Stem Cells Secretome from Oral Tissue Could Represent a Promising Therapeutic Approach in COVID-19-Disease?
Abstract
1. COVID-19
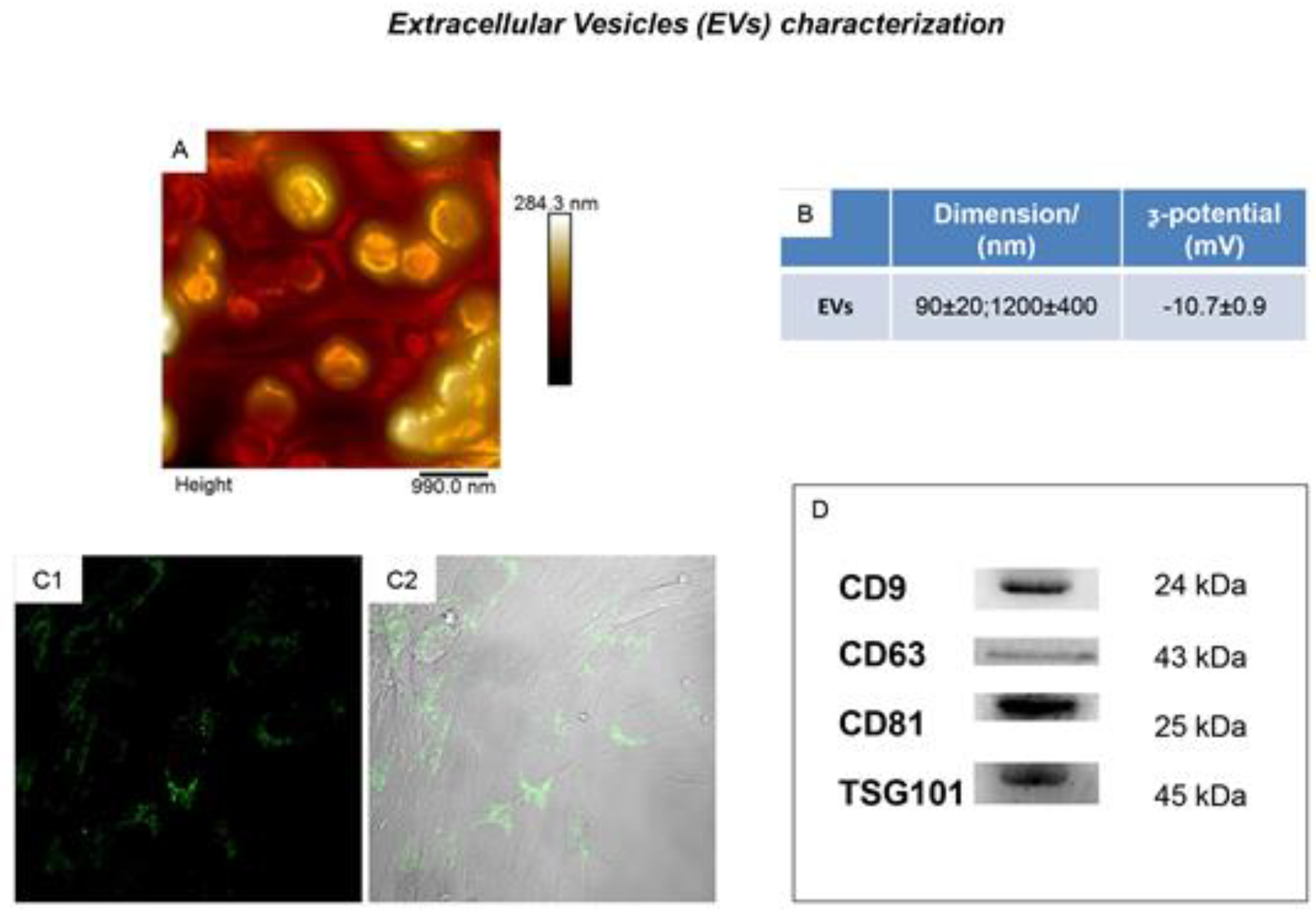
2. Secretome from Human Oral Mesenchymal Stem Cells
3. The Potential Use of hOMSCs-Derived Secretome in COVID-19
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| hOMSCs | human Oral Mesenchymal Stem Cells |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome Coronavirus-2 |
| COVID-19 | Coronavirus Disease 2019 |
| ARDS | Acute Respiratory Distress Syndrome |
| IL | Interleukin |
| TLR | Toll Like Receptor |
| MSCs | Mesenchymal Stem Cells |
| SHED | Exfoliated Deciduous Teeth |
| SCAP | Stem Cells From Apical Papilla |
| PDLSCs | Periodontal Ligament Stem Cells |
| DFPCs | Dental Follicle Progenitor Cells |
| GMSCs | Gingival Mesenchymal Stem Cells |
| DPSCs | Dental Pulp Stem Cells |
| CD | Cluster of Differentiation |
| HLA | Human Leucocyte Antigen |
| EVs | Extracellular Vesicles |
| SDF-1α | Stromal Cell-Derived factor-1α |
| BM | Bone Marrow |
| PMN | Polymorphonuclear Neutrophil |
| VEGF | Vascular Endothelial Growth factor |
| SPMs | Specialized Proresolving Lipid Mediators |
| EAE | Experimental Autoimmune Encephalomyelitis |
| H | Hypoxia |
| CM | Conditioned Medium |
References
- Zumla, A.; Niederman, M.S. Editorial: The explosive epidemic outbreak of novel coronavirus disease 2019 (COVID-19) and the persistent threat of respiratory tract infectious diseases to global health security. Curr. Opin. Pulm. Med. 2020, 26, 193–196. [Google Scholar] [CrossRef]
- Scavone, C.; Brusco, S.; Bertini, M.; Sportiello, L.; Rafaniello, C.; Zoccoli, A.; Berrino, L.; Racagni, G.; Rossi, F.; Capuano, A. Current pharmacological treatments for COVID-19: What’s next? Br. J. Pharm. 2020. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020, 8, 420–422. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Kruger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280. [Google Scholar] [CrossRef]
- Conti, P.; Gallenga, C.E.; Tete, G.; Caraffa, A.; Ronconi, G.; Younes, A.; Toniato, E.; Ross, R.; Kritas, S.K. How to reduce the likelihood of coronavirus-19 (CoV-19 or SARS-CoV-2) infection and lung inflammation mediated by IL-1. J. Biol. Regul. Homeost. Agents 2020, 34. [Google Scholar] [CrossRef]
- Conti, P.; Ronconi, G.; Caraffa, A.; Gallenga, C.E.; Ross, R.; Frydas, I.; Kritas, S.K. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): Anti-inflammatory strategies. J. Biol. Regul. Homeost. Agents 2020, 34. [Google Scholar] [CrossRef]
- Leng, Z.K.; Zhu, R.J.; Hou, W.; Feng, Y.M.; Yang, Y.L.; Han, Q.; Shan, G.L.; Meng, F.Y.; Du, D.S.; Wang, S.H.; et al. Transplantation of ACE2(-) Mesenchymal Stem Cells Improves the Outcome of Patients with COVID-19 Pneumonia. Aging Dis. 2020, 11, 216–228. [Google Scholar] [CrossRef]
- Cascini, V.; Lisi, G.; Lauriti, G.; Sindici, G.; Chiesa, P.L. Giant abdomino-pelvic adipose tumors of childhood. Pediatric Surg. Int. 2012, 28, 89–93. [Google Scholar] [CrossRef]
- Pizzicannella, J.; Diomede, F.; Gugliandolo, A.; Chiricosta, L.; Bramanti, P.; Merciaro, I.; Orsini, T.; Mazzon, E.; Trubiani, O. 3D Printing PLA/Gingival Stem Cells/EVs Upregulate miR-2861 and -210 during Osteoangiogenesis Commitment. Int. J. Mol. Sci. 2019, 20, 3256. [Google Scholar] [CrossRef]
- Diomede, F.; Zini, N.; Pizzicannella, J.; Merciaro, I.; Pizzicannella, G.; D’Orazio, M.; Piattelli, A.; Trubiani, O. 5-Aza Exposure Improves Reprogramming Process Through Embryoid Body Formation in Human Gingival Stem Cells. Front. Genet. 2018, 9, 419. [Google Scholar] [CrossRef]
- Pizzicannella, J.; Diomede, F.; Merciaro, I.; Caputi, S.; Tartaro, A.; Guarnieri, S.; Trubiani, O. Endothelial committed oral stem cells as modelling in the relationship between periodontal and cardiovascular disease. J. Cell. Physiol. 2018, 233, 6734–6747. [Google Scholar] [CrossRef] [PubMed]
- Trubiani, O.; Pizzicannella, J.; Caputi, S.; Marchisio, M.; Mazzon, E.; Paganelli, R.; Paganelli, A.; Diomede, F. Periodontal Ligament Stem Cells: Current Knowledge and Future Perspectives. Stem Cells Dev. 2019, 28, 995–1003. [Google Scholar] [CrossRef]
- Trubiani, O.; Marconi, G.D.; Pierdomenico, S.D.; Piattelli, A.; Diomede, F.; Pizzicannella, J. Human Oral Stem Cells, Biomaterials and Extracellular Vesicles: A Promising Tool in Bone Tissue Repair. Int. J. Mol. Sci. 2019, 20, 4987. [Google Scholar] [CrossRef] [PubMed]
- Chiricosta, L.; Silvestro, S.; Pizzicannella, J.; Diomede, F.; Bramanti, P.; Trubiani, O.; Mazzon, E. Transcriptomic Analysis of Stem Cells Treated with Moringin or Cannabidiol: Analogies and Differences in Inflammation Pathways. Int. J. Mol. Sci. 2019, 20, 6039. [Google Scholar] [CrossRef] [PubMed]
- Mammana, S.; Gugliandolo, A.; Cavalli, E.; Diomede, F.; Iori, R.; Zappacosta, R.; Bramanti, P.; Conti, P.; Fontana, A.; Pizzicannella, J.; et al. Human gingival mesenchymal stem cells pretreated with vesicular moringin nanostructures as a new therapeutic approach in a mouse model of spinal cord injury. J. Tissue Eng. Regen. Med. 2019, 13, 1109–1121. [Google Scholar] [CrossRef]
- Sinjari, B.; Pizzicannella, J.; D’Aurora, M.; Zappacosta, R.; Gatta, V.; Fontana, A.; Trubiani, O.; Diomede, F. Curcumin/Liposome Nanotechnology as Delivery Platform for Anti-inflammatory Activities via NFkB/ERK/pERK Pathway in Human Dental Pulp Treated With 2-HydroxyEthyl MethAcrylate (HEMA). Front. Physiol. 2019, 10, 633. [Google Scholar] [CrossRef]
- Ballerini, P.; Diomede, F.; Petragnani, N.; Cicchitti, S.; Merciaro, I.; Cavalcanti, M.; Trubiani, O. Conditioned medium from relapsing-remitting multiple sclerosis patients reduces the expression and release of inflammatory cytokines induced by LPS-gingivalis in THP-1 and MO3.13 cell lines. Cytokine 2017, 96, 261–272. [Google Scholar] [CrossRef]
- Oses, C.; Olivares, B.; Ezquer, M.; Acosta, C.; Bosch, P.; Donoso, M.; Leniz, P.; Ezquer, F. Preconditioning of adipose tissue-derived mesenchymal stem cells with deferoxamine increases the production of pro-angiogenic, neuroprotective and anti-inflammatory factors: Potential application in the treatment of diabetic neuropathy. PLoS ONE 2017, 12, e0178011. [Google Scholar] [CrossRef]
- Giacoppo, S.; Thangavelu, S.R.; Diomede, F.; Bramanti, P.; Conti, P.; Trubiani, O.; Mazzon, E. Anti-inflammatory effects of hypoxia-preconditioned human periodontal ligament cell secretome in an experimental model of multiple sclerosis: A key role of IL-37. Faseb J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2017, 31, 5592–5608. [Google Scholar] [CrossRef]
- Silvestro, S.; Chiricosta, L.; Gugliandolo, A.; Pizzicannella, J.; Diomede, F.; Bramanti, P.; Trubiani, O.; Mazzon, E. Extracellular Vesicles Derived from Human Gingival Mesenchymal Stem Cells: A Transcriptomic Analysis. Genes 2020, 11, 118. [Google Scholar] [CrossRef]
- Pizzicannella, J.; Cavalcanti, M.; Trubiani, O.; Diomede, F. MicroRNA 210 Mediates VEGF Upregulation in Human Periodontal Ligament Stem Cells Cultured on 3DHydroxyapatite Ceramic Scaffold. Int. J. Mol. Sci. 2018, 19, 3916. [Google Scholar] [CrossRef] [PubMed]
- Diomede, F.; D’Aurora, M.; Gugliandolo, A.; Merciaro, I.; Orsini, T.; Gatta, V.; Piattelli, A.; Trubiani, O.; Mazzon, E. Biofunctionalized Scaffold in Bone Tissue Repair. Int. J. Mol. Sci. 2018, 19, 1022. [Google Scholar] [CrossRef] [PubMed]
- Diomede, F.; D’Aurora, M.; Gugliandolo, A.; Merciaro, I.; Ettorre, V.; Bramanti, A.; Piattelli, A.; Gatta, V.; Mazzon, E.; Fontana, A.; et al. A novel role in skeletal segment regeneration of extracellular vesicles released from periodontal-ligament stem cells. Int. J. Nanomed. 2018, 13, 3805–3825. [Google Scholar] [CrossRef] [PubMed]
- Hung, W.T.; Hong, X.; Christenson, L.K.; McGinnis, L.K. Extracellular Vesicles from Bovine Follicular Fluid Support Cumulus Expansion. Biol. Reprod. 2015, 93, 117. [Google Scholar] [CrossRef]
- Diomede, F.; Gugliandolo, A.; Cardelli, P.; Merciaro, I.; Ettorre, V.; Traini, T.; Bedini, R.; Scionti, D.; Bramanti, A.; Nanci, A.; et al. Three-dimensional printed PLA scaffold and human gingival stem cell-derived extracellular vesicles: A new tool for bone defect repair. Stem Cell Res. Ther. 2018, 9, 104. [Google Scholar] [CrossRef]
- Trubiani, O.; Isgro, A.; Zini, N.; Antonucci, I.; Aiuti, F.; Di Primio, R.; Nanci, A.; Caputi, S.; Paganelli, R. Functional interleukin-7/interleukin-7Ralpha, and SDF-1alpha/CXCR4 are expressed by human periodontal ligament derived mesenchymal stem cells. J. Cell. Physiol. 2008, 214, 706–713. [Google Scholar] [CrossRef]
- Cianci, E.; Recchiuti, A.; Trubiani, O.; Diomede, F.; Marchisio, M.; Miscia, S.; Colas, R.A.; Dalli, J.; Serhan, C.N.; Romano, M. Human Periodontal Stem Cells Release Specialized Proresolving Mediators and Carry Immunomodulatory and Prohealing Properties Regulated by Lipoxins. Stem Cells Transl. Med. 2016, 5, 20–32. [Google Scholar] [CrossRef]
- Rajan, T.S.; Giacoppo, S.; Diomede, F.; Ballerini, P.; Paolantonio, M.; Marchisio, M.; Piattelli, A.; Bramanti, P.; Mazzon, E.; Trubiani, O. The secretome of periodontal ligament stem cells from MS patients protects against EAE. Sci. Rep. 2016, 6, 38743. [Google Scholar] [CrossRef]
- Kardia, E.; Yusoff, N.M.; Zakaria, Z.; Yahaya, B. Aerosol-based delivery of fibroblast cells for treatment of lung diseases. J. Aerosol Med. Pulm. Drug Deliv. 2014, 27, 30–34. [Google Scholar] [CrossRef]
- Halim, N.S.S.; Ch’ng, E.S.; Kardia, E.; Ali, S.A.; Radzi, R.; Yahaya, B.H. Aerosolised Mesenchymal Stem Cells Expressing Angiopoietin-1 Enhances Airway Repair. Stem Cell Rev. Rep. 2019, 15, 112–125. [Google Scholar] [CrossRef]

| Secretome/EVs Content | |||
|---|---|---|---|
| Interleukins (IL) | Protein of the TGF-β Family | Protein of the Wnt Family | Growth Factors |
| IL1B | TGFb1 Transforming Growth Factor β 1 | WNT2B Wnt Family Member 2B | FGF1 Fibroblast Growth Factor 1 |
| IL5 | TGFb2 Transforming Growth Factor β 2 | WNT3 Wnt Family Member 3 | FGF4 Fibroblast Growth Factor 4 |
| IL6 | TGFb3 Transforming Growth Factor β 3 | WNT4 Wnt Family Member 4 | FGF6 Fibroblast Growth Factor 6 |
| IL7 | BMP1 Bone Morphogenetic Protein1 | WNT5A Wnt Family Member 5A | FGF7 Fibroblast Growth Factor 7 |
| IL12A | BMP2 Bone Morphogenetic Protein 2 | WNT5B Wnt Family Member 5B | FGF9 Fibroblast Growth Factor 9 |
| IL12B | BMP3 Bone Morphogenetic Protein 3 | WNT7A Wnt Family Member 7A | FGF11 Fibroblast Growth Factor 11 |
| IL15 | BMP4 Bone Morphogenetic Protein 4 | WNT8A Wnt Family Member 8A | FGF12 Fibroblast Growth Factor 12 |
| IL16 | BMP5 Bone Morphogenetic Protein 5 | WNT9A Wnt Family Member 9A | FGF14 Fibroblast Growth Factor 14 |
| IL17A | BMP6 Bone Morphogenetic Protein 6 | WNT10A Wnt Family Member 10A | FGF18 Fibroblast Growth Factor 18 |
| IL19 | BMP7 Bone Morphogenetic Protein 7 | WNT11 Wnt Family Member 11 | FGF20 Fibroblast Growth Factor 20 |
| IL21 | BMP8A Bone Morphogenetic Protein 8a | WNT16 Wnt Family Member 16 | FGF23 Fibroblast Growth Factor 23 |
| IL24 | BMP8B Bone Morphogenetic Protein 8b | PSPN Persephin | |
| IL25 | BMP10 Bone Morphogenetic Protein | GDNF Glial Cell Derived Neurotrophic Factor | |
| IL27 | BMP15 Bone Morphogenetic Protein 15 | VEGFA Vascular Endothelial Growth Factor A | |
| IL32 | AMH Anti-Mullerian Hormone | VEGFB Vascular Endothelial Growth Factor B | |
| IL33 | GDF1 Growth Differentiation Factor 1 | VEGFC Vascular Endothelial Growth Factor C | |
| IL36B | GDF2 Growth Differentiation Factor 2 | NGF Nerve Growth Factor | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diomede, F.; Marconi, G.D.; Fonticoli, L.; Pizzicannella, J.; Trubiani, O. Stem Cells Secretome from Oral Tissue Could Represent a Promising Therapeutic Approach in COVID-19-Disease? Int. J. Mol. Sci. 2020, 21, 6833. https://doi.org/10.3390/ijms21186833
Diomede F, Marconi GD, Fonticoli L, Pizzicannella J, Trubiani O. Stem Cells Secretome from Oral Tissue Could Represent a Promising Therapeutic Approach in COVID-19-Disease? International Journal of Molecular Sciences. 2020; 21(18):6833. https://doi.org/10.3390/ijms21186833
Chicago/Turabian StyleDiomede, Francesca, Guya D. Marconi, Luigia Fonticoli, Jacopo Pizzicannella, and Oriana Trubiani. 2020. "Stem Cells Secretome from Oral Tissue Could Represent a Promising Therapeutic Approach in COVID-19-Disease?" International Journal of Molecular Sciences 21, no. 18: 6833. https://doi.org/10.3390/ijms21186833
APA StyleDiomede, F., Marconi, G. D., Fonticoli, L., Pizzicannella, J., & Trubiani, O. (2020). Stem Cells Secretome from Oral Tissue Could Represent a Promising Therapeutic Approach in COVID-19-Disease? International Journal of Molecular Sciences, 21(18), 6833. https://doi.org/10.3390/ijms21186833





