Interferon Crevicular Fluid Profile and Correlation with Periodontal Disease and Wound Healing: A Systemic Review of Recent Data
Abstract
:1. Introduction
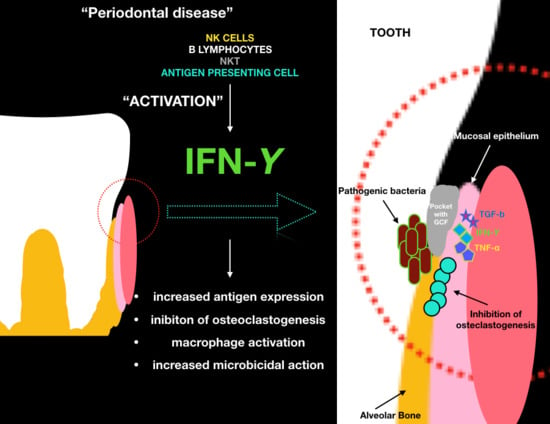
- In macrophages: Causes classical activation along with Toll-like receptor signals. In these cells it activates numerous transcription factors such as STAT1, NF-κB and AP-1 that induce the transcription of different enzymes involved in phagocytosis, such as phagocytic oxidase, inducible nitric oxide synthase and other lysosomal enzymes.
- In B lymphocytes: Promotes class exchange between the various Ig subclasses.
- In TH1 lymphocytes: Stimulates the CD4 T lymphocytes to differentiate into TH1 lymphocytes, inhibiting TH2 and TH17.
- In MHC: Acts on MHC molecules, inducing the expression of proteins that improve the binding with the peptide and the consequent presentation [2].
2. Results
2.1. Study Selection
2.2. Study Characteristics
2.3. Risk of Bias within Studies
2.4. Risk of Bias across Studies
3. Discussion
Limitations
4. Material and Methods
4.1. Protocol and Registration
4.2. Focus Question
4.3. Information Sources
4.4. Searches
4.5. Selection of Studies
4.6. Types of Manuscripts Selected
4.7. Types of Studies
4.8. Disease Definition
4.9. Inclusion and Exclusion Criteria
- Correlation between interferon gamma levels and periodontitis.
- Periodontitis and biomarker levels in the crevicular fluid.
- Periodontal therapy and variation of inflammatory mediators levels in the crevicular fluid.
- Correlation between levels of interferon oral ranges and diseases in other districts.
- All human prospective or retrospective follow-up studies and clinical trials, cohort studies, case–control studies, and case series studies with a six-month follow-up.
- Animal or in vitro studies.
- Studies involving patients with specific diseases, immunologic disorders, uncontrolled diabetes mellitus, osteoporosis, or other implant risk-related systemic conditions.
- Not enough information regarding the selected topic.
- Articles published prior to 1 January 2010.
- No access to the title and abstract in English language.
4.10. Sequential Search Strategy
4.11. Data Extraction
4.12. Data Collection
- “Author (Year)”—Revealed the author and year of publication.
- “Type of study”.
- “Sample size”—Described the number of patients, animals or models examined.
- “Inflammatory mediators investigated”—Described types of inflammatory mediators evaluated in studies.
- “IFN-gamma”—Interferon gamma levels evaluated or not.
- “Statistics”—Described the presence of significant or nonsignificant mediator levels.
4.13. Risk of Bias Assessment
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Niedzielska, I.; Cierpka, S. Interferon gamma in the etiology of atherosclerosis and periodontitis. Thromb. Res. 2010, 126, 324–327. [Google Scholar] [CrossRef] [PubMed]
- Abul, K.; Abbas, A.H.; Lichtman, S.P. Immunologia Cellulare e Molecolare; Masson, E., Ed.; Elsevier: Philadelphia, PA, USA, 2012; Volume 2. [Google Scholar]
- Berglundh, T.; Liljenberg, B.; Lindhe, J. Some cytokine profiles of T helper cells in lesions of advanced periodontitis. J. Clin. Periodontol. 2002, 29, 705–709. [Google Scholar] [CrossRef] [PubMed]
- Lemos, J.C.; Gurgel, B.C.D.V.; Freitas, R.D.A. Th2 cells and the IFN-γ R1 subunit in early and advanced experimental periodontitis in rats; an immunohistochemical study. Braz. J. Oral Sci. 2015, 14, 106–111. [Google Scholar] [CrossRef]
- Mermut, S.; Bengi, A.O.; Akin, E.; Kürkçü, M.; Karaçay, Ş. Effects of Interferon-Gamma on Bone Remodeling during Experimental Tooth Movement. Angle Orthod. 2007, 77, 135–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaddox, L.M.; Wiedey, J.; Calderon, N.L.; Magnusson, I.; Bimstein, E.; Bidwell, J.A.; Zapert, E.F.; Aukhil, I.; Wallet, S.M. Local inflammatory markers and systemic endotoxin in aggressive periodontitis. J. Dent. Res. 2011, 90, 1140–1144. [Google Scholar] [CrossRef] [PubMed]
- Thunell, D.H.; Tymkiw, K.D.; Johnson, G.K.; Joly, S.; Burnell, K.K.; Cavanaugh, J.E.; Brogden, K.A.; Guthmiller, J.M. A multiplex immunoassay demonstrates reductions in gingival crevicular fluid cytokines following initial periodontal therapy. J. Periodontal Res. 2010, 45, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Morozumi, T.; Yashima, A.; Gomi, K.; Ujiie, Y.; Izumi, Y.; Akizuki, T.; Mizutani, K.; Takamatsu, H.; Minabe, M.; Miyauchi, S.; et al. Increased systemic levels of inflammatory mediators following one-stage full-mouth scaling and root planing. J. Periodontal Res. 2018. [Google Scholar] [CrossRef] [PubMed]
- Lomba, K.S.; Beller, T.F.; Sete, M.R.; Pires, F.S.; Figueredo, C.M. Use of minimally invasive gingival biopsies in the study of inflammatory mediators expression and their correlation with gingival fluid patients with chronic periodontitis. Indian J. Dent. Res. 2015, 26, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Shaddox, L.M.; Gonçalves, P.F.; Vovk, A.; Allin, N.; Huang, H.; Hou, W.; Aukhil, I.; Wallet, S.M. LPS-induced inflammatory response after therapy of aggressive periodontitis. J. Dent. Res. 2013, 92, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Fu, Q.Y.; Zhang, L.; Duan, L.; Qian, S.Y.; Pang, H.X. Correlation of chronic periodontitis in tropical area and IFN-γ, IL-10, IL-17 levels. Asian Pac. J. Trop. Med. 2013, 6, 489–492. [Google Scholar] [CrossRef]
- De Lima Oliveira, A.P.; de Faveri, M.; Gursky, L.C.; Mestnik, M.J.; Feres, M.; Haffajee, A.D.; Socransky, S.S.; Teles, R.P. Effects of periodontal therapy on GCF cytokines in generalized aggressive periodontitis subjects. J. Clin. Periodontol. 2012, 39, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Crivello, A.; Offenbacher, S.; Moretti, A.; Paquette, D.W.; Barros, S.P. Interferon-gamma promoter hypomethylation and increased expression in chronic periodontitis. J. Clin. Periodontol. 2010, 37, 953–961. [Google Scholar] [CrossRef] [PubMed]
- Arjunkumar, R.; Sudhakar, U.; Jayakumar, P.; Arunachalam, L.; Suresh, S.; Virupapuram, P. Comparative analysis of gingival crevicular fluid neopterin levels in health and periodontal disease: A biochemical study. Indian J. Dent. Res. 2013, 24, 582–586. [Google Scholar] [CrossRef] [PubMed]
- Sinrod, H.S. Periodontal Disease in Developing Nations. Science 1965, 149, 400–402. [Google Scholar] [CrossRef] [PubMed]
- Mastrangelo, F.; Dedola, A.; Cattoni, F.; Ferrini, F.; Bova, F.; Tatullo, M.; Gherlone, E.; Lo, L.M. Etiological periodontal treatment with and without low-level laser therapy on IL-1β level in gingival crevicular fluid: An in vivo multicentric pilot study. J. Biol. Regul. Homeost. Agents 2018, 32, 425–431. [Google Scholar] [PubMed]
- Ballini, A.; Cantore, S.; Dedola, A.; Santacroce, L.; Laino, L.; Cicciù, M.; Mastrangelo, F. IL-1 haplotype analysis in periodontal disease. J. Biol. Regul. Homeost. Agents 2018, 32, 433–437. [Google Scholar] [PubMed]
- Beck, J.D.; Eke, P.; Heiss, G.; Madianos, P.; Couper, D.; Lin, D.; Moss, K.; Elter, J.; Offenbacher, S. Periodontal Disease and Coronary Heart Disease: A Reappraisal of the Exposure. Circulation 2005, 112, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Ralph, S.; Malcolm, W. Increasing Evidence for an Association between Periodontitis and Cardiovascular Disease. Circulation 2016, 133, 549–551. [Google Scholar] [CrossRef]
- Cicciù, M. Neurodegenerative Disorders and Periodontal Disease: Is There a Logical Connection? Neuroepidemiology 2016, 47, 94–95. [Google Scholar] [CrossRef] [PubMed]
- Cicciù, M.; Matacena, G.; Signorino, F.; Brugaletta, A.; Cicciù, A.; Bramanti, E. Relationship between oral health and its impact on the quality life of Alzheimer’s disease patients: A supportive care trial. Int. J. Clin. Exp. Med. 2013, 6, 766–772. [Google Scholar] [PubMed]
- Oteri, G.; Bramanti, E.; Nigrone, V.; Cicciù, M. Decayed, Missing, and Filled Teeth Index and Periodontal Health in Osteoporotic Patients Affected by BRONJ: An Observational Study. J. Osteoporos. 2013, 2013, 231289. [Google Scholar] [CrossRef] [PubMed]
- Cicciù, M.; Cervino, G.; Herford, A.S.; Famà, F.; Bramanti, E.; Fiorillo, L.; Lauritano, F.; Sambataro, S.; Troiano, G.; Laino, L. Facial Bone Reconstruction Using both Marine or Non–Marine Bone Substitutes: Evaluation of Current Outcomes in a Systematic Literature Review. Mar. Drugs 2018, 16, E27. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Romeo, U.; Lauritano, F.; Bramanti, E.; Fiorillo, L.; D’Amico, C.; Milone, D.; Laino, L.; Campolongo, F.; Rapisarda, S.; et al. Fem and Von Mises Analysis of OSSTEM® Dental Implant Structural Components: Evaluation of Different Direction Dynamic Loads. Open Dent. J. 2018, 12, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Savage, A.; Eaton, K.A.; Moles, D.R.; Needleman, I. A systematic review of definitions of periodontitis and methods that have been used to identify this disease. J. Clin. Periodontol. 2009, 36, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Matarese, G.; Ramaglia, L.; Fiorillo, L.; Cervino, G.; Lauritano, F.; Isola, G. Implantology and Periodontal Disease: The Panacea to Problem Solving? Open Dent. J. 2017, 11, 460–465. [Google Scholar] [CrossRef] [PubMed]
- Zitzmann, N.U.; Berglundh, T.; Ericsson, I.; Lindhe, J. Spontaneous progression of experimentally induced periimplantitis. J. Clin. Periodontol. 2004, 31, 845–849. [Google Scholar] [CrossRef] [PubMed]
- Kinane, D.F.; Stathopoulou, P.G.; Papapanou, P.N. Periodontal diseases. Nat. Rev. Dis. Primers 2017, 3, 17038. [Google Scholar] [CrossRef] [PubMed]
- Pihlstrom, B.L.; Michalowicz, B.S.; Johnson, N.W. Periodontal diseases. Lancet 2005, 366, 1809–1820. [Google Scholar] [CrossRef]
- GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G. Assessing Risk of Bias in Included Studies. In Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series; Higgins, J.P.T., Green, S., Eds.; Wiley: Chichester, UK, 2008. [Google Scholar]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Reference | Authors | Type of Investigation | No. of Sample (Control) | Mediators Evaluated | IFN-γ | Results | Statistics |
|---|---|---|---|---|---|---|---|
| [6] | Shaddox et al. | Milliplex®, Luminex® | 34 (+10 controls) | TNF-α, IFN-γ, IL-1β, IL-2, IL-10, IL-12p40, GMCSF, M1P1a | Yes | Diseased sites from LAP participants presented higher levels of IFN-γ when compared with levels in their own healthy sites. | p < 0.001 |
| [7] | Thunell et al. | Periodontal treatment | 6 | IFN-γ, IL-1α, IL-1β, IL-2, IL-13, IL-3, IL-4, IL-6, IL-12p40, GMCSF, TNF-α | Yes | IFN-γ is significantly higher in sites | p < 0.0001 |
| [13] | Zhang et al. | PCA-RT | 12 (+47 controls) | mRNA expressions of IFN-γ | No | The transcription levels of IFN-γ was increased and significantly higher in the periodontitis biopsy samples | p = 0.04 |
| [9] | Lomba et al. | Luminex® | 22 | IFN-γ, IFN-1β, interleukin-6, interleukin-17α, interleukin-17F | Yes | There are differences between mediators in swallow and deep sites. | IFN-γ p = 0.233 |
| [10] | Shaddox et al. | Luminex®, periodontal treatment | 59 | IFN-γ, IL10, IL12p40, IL1β, IL6, MCP1, GM-CSF, IP10, TNFα | Yes | Periodontal treatment resulted in significant improvement in most clinical parameters and LPS induced inflammatory response. | E. Coli: p = 0.14; Porphyromonas gingivalis: p = 0.001 |
| [11] | Fu et al. | Periodontal treatment | 148 (+132 control) | IFN-γ, IL10, IL17 | Yes | Experimental studies have demonstrated that IFN-γ positive cells * as Th1 cells play a prominent role in mediating periodontal tissue destruction | No significant differences after therapy |
| [12] | Oliveira et al. | Luminex®, periodontal treatment | 895 | IFN-γ, IL-10, IL-1β, IL-2, IL-6, TNF-α | Yes | No effect of periodontal therapy on GVF levels of IFN-γ | p = 0.4–0.7 |
| [8] | Marazumi et al. | Periodontal treatment | 39 | IFN-γ, IL-4, IL-5, IL-6, IL-12p70, TNF-α | Yes | After treatment, significant levels of IFN-γ were present | p < 0.001 |
| [14] | Arjunkunan et al. | / | 30 | Neopterin | No | Upon stimulation by IFN-γ, neopterin is released, but there is no significant difference between groups | p > 0.05 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fiorillo, L.; Cervino, G.; Herford, A.S.; Lauritano, F.; D’Amico, C.; Lo Giudice, R.; Laino, L.; Troiano, G.; Crimi, S.; Cicciù, M. Interferon Crevicular Fluid Profile and Correlation with Periodontal Disease and Wound Healing: A Systemic Review of Recent Data. Int. J. Mol. Sci. 2018, 19, 1908. https://doi.org/10.3390/ijms19071908
Fiorillo L, Cervino G, Herford AS, Lauritano F, D’Amico C, Lo Giudice R, Laino L, Troiano G, Crimi S, Cicciù M. Interferon Crevicular Fluid Profile and Correlation with Periodontal Disease and Wound Healing: A Systemic Review of Recent Data. International Journal of Molecular Sciences. 2018; 19(7):1908. https://doi.org/10.3390/ijms19071908
Chicago/Turabian StyleFiorillo, Luca, Gabriele Cervino, Alan Scott Herford, Floriana Lauritano, Cesare D’Amico, Roberto Lo Giudice, Luigi Laino, Giuseppe Troiano, Salvatore Crimi, and Marco Cicciù. 2018. "Interferon Crevicular Fluid Profile and Correlation with Periodontal Disease and Wound Healing: A Systemic Review of Recent Data" International Journal of Molecular Sciences 19, no. 7: 1908. https://doi.org/10.3390/ijms19071908
APA StyleFiorillo, L., Cervino, G., Herford, A. S., Lauritano, F., D’Amico, C., Lo Giudice, R., Laino, L., Troiano, G., Crimi, S., & Cicciù, M. (2018). Interferon Crevicular Fluid Profile and Correlation with Periodontal Disease and Wound Healing: A Systemic Review of Recent Data. International Journal of Molecular Sciences, 19(7), 1908. https://doi.org/10.3390/ijms19071908