Hungry Neurons: Metabolic Insights on Seizure Dynamics
Abstract
:1. Introduction
2. Metabolism and Seizures—Patients’ Studies
3. Metabolism and Seizures—Preclinical Studies
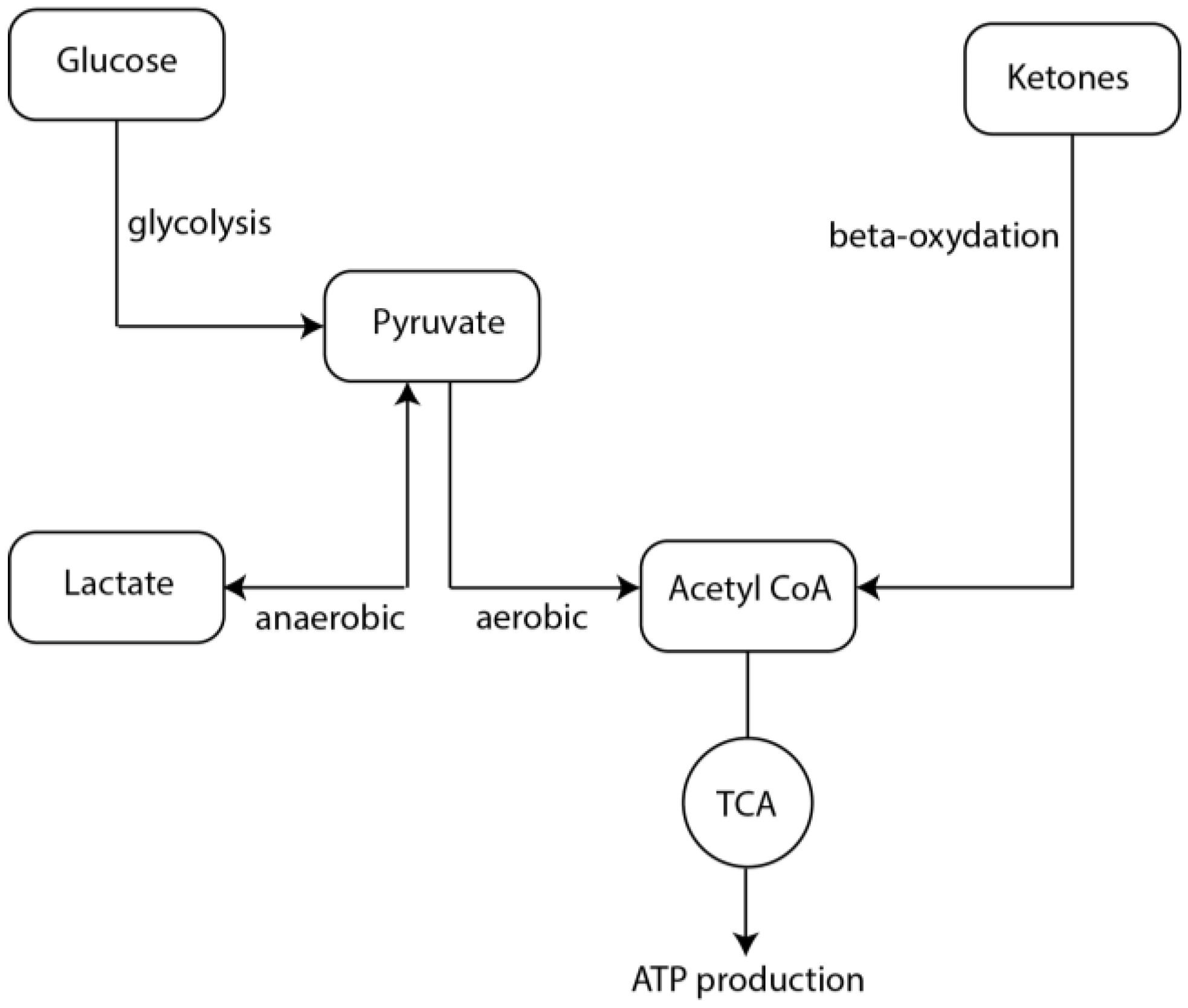
4. Mechanisms of Altered Metabolism and Epileptogenesis
5. Metabolism during Seizures
6. Metabolism and Seizure Termination
7. Conclusions
Acknowledgments
Conflicts of Interest
References
- Foundation, E. Epilepsy Statistics. Available online: http://www.epilepsy.com/learn/epilepsy-statistics (accessed on 12 July 2017).
- DiNuzzo, M.; Mangia, S.; Maraviglia, B.; Giove, F. Physiological bases of the K+ and the glutamate/GABA hypotheses of epilepsy. Epilepsy Res. 2014, 108, 995–1012. [Google Scholar] [CrossRef] [PubMed]
- Rajakulendran, S.; Hanna, M.G. The role of calcium channels in epilepsy. Cold Spring Harb. Perspect. Med. 2016, 6, a022723. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, D.I.; Isom, L.L.; Petrou, S. Role of sodium channels in epilepsy. Cold Spring Harb. Perspect. Med. 2016, 6. [Google Scholar] [CrossRef] [PubMed]
- Raimondo, J.V.; Burman, R.J.; Katz, A.A.; Akerman, C.J. Ion dynamics during seizures. Front. Cell. Neurosci. 2015, 9, 419. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Brunengraber, H. Glutamate, a window on liver intermediary metabolism. J. Nutr. 2000, 130, 991S–994S. [Google Scholar] [PubMed]
- Rutter, J.; Winge, D.R.; Schiffman, J.D. Succinate dehydrogenase—Assembly, regulation and role in human disease. Mitochondrion 2010, 10, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Semenza, G.L. Oxygen-dependent regulation of mitochondrial respiration by hypoxia-inducible factor 1. Biochem. J. 2007, 405, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Diehl, B.; Knecht, S.; Deppe, M.; Young, C.; Stodieck, S.R. Cerebral hemodynamic response to generalized spike-wave discharges. Epilepsia 1998, 39, 1284–1289. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Suh, M.; Ma, H.; Perry, C.; Geneslaw, A.; Schwartz, T.H. Focal increases in perfusion and decreases in hemoglobin oxygenation precede seizure onset in spontaneous human epilepsy. Epilepsia 2007, 48, 2059–2067. [Google Scholar] [CrossRef] [PubMed]
- Federico, P.; Abbott, D.F.; Briellmann, R.S.; Harvey, A.S.; Jackson, G.D. Functional MRI of the pre-ictal state. Brain J. Neurol. 2005, 128, 1811–1817. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, C.; Serles, W.; Leutmezer, F.; Pataraia, E.; Aull, S.; Czech, T.; Pietrzyk, U.; Relic, A.; Podreka, I. Preictal SPECT in temporal lobe epilepsy: Regional cerebral blood flow is increased prior to electroencephalography-seizure onset. J. Nuclear Med. Off. Publ. Soc. Nucl. Med. 1998, 39, 978–982. [Google Scholar]
- Weinand, M.E.; Carter, L.P.; el-Saadany, W.F.; Sioutos, P.J.; Labiner, D.M.; Oommen, K.J. Cerebral blood flow and temporal lobe epileptogenicity. J. Neurosurg. 1997, 86, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Boling, W.W.; Lancaster, M.; Kraszpulski, M.; Palade, A.; Marano, G.; Puce, A. Fluorodeoxyglucose-positron emission tomographic imaging for the diagnosis of mesial temporal lobe epilepsy. Neurosurgery 2008, 63, 1130–1138; discussion 1138. [Google Scholar] [CrossRef] [PubMed]
- Liew, C.J.; Lim, Y.M.; Bonwetsch, R.; Shamim, S.; Sato, S.; Reeves-Tyer, P.; Herscovitch, P.; Dustin, I.; Bagic, A.; Giovacchini, G.; et al. 18F-FCWAY and 18F-FDG PET in MRI-negative temporal lobe epilepsy. Epilepsia 2009, 50, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Vinton, A.B.; Carne, R.; Hicks, R.J.; Desmond, P.M.; Kilpatrick, C.; Kaye, A.H.; O’Brien, T.J. The extent of resection of FDG-PET hypometabolism relates to outcome of temporal lobectomy. Brain: J. Neurol. 2007, 130, 548–560. [Google Scholar] [CrossRef] [PubMed]
- Lake, E.M.; Bazzigaluppi, P.; Stefanovic, B. Functional magnetic resonance imaging in chronic ischaemic stroke. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2016, 371. [Google Scholar] [CrossRef] [PubMed]
- Urenjak, J.; Williams, S.R.; Gadian, D.G.; Noble, M. Specific expression of N-acetylaspartate in neurons, oligodendrocyte-type-2 astrocyte progenitors, and immature oligodendrocytes in vitro. J. Neurochem. 1992, 59, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Patel, T.B.; Clark, J.B. Synthesis of N-acetyl-L-aspartate by rat brain mitochondria and its involvement in mitochondrial/cytosolic carbon transport. Biochem. J. 1979, 184, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, F.B. The enzymatic synthesis of N-acetyl-L-aspartic acid by subcellular preparations of rat brain. J. Biol. Chem. 1969, 244, 4257–4260. [Google Scholar] [PubMed]
- Heales, S.J.; Davies, S.E.; Bates, T.E.; Clark, J.B. Depletion of brain glutathione is accompanied by impaired mitochondrial function and decreased N-acetyl aspartate concentration. Neurochem. Res. 1995, 20, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Bates, T.E.; Strangward, M.; Keelan, J.; Davey, G.P.; Munro, P.M.; Clark, J.B. Inhibition of N-acetylaspartate production: Implications for 1H MRS studies in vivo. Neuroreport 1996, 7, 1397–1400. [Google Scholar] [CrossRef] [PubMed]
- Hetherington, H.; Kuzniecky, R.; Pan, J.; Mason, G.; Morawetz, R.; Harris, C.; Faught, E.; Vaughan, T.; Pohost, G. Proton nuclear magnetic resonance spectroscopic imaging of human temporal lobe epilepsy at 4.1 T. Ann. Neurol. 1995, 38, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Cendes, F.; Caramanos, Z.; Andermann, F.; Dubeau, F.; Arnold, D.L. Proton magnetic resonance spectroscopic imaging and magnetic resonance imaging volumetry in the lateralization of temporal lobe epilepsy: A series of 100 patients. Ann. Neurol. 1997, 42, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Connelly, A.; Jackson, G.D.; Duncan, J.S.; King, M.D.; Gadian, D.G. Magnetic resonance spectroscopy in temporal lobe epilepsy. Neurology 1994, 44, 1411–1417. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.A. Temporal lobe hypometabolism. Neurology 1994, 44, 583–585. [Google Scholar] [CrossRef] [PubMed]
- Foldvary, N.; Lee, N.; Hanson, M.W.; Coleman, R.E.; Hulette, C.M.; Friedman, A.H.; Bej, M.D.; Radtke, R.A. Correlation of hippocampal neuronal density and FDG-PET in mesial temporal lobe epilepsy. Epilepsia 1999, 40, 26–29. [Google Scholar] [CrossRef] [PubMed]
- Caudle, W.M.; Pan, S.; Shi, M.; Quinn, T.; Hoekstra, J.; Beyer, R.P.; Montine, T.J.; Zhang, J. Proteomic identification of proteins in the human brain: Towards a more comprehensive understanding of neurodegenerative disease. Proteom. Clin. Appl. 2008, 2, 1484–1497. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.W.; Bebin, E.M.; Chu, W.J.; Hetherington, H.P. Ketosis and epilepsy: 31P spectroscopic imaging at 4.1 T. Epilepsia 1999, 40, 703–707. [Google Scholar] [CrossRef]
- Bough, K. Energy metabolism as part of the anticonvulsant mechanism of the ketogenic diet. Epilepsia 2008, 49, 91–93. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.R.; O’Brien, T.J.; Stefanidou, M.; Kuzniecky, R.I. Neuroimaging the epileptogenic process. Neurother. J. Am. Soc. Exp. Neurother. 2014, 11, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Makiranta, M.; Ruohonen, J.; Suominen, K.; Niinimaki, J.; Sonkajarvi, E.; Kiviniemi, V.; Seppanen, T.; Alahuhta, S.; Jantti, V.; Tervonen, O. BOLD signal increase preceeds EEG spike activity—A dynamic penicillin induced focal epilepsy in deep anesthesia. NeuroImage 2005, 27, 715–724. [Google Scholar] [CrossRef] [PubMed]
- Hoshi, Y.; Tamura, M. Cerebral oxygenation state in chemically-induced seizures in the rat—Study by near infrared spectrophotometry. Adv. Exp. Med. Biol. 1992, 316, 137–142. [Google Scholar] [PubMed]
- Zhao, M.; Nguyen, J.; Ma, H.; Nishimura, N.; Schaffer, C.B.; Schwartz, T.H. Preictal and ictal neurovascular and metabolic coupling surrounding a seizure focus. J. Neurosci. Off. J. Soc. Neurosci. 2011, 31, 13292–13300. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Ma, H.; Suh, M.; Schwartz, T.H. Spatiotemporal dynamics of perfusion and oximetry during ictal discharges in the rat neocortex. J. Neurosci. Off. J. Soc. Neurosci. 2009, 29, 2814–2823. [Google Scholar] [CrossRef] [PubMed]
- Litt, B.; Esteller, R.; Echauz, J.; D’Alessandro, M.; Shor, R.; Henry, T.; Pennell, P.; Epstein, C.; Bakay, R.; Dichter, M.; et al. Epileptic seizures may begin hours in advance of clinical onset: A report of five patients. Neuron 2001, 30, 51–64. [Google Scholar] [CrossRef]
- Ingvar, M. Cerebral blood flow and metabolic rate during seizures. Relationship to epileptic brain damage. Ann. N. Y. Acad. Sci. 1986, 462, 194–206. [Google Scholar] [CrossRef] [PubMed]
- Pereira de Vasconcelos, A.; Ferrandon, A.; Nehlig, A. Local cerebral blood flow during lithium-pilocarpine seizures in the developing and adult rat: Role of coupling between blood flow and metabolism in the genesis of neuronal damage. J. Cereb. Blood Flow Metab. Off. J. Int. Soc. Cereb. Blood Flow Metab. 2002, 22, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Ingvar, M.; Siesjo, B.K. Local blood flow and glucose consumption in the rat brain during sustained bicuculline-induced seizures. Acta Neurol. Scand. 1983, 68, 129–144. [Google Scholar] [CrossRef] [PubMed]
- Alvestad, S.; Hammer, J.; Eyjolfsson, E.; Qu, H.; Ottersen, O.P.; Sonnewald, U. Limbic structures show altered glial-neuronal metabolism in the chronic phase of kainate induced epilepsy. Neurochem. Res. 2008, 33, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Cloix, J.F.; Hevor, T. Epilepsy, regulation of brain energy metabolism and neurotransmission. Curr. Med. Chem. 2009, 16, 841–853. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Gao, F.; Wang, S.; Ding, Y.; Zhang, H.; Wang, J.; Ding, M.P. In vivo mapping of temporospatial changes in glucose utilization in rat brain during epileptogenesis: An 18F-fluorodeoxyglucose-small animal positron emission tomography study. Neuroscience 2009, 162, 972–979. [Google Scholar] [CrossRef] [PubMed]
- Jupp, B.; Williams, J.; Binns, D.; Hicks, R.J.; Cardamone, L.; Jones, N.; Rees, S.; O’Brien, T.J. Hypometabolism precedes limbic atrophy and spontaneous recurrent seizures in a rat model of TLE. Epilepsia 2012, 53, 1233–1244. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.R.; Cardamone, L.; Liu, Y.R.; Hogan, R.E.; Maccotta, L.; Wright, D.K.; Zheng, P.; Koe, A.; Gregoire, M.C.; Williams, J.P.; et al. Can structural or functional changes following traumatic brain injury in the rat predict epileptic outcome? Epilepsia 2013, 54, 1240–1250. [Google Scholar] [CrossRef] [PubMed]
- Samokhina, E.; Popova, I.; Malkov, A.; Ivanov, A.I.; Papadia, D.; Osypov, A.; Molchanov, M.; Paskevich, S.; Fisahn, A.; Zilberter, M.; et al. Chronic inhibition of brain glycolysis initiates epileptogenesis. J. Neurosci. Res. 2017, 95, 2195–2206. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.M.; Park, G.Y.; Im, K.C.; Kim, S.T.; Woo, C.W.; Chung, J.H.; Kim, K.S.; Kim, J.S.; Shon, Y.M.; Kim, Y.I.; et al. Changes in glucose metabolism and metabolites during the epileptogenic process in the lithium-pilocarpine model of epilepsy. Epilepsia 2012, 53, 860–869. [Google Scholar] [CrossRef] [PubMed]
- King, L.J.; Lowry, O.H.; Passonneau, J.V.; Venson, V. Effects of convulsants on energy reserves in the cerebral cortex. J. Neurochem. 1967, 14, 599–611. [Google Scholar] [CrossRef] [PubMed]
- Folbergrova, J.; Druga, R.; Haugvicova, R.; Mares, P.; Otahal, J. Anticonvulsant and neuroprotective effect of (S)-3,4-dicarboxyphenylglycine against seizures induced in immature rats by homocysteic acid. Neuropharmacology 2008, 54, 665–675. [Google Scholar] [CrossRef] [PubMed]
- Folbergrova, J. Energy metabolism of mouse cerebral cortex during homocysteine convulsions. Brain Res. 1974, 81, 443–454. [Google Scholar] [CrossRef]
- Nahorski, S.R.; Roberts, D.J.; Stewart, G.G. Some neurochemical aspects of pentamethylenetetrazole convulsive activity in rat brain. J. Neurochem. 1970, 17, 621–631. [Google Scholar] [CrossRef] [PubMed]
- Folbergrova, J.; Ingvar, M.; Siesjo, B.K. Metabolic changes in cerebral cortex, hippocampus, and cerebellum during sustained bicuculline-induced seizures. J. Neurochem. 1981, 37, 1228–1238. [Google Scholar] [CrossRef] [PubMed]
- Chapman, A.G.; Meldrum, B.S.; Siesjo, B.K. Cerebral metabolic changes during prolonged epileptic seizures in rats. J. Neurochem. 1977, 28, 1025–1035. [Google Scholar] [CrossRef] [PubMed]
- Bak, L.K.; Schousboe, A.; Waagepetersen, H.S. The glutamate/GABA-glutamine cycle: Aspects of transport, neurotransmitter homeostasis and ammonia transfer. J. Neurochem. 2006, 98, 641–653. [Google Scholar] [CrossRef] [PubMed]
- Pumain, R.; Ahmed, M.S.; Kurcewicz, I.; Trottier, S.; Louvel, J.; Turak, B.; Devaux, B.; Laschet, J. Lability of GABAA receptor function in human partial epilepsy: Possible relationship to hypometabolism. Epilepsia 2008, 49, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Hyder, F.; Patel, A.B.; Gjedde, A.; Rothman, D.L.; Behar, K.L.; Shulman, R.G. Neuronal-glial glucose oxidation and glutamatergic-GABAergic function. J. Cereb. Blood Flow Metab.: Off. J. Int. Soc. Cereb. Blood Flow Metab. 2006, 26, 865–877. [Google Scholar] [CrossRef] [PubMed]
- Laschet, J.J.; Minier, F.; Kurcewicz, I.; Bureau, M.H.; Trottier, S.; Jeanneteau, F.; Griffon, N.; Samyn, B.; van Beeumen, J.; Louvel, J.; et al. Glyceraldehyde-3-phosphate dehydrogenase is a GABAA receptor kinase linking glycolysis to neuronal inhibition. J. Neurosci. Official J. Soc. Neurosci. 2004, 24, 7614–7622. [Google Scholar] [CrossRef] [PubMed]
- Pumain, R.; Laschet, J. A key glycolytic enzyme plays a dual role in GABAergic neurotransmission and in human epilepsy. Crit. Rev. Neurobiol. 2006, 18, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Rolfe, D.F.; Brown, G.C. Cellular energy utilization and molecular origin of standard metabolic rate in mammals. Physiol. Rev. 1997, 77, 731–758. [Google Scholar] [PubMed]
- Reime Kinjo, E.; Arida, R.M.; Mara de Oliveira, D.; da Silva Fernandes, M.J. The Na+/K+-ATPase activity is increased in the hippocampus after multiple status epilepticus induced by pilocarpine in developing rats. Brain Res. 2007, 1138, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Isaksen, T.J.; Lykke-Hartmann, K. Insights into the pathology of the α2-Na+/K+-ATPase in neurological disorders; lessons from animal models. Front. Physiol. 2016, 7, 161. [Google Scholar] [CrossRef] [PubMed]
- Renkawek, K.; Renier, W.O.; de Pont, J.J.; Vogels, O.J.; Gabreels, F.J. Neonatal status convulsivus, spongiform encephalopathy, and low activity of Na+/K+-ATPase in the brain. Epilepsia 1992, 33, 58–64. [Google Scholar] [CrossRef] [PubMed]
- De Souza Wyse, A.T.; Streck, E.L.; Worm, P.; Wajner, A.; Ritter, F.; Netto, C.A. Preconditioning prevents the inhibition of Na+/K+-ATPase activity after brain ischemia. Neurochem. Res. 2000, 25, 971–975. [Google Scholar] [CrossRef] [PubMed]
- Silva, L.F.; Hoffmann, M.S.; Rambo, L.M.; Ribeiro, L.R.; Lima, F.D.; Furian, A.F.; Oliveira, M.S.; Fighera, M.R.; Royes, L.F. The involvement of Na+/K+-ATPase activity and free radical generation in the susceptibility to pentylenetetrazol-induced seizures after experimental traumatic brain injury. J. Neurol. Sci. 2011, 308, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Maheandiran, M.; Mylvaganam, S.; Wu, C.; El-Hayek, Y.; Sugumar, S.; Hazrati, L.; del Campo, M.; Giacca, A.; Zhang, L.; Carlen, P.L. Severe hypoglycemia in a juvenile diabetic rat model: Presence and severity of seizures are associated with mortality. PLoS ONE 2013, 8, e83168. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Batra, A.; Hirve, M.; Chowdhury, D.; Khwaja, G.A.; Mishra, P.K. Paroxysmal dystonic choreoathetosis with symptomatic seizures secondary to hypoglycemia caused by insulinoma. Ann. Ind. Acad. Neurol. 2011, 14, 313–315. [Google Scholar] [CrossRef] [PubMed]
- Vespa, P.M.; Miller, C.; McArthur, D.; Eliseo, M.; Etchepare, M.; Hirt, D.; Glenn, T.C.; Martin, N.; Hovda, D. Nonconvulsive electrographic seizures after traumatic brain injury result in a delayed, prolonged increase in intracranial pressure and metabolic crisis. Crit. Care Med. 2007, 35, 2830–2836. [Google Scholar] [CrossRef] [PubMed]
- Pitkanen, A.; Roivainen, R.; Lukasiuk, K. Development of epilepsy after ischaemic stroke. Lancet Neurol. 2016, 15, 185–197. [Google Scholar] [CrossRef]
- Hasselbalch, S.G.; Knudsen, G.M.; Jakobsen, J.; Hageman, L.P.; Holm, S.; Paulson, O.B. Blood-brain barrier permeability of glucose and ketone bodies during short-term starvation in humans. Am. J. Physiol. 1995, 268, E1161–E1166. [Google Scholar] [PubMed]
- Achanta, L.B.; Rowlands, B.D.; Thomas, D.S.; Housley, G.D.; Rae, C.D. β-Hydroxybutyrate boosts mitochondrial and neuronal metabolism but is not preferred over glucose under activated conditions. Neurochem. Res. 2017, 42, 1710–1723. [Google Scholar] [CrossRef] [PubMed]
- LaManna, J.C.; Salem, N.; Puchowicz, M.; Erokwu, B.; Koppaka, S.; Flask, C.; Lee, Z. Ketones suppress brain glucose consumption. Adv. Exp. Med. Biol. 2009, 645, 301–306. [Google Scholar] [PubMed]
- Chang, A.S.; D’Alecy, L.G. Hypoxia and β-hydroxybutyrate acutely reduce glucose extraction by the brain in anesthetized dogs. Can. J. Physiol. Pharmacol. 1993, 71, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Julio-Amilpas, A.; Montiel, T.; Soto-Tinoco, E.; Geronimo-Olvera, C.; Massieu, L. Protection of hypoglycemia-induced neuronal death by β-hydroxybutyrate involves the preservation of energy levels and decreased production of reactive oxygen species. J. Cereb. Blood Flow Metab. Off. J. Int. Soc. Cereb. Blood Flow Metab. 2015, 35, 851–860. [Google Scholar] [CrossRef] [PubMed]
- Clanton, R.M.; Wu, G.; Akabani, G.; Aramayo, R. Control of seizures by ketogenic diet-induced modulation of metabolic pathways. Amino Acids 2017, 49, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Rogovik, A.L.; Goldman, R.D. Ketogenic diet for treatment of epilepsy. Can. Fam. Phys. Med. Fam. Can. 2010, 56, 540–542. [Google Scholar]
- Schoeler, N.E.; Cross, J.H. Ketogenic dietary therapies in adults with epilepsy: A practical guide. Pract. Neurol. 2016, 16, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Schugar, R.C.; Crawford, P.A. Low-carbohydrate ketogenic diets, glucose homeostasis, and nonalcoholic fatty liver disease. Curr. Opin. Clin. Nutr. Metab. Care 2012, 15, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Borges, K. Mouse models: The ketogenic diet and polyunsaturated fatty acids. Epilepsia 2008, 49, 64–66. [Google Scholar] [CrossRef] [PubMed]
- Yellen, G. Ketone bodies, glycolysis, and KATP channels in the mechanism of the ketogenic diet. Epilepsia 2008, 49, 80–82. [Google Scholar] [CrossRef] [PubMed]
- Simeone, T.A.; Simeone, K.A.; Rho, J.M. Ketone bodies as anti-seizure agents. Neurochem. Res. 2017, 42, 2011–2018. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Berg, J.; Yellen, G. Ketogenic diet metabolites reduce firing in central neurons by opening K(ATP) channels. J. Neurosci. Off. J. Soc. Neurosci. 2007, 27, 3618–3625. [Google Scholar] [CrossRef] [PubMed]
- Samala, R.; Klein, J.; Borges, K. The ketogenic diet changes metabolite levels in hippocampal extracellular fluid. Neurochem. Int. 2011, 58, 5–8. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, M., Jr.; Ruskin, D.N.; Masino, S.A. Metabolic autocrine regulation of neurons involves cooperation among pannexin hemichannels, adenosine receptors, and KATP channels. J. Neurosci. Off. J. Soc. Neurosci. 2010, 30, 3886–3895. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.J.; Jackson, M.F.; Olah, M.E.; Rungta, R.L.; Hines, D.J.; Beazely, M.A.; MacDonald, J.F.; MacVicar, B.A. Activation of pannexin-1 hemichannels augments aberrant bursting in the hippocampus. Science 2008, 322, 1555–1559. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.J. Pannexin channels and ischaemia. J. Physiol. 2015, 593, 3463–3470. [Google Scholar] [CrossRef] [PubMed]
- Aquilino, M.S.; Whyte-Fagundes, P.; Zoidl, G.; Carlen, P.L. Pannexin-1 channels in epilepsy. Neurosci. Lett. 2017. [Google Scholar] [CrossRef] [PubMed]
- Wasterlain, C.G.; Fujikawa, D.G.; Penix, L.; Sankar, R. Pathophysiological mechanisms of brain damage from status epilepticus. Epilepsia 1993, 34, S37–S53. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Wu, J.; Guo, R.; Peng, Y.; Zheng, W.; Liu, D.; Song, Z. Glycolysis in energy metabolism during seizures. Neural Regen. Res. 2013, 8, 1316–1326. [Google Scholar] [PubMed]
- Folbergrova, J.; Jesina, P.; Drahota, Z.; Lisy, V.; Haugvicova, R.; Vojtiskova, A.; Houstek, J. Mitochondrial complex I inhibition in cerebral cortex of immature rats following homocysteic acid-induced seizures. Exp. Neurol. 2007, 204, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Acharya, M.M.; Katyare, S.S. Structural and functional alterations in mitochondrial membrane in picrotoxin-induced epileptic rat brain. Exp. Neurol. 2005, 192, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Sacktor, B.; Wilson, J.E.; Tiekert, C.G. Regulation of glycolysis in brain, in situ, during convulsions. J. Biol. Chem. 1966, 241, 5071–5075. [Google Scholar] [PubMed]
- Neppl, R.; Nguyen, C.M.; Bowen, W.; Al-Saadi, T.; Pallagi, J.; Morris, G.; Mueller, W.; Johnson, R.; Prost, R.; Rand, S.D. In vivo detection of postictal perturbations of cerebral metabolism by use of proton MR spectroscopy: Preliminary results in a canine model of prolonged generalized seizures. AJNR. Am. J. Neuroradiol. 2001, 22, 1933–1943. [Google Scholar] [PubMed]
- Darbin, O.; Risso, J.J.; Carre, E.; Lonjon, M.; Naritoku, D.K. Metabolic changes in rat striatum following convulsive seizures. Brain Res. 2005, 1050, 124–129. [Google Scholar] [CrossRef] [PubMed]
- During, M.J.; Fried, I.; Leone, P.; Katz, A.; Spencer, D.D. Direct measurement of extracellular lactate in the human hippocampus during spontaneous seizures. J. Neurochem. 1994, 62, 2356–2361. [Google Scholar] [CrossRef] [PubMed]
- Fornai, F.; Bassi, L.; Gesi, M.; Giorgi, F.S.; Guerrini, R.; Bonaccorsi, I.; Alessandri, M.G. Similar increases in extracellular lactic acid in the limbic system during epileptic and/or olfactory stimulation. Neuroscience 2000, 97, 447–458. [Google Scholar] [CrossRef]
- Kuhr, W.G.; Korf, J. Extracellular lactic acid as an indicator of brain metabolism: Continuous on-line measurement in conscious, freely moving rats with intrastriatal dialysis. J. Cereb. Blood Flow Metab. Off. J. Int. Soc. Cereb. Blood Flow Metab. 1988, 8, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Kuhr, W.G.; Korf, J. N-methyl-D-aspartate receptor involvement in lactate production following ischemia or convulsion in rats. Eur. J. Pharmacol. 1988, 155, 145–149. [Google Scholar] [CrossRef]
- Dalsgaard, M.K.; Secher, N.H. The brain at work: A cerebral metabolic manifestation of central fatigue? J. Neurosci. Res. 2007, 85, 3334–3339. [Google Scholar] [CrossRef] [PubMed]
- Pellerin, L.; Bouzier-Sore, A.K.; Aubert, A.; Serres, S.; Merle, M.; Costalat, R.; Magistretti, P.J. Activity-dependent regulation of energy metabolism by astrocytes: An update. Glia 2007, 55, 1251–1262. [Google Scholar] [CrossRef] [PubMed]
- Rouach, N.; Koulakoff, A.; Abudara, V.; Willecke, K.; Giaume, C. Astroglial metabolic networks sustain hippocampal synaptic transmission. Science 2008, 322, 1551–1555. [Google Scholar] [CrossRef] [PubMed]
- Schurr, A.; West, C.A.; Rigor, B.M. Lactate-supported synaptic function in the rat hippocampal slice preparation. Science 1988, 240, 1326–1328. [Google Scholar] [CrossRef] [PubMed]
- Schurr, A.; Payne, R.S.; Miller, J.J.; Rigor, B.M. Brain lactate, not glucose, fuels the recovery of synaptic function from hypoxia upon reoxygenation: An in vitro study. Brain Res. 1997, 744, 105–111. [Google Scholar] [CrossRef]
- Schurr, A.; Miller, J.J.; Payne, R.S.; Rigor, B.M. An increase in lactate output by brain tissue serves to meet the energy needs of glutamate-activated neurons. J. Neurosci. Off. J. Soc. Neurosci. 1999, 19, 34–39. [Google Scholar]
- Farrell, J.S.; Gaxiola-Valdez, I.; Wolff, M.D.; David, L.S.; Dika, H.I.; Geeraert, B.L.; Rachel Wang, X.; Singh, S.; Spanswick, S.C.; Dunn, J.F.; et al. Postictal behavioural impairments are due to a severe prolonged hypoperfusion/hypoxia event that is COX-2 dependent. eLife 2016, 5. [Google Scholar] [CrossRef] [PubMed]
- Solaini, G.; Baracca, A.; Lenaz, G.; Sgarbi, G. Hypoxia and mitochondrial oxidative metabolism. Biochim. Biophys. Acta 2010, 1797, 1171–1177. [Google Scholar] [CrossRef] [PubMed]
- De Curtis, M.; Avoli, M. Initiation, propagation, and termination of partial (focal) seizures. Cold Spring Harb. Perspect. Med. 2015, 5, a022368. [Google Scholar] [CrossRef] [PubMed]
- Sinning, A.; Hubner, C.A. Minireview: pH and synaptic transmission. FEBS Lett. 2013, 587, 1923–1928. [Google Scholar] [CrossRef] [PubMed]
- Nakada, H.I.; Wick, A.N. The effect of 2-deoxyglucose on the metabolism of glucose, fructose, and galactose by rat diaphragm. J. Biol. Chem. 1956, 222, 671–676. [Google Scholar] [PubMed]
- Wick, A.N.; Drury, D.R.; Nakada, H.I.; Wolfe, J.B. Localization of the primary metabolic block produced by 2-deoxyglucose. J. Biol. Chem. 1957, 224, 963–969. [Google Scholar] [PubMed]
- Garriga-Canut, M.; Schoenike, B.; Qazi, R.; Bergendahl, K.; Daley, T.J.; Pfender, R.M.; Morrison, J.F.; Ockuly, J.; Stafstrom, C.; Sutula, T.; et al. 2-Deoxy-D-glucose reduces epilepsy progression by NRSF-CtBP-dependent metabolic regulation of chromatin structure. Nat. Neurosci. 2006, 9, 1382–1387. [Google Scholar] [CrossRef] [PubMed]
- Gasior, M.; Yankura, J.; Hartman, A.L.; French, A.; Rogawski, M.A. Anticonvulsant and proconvulsant actions of 2-deoxy-D-glucose. Epilepsia 2010, 51, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Bazzigaluppi, P.; Weisspapir, I.; Stefanovic, B.; Leybaert, L.; Carlen, P.L. Astrocytic gap junction blockade markedly increases extracellular potassium without causing seizures in the mouse neocortex. Neurobiol. Dis. 2017, 101, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Pena, F.; Tapia, R. Seizures and neurodegeneration induced by 4-aminopyridine in rat hippocampus in vivo: Role of glutamate- and GABA-mediated neurotransmission and of ion channels. Neuroscience 2000, 101, 547–561. [Google Scholar] [CrossRef]
- Reddy, D.S.; Kuruba, R. Experimental models of status epilepticus and neuronal injury for evaluation of therapeutic interventions. Int. J. Mol. Sci. 2013, 14, 18284–18318. [Google Scholar] [CrossRef] [PubMed]
- Bazzigaluppi, P.; Dufour, S.; Carlen, P.L. Wide field fluorescent imaging of extracellular spatiotemporal potassium dynamics in vivo. NeuroImage 2015, 104, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Sada, N.; Lee, S.; Katsu, T.; Otsuki, T.; Inoue, T. Epilepsy treatment. Targeting LDH enzymes with a stiripentol analog to treat epilepsy. Science 2015, 347, 1362–1367. [Google Scholar] [CrossRef] [PubMed]
- Popova, I.; Malkov, A.; Ivanov, A.I.; Samokhina, E.; Buldakova, S.; Gubkina, O.; Osypov, A.; Muhammadiev, R.S.; Zilberter, T.; Molchanov, M.; et al. Metabolic correction by pyruvate halts acquired epilepsy in multiple rodent models. Neurobiol. Dis. 2017, 106, 244–254. [Google Scholar] [CrossRef] [PubMed]
- Rho, J.M. Inhibition of Lactate Dehydrogenase to Treat Epilepsy. N. Engl. J. Med. 2015, 373, 187–189. [Google Scholar] [CrossRef] [PubMed]
- Gano, L.B.; Patel, M. Fermenting seizures with lactate dehydrogenase. Epilepsy Curr. 2015, 15, 274–276. [Google Scholar] [CrossRef] [PubMed]
- Scharfman, H.E. Neuroscience. Metabolic control of epilepsy. Science 2015, 347, 1312–1313. [Google Scholar] [PubMed]
- Picot, M.C.; Baldy-Moulinier, M.; Daures, J.P.; Dujols, P.; Crespel, A. The prevalence of epilepsy and pharmacoresistant epilepsy in adults: A population-based study in a Western European country. Epilepsia 2008, 49, 1230–1238. [Google Scholar] [CrossRef] [PubMed]
- Kwan, P.; Schachter, S.C.; Brodie, M.J. Drug-resistant epilepsy. N. Engl. J. Med. 2011, 365, 919–926. [Google Scholar] [CrossRef] [PubMed]

© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bazzigaluppi, P.; Ebrahim Amini, A.; Weisspapir, I.; Stefanovic, B.; Carlen, P.L. Hungry Neurons: Metabolic Insights on Seizure Dynamics. Int. J. Mol. Sci. 2017, 18, 2269. https://doi.org/10.3390/ijms18112269
Bazzigaluppi P, Ebrahim Amini A, Weisspapir I, Stefanovic B, Carlen PL. Hungry Neurons: Metabolic Insights on Seizure Dynamics. International Journal of Molecular Sciences. 2017; 18(11):2269. https://doi.org/10.3390/ijms18112269
Chicago/Turabian StyleBazzigaluppi, Paolo, Azin Ebrahim Amini, Iliya Weisspapir, Bojana Stefanovic, and Peter L. Carlen. 2017. "Hungry Neurons: Metabolic Insights on Seizure Dynamics" International Journal of Molecular Sciences 18, no. 11: 2269. https://doi.org/10.3390/ijms18112269
APA StyleBazzigaluppi, P., Ebrahim Amini, A., Weisspapir, I., Stefanovic, B., & Carlen, P. L. (2017). Hungry Neurons: Metabolic Insights on Seizure Dynamics. International Journal of Molecular Sciences, 18(11), 2269. https://doi.org/10.3390/ijms18112269




