Activation of Adenosine A3 Receptor Inhibits Microglia Reactivity Elicited by Elevated Pressure
Abstract
1. Introduction
2. Results
2.1. Effect of EHP in the Expression of A3R in BV-2 Cells
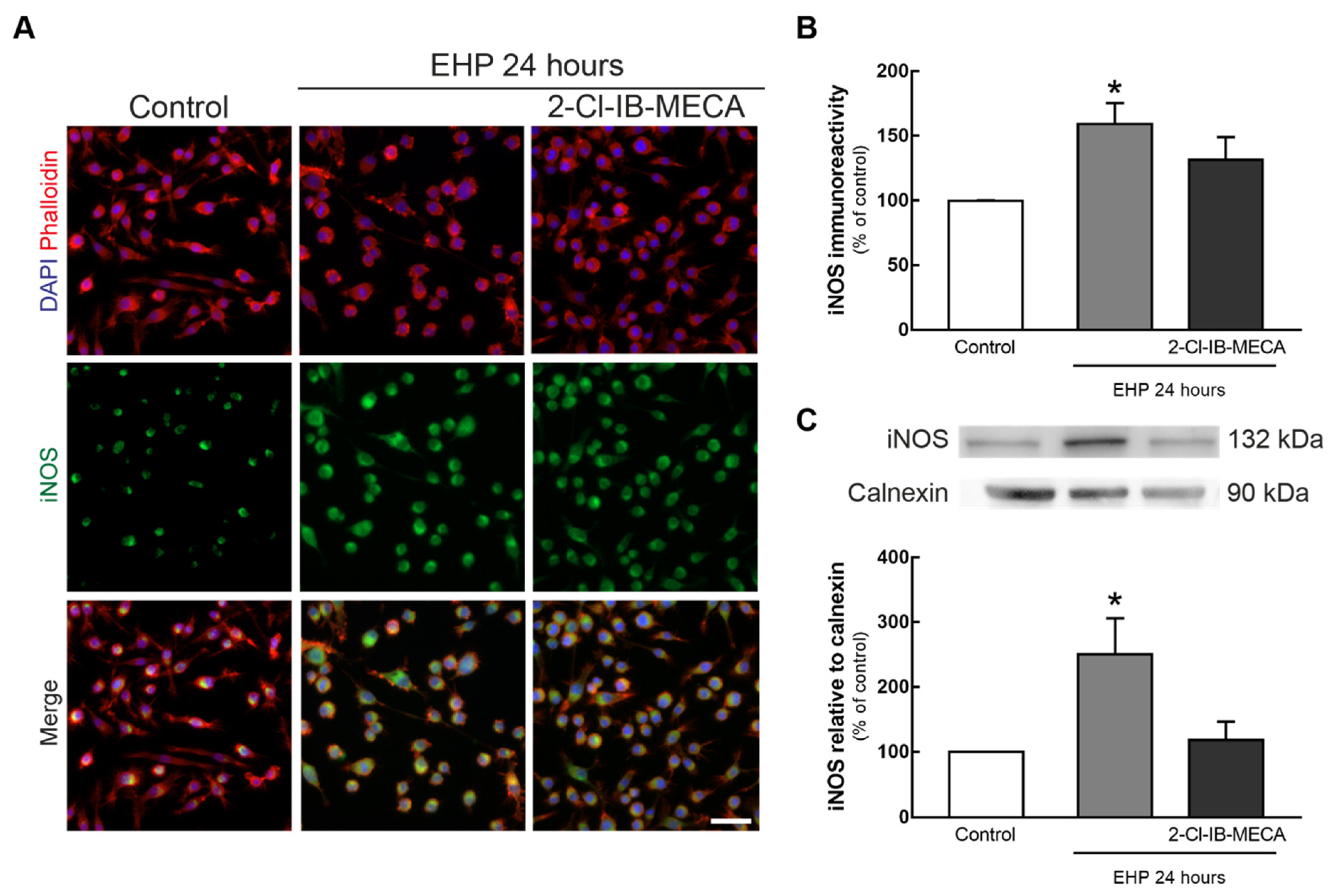
2.2. 2-Cl-IB-MECA Hampers the Increase in iNOS Induced by EHP in BV-2 Cells
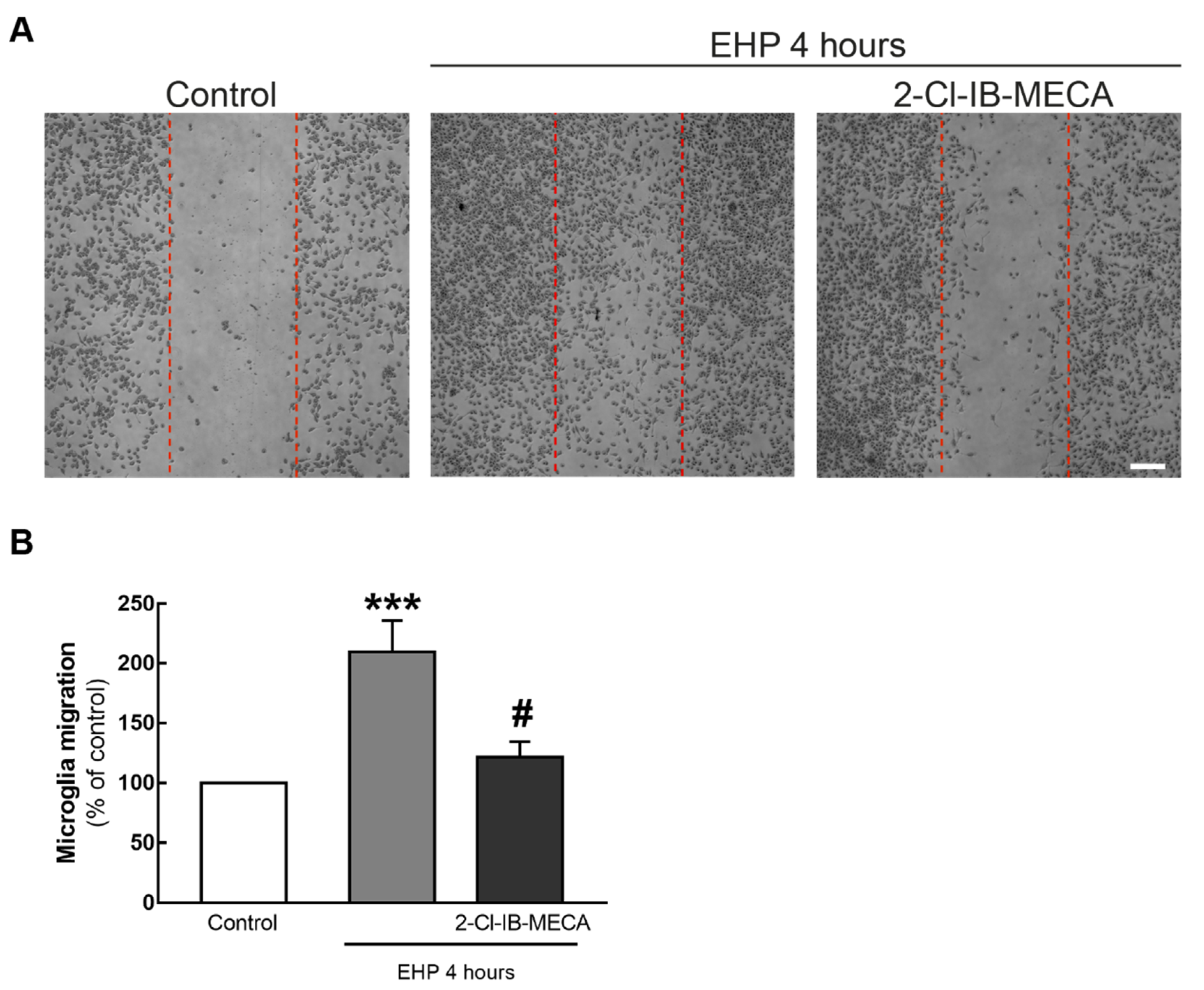
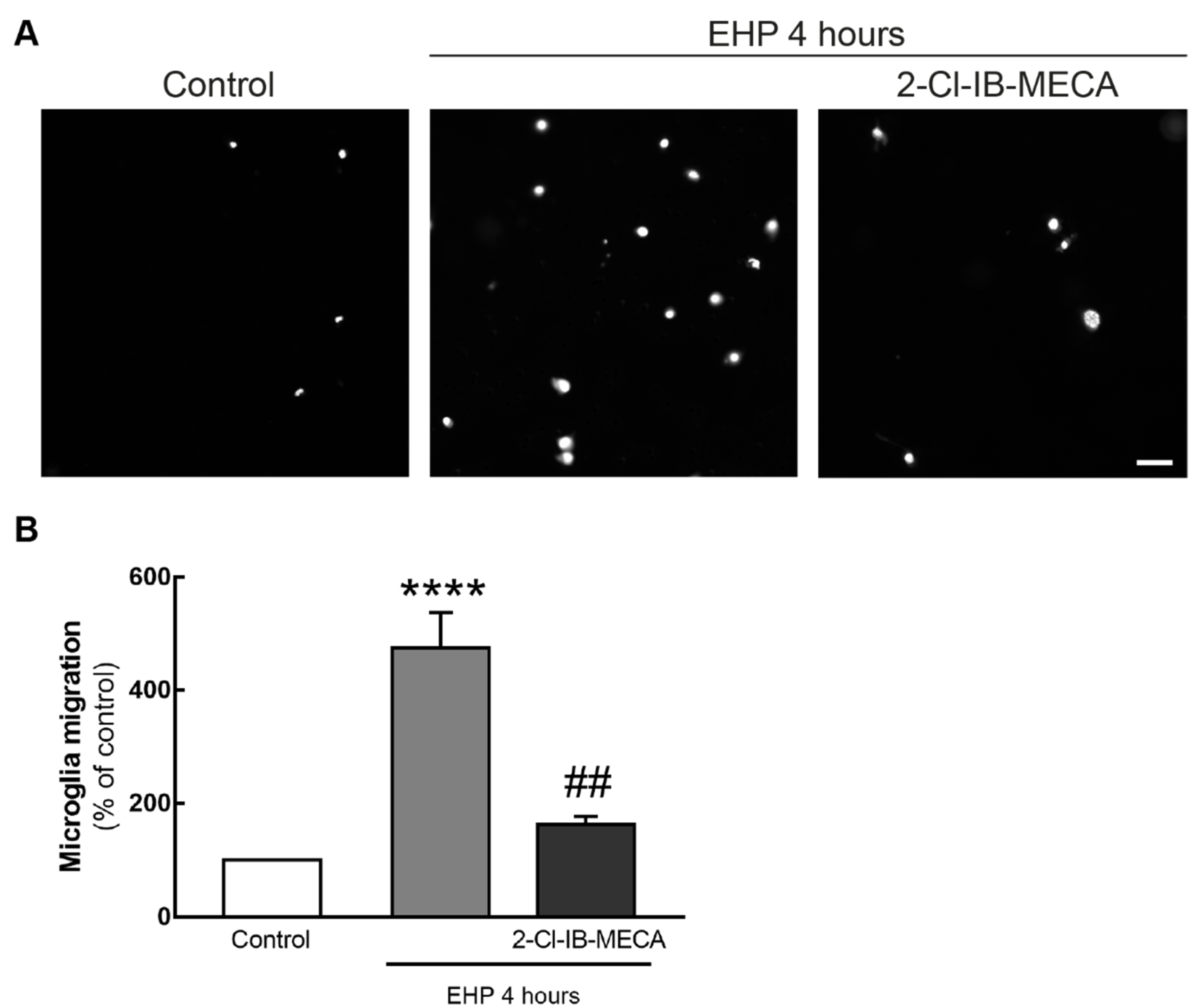
2.3. The Agonist of A3R Prevents EHP-Induced BV-2 Cell Migration
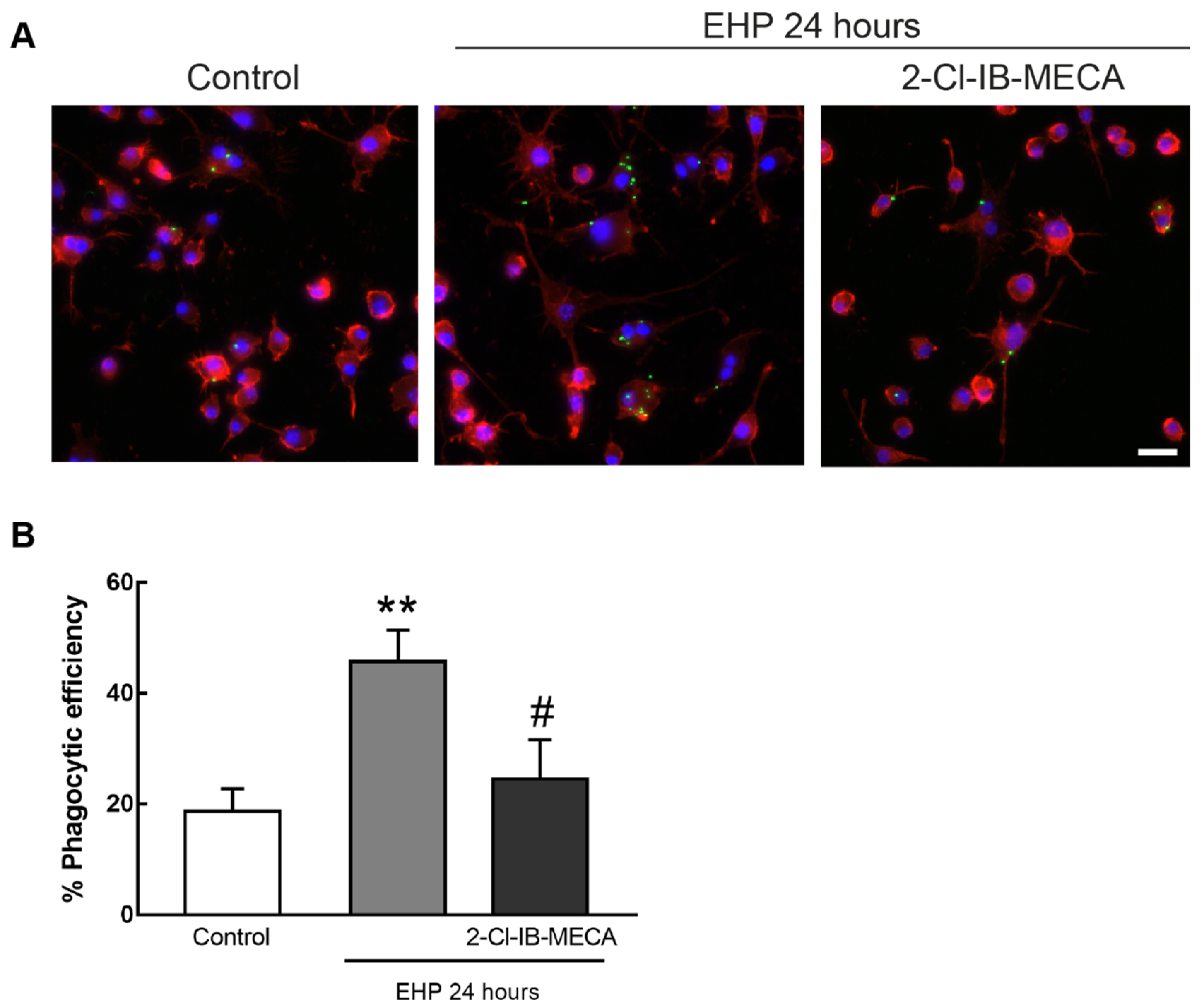
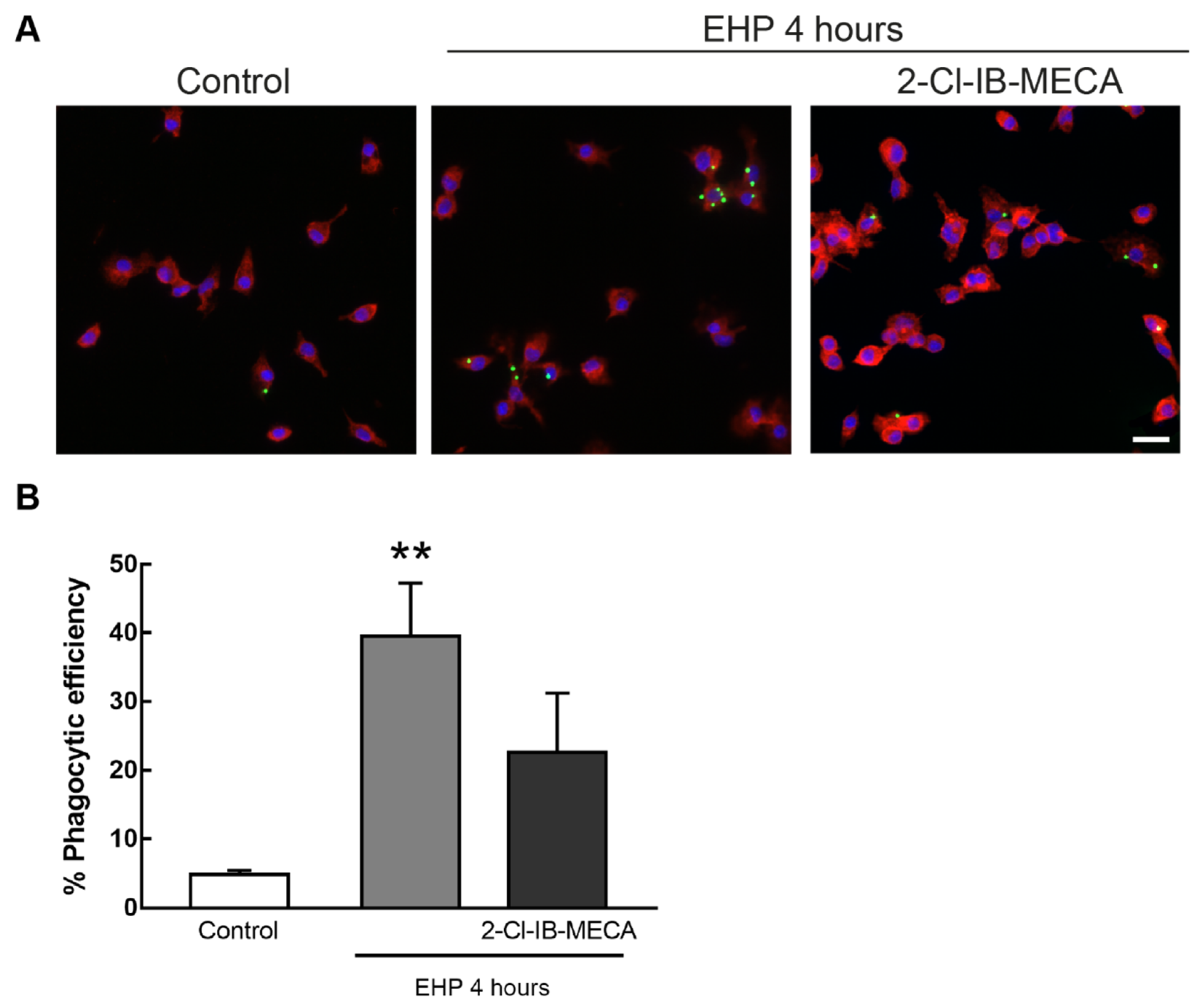
2.4. The Activation of A3R Prevents EHP-Induced Increase in Microglia Phagocytic Efficiency
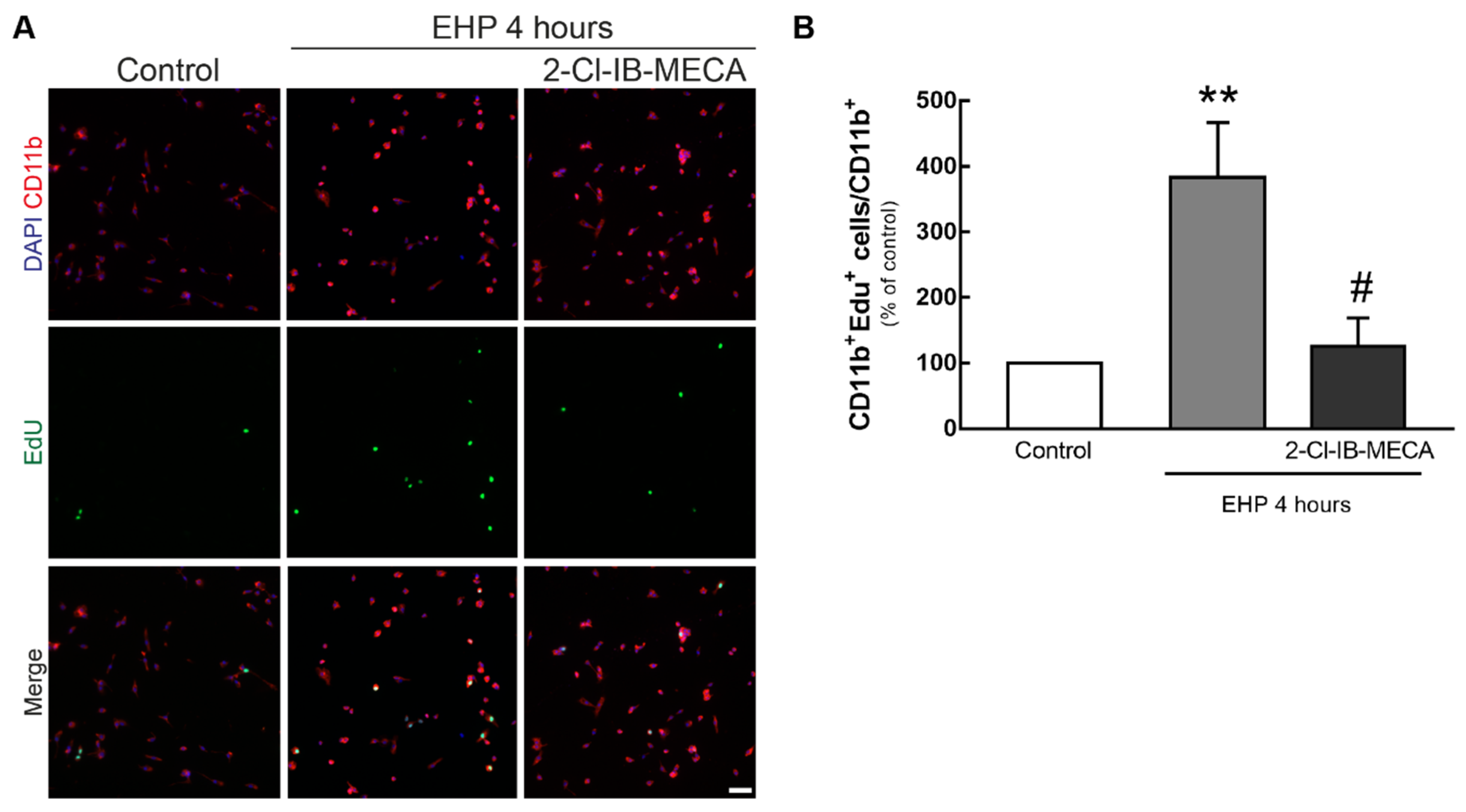
2.5. The Activation of A3R Prevents the Proliferation of Primary Retinal Microglial Cell Elicited by EHP
3. Discussion
4. Materials and Methods
4.1. Microglial Cell Line
4.2. Primary Retinal Microglial Cell Cultures
4.3. Cell Treatment
4.4. Immunocytochemistry
4.5. Densitometric Analysis of iNOS Immunoreactivity
4.6. Scratch Wound Assay
4.7. Boyden Chamber Migration Assay
4.8. Phagocytosis Assay
4.9. Cell Proliferation Assay
4.10. Western Blot
4.11. Image Acquisition and Analysis
4.12. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| A3R | Adenosine A3 receptor |
| BCA | Bicinchoninic acid |
| BSA | Bovine serum albumin |
| CD11b | Cluster of differentiation molecule 11b |
| CTCF | Corrected total cell fluorescence |
| DAPI | 4′,6-diamidino-2-phenylindole |
| DOC | Sodium dexycholate |
| ECF | Enhanced Chemifluorescence |
| ECL | Enhanced Chemiluminescence |
| EDTA | Ethylenediamine tetra-acetic acid |
| EHP | Elevated hydrostatic pressure |
| FBS | Fetal bovine serum |
| HIF-1α | Hypoxia-inducible factor 1-alpha |
| IB-MECA | N6-(3-Iodobenzyl)adenosine-5′-N-methyluronamide |
| iNOS | Inducible nitric oxide synthase |
| IOP | Intraocular pressure |
| LPS | Lipopolysaccharide |
| NMDA | N-methyl-D-aspartate |
| Nos2 | Nitric oxide synthase 2, inducible |
| PFA | Paraformaldehyde |
| Pen/Strep | Penicillin/Streptomycin |
| PVDF | Polyvinyl difluoride |
| RGCs | Retinal ganglion cells |
| RIPA | Radioimmunoprecipitation assay |
| RPMI | Roswell Park Memorial Institute |
| SDS | Sodium dodecyl sulfate |
| TBS-T | Tris-buffered saline with Tween-20 |
| thio-Cl-IB-MECA | 2-chloro-N6-(3-iodobenzyl)-4′-thioadenosine-5′-N-methyluronamide |
| TRITC | Tetramethylrhodamine B isothiocyanate |
References
- Pascolini, D.; Mariotti, S.P. Global estimates of visual impairment: 2010. Br. J. Ophthalmol. 2012, 96, 614–618. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.B.; Aung, T.; Bourne, R.R.; Bron, A.M.; Ritch, R.; Panda-Jonas, S. Glaucoma. Lancet 2017, 390, 2183–2193. [Google Scholar] [CrossRef]
- Cohen, L.P.; Pasquale, L.R. Clinical characteristics and current treatment of glaucoma. Cold Spring Harb. Perspect. Med. 2014, 4. [Google Scholar] [CrossRef]
- Soto, I.; Howell, G.R. The complex role of neuroinflammation in glaucoma. Cold Spring Harb. Perspect. Med. 2014, 4. [Google Scholar] [CrossRef]
- Madeira, M.H.; Boia, R.; Santos, P.F.; Ambrosio, A.F.; Santiago, A.R. Contribution of microglia-mediated neuroinflammation to retinal degenerative diseases. Mediat. Inflamm. 2015, 2015, 673090. [Google Scholar] [CrossRef] [PubMed]
- Naskar, R.; Wissing, M.; Thanos, S. Detection of early neuron degeneration and accompanying microglial responses in the retina of a rat model of glaucoma. Investig. Ophthalmol. Vis. Sci. 2002, 43, 2962–2968. [Google Scholar]
- Liu, S.; Li, Z.W.; Weinreb, R.N.; Xu, G.; Lindsey, J.D.; Ye, C.; Yung, W.H.; Pang, C.P.; Lam, D.S.; Leung, C.K. Tracking retinal microgliosis in models of retinal ganglion cell damage. Investig. Ophthalmol. Vis. Sci. 2012, 53, 6254–6262. [Google Scholar] [CrossRef]
- Chidlow, G.; Ebneter, A.; Wood, J.P.; Casson, R.J. Evidence Supporting an Association Between Expression of Major Histocompatibility Complex II by Microglia and Optic Nerve Degeneration During Experimental Glaucoma. J. Glaucoma 2016, 25, 681–691. [Google Scholar] [CrossRef]
- Madeira, M.H.; Elvas, F.; Boia, R.; Goncalves, F.Q.; Cunha, R.A.; Ambrosio, A.F.; Santiago, A.R. Adenosine A2AR blockade prevents neuroinflammation-induced death of retinal ganglion cells caused by elevated pressure. J. Neuroinflamm. 2015, 12, 115. [Google Scholar] [CrossRef]
- Madeira, M.H.; Boia, R.; Elvas, F.; Martins, T.; Cunha, R.A.; Ambrosio, A.F.; Santiago, A.R. Selective A2A receptor antagonist prevents microglia-mediated neuroinflammation and protects retinal ganglion cells from high intraocular pressure-induced transient ischemic injury. Transl. Res. J. Lab. Clin. Med. 2016, 169, 112–128. [Google Scholar] [CrossRef]
- Bosco, A.; Steele, M.R.; Vetter, M.L. Early microglia activation in a mouse model of chronic glaucoma. J. Comp. Neurol. 2011, 519, 599–620. [Google Scholar] [CrossRef] [PubMed]
- Boia, R.; Elvas, F.; Madeira, M.H.; Aires, I.D.; Rodrigues-Neves, A.C.; Tralhao, P.; Szabo, E.C.; Baqi, Y.; Muller, C.E.; Tome, A.R.; et al. Treatment with A2A receptor antagonist KW6002 and caffeine intake regulate microglia reactivity and protect retina against transient ischemic damage. Cell Death Dis. 2017, 8, e3065. [Google Scholar] [CrossRef]
- Cho, K.J.; Kim, J.H.; Park, H.Y.; Park, C.K. Glial cell response and iNOS expression in the optic nerve head and retina of the rat following acute high IOP ischemia-reperfusion. Brain Res. 2011, 1403, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Schuetz, E.; Thanos, S. Neuro-glial interactions in the adult rat retina after reaxotomy of ganglion cells: Examination of neuron survival and phagocytic microglia using fluorescent tracers. Brain Res. Bull. 2004, 62, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Thanos, S. The Relationship of Microglial Cells to Dying Neurons during Natural Neuronal Cell Death and Axotomy-induced Degeneration of the Rat Retina. Eur. J. Neurosci. 1991, 3, 1189–1207. [Google Scholar] [CrossRef]
- Guo, C.; Qu, X.; Rangaswamy, N.; Leehy, B.; Xiang, C.; Rice, D.; Prasanna, G. A murine glaucoma model induced by rapid in vivo photopolymerization of hyaluronic acid glycidyl methacrylate. PLoS ONE 2018, 13, e0196529. [Google Scholar] [CrossRef]
- Cunha, R.A. How does adenosine control neuronal dysfunction and neurodegeneration? J. Neurochem. 2016, 139, 1019–1055. [Google Scholar] [CrossRef]
- Schulte, G.; Fredholm, B.B. Signalling from adenosine receptors to mitogen-activated protein kinases. Cell Signal. 2003, 15, 813–827. [Google Scholar] [CrossRef]
- Jacobson, K.A.; Merighi, S.; Varani, K.; Borea, P.A.; Baraldi, S.; Aghazadeh Tabrizi, M.; Romagnoli, R.; Baraldi, P.G.; Ciancetta, A.; Tosh, D.K.; et al. A3 Adenosine Receptors as Modulators of Inflammation: From Medicinal Chemistry to Therapy. Med. Res. Rev. 2018, 38, 1031–1072. [Google Scholar] [CrossRef]
- Beach, K.M.; Hung, L.F.; Arumugam, B.; Smith, E.L., 3rd; Ostrin, L.A. Adenosine receptor distribution in Rhesus monkey ocular tissue. Exp. Eye Res. 2018, 174, 40–50. [Google Scholar] [CrossRef]
- Vindeirinho, J.; Costa, G.N.; Correia, M.B.; Cavadas, C.; Santos, P.F. Effect of diabetes/hyperglycemia on the rat retinal adenosinergic system. PLoS ONE 2013, 8, e67499. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Budak, M.T.; Lu, W.; Khurana, T.S.; Zhang, X.; Laties, A.M.; Mitchell, C.H. Identification of the A3 adenosine receptor in rat retinal ganglion cells. Mol. Vis. 2006, 12, 937–948. [Google Scholar]
- Boia, R.; Salinas-Navarro, M.; Gallego-Ortega, A.; Galindo-Romero, C.; Aires, I.D.; Agudo-Barriuso, M.; Ambrosio, A.F.; Vidal-Sanz, M.; Santiago, A.R. Activation of adenosine A3 receptor protects retinal ganglion cells from degeneration induced by ocular hypertension. Cell Death Dis. 2020, 11, 401. [Google Scholar] [CrossRef] [PubMed]
- Galvão, J.; Elvas, F.; Martins, T.; Cordeiro, M.F.; Ambrosio, A.F.; Santiago, A.R. Adenosine A3 receptor activation is neuroprotective against retinal neurodegeneration. Exp. Eye Res. 2015, 140, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, K.I.; Iwao, K.; Inoue, T.; Haga, A.; Tsutsumi, T.; Mochita, M.I.; Fujimoto, T.; Tanihara, H. Stimulation of the adenosine A3 receptor, not the A1 or A2 receptors, promote neurite outgrowth of retinal ganglion cells. Exp. Eye Res. 2018, 170, 160–168. [Google Scholar] [CrossRef]
- Aires, I.D.; Boia, R.; Rodrigues-Neves, A.C.; Madeira, M.H.; Marques, C.; Ambrosio, A.F.; Santiago, A.R. Blockade of microglial adenosine A2A receptor suppresses elevated pressure-induced inflammation, oxidative stress, and cell death in retinal cells. Glia 2019, 67, 896–914. [Google Scholar] [CrossRef]
- Hammarberg, C.; Schulte, G.; Fredholm, B.B. Evidence for functional adenosine A3 receptors in microglia cells. J. Neurochem. 2003, 86, 1051–1054. [Google Scholar] [CrossRef]
- Rodrigues-Neves, A.C.; Aires, I.D.; Vindeirinho, J.; Boia, R.; Madeira, M.H.; Goncalves, F.Q.; Cunha, R.A.; Santos, P.F.; Ambrosio, A.F.; Santiago, A.R. Elevated Pressure Changes the Purinergic System of Microglial Cells. Front. Pharmacol. 2018, 9, 16. [Google Scholar] [CrossRef]
- Trincavelli, M.L.; Tuscano, D.; Marroni, M.; Falleni, A.; Gremigni, V.; Ceruti, S.; Abbracchio, M.P.; Jacobson, K.A.; Cattabeni, F.; Martini, C. A3 adenosine receptors in human astrocytoma cells: Agonist-mediated desensitization, internalization, and down-regulation. Mol. Pharmacol. 2002, 62, 1373–1384. [Google Scholar] [CrossRef]
- Ochaion, A.; Bar-Yehuda, S.; Cohen, S.; Amital, H.; Jacobson, K.A.; Joshi, B.V.; Gao, Z.G.; Barer, F.; Patoka, R.; Del Valle, L.; et al. The A3 adenosine receptor agonist CF502 inhibits the PI3K, PKB/Akt and NF-kappaB signaling pathway in synoviocytes from rheumatoid arthritis patients and in adjuvant-induced arthritis rats. Biochem. Pharmacol. 2008, 76, 482–494. [Google Scholar] [CrossRef]
- Martin, L.; Pingle, S.C.; Hallam, D.M.; Rybak, L.P.; Ramkumar, V. Activation of the adenosine A3 receptor in RAW 264.7 cells inhibits lipopolysaccharide-stimulated tumor necrosis factor-alpha release by reducing calcium-dependent activation of nuclear factor-kappaB and extracellular signal-regulated kinase 1/2. J. Pharmacol. Exp. Ther. 2006, 316, 71–78. [Google Scholar] [CrossRef]
- Lee, J.Y.; Jhun, B.S.; Oh, Y.T.; Lee, J.H.; Choe, W.; Baik, H.H.; Ha, J.; Yoon, K.S.; Kim, S.S.; Kang, I. Activation of adenosine A3 receptor suppresses lipopolysaccharide-induced TNF-alpha production through inhibition of PI 3-kinase/Akt and NF-kappaB activation in murine BV2 microglial cells. Neurosci. Lett. 2006, 396, 1–6. [Google Scholar] [CrossRef]
- Lee, H.S.; Chung, H.J.; Lee, H.W.; Jeong, L.S.; Lee, S.K. Suppression of inflammation response by a novel A(3) adenosine receptor agonist thio-Cl-IB-MECA through inhibition of Akt and NF-kappaB signaling. Immunobiology 2011, 216, 997–1003. [Google Scholar] [CrossRef]
- Terayama, R.; Tabata, M.; Maruhama, K.; Iida, S. A3 adenosine receptor agonist attenuates neuropathic pain by suppressing activation of microglia and convergence of nociceptive inputs in the spinal dorsal horn. Exp. Brain Res. 2018, 236, 3203–3213. [Google Scholar] [CrossRef]
- Borea, P.A.; Varani, K.; Vincenzi, F.; Baraldi, P.G.; Tabrizi, M.A.; Merighi, S.; Gessi, S. The A3 adenosine receptor: History and perspectives. Pharmacol. Rev. 2015, 67, 74–102. [Google Scholar] [CrossRef]
- Hasko, G.; Szabo, C.; Nemeth, Z.H.; Kvetan, V.; Pastores, S.M.; Vizi, E.S. Adenosine receptor agonists differentially regulate IL-10, TNF-alpha, and nitric oxide production in RAW 264.7 macrophages and in endotoxemic mice. J. Immunol. 1996, 157, 4634–4640. [Google Scholar] [PubMed]
- Xavier, A.L.; Menezes, J.R.; Goldman, S.A.; Nedergaard, M. Fine-tuning the central nervous system: Microglial modelling of cells and synapses. Philos. Trans. R. Soc. Lond. Ser. Biol. Sci. 2014, 369, 20130593. [Google Scholar] [CrossRef] [PubMed]
- Choi, I.Y.; Lee, J.C.; Ju, C.; Hwang, S.; Cho, G.S.; Lee, H.W.; Choi, W.J.; Jeong, L.S.; Kim, W.K. A3 adenosine receptor agonist reduces brain ischemic injury and inhibits inflammatory cell migration in rats. Am. J. Pathol. 2011, 179, 2042–2052. [Google Scholar] [CrossRef]
- Ohsawa, K.; Sanagi, T.; Nakamura, Y.; Suzuki, E.; Inoue, K.; Kohsaka, S. Adenosine A3 receptor is involved in ADP-induced microglial process extension and migration. J. Neurochem. 2012, 121, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Haynes, S.E.; Hollopeter, G.; Yang, G.; Kurpius, D.; Dailey, M.E.; Gan, W.B.; Julius, D. The P2Y12 receptor regulates microglial activation by extracellular nucleotides. Nat. Neurosci. 2006, 9, 1512–1519. [Google Scholar] [CrossRef]
- Miller, A.M.; Stella, N. Microglial cell migration stimulated by ATP and C5a involve distinct molecular mechanisms: Quantification of migration by a novel near-infrared method. Glia 2009, 57, 875–883. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, P.C. Assays of leukocyte locomotion and chemotaxis. J. Immunol. Methods 1998, 216, 139–153. [Google Scholar] [CrossRef]
- Welch, M.D.; Mullins, R.D. Cellular Control of Actin Nucleation. Annu. Rev. Cell Dev. Biol. 2002, 18, 247–288. [Google Scholar] [CrossRef] [PubMed]
- Kettenmann, H.; Hanisch, U.K.; Noda, M.; Verkhratsky, A. Physiology of microglia. Physiol. Rev. 2011, 91, 461–553. [Google Scholar] [CrossRef]
- Langmann, T. Microglia activation in retinal degeneration. J. Leukoc. Biol. 2007, 81, 1345–1351. [Google Scholar] [CrossRef]
- Streit, W.J. Chapter 2—The Role of Microglia in Neurotoxicity. In The Role of Glia in Neurotoxicity; Aschner, M., Costa, L.G., Eds.; CRC Press: Boca Raton, FL, USA, 2004; p. 480. [Google Scholar]
- Barron, K.D. The microglial cell. A historical review. J. Neurol. Sci. 1995, 134, 57–68. [Google Scholar] [CrossRef]
- Inman, D.M.; Horner, P.J. Reactive nonproliferative gliosis predominates in a chronic mouse model of glaucoma. Glia 2007, 55, 942–953. [Google Scholar] [CrossRef]
- Kuehn, S.; Reinehr, S.; Stute, G.; Rodust, C.; Grotegut, P.; Hensel, A.T.; Dick, H.B.; Joachim, S.C. Interaction of complement system and microglia activation in retina and optic nerve in a NMDA damage model. Mol. Cell. Neurosci. 2018, 89, 95–106. [Google Scholar] [CrossRef]

| Supplier (Cat. No.) | Host | Application | Dilution | |
|---|---|---|---|---|
| Primary antibodies | ||||
| Anti-iNOS | Santa Cruz (SC-650) | Rabbit | Immunocytochemistry | 1:1000 |
| Western Blot | 1:500 | |||
| Anti-CD11b | Bio-Rad (MCA 275G) | Mouse | Immunocytochemistry | 1:500 |
| Anti-A3R | Millipore (AB1590P) | Rabbit | Western Blot | 1:1000 |
| Anti-Calnexin | Sicgen (AB0041-500) | Goat | Western Blot | 1:5000 |
| Secondary antibodies | ||||
| Alexa Fluor® 488 anti-rabbit IgG (H+L) | Thermo Fisher Scientific (A11008) | Goat | Immunocytochemistry | 1:500 |
| Alexa Fluor® 568 anti-mouse IgG (H+L) | Thermo Fisher Scientific (A11004) | Goat | Immunocytochemistry | 1:500 |
| Alkaline phosphatase anti-rabbit IgG | Sigma (A3687) | Goat | Western Blot | 1:10,000 |
| Alkaline phosphatase anti-goat IgG | Thermo Fisher Scientific (31–300) | Rabbit | Western Blot | 1:10,000 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferreira-Silva, J.; Aires, I.D.; Boia, R.; Ambrósio, A.F.; Santiago, A.R. Activation of Adenosine A3 Receptor Inhibits Microglia Reactivity Elicited by Elevated Pressure. Int. J. Mol. Sci. 2020, 21, 7218. https://doi.org/10.3390/ijms21197218
Ferreira-Silva J, Aires ID, Boia R, Ambrósio AF, Santiago AR. Activation of Adenosine A3 Receptor Inhibits Microglia Reactivity Elicited by Elevated Pressure. International Journal of Molecular Sciences. 2020; 21(19):7218. https://doi.org/10.3390/ijms21197218
Chicago/Turabian StyleFerreira-Silva, Joana, Inês D. Aires, Raquel Boia, António Francisco Ambrósio, and Ana Raquel Santiago. 2020. "Activation of Adenosine A3 Receptor Inhibits Microglia Reactivity Elicited by Elevated Pressure" International Journal of Molecular Sciences 21, no. 19: 7218. https://doi.org/10.3390/ijms21197218
APA StyleFerreira-Silva, J., Aires, I. D., Boia, R., Ambrósio, A. F., & Santiago, A. R. (2020). Activation of Adenosine A3 Receptor Inhibits Microglia Reactivity Elicited by Elevated Pressure. International Journal of Molecular Sciences, 21(19), 7218. https://doi.org/10.3390/ijms21197218






