesion, migration and angiogenesis. RSC Adv. 2022, 12, 31747–31756. [Google Scholar] [CrossRef] [PubMed]
- Mokhtari, R.B.; Homayouni, T.S.; Baluch, N.; Morgatskaya, E.; Kumar, S.; Das, B.; Yeger, H. Combination therapy in combating cancer. Oncotarget 2017, 8, 38022–38043. [Google Scholar] [CrossRef] [PubMed]
- García, M.C.G.; Radix, C.; Villard, C.; Breuzard, G.; Mansuelle, P.; Barbier, P.; Tsvetkov, P.O.; De Pomyers, H.; Gigmes, D.; Devred, F.; et al. Myotoxin-3 from the Pacific Rattlesnake Crotalus oreganus oreganus Venom Is a New Microtubule-Targeting Agent. Molecules 2022, 27, 8241. [Google Scholar] [CrossRef]
- Haddoub, C.; Rima, M.; Heurtebise, S.; Lawand, M.; Jundi, D.; Sadek, R.; Amigorena, S.; Fajloun, Z.; Karam, M.C. Cytotoxic effect of Montivipera bornmuelleri’s venom on cancer cell lines: In vitro and in vivo studies. PeerJ 2020, 8, e9909. [Google Scholar] [CrossRef]
- Offor, B.C.; Piater, L.A. Snake venom toxins: Potential anticancer therapeutics. J. Appl. Toxicol. 2023, 44, 666–685. [Google Scholar] [CrossRef]
- Wehbe, R.; Frangieh, J.; Rima, M.; El Obeid, D.; Sabatier, J.-M.; Fajloun, Z. Bee Venom: Overview of Main Compounds and Bioactivities for Therapeutic Interests. Molecules 2019, 24, 2997. [Google Scholar] [CrossRef]
- Sung, S.-H.; Kim, J.-W.; Han, J.-E.; Shin, B.-C.; Park, J.-K.; Lee, G. Animal Venom for Medical Usage in Pharmacopuncture in Korean Medicine: Current Status and Clinical Implication. Toxins 2021, 13, 105. [Google Scholar] [CrossRef]
- Małek, A.; Strzemski, M.; Kurzepa, J.; Kurzepa, J. Can Bee Venom Be Used as Anticancer Agent in Modern Medicine? Cancers 2023, 15, 3714. [Google Scholar] [CrossRef]
- Kim, D.H.; Yang, E.J.; Lee, J.; Chang, J.H. Ginkgo biloba Leaf Extract Regulates Cell Proliferation and Gastric Cancer Cell Death. Biomed. Sci. Lett. 2022, 28, 92–100. [Google Scholar] [CrossRef]
- He, C.; Zhang, Z.; Ding, Y.; Xue, K.; Wang, X.; Yang, R.; An, Y.; Liu, D.; Hu, C.; Tang, Q. LRP1-mediated pH-sensitive polymersomes facilitate combination therapy of glioblastoma in vitro and in vivo. J. Nanobiotechnology 2021, 19, 29. [Google Scholar] [CrossRef]
- Sisakht, M.; Mashkani, B.; Bazi, A.; Ostadi, H.; Zare, M.; Avval, F.Z.; Sadeghnia, H.R.; Mojarad, M.; Nadri, M.; Ghorbani, A.; et al. Bee venom induces apoptosis and suppresses matrix metaloprotease-2 expression in human glioblastoma cells. Rev. Bras. Farm. 2017, 27, 324–328. [Google Scholar] [CrossRef]
- Małek, A.; Kocot, J.; Mitrowska, K.; Posyniak, A.; Kurzepa, J. Bee Venom Effect on Glioblastoma Cells Viability and Gelatinase Secretion. Front. Neurosci. 2022, 16, 792970. [Google Scholar] [CrossRef]
- Ertilav, K.; Nazıroğlu, M. Honey bee venom melittin increases the oxidant activity of cisplatin and kills human glioblastoma cells by stimulating the TRPM2 channel. Toxicon 2023, 222, 106993. [Google Scholar] [CrossRef]
- Yaacoub, C.; Wehbe, R.; Salma, Y.; El-Obeid, D.; El Bersaoui, R.; Coutard, B.; Fajloun, Z. Apis mellifera syriaca Venom: Evaluation of Its Anticoagulant Effect, Proteolytic Activity, and Cytotoxicity along with Its Two Main Compounds—MEL and PLA2—On HeLa Cancer Cells. Molecules 2022, 27, 1653. [Google Scholar] [CrossRef] [PubMed]
- Nehme, H.; Ayde, H.; El Obeid, D.; Sabatier, J.M.; Fajloun, Z. Potential Inhibitory Effect of Apis mellifera’s Venom and of Its Two Main Components—Melittin and PLA2—On Escherichia coli F1F0-ATPase. Antibiotics 2020, 9, 824. [Google Scholar] [CrossRef] [PubMed]
- Frangieh, J.; Salma, Y.; Haddad, K.; Mattei, C.; Legros, C.; Fajloun, Z.; El Obeid, D. First Characterization of The Venom from Apis mellifera syriaca, A Honeybee from The Middle East Region. Toxins 2019, 11, 191. [Google Scholar] [CrossRef]
- Yaacoub, C.; Rifi, M.; El-Obeid, D.; Mawlawi, H.; Sabatier, J.-M.; Coutard, B.; Fajloun, Z. The Cytotoxic Effect of Apis mellifera Venom with a Synergistic Potential of Its Two Main Components—Melittin and PLA2—On Colon Cancer HCT116 Cell Lines. Molecules 2021, 26, 2264. [Google Scholar] [CrossRef] [PubMed]
- Gobeil, S.; Boucher, C.C.; Nadeau, D.; Poirier, G.G. Characterization of the necrotic cleavage of poly(ADP-ribose) polymerase (PARP-1): Implication of lysosomal proteases. Cell Death Differ. 2001, 8, 588–594. [Google Scholar] [CrossRef]
- Li, R.; Tao, T.; Ren, Q.; Xie, S.; Gao, X.; Wu, J.; Chen, D.; Xu, C. Key Genes Are Associated with the Prognosis of Glioma, and Melittin Can Regulate the Expression of These Genes in Glioma U87 Cells. BioMed Res. Int. 2022, 2022, 7033478. [Google Scholar] [CrossRef]
- Rady, I.; Siddiqui, I.A.; Rady, M.; Mukhtar, H. Melittin, a major peptide component of bee venom, and its conjugates in cancer therapy. Cancer Lett. 2017, 402, 16–31. [Google Scholar] [CrossRef]
- Lee, M.-T.; Sun, T.-L.; Hung, W.-C.; Huang, H.W. Process of inducing pores in membranes by melittin. Proc. Natl. Acad. Sci. USA 2013, 110, 14243–14248. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Chen, T.; Zhang, N.; Yang, M.; Li, B.; Lu, X.; Cao, X.; Ling, C. Melittin, a Major Component of Bee Venom, Sensitizes Human Hepatocellular Carcinoma Cells to Tumor Necrosis Factor-related Apoptosis-inducing Ligand (TRAIL)-induced Apoptosis by Activating CaMKII-TAK1-JNK/p38 and Inhibiting IκBα Kinase-NFκB. J. Biol. Chem. 2009, 284, 3804–3813. [Google Scholar] [CrossRef]
- Shin, H.-J.; Kwon, H.-K.; Lee, J.-H.; Gui, X.; Achek, A.; Kim, J.-H.; Choi, S. Doxorubicin-induced necrosis is mediated by poly-(ADP-ribose) polymerase 1 (PARP1) but is independent of p53. Sci. Rep. 2015, 5, 15798. [Google Scholar] [CrossRef]
- Yu, J.E.; Kim, Y.; Hong, D.E.; Lee, D.W.; Chang, J.Y.; Yoo, S.S.; Kim, M.J.; Son, D.J.; Yun, J.; Han, S.-B.; et al. Bee Venom Triggers Autophagy-Induced Apoptosis in Human Lung Cancer Cells via the mTOR Signaling Pathway. J. Oncol. 2022, 2022, 8916464. [Google Scholar] [CrossRef] [PubMed]
- Tetikoğlu, S.; Çelik-Uzuner, S. Bee Venom Induces the Interaction between Phosphorylated Histone Variant, H2AX, and the Intracellular Site of beta-Actin in Liver and Breast Cancer Cells. Chem. Biodivers. 2023, 20, e202300401. [Google Scholar] [CrossRef]
- Lee, H.-S.; Kim, Y.S.; Lee, K.-S.; Seo, H.-S.; Lee, C.-Y.; Kim, K.K. Detoxification of Bee Venom Increases Its Anti-inflammatory Activity and Decreases Its Cytotoxicity and Allergenic Activity. Appl. Biochem. Biotechnol. 2021, 193, 4068–4082. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Kum, Y.S.; Park, Y.Y.; Park, J.H.; Kim, S.J.; Lee, W.R.; Lee, K.G.; Han, S.M.; Park, K.K. The Protective Effect of Bee Venom against Ethanol-Induced Hepatic Injury via Regulation of the Mitochondria-Related Apoptotic Pathway. Basic Clin. Pharmacol. Toxicol. 2010, 107, 619–624. [Google Scholar] [CrossRef] [PubMed]
- Kong, G.M.; Tao, W.H.; Diao, Y.L.; Fang, P.H.; Wang, J.J.; Bo, P.; Qian, F. Melittin induces human gastric cancer cell apoptosis via activation of mitochondrial pathway. World J. Gastroenterol. 2016, 22, 3186. [Google Scholar] [CrossRef] [PubMed]
- Putz, T.; Ramoner, R.; Gander, H.; Rahm, A.; Bartsch, G.; Thurnher, M. Antitumor action and immune activation through cooperation of bee venom secretory phospholipase A2 and phosphatidylinositol-(3,4)-bisphosphate. Cancer Immunol. Immunother. 2006, 55, 1374–1383. [Google Scholar] [CrossRef] [PubMed]
- Shi, P.; Xie, S.; Yang, J.; Zhang, Y.; Han, S.; Su, S.; Yao, H. Pharmacological effects and mechanisms of bee venom and its main components: Recent progress and perspective. Front. Pharmacol. 2022, 13, 1001553. [Google Scholar] [CrossRef] [PubMed]
- Pandey, P.; Khan, F.; Khan, M.A.; Kumar, R.; Upadhyay, T.K. An Updated Review Summarizing the Anticancer Efficacy of Melittin from Bee Venom in Several Models of Human Cancers. Nutrients 2023, 15, 3111. [Google Scholar] [CrossRef]
- Sahyoun, C.; Krezel, W.; Mattei, C.; Sabatier, J.-M.; Legros, C.; Fajloun, Z.; Rima, M. Neuro- and Cardiovascular Activities of Montivipera bornmuelleri Snake Venom. Biology 2022, 11, 888. [Google Scholar] [CrossRef]
- Rima, M.; Lattouf, Y.; Abi Younes, M.; Bullier, E.; Legendre, P.; Mangin, J.M.; Hong, E. Dynamic regulation of the cholinergic system in the spinal central nervous system. Sci. Rep. 2020, 10, 15338. Available online: https://pubmed.ncbi.nlm.nih.gov/32948826 (accessed on 1 June 2024). [CrossRef]



| Molecule | Composition, Molecular Weight | Abundance | Function |
|---|---|---|---|
| Apamin | 18 a.a., 2027 Da | + | Neurotoxin |
| Melittin | 26 a.a., 2846.4 Da | +++ | Main component and the major pain-producing substance of honeybee venom |
| Phospholipase A2 | 128 a.a., 18,964 Da | +++ | Enzyme responsible for phospholipid hydrolysis |
| MCD-peptide | 22 a.a., 2599.8 Da | + | Potent and selective blocker of KV1.1 and KV1.2 channels |
| Hyaluronidase | 349 a.a., 53,875.6 Da | + | Enzyme that temporarily and reversibly depolymerizes hyaluronic acid |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chahla, C.; Rima, M.; Mouawad, C.; Roufayel, R.; Kovacic, H.; El Obeid, D.; Sabatier, J.-M.; Luis, J.; Fajloun, Z.; El-Waly, B. Effect of Apis mellifera syriaca Bee Venom on Glioblastoma Cancer: In Vitro and In Vivo Studies. Molecules 2024, 29, 3950. https://doi.org/10.3390/molecules29163950
Chahla C, Rima M, Mouawad C, Roufayel R, Kovacic H, El Obeid D, Sabatier J-M, Luis J, Fajloun Z, El-Waly B. Effect of Apis mellifera syriaca Bee Venom on Glioblastoma Cancer: In Vitro and In Vivo Studies. Molecules. 2024; 29(16):3950. https://doi.org/10.3390/molecules29163950
Chicago/Turabian StyleChahla, Charbel, Mohamad Rima, Charbel Mouawad, Rabih Roufayel, Hervé Kovacic, Dany El Obeid, Jean-Marc Sabatier, José Luis, Ziad Fajloun, and Bilal El-Waly. 2024. "Effect of Apis mellifera syriaca Bee Venom on Glioblastoma Cancer: In Vitro and In Vivo Studies" Molecules 29, no. 16: 3950. https://doi.org/10.3390/molecules29163950
APA StyleChahla, C., Rima, M., Mouawad, C., Roufayel, R., Kovacic, H., El Obeid, D., Sabatier, J.-M., Luis, J., Fajloun, Z., & El-Waly, B. (2024). Effect of Apis mellifera syriaca Bee Venom on Glioblastoma Cancer: In Vitro and In Vivo Studies. Molecules, 29(16), 3950. https://doi.org/10.3390/molecules29163950








