The Association between Excess Body Mass and Disturbances in Somatic Mineral Levels
Abstract
1. Introduction
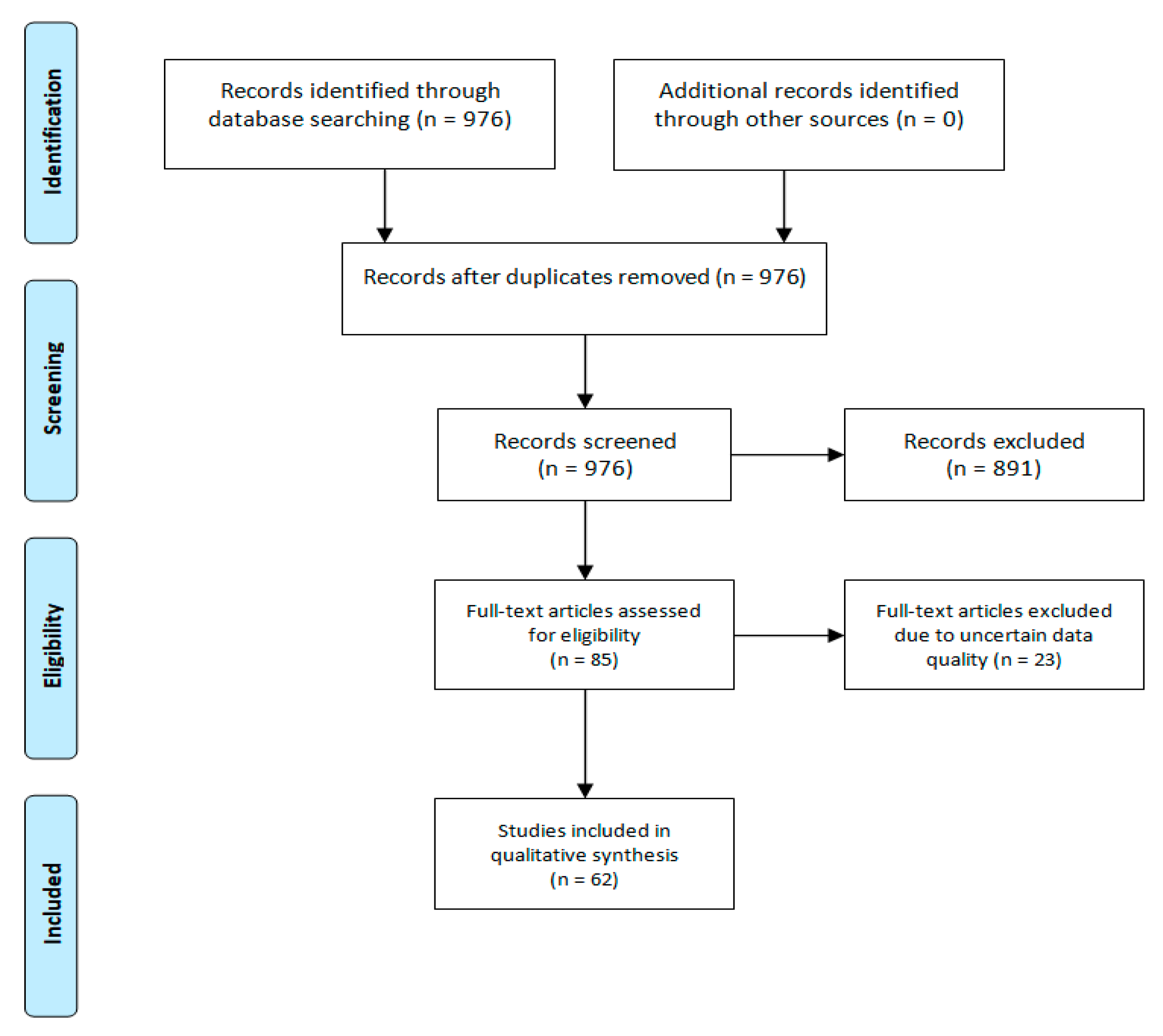
2. Methodology
3. Results and Discussion
3.1. Iron
3.2. Calcium
3.3. Magnesium
3.4. Trace Elements
3.4.1. Copper
3.4.2. Selenium
3.4.3. Zinc
3.4.4. Iodine
3.4.5. Chromium
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| %BF | percentage body fat |
| A2M | alpha2-macroglobulin |
| APR | acute phase response |
| ATPase | adenosine 5′-triphosphatase |
| BMI | body mass index |
| Ca | calcium |
| Cp | ceruloplasmin |
| Cr | chromium |
| CrCl3 | chromium chloride |
| CRP | C-reactive protein |
| CrPic | Cr picolinate |
| Cu | copper |
| CVD | cardiovascular disease |
| DNA | deoxyribonucleic acid |
| Fe | iron |
| GTF | glucose tolerance factor |
| IDA | iron-deficiency anemia |
| LDL | low-density lipoprotein |
| LOE | level of evidence |
| Mg | magnesium |
| mRNA | messenger ribonucleic acid |
| NAFLD | nonalcoholic fatty liver disease |
| NASH | nonalcoholic steatohepatitis |
| NBC | niacin-bound Cr |
| NIS | sodium/iodide symporter |
| ROS | reactive oxygen species |
| Se | selenium |
| SOD | superoxide dismutase |
| SSAO | semicarbazide-sensitive amine oxidase |
| UIC | urine iodine concentration |
| VEGF | vascular endothelial growth factor |
| ZAG | zinc-alpha-2-glycoprotein |
| Zn | zinc |
References
- Levesque, R.J.R. Obesity and Overweight. In Encyclopedia of Adolescence; Levesque, R.J.R., Ed.; Springer: London, UK, 2011; pp. 1913–1915. [Google Scholar]
- Chooi, Y.C.; Ding, C.; Magkos, F. The epidemiology of obesity. Metabolism 2019, 92, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Dobbs, R.; Sawers, C.; Thompson, F.; Manyika, J.; Woetzel, J.; Child, P.; McKenna, S.; Spatharou, A. Overcoming Obesity: An Initial Economic Analysis; McKinsey Global Institute: New York, NY, USA, 2014; pp. 1–120. [Google Scholar]
- World Health Organization. Mortality and Burden of Disease Attributable to Selected Major Risks; World Health Organization: Geneva, Switzerland, 2009; pp. 1–70. ISBN 9789241563871. [Google Scholar]
- Grandone, A.; Marzuillo, P.; Perrone, L.; del Giudice, E.M. Iron metabolism dysregulation and cognitive dysfunction in pediatric obesity: Is there a connection? Nutrients 2015, 7, 9163–9170. [Google Scholar] [CrossRef]
- Elaïb, Z.; Lopez, J.J.; Coupaye, M.; Zuber, K.; Becker, Y.; Kondratieff, A.; Repérant, C.; Pépin, M.; Salomon, L.; Teillet, F.; et al. Platelet Functions are Decreased in Obesity and Restored after Weight Loss: Evidence for a Role of the SERCA3-Dependent ADP Secretion Pathway. Thromb. Haemost. 2019, 119, 384–396. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Q.; Lin, R.; Nong, Q. Adiposity and serum selenium in USA adults. Nutrients 2018, 10, 727. [Google Scholar] [CrossRef] [PubMed]
- Lecube, A.; Zafon, C.; Gromaz, A.; Fort, J.M.; Caubet, E.; Baena, J.A.; Tortosa, F. Iodine Deficiency Is Higher in Morbid Obesity in Comparison with Late After Bariatric Surgery and Non-obese Women. Obes. Surg. 2015, 25, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Kaur, A.; Johnston, D.G. Does metabolic health in overweight and obesity persist—Individual variation and cardiovascular mortality over two decades. Eur. J. Endocrinol. 2016, 175, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Corey, K.E.; Kaplan, L.M. Obesity and liver disease. The epidemic of the twenty-first century. Clin. Liver Dis. 2014, 18, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, B.J.; Stults, H.B.; Mayer, J. Hypoferraemia in obese adolescents. Lancet 1962, 2, 327–328. [Google Scholar] [CrossRef]
- Coates, C.J.; Decker, H. Immunological properties of oxygen-transport proteins: Hemoglobin, hemocyanin and hemerythrin. Cell. Mol. Life Sci. 2016, 74, 293–317. [Google Scholar] [CrossRef]
- Jones, A.D.; Zhao, G.; Jiang, Y.P.; Zhou, M.; Xu, G.; Kaciroti, N.; Zhang, Z.; Lozoff, B. Maternal obesity during pregnancy is negatively associated with maternal and neonatal iron status. Eur. J. Clin. Nutr. 2016, 70, 918–924. [Google Scholar] [CrossRef]
- Hutchinson, C. A review of iron studies in overweight and obese children and adolescents: A double burden in the young? Eur. J. Nutr. 2016, 55, 2179–2197. [Google Scholar] [CrossRef] [PubMed]
- Cepeda-Lopez, A.C.; Melse-Boonstra, A.; Zimmermann, M.B.; Herter-Aeberli, I. In overweight and obese women, dietary iron absorption is reduced and the enhancement of iron absorption by ascorbic acid is one-half that in normal-weight women. Am. J. Clin. Nutr. 2015, 102, 1389–1397. [Google Scholar] [CrossRef] [PubMed]
- Citelli, M.; Fonte-Faria, T.; Nascimento-Silva, V.; Renovato-Martins, M.; Silva, R.; Luna, A.; Silva, S.; Barja-Fidalgo, C. Obesity Promotes Alterations in Iron Recycling. Nutrients 2015, 7, 335–348. [Google Scholar] [CrossRef] [PubMed]
- Skrypnik, D.; Mostowska, A.; Jagodziński, P.P.; Bogdański, P. Association of rs699947 (−2578 C/A) and rs2010963 (−634 G/C) Single Nucleotide Polymorphisms of the VEGF Gene, VEGF-A and Leptin Serum Level, and Cardiovascular Risk in Patients with Excess Body Mass: A Case–Control Study. J. Clin. Med. 2020, 9, 469. [Google Scholar] [CrossRef] [PubMed]
- Gruys, E.; Toussaint, M.J.M.; Niewold, T.A.; Koopmans, S.J. Acute phase reaction and acute phase proteins. J. Zhejiang Univ. Sci. 2005, 6, 1045–1056. [Google Scholar] [CrossRef] [PubMed]
- Oldewage-Theron, W.H.; Egal, A.A.; Grobler, C.J. Is obesity associated with iron status in the elderly? A case study from Sharpeville, South Africa. Public Health Nutr. 2015, 18, 521–529. [Google Scholar] [CrossRef]
- Rad, H.A.; Asghar Sefidgar, S.A.; Tamadoni, A.; Sedaghat, S.; Bakouei, F.; Bijani, A.; Omidvar, S. Obesity and iron-deficiency anemia in women of reproductive age in northern Iran. J. Educ. Health Promot. 2019, 8. [Google Scholar] [CrossRef]
- Wang, H.; Jiang, X.; Wu, J.; Zhang, L.; Huang, J.; Zhang, Y.; Zou, X.; Liang, B. Iron overload coordinately promotes ferritin expression and fat accumulation in Caenorhabditis Elegans. Genetics 2016, 203, 241–253. [Google Scholar] [CrossRef]
- Hasebe, T.; Tanaka, H.; Sawada, K.; Nakajima, S.; Ohtake, T.; Fujiya, M.; Kohgo, Y. Bone morphogenetic protein-binding endothelial regulator of liver sinusoidal endothelial cells induces iron overload in a fatty liver mouse model. J. Gastroenterol. 2017, 52, 341–351. [Google Scholar] [CrossRef]
- Tallis, J.; James, R.S.; Seebacher, F. The effects of obesity on skeletal muscle contractile function. J. Exp. Biol. 2018, 221. [Google Scholar] [CrossRef]
- Ciapaite, J.; van den Berg, S.A.; Houten, S.M.; Nicolay, K.; Willems van Dijk, K.; Jeneson, J.A. Fiber-type-specific sensitivities and phenotypic adaptations to dietary fat overload differentially impact fast- versus slow-twitch muscle contractile function in C57BL/6J mice. J. Nutr. Biochem. 2015, 26, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Eshima, H.; Tamura, Y.; Kakehi, S.; Kurebayashi, N.; Murayama, T.; Nakamura, K.; Kakigi, R.; Okada, T.; Sakurai, T.; Kawamori, R.; et al. Long-term, but not short-term high-fat diet induces fiber composition changes and impaired contractile force in mouse fast-twitch skeletal muscle. Physiol. Rep. 2017, 5. [Google Scholar] [CrossRef] [PubMed]
- Espinosa, A.; Henríquez-Olguín, C.; Jaimovich, E. Reactive oxygen species and calcium signals in skeletal muscle: A crosstalk involved in both normal signaling and disease. Cell Calcium 2016, 60, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Di Meo, S.; Iossa, S.; Venditti, P. Improvement of obesity-linked skeletal muscle insulin resistance by strength and endurance training. J. Endocrinol. 2017, 234, R159–R181. [Google Scholar] [CrossRef]
- Orfanos, S.; Jude, J.; Deeney, B.T.; Cao, G.; Rastogi, D.; van Zee, M.; Pushkarsky, I.; Munoz, H.E.; Damoiseaux, R.; Di Carlo, D.; et al. Obesity increases airway smooth muscle responses to contractile agonists. Am. J. Physiol. Lung Cell. Mol. Physiol. 2018, 315, L673–L681. [Google Scholar] [CrossRef]
- Deus, A.F.; Vileigas, D.F.; Silva, D.C.T.; Tomasi, L.C.; Campos, D.H.S.; Okoshi, K.; Padovani, C.R.; Cicogna, A.C. Cardiac function and intracellular Ca2 + handling proteins are not impaired by high-saturated-fat diet-induced obesity. Brazilian J. Med. Biol. Res. 2019, 52. [Google Scholar] [CrossRef]
- Bertinato, J.; Wu Xiao, C.; Ratnayake, W.M.N.; Fernandez, L.; Lavergne, C.; Wood, C.; Swist, E. Lower serum magnesium concentration is associated with diabetes, insulin resistance, and obesity in South Asian and white Canadian women but not men. Food Nutr. Res. 2015, 59, 25974. [Google Scholar] [CrossRef]
- Morais, J.B.S.; Severo, J.S.; dos Santos, L.R.; de Sousa Melo, S.R.; de Oliveira Santos, R.; de Oliveira, A.R.S.; Cruz, K.J.C.; do Nascimento Marreiro, D. Role of Magnesium in Oxidative Stress in Individuals with Obesity. Biol. Trace Elem. Res. 2017, 176, 20–26. [Google Scholar] [CrossRef]
- Kolisek, M.; Montezano, A.C.; Sponder, G.; Anagnostopoulou, A.; Vormann, J.; Touyz, R.M.; Aschenbach, J.R. PARK7/DJ-1 dysregulation by oxidative stress leads to magnesium deficiency: Implications in degenerative and chronic diseases. Clin. Sci. 2015, 129, 1143–1150. [Google Scholar] [CrossRef]
- Hosseini, B.; Saedisomeolia, A.; Allman-Farinelli, M. Association Between Antioxidant Intake/Status and Obesity: A Systematic Review of Observational Studies. Biol. Trace Elem. Res. 2017, 175, 287–297. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Flores-García, A.; Saldaña-Guerrero, S.; Simental-Mendía, L.E.; Rodríguez-Morán, M. Obesity and hypomagnesemia. Eur. J. Intern. Med. 2016, 34, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Kew, K.M.; Kirtchuk, L.; Michell, C.I. Intravenous magnesium sulfate for treating adults with acute asthma in the emergency department. Cochrane Database Syst. Rev. 2014, 2014. [Google Scholar] [CrossRef]
- Cahill, F.; Shahidi, M.; Shea, J.; Wadden, D.; Gulliver, W.; Randell, E.; Vasdev, S.; Sun, G. High Dietary Magnesium Intake Is Associated with Low Insulin Resistance in the Newfoundland Population. PLoS ONE 2013, 8. [Google Scholar] [CrossRef] [PubMed]
- Morais, J.B.S.; Severo, J.S.; de Oliveira, A.R.S.; Cruz, K.J.C.; da Silva Dias, T.M.; de Assis, R.C.; Colli, C.; do Nascimento Marreiro, D. Magnesium Status and Its Association with Oxidative Stress in Obese Women. Biol. Trace Elem. Res. 2017, 175, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Skalnaya, M.G.; Skalny, A.V.; Grabeklis, A.R.; Serebryansky, E.P.; Demidov, V.A.; Tinkov, A.A. Hair Trace Elements in Overweight and Obese Adults in Association with Metabolic Parameters. Biol. Trace Elem. Res. 2018, 186, 12–20. [Google Scholar] [CrossRef]
- Skrypnik, D.; Bogdański, P.; Skrypnik, K.; Mądry, E.; Karolkiewicz, J.; Szulińska, M.; Suliburska, J.; Walkowiak, J. Influence of endurance and endurance-strength training on mineral status in women with abdominal obesity: A randomized trial. Medicine 2019, 98, e14909. [Google Scholar] [CrossRef]
- Yang, H.; Liu, C.N.; Wolf, R.M.; Ralle, M.; Dev, S.; Pierson, H.; Askin, F.; Steele, K.E.; Magnuson, T.H.; Schweitzer, M.A.; et al. Obesity is associated with copper elevation in serum and tissues. Metallomics 2019, 11, 1363–1371. [Google Scholar] [CrossRef]
- Fan, Y.; Zhang, C.; Bu, J. Relationship between selected serum metallic elements and obesity in children and adolescent in the USA. Nutrients 2017, 9, 104. [Google Scholar] [CrossRef]
- Habib, S.A.; Saad, E.A.; Elsharkawy, A.A.; Attia, Z.R. Pro-inflammatory adipocytokines, oxidative stress, insulin, Zn and Cu: Interrelations with obesity in Egyptian non-diabetic obese children and adolescents. Adv. Med. Sci. 2015, 60, 179–185. [Google Scholar] [CrossRef]
- Kazi, T.G.; Afridi, H.I.; Kazi, N.; Jamali, M.K.; Arain, M.B.; Jalbani, N.; Kandhro, G.A. Copper, chromium, manganese, iron, nickel, and zinc levels in biological samples of diabetes mellitus patients. Biol. Trace Elem. Res. 2008, 122, 1–18. [Google Scholar] [CrossRef]
- Jaksic, M.; Martinovic, M.; Gligorovic-Barhanovic, N.; Vujacic, A.; Djurovic, D.; Nedovic-Vukovic, M. Association between inflammation, oxidative stress, vitamin D, copper and zinc with pre-obesity and obesity in school children from the city of Podgorica, Montenegro. J. Pediatr. Endocrinol. Metab. 2019, 32, 951–957. [Google Scholar] [CrossRef] [PubMed]
- Asghari, G.; Khalaj, A.; Ghadimi, M.; Mahdavi, M.; Farhadnejad, H.; Valizadeh, M.; Azizi, F.; Barzin, M.; Hosseinpanah, F. Prevalence of Micronutrient Deficiencies Prior to Bariatric Surgery: Tehran Obesity Treatment Study (TOTS). Obes. Surg. 2018, 28, 2465–2472. [Google Scholar] [CrossRef] [PubMed]
- Calderón, B.; Hevia, V.; Vega-Piñero, B.; Martín-Hidalgo, A.; Mendez-del Sol, H.; Escobar-Morreale, H.F.; Botella-Carretero, J.I. Serum Retinol, Folic Acid, and Copper Are Associated with Sperm Abnormalities in Men with Obesity. J. Am. Coll. Nutr. 2018, 37, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Carpéné, C.; Boulet, N.; Chaplin, A.; Mercader, J. Past, Present and Future Anti-Obesity Effects of Flavin-Containing and/or Copper-Containing Amine Oxidase Inhibitors. Medicines 2019, 6, 9. [Google Scholar] [CrossRef]
- Krishnamoorthy, L.; Cotruvo, J.A.; Chan, J.; Kaluarachchi, H.; Muchenditsi, A.; Pendyala, V.S.; Jia, S.; Aron, A.T.; Ackerman, C.M.; Wal, M.N.V.; et al. Copper regulates cyclic-AMP-dependent lipolysis. Nat. Chem. Biol. 2016, 12, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Klecha, B.; Bukowska, B. Selenium in human organism—Characteristic of the element and its potential therapeutic applocation. Bromatol. Chem. Toksykol. 2016, 4, 818–829. [Google Scholar]
- Błazewicz, A.; Klatka, M.; Astel, A.; Korona-Glowniak, I.; Dolliver, W.; Szwerc, W.; Kocjan, R. Serum and urinary selenium levels in obese children: A cross-sectional study. J. Trace Elem. Med. Biol. 2015, 29, 116–122. [Google Scholar] [CrossRef]
- Martins, L.M.; de Oliveira, A.R.S.; Cruz, K.J.C.; de Araújo, C.G.B.; de Oliveira, F.E.; de Sousa, G.S.; Nogueira, N.N.; Marreiro, D.N. Influencia del cortisol sobre el metabolismo del zinc en mujeres obesas mórbidas. Nutr. Hosp. 2014, 29, 57–63. [Google Scholar] [CrossRef]
- Severo, J.S.; Morais, J.B.S.; Beserra, J.B.; dos Santos, L.R.; de Sousa Melo, S.R.; de Sousa, G.S.; de Matos Neto, E.M.; Henriques, G.S.; do Nascimento Marreiro, D. Role of Zinc in Zinc-α2-Glycoprotein Metabolism in Obesity: A Review of Literature. Biol. Trace Elem. Res. 2020, 193, 81–88. [Google Scholar] [CrossRef]
- Begin-Heick, N.; Dalpe-Scott, M.; Rowe, J.; Heick, H.M.C. Zinc supplementation attenuates insulin secretory activity in pancreatic islets of the ob/ob mouse. Diabetes 1985, 34, 179–184. [Google Scholar] [CrossRef]
- Payahoo, L.; Ostadrahimi, A.; Mobasseri, M.; Bishak, Y.K.; Farrin, N.; Jafarabadi, M.A.; Mahluji, S. Effects of zinc supplementation on the anthropometric measurements, lipid profiles and fasting blood glucose in the healthy obese adults. Adv. Pharm. Bull. 2013, 3, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Pyka, B.; Zieleń-Zynel, I.; Kowalska, J.; Ziółkowski, G.; Hudzik, B.; Gąsior, M.; Zubulewicz-Szkodzińska, B. Dietary recommendations for iodine intake—In search of a consensus between cardiologists and endocrinologists. Folia Cardiol. 2019, 14, 161–165. [Google Scholar]
- Jeejeebhoy, K.N.; Hu, F.B. The role of chromium in nutrition and therapeutics and as a potential toxin. Nutr. Rev. 1999, 57, 329–335. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. Office of Dietary Supplements National Institutes of Health Dietary Supplement Fact Sheet Iron—Health Professional Fact Sheet. Natl. Institutes Heal. Diet. Suppl. 2016. Available online: https://ods.od.nih.gov/factsheets/Iron-HealthProfessional/ (accessed on 15 August 2016).
- Offenbacher, E.G.; Pi-Sunyer, F.X. Beneficial effect of chromium-rich yeast on glucose tolerance and blood lipids in elderly subjects. Diabetes 1980, 29, 919–925. [Google Scholar] [CrossRef]
- Albarracin, C.A.; Fuqua, B.C.; Evans, J.L.; Goldfine, I.D. Chromium picolinate and biotin combination improves glucose metabolism in treated, uncontrolled overweight to obese patients with type 2 diabetes. Diabetes. Metab. Res. Rev. 2008, 24, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Zafra-Stone, S.; Yasmin, T.; Bagchi, M.; Chatterjee, A.; Vinson, J.A.; Bagchi, D. Berry anthocyanins as novel antioxidants in human health and disease prevention. Mol. Nutr. Food Res. 2007, 51, 675–683. [Google Scholar] [CrossRef]
- Grant, K.E.; Chandler, R.M.; Castle, A.L.; Ivy, J.L. Chromium and exercise training: Effect on obese women. Med. Sci. Sports Exerc. 1997, 29, 992–998. [Google Scholar] [CrossRef]
- Crawford, V.; Scheckenbach, R.; Preuss, H.G. Effects of niacin-bound chromium supplementation on body composition in overweight African-American women. Diabetes Obes. Metab. 1999, 1, 331–337. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banach, W.; Nitschke, K.; Krajewska, N.; Mongiałło, W.; Matuszak, O.; Muszyński, J.; Skrypnik, D. The Association between Excess Body Mass and Disturbances in Somatic Mineral Levels. Int. J. Mol. Sci. 2020, 21, 7306. https://doi.org/10.3390/ijms21197306
Banach W, Nitschke K, Krajewska N, Mongiałło W, Matuszak O, Muszyński J, Skrypnik D. The Association between Excess Body Mass and Disturbances in Somatic Mineral Levels. International Journal of Molecular Sciences. 2020; 21(19):7306. https://doi.org/10.3390/ijms21197306
Chicago/Turabian StyleBanach, Weronika, Karolina Nitschke, Natalia Krajewska, Wojciech Mongiałło, Oskar Matuszak, Józef Muszyński, and Damian Skrypnik. 2020. "The Association between Excess Body Mass and Disturbances in Somatic Mineral Levels" International Journal of Molecular Sciences 21, no. 19: 7306. https://doi.org/10.3390/ijms21197306
APA StyleBanach, W., Nitschke, K., Krajewska, N., Mongiałło, W., Matuszak, O., Muszyński, J., & Skrypnik, D. (2020). The Association between Excess Body Mass and Disturbances in Somatic Mineral Levels. International Journal of Molecular Sciences, 21(19), 7306. https://doi.org/10.3390/ijms21197306





