Austalide K from the Fungus Penicillium rudallense Prevents LPS-Induced Bone Loss in Mice by Inhibiting Osteoclast Differentiation and Promoting Osteoblast Differentiation
Abstract
:1. Introduction
2. Results
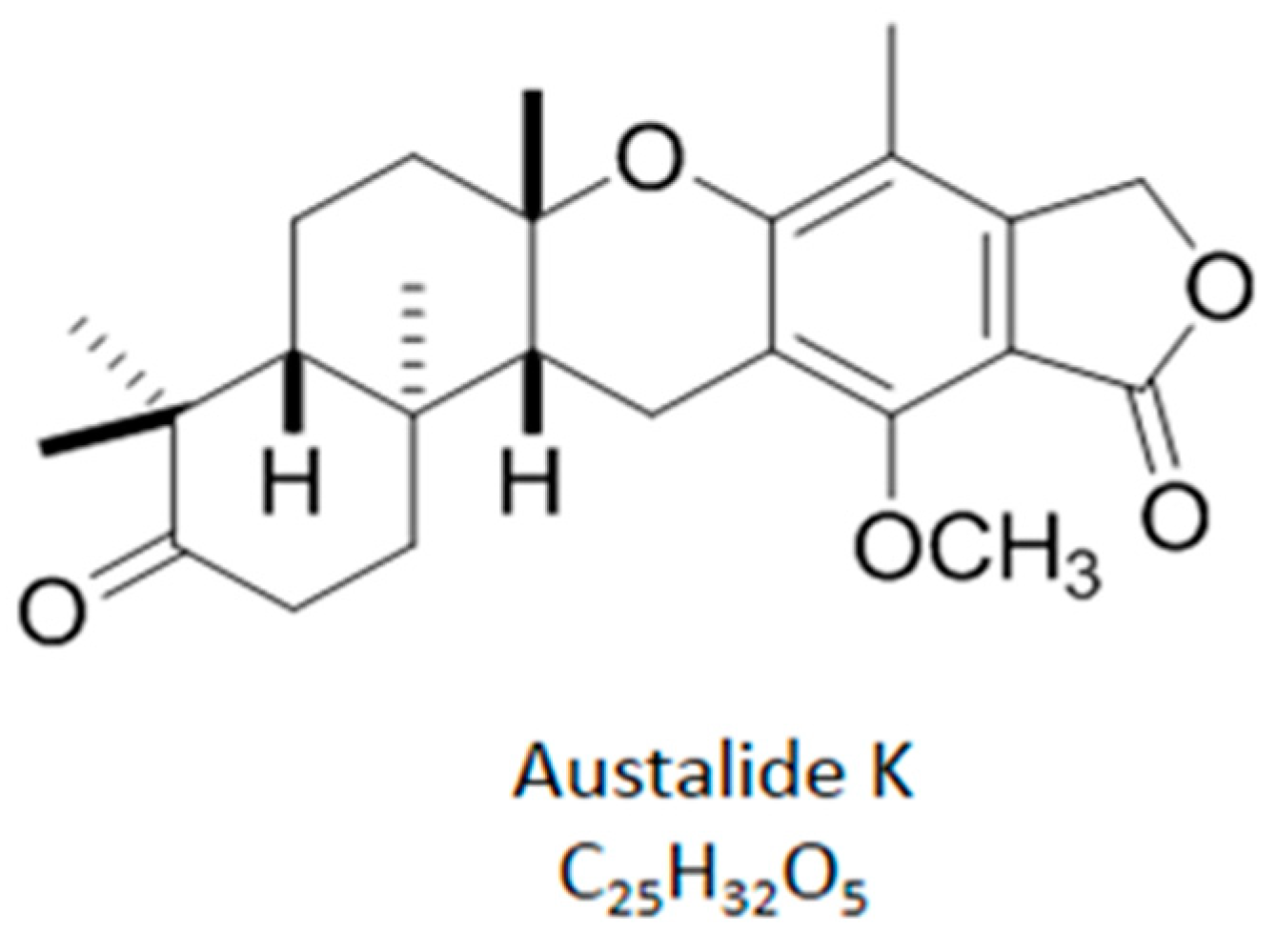
2.1. Chemical Structure of Austalide K
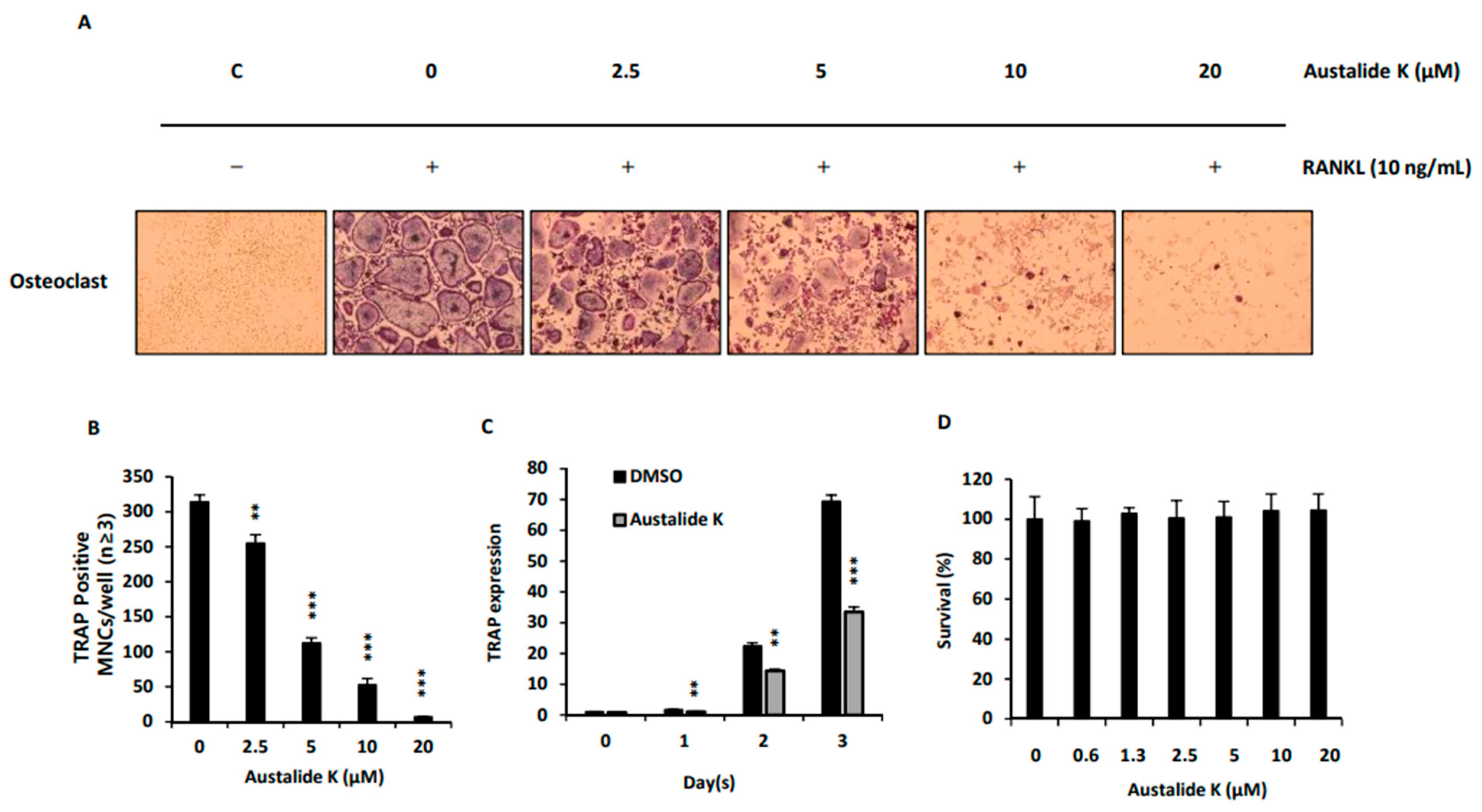
2.2. Effect of Austalide K on RANKL-Induced Osteoclast Differentiation
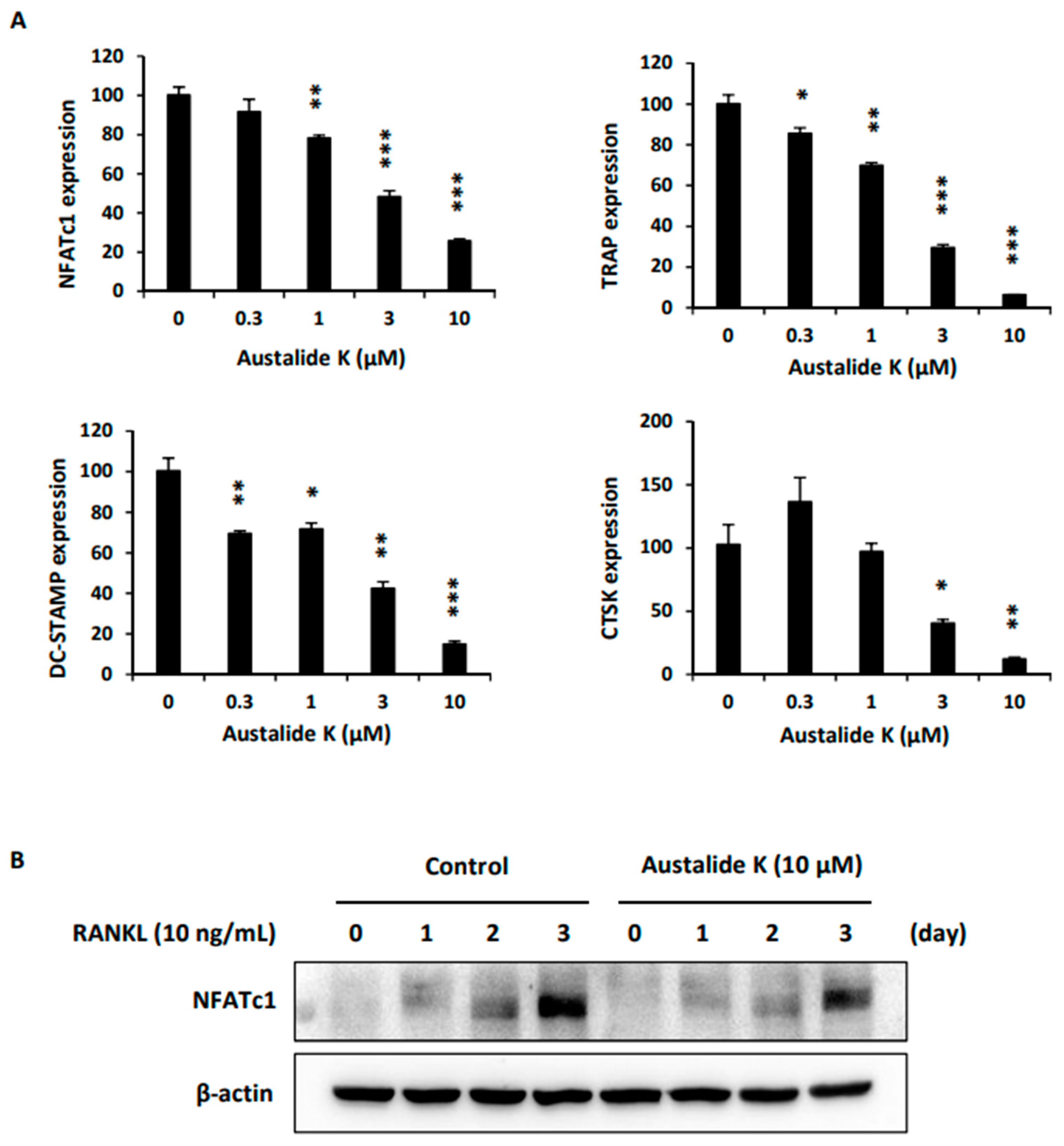
2.3. Effect of Austalide K on Expression of Osteoclastogenesis-Related Genes.
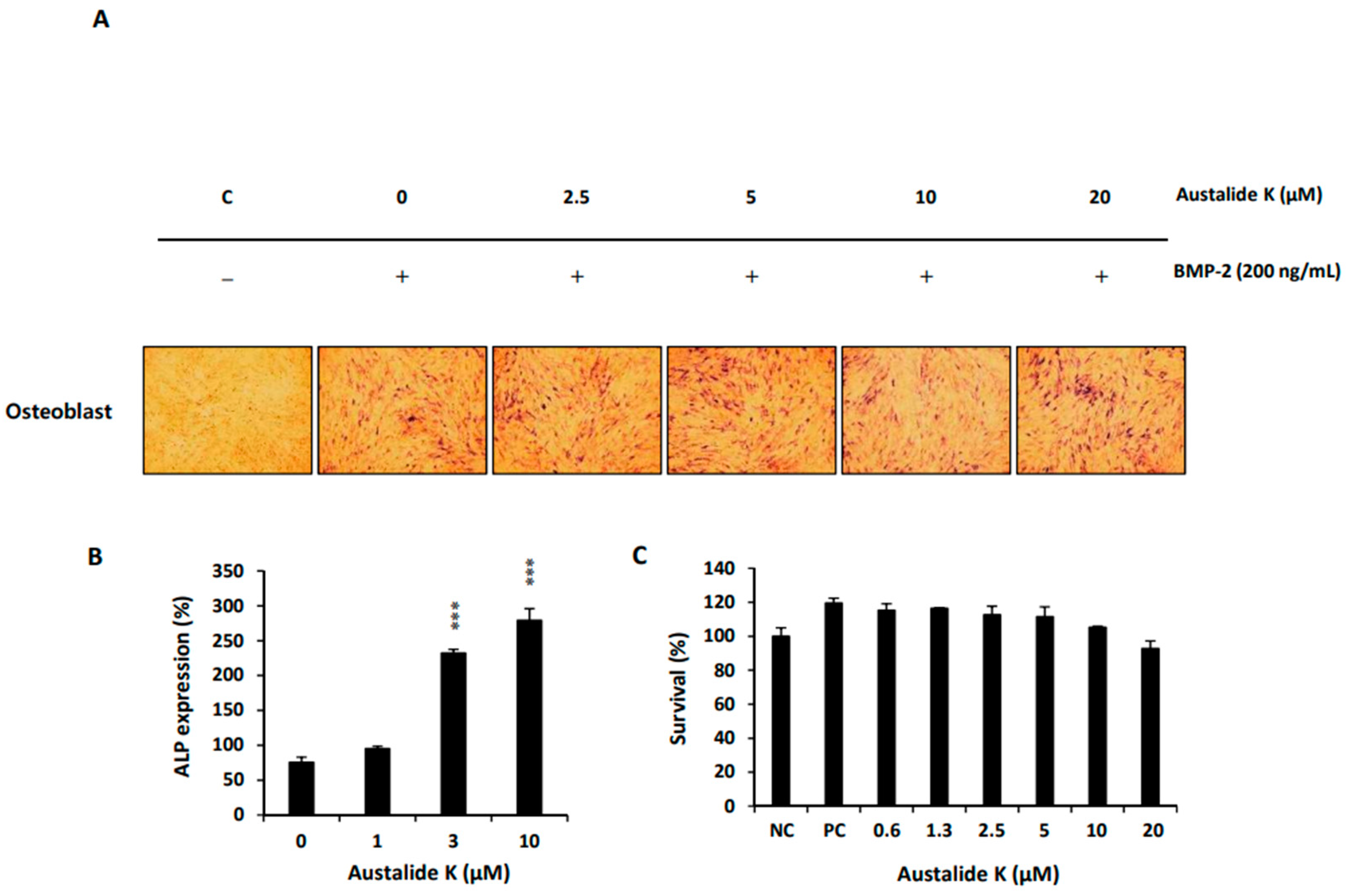
2.4. Austalide K Increased Osteoblast Differentiation
2.5. Austalide K Increased Osteoblast-Differentiation-Related Genes
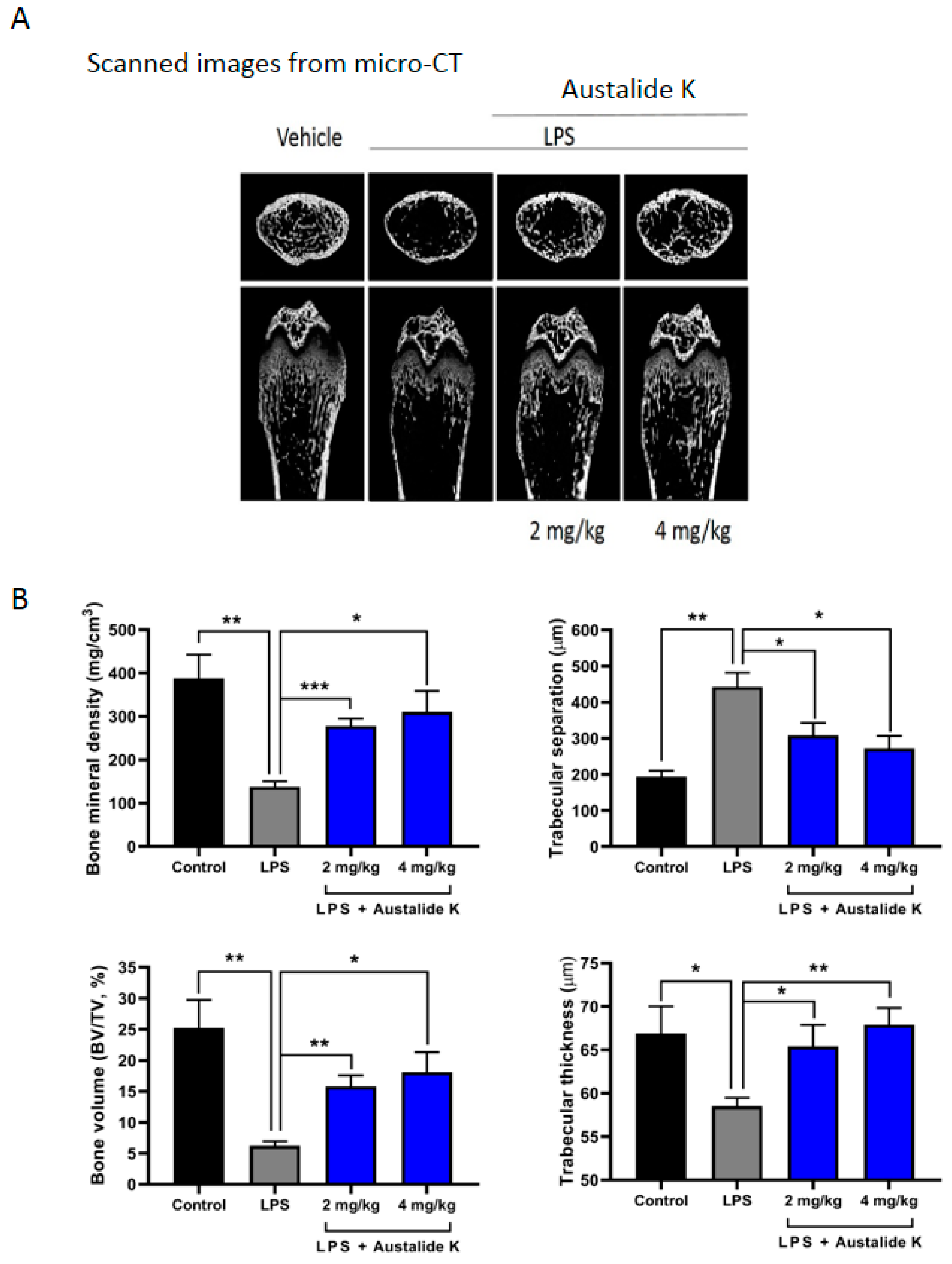
2.6. Austalide K Changed Bone Parameters of LPS-Induced Bone Loss in In Vivo Model
3. Discussion
4. Materials and Methods
4.1. General Experimental Procedures
4.2. Isolation and Cultivation of the Fungal Strain
4.3. Extraction and Isolation of Secondary Metabolites from Seawater PDB Medium
4.4. Osteoclast Cell Culture and Differentiation
4.5. TRAP-Staining Assay
4.6. Osteoclast Cytotoxicity Assay
4.7. Osteoblast Culture and Differentiation
4.8. Alkaline Phosphatase Staining
4.9. Osteoblast Cytotoxicity Assay
4.10. Western Blot and Real-Time PCR Analysis
4.11. In Vivo LPS-Induced Bone Erosion Model
4.12. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- French, D.; Muir, J.; Webber, C. The ovariectomized, mature rat model of postmenopausal osteoporosis: An assessment of the bone sparing effects of curcumin. Phytomedicine 2008, 15, 1069–1078. [Google Scholar] [CrossRef] [PubMed]
- Raggatt, L.J.; Partridge, N.C. Cellular and molecular mechanisms of bone remodeling. J. Biol. Chem. 2010, 285, 25103–25108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edwards, J.R.; Mundy, G.R. Advances in osteoclast biology: Old findings and new insights from mouse models. Nat. Rev. Rheumatol. 2011, 7, 235. [Google Scholar] [CrossRef] [PubMed]
- Kessenich, C.R. The pathophysiology of osteoporotic vertebral fractures. Rehabil. Nurs. 1997, 22, 192–195. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, J.C.; Sai, A. Molecular biology of bone remodeling: Implications for new therapeutic targets for osteoporosis. Maturitas 2010, 65, 301–307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eastell, R.; Rosen, C.J.; Black, D.M.; Cheung, A.M.; Murad, M.H.; Shoback, D. Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society* Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2019, 104, 1595–1622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fleisch, H. Bisphosphonates in osteoporosis. The Aging Spine 2003, 12, 60–64. [Google Scholar]
- Papapetrou, P.D. Bisphosphonate-associated adverse events. Hormones 2009, 8, 96–110. [Google Scholar] [CrossRef] [PubMed]
- Welton, J.L.; Morgan, M.P.; Marti, S.; Stone, M.D.; Moser, B.; Sewell, A.K.; Turton, J.; Eberl, M. Monocytes and γδ T cells control the acute-phase response to intravenous zoledronate: Insights from a phase IV safety trial. J. Bone Miner. Res. 2013, 28, 464–471. [Google Scholar] [CrossRef] [Green Version]
- Jonville-Bera, A.P.; Autret-Leca, E. [Adverse drug reactions of strontium ranelate (Protelos (®) in France]. La Presse Médicale 2011, 40, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Riggs, B.L.; Hodgson, S.F.; O’fallon, W.M.; Chao, E.Y.; Wahner, H.W.; Muhs, J.M.; Cedel, S.L.; Melon, L.J., III. Effect of fluoride treatment on the fracture rate in postmenopausal women with osteoporosis. Engl. J. Med. 1990, 322, 802–809. [Google Scholar] [CrossRef]
- Hodsman, A.B.; Bauer, D.C.; Dempster, D.W.; Dian, L.; Hanley, D.A.; Harris, S.T.; Kendler, D.L.; McClung, M.R.; Miller, P.D.; Olszynski, W.P. Parathyroid hormone and teriparatide for the treatment of osteoporosis: A review of the evidence and suggested guidelines for its use. Endocr. Rev. 2005, 26, 688–703. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.; Kim, K.-J.; Yeon, J.-T.; Kim, S.H.; Won, D.H.; Choi, H.; Nam, S.-J.; Son, Y.-J.; Kang, H. Placotylene A, an inhibitor of the receptor activator of nuclear factor-κB ligand-induced osteoclast differentiation, from a Korean sponge Placospongia sp. Mar. Drugs 2014, 12, 2054–2065. [Google Scholar] [CrossRef] [Green Version]
- Yeon, J.-T.; Kim, H.; Kim, K.-J.; Lee, J.; Won, D.H.; Nam, S.-J.; Kim, S.H.; Kang, H.; Son, Y.-J. Acredinone C and the Effect of Acredinones on Osteoclastogenic and Osteoblastogenic Activity. J. Nat. Prod. 2016, 79, 1730–1736. [Google Scholar] [CrossRef]
- Zhou, Y.; Debbab, A.; Wray, V.; Lin, W.; Schulz, B.; Trepos, R.; Pile, C.; Hellio, C.; Proksch, P.; Aly, A.H. Marine bacterial inhibitors from the sponge-derived fungus Aspergillus sp. Tetrahedron Lett. 2014, 55, 2789–2792. [Google Scholar] [CrossRef] [Green Version]
- Zhuravleva, O.I.; Sobolevskaya, M.P.; Leshchenko, E.V.; Kirichuk, N.N.; Denisenko, V.A.; Dmitrenok, P.S.; Dyshlovoy, S.A.; Zakharenko, A.M.; Kim, N.Y.; Afiyatullov, S.S. Meroterpenoids from the alga-derived fungi Penicillium thomii Maire and Penicillium lividum Westling. J. Nat. Prod. 2014, 77, 1390–1395. [Google Scholar] [CrossRef] [PubMed]
- Yeon, J.T.; Kim, K.J.; Choi, S.W.; Moon, S.H.; Park, Y.S.; Ryu, B.J.; Oh, J.; Kim, M.S.; Erkhembaatar, M.; Son, Y.J. Anti-osteoclastogenic activity of praeruptorin A via inhibition of p38/Akt-c-Fos-NFATc1 signaling and PLCγ-independent Ca2+ oscillation. PLoS ONE 2014, 9, e88974. [Google Scholar] [CrossRef] [PubMed]
- Fuller, K.; Lawrence, K.M.; Ross, J.L.; Grabowska, U.B.; Shiroo, M.; Samuelsson, B.; Chambers, T.J. CTSK inhibitors prevent matrix-derived growth factor degradation by human osteoclasts. Bone 2008, 42, 200–211. [Google Scholar] [CrossRef]
- Yagi, M.; Ninomiya, K.; Fujita, N.; Suzuki, T.; Iwasaki, R.; Morita, K.; Hosogane, N.; Matsuo, K.; Toyama, Y.; Suda, T.J. Induction of DC-STAMP by alternative activation and downstream signaling mechanisms. Bone Miner. Res. 2007, 22, 992–1001. [Google Scholar] [CrossRef]
- Ohara, N.; Hayashi, Y.; Yamada, S.; Kim, S.-K.; Matsunaga, T.; Yanagiguchi, K.; Ikeda, T. Early gene expression analyzed by cDNA microarray and RT-PCR in osteoblasts cultured with water-soluble and low molecular chitooligosaccharide. Biomaterials 2004, 25, 1749–1754. [Google Scholar] [CrossRef]
- Jönsson, S.; Hjorth-Hansen, H.; Olsson, B.; Wadenvik, H.; Sundan, A.; Standal, T. Imatinib inhibits proliferation of human mesenchymal stem cells and promotes early but not late osteoblast differentiation in vitro. J. Bone Miner. Res. Metab. 2012, 30, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Karsenty, G. Role of Cbfa1 in osteoblast differentiation and function. Semin. Cell Dev. Biol. 2000, 11, 343–346. [Google Scholar] [CrossRef]
- Zhang, X.; Yang, M.; Lin, L.; Chen, P.; Ma, K.; Zhou, C.; Ao, Y. Runx2 overexpression enhances osteoblastic differentiation and mineralization in adipose--derived stem cells in vitro and in vivo. Calcif. Tissue Int. 2006, 79, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Takayanagi, H. Osteoimmunology: Shared mechanisms and crosstalk between the immune and bone systems. Nat. Rev. Immunol. 2007, 7, 292–304. [Google Scholar] [CrossRef]
- Li, J.; Zeng, L.; Xie, J.; Yue, Z.; Deng, H.; Ma, X.; Zheng, C.; Wu, X.; Luo, J.; Liu, M. Inhibition of Osteoclastogenesis and Bone Resorption in vitro and in vivo by a prenylflavonoid xanthohumol from hops. Sci. Rep. 2015, 5, 17605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chung, H.J.; Kim, W.K.; Oh, J.; Kim, M.R.; Shin, J.S.; Lee, J.; Ha, I.H.; Lee, S.K. Anti-Osteoporotic Activity of Harpagoside by Upregulation of the BMP2 and Wnt Signaling Pathways in Osteoblasts and Suppression of Differentiation in Osteoclasts. J. Nat. Prod. 2017, 80, 434–442. [Google Scholar] [CrossRef]
- Blunt, J.W.; Copp, B.R.; Keyzers, R.A.; Munro, M.H.; Prinsep, M.R. Marine natural products. Nat. Prod. Rep. 2015, 32, 116–211. [Google Scholar] [CrossRef] [Green Version]
- Hayman, A.R.; Bune, A.J.; Bradley, J.R.; Rashbass, J.; Cox, T.M. Osteoclastic tartrate-resistant acid phosphatase (Acp 5): Its localization to dendritic cells and diverse murine tissues. J. Histochem. Cytochem. 2000, 48, 219–227. [Google Scholar] [CrossRef] [Green Version]
- Shikov, A.N.; Flisyuk, E.V.; Obluchinskaya, E.D.; Pozharitskaya, O.N. Pharmacokinetics of Marine-Derived Drugs. Mar. Drugs 2020, 18, 557. [Google Scholar] [CrossRef]
- Koyama, T. Extracts of marine algae show inhibitory activity against osteoclast differentiation. Adv. Food Nutr. Res. 2011, 64, 443–454. [Google Scholar]
- Carson, M.A.; Nelson, J.; Cancela, M.L.; Laizé, V.; Gavaia, P.J.; Rae, M.; Heesch, S.; Verzin, E.; Gilmore, B.F.; Clarke, S.A. Screening for osteogenic activity in extracts from Irish marine organisms: The potential of Ceramium pallidum. PLoS ONE 2018, 13, e0207303. [Google Scholar] [CrossRef] [PubMed]
- Rozen, S.; Skaletsky, H. Primer3 on the WWW for general users and for biologist programmers. Methods Mol. Biol. 2000, 132, 365–386. [Google Scholar] [PubMed] [Green Version]

| Target Gene | Forward Primer (5′–3′) | Reverse Primer (5′–3′) |
|---|---|---|
| TRAP | GATGACTTTGCCAGTCAGCA | ACATAGCCCACACCGTTCTC |
| NFATc1 | GGGTCAGTGTGACCGAAGAT | GGAAGTCAGAAGTGGGTGGA |
| DC-STAMP | CCAAGGAGTCGTCCATGATT | GGCTGCTTTGATCGTTTCTC |
| CTSK | GGCCAACTCAAGAAGAAAAC | GTGCTTGCTTCCCTTCTGG |
| ALP | GATGGCGTATGCCTCCTGCA | CGGTGGTGGGCCACAAAAGG |
| Runx2 | CCAGAATGATGGTGTTGACG | AGGGTTGCAAGATCATGACT |
| OCN | TATGTGTCCTCCGGGTTCAT | GCCCTCTGCAGGTCATAGAG |
| OPN | GCTAGTCCTAGACCCTAAGA | TCCTGCTTAATCCTCACTAA |
| GAPDH | AACTTTGGCATTGTGGAAGG | ACACATTGGGGGTAGGAACA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, K.-J.; Lee, J.; Wang, W.; Lee, Y.; Oh, E.; Park, K.-H.; Park, C.; Woo, G.-E.; Son, Y.-J.; Kang, H. Austalide K from the Fungus Penicillium rudallense Prevents LPS-Induced Bone Loss in Mice by Inhibiting Osteoclast Differentiation and Promoting Osteoblast Differentiation. Int. J. Mol. Sci. 2021, 22, 5493. https://doi.org/10.3390/ijms22115493
Kim K-J, Lee J, Wang W, Lee Y, Oh E, Park K-H, Park C, Woo G-E, Son Y-J, Kang H. Austalide K from the Fungus Penicillium rudallense Prevents LPS-Induced Bone Loss in Mice by Inhibiting Osteoclast Differentiation and Promoting Osteoblast Differentiation. International Journal of Molecular Sciences. 2021; 22(11):5493. https://doi.org/10.3390/ijms22115493
Chicago/Turabian StyleKim, Kwang-Jin, Jusung Lee, Weihong Wang, Yongjin Lee, Eunseok Oh, Kyu-Hyung Park, Chanyoon Park, Gee-Eun Woo, Young-Jin Son, and Heonjoong Kang. 2021. "Austalide K from the Fungus Penicillium rudallense Prevents LPS-Induced Bone Loss in Mice by Inhibiting Osteoclast Differentiation and Promoting Osteoblast Differentiation" International Journal of Molecular Sciences 22, no. 11: 5493. https://doi.org/10.3390/ijms22115493






