The Evolving Role of Fetuin-A in Nonalcoholic Fatty Liver Disease: An Overview from Liver to the Heart
Abstract
1. Introduction
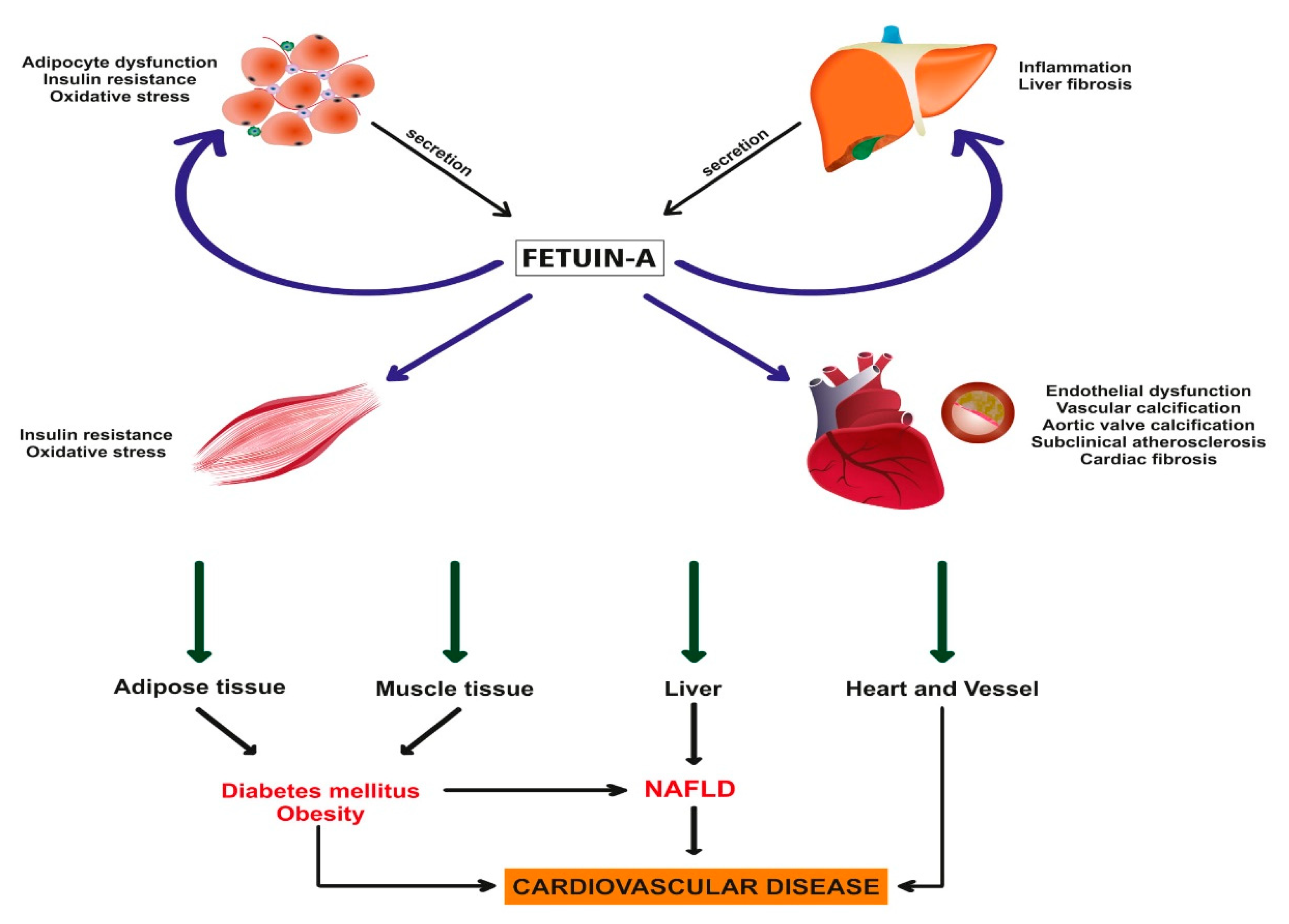
2. The Role of Fetuin-A in NAFLD; from Hepatic Steatosis to Inflammation and Fibrosis
2.1. Studies Investigating Fetuin-A in Subjects with Radiologically Diagnosed NAFLD
2.2. Studies Investigating Fetuin-A in Histologically Diagnosed Subjects with NAFLD
3. The Relationship of Fetuin-A with NAFLD Associated CVD Risk
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, J.; Zou, B.; Yeo, Y.H.; Feng, Y.; Xie, X.; Lee, D.H.; Fujii, H.; Wu, Y.; Kam, L.Y.; Ji, F.; et al. Prevalence, incidence, and outcome of nonalcoholic fatty liver disease in Asia, 1999–2019: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2019, 4, 389–398. [Google Scholar] [CrossRef]
- Browning, J.D.; Szczepaniak, L.S.; Dobbins, R.; Nuremberg, P.; Horton, J.D.; Cohen, J.C.; Grundy, S.M.; Hobbs, H.H. Prevalence of hepatic steatosis in an urban population in the United States: Impact of ethnicity. Hepatology 2004, 40, 1387–1395. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016, 64, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Silverman, J.F.; O’Brien, K.F.; Long, S.; Leggett, N.; Khazanie, P.G.; Pories, W.J.; Norris, H.T.; Caro, J.F. Liver pathology in morbidly obese patients with and without diabetes. Am. J. Gastroenterol. 1990, 85, 1349–1355. [Google Scholar] [PubMed]
- Subichin, M.; Clanton, J.; Makuszewski, M.; Bohon, A.; Zografakis, J.G.; Dan, A. Liver disease in the morbidly obese: A review of 1000 consecutive patients undergoing weight loss surgery. Surg. Obes. Relat. Dis. 2015, 11, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, A.; Nitta, H.; Otsuka, K.; Umemura, A.; Baba, S.; Obuchi, T.; Wakabayashi, G. Bariatric surgery and nonalcoholic fatty liver disease: Current and potential future treatments. Front. Endocrinol. 2014, 5, 164. [Google Scholar] [CrossRef] [PubMed]
- Toplak, H.; Stauber, R.; Sourij, H. EASL-EASD-EASO clinical practice guidelines for the management of nonalcoholic fatty liver disease: Guidelines, clinical reality and health economic aspects. Diabetologia 2016, 59, 1148–1149. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018, 67, 328–357. [Google Scholar] [CrossRef]
- Singh, S.; Allen, A.M.; Wang, Z.; Prokop, L.J.; Murad, M.H.; Loomba, R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: A systematic review and meta-analysis of paired-biopsy studies. Clin. Gastroenterol. Hepatol. 2015, 13, 643–654.e9. [Google Scholar] [CrossRef]
- Lonardo, A.; Leoni, S.; Alswat, K.A.; Fouad, Y. History of nonalcoholic fatty liver disease. Int. J. Mol. Sci. 2020, 21, 5888. [Google Scholar] [CrossRef]
- Yki-Järvinen, H. Nonalcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014, 2, 901–910. [Google Scholar] [CrossRef]
- Ercin, C.N.; Dogru, T.; Genc, H.; Celebi, G.; Aslan, F.; Gurel, H.; Kara, M.; Sertoglu, E.; Tapan, S.; Bagci, S.; et al. Insulin resistance but not visceral adiposity index is associated with liver fibrosis in nondiabetic subjects with nonalcoholic fatty liver disease. Metab. Syndr. Relat. Disord. 2015, 13, 319–325. [Google Scholar] [CrossRef]
- Byrne, C.D.; Targher, G. NAFLD: A multisystem disease. J. Hepatol. 2015, 62, S47–S64. [Google Scholar] [CrossRef]
- Meex, R.C.R.; Watt, M.J. Hepatokines: Linking nonalcoholic fatty liver disease and insulin resistance. Nat. Rev. Endocrinol. 2017, 13, 509–520. [Google Scholar] [CrossRef]
- Jirak, P.; Stechemesser, L.; Moré, E.; Franzen, M.; Topf, A.; Mirna, M.; Paar, V.; Pistulli, R.; Kretzschmar, D.; Wernly, B.; et al. Clinical implications of fetuin-A. Int. Rev. Cytol. 2019, 89, 79–130. [Google Scholar] [CrossRef]
- Bril, F.; Cusi, K. Nonalcoholic fatty liver disease. Endocrinol. Metab. Clin. N. Am. 2016, 45, 765–781. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, M.; Adams, L.A.; Canbay, A.; Syn, W.K. Extrahepatic complications of nonalcoholic fatty liver disease. Hepatology 2014, 59, 1174–1197. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Zeng, L.; Liang, B.; Shu, X.; Xie, D. High prevalence of coronary heart disease in type 2 diabetic patients with nonalcoholic fatty liver disease. Arch. Med. Res. 2009, 40, 571–575. [Google Scholar] [CrossRef]
- Targher, G.; Bertolini, L.; Padovani, R.; Poli, F.; Scala, L.; Tessari, R.; Zenari, L.; Falezza, G. Increased prevalence of cardiovascular disease in type 2 diabetic patients with nonalcoholic fatty liver disease. Diabet. Med. 2006, 23, 403–409. [Google Scholar] [CrossRef]
- Stepanova, M.; Rafiq, N.; Makhlouf, H.; Agrawal, R.; Kaur, I.; Younoszai, Z.; McCullough, A.; Goodman, Z.; Younossi, Z.M. Predictors of all-cause mortality and liver-related mortality in patients with nonalcoholic fatty liver disease (NAFLD). Dig. Dis. Sci. 2013, 58, 3017–3023. [Google Scholar] [CrossRef]
- Söderberg, C.; Stål, P.; Askling, J.; Glaumann, H.; Lindberg, G.; Marmur, J.; Hultcrantz, R. Decreased survival of subjects with elevated liver function tests during a 28-year follow-up. Hepatology 2010, 51, 595–602. [Google Scholar] [CrossRef]
- Targher, G.; Bertolini, L.; Rodella, S.; Tessari, R.; Zenari, L.; Lippi, G.; Arcaro, G. Nonalcoholic fatty liver disease is independently associated with an increased incidence of cardiovascular events in type 2 diabetic patients. Diabetes Care 2007, 30, 2119–2121. [Google Scholar] [CrossRef]
- Targher, G.; Bertolini, L.; Poli, F.; Rodella, S.; Scala, L.; Tessari, R.; Zenari, L.; Falezza, G. Nonalcoholic fatty liver disease and risk of future cardiovascular events among type 2 diabetic patients. Diabetes 2005, 54, 3541–3546. [Google Scholar] [CrossRef]
- Bril, F.; Sninsky, J.J.; Baca, A.M.; Superko, H.R.; Sanchez, P.P.; Biernacki, D.; Maximos, M.; Lomonaco, R.; Orsak, B.; Suman, A.; et al. Hepatic steatosis and insulin resistance, but not steatohepatitis, promote atherogenic dyslipidemia in NAFLD. J. Clin. Endocrinol. Metab. 2016, 101, 644–652. [Google Scholar] [CrossRef]
- Lomonaco, R.; Bril, F.; Portillo-Sanchez, P.; Ortiz-Lopez, C.; Orsak, B.; Biernacki, D.; Lo, M.; Suman, A.; Weber, M.H.; Cusi, K. Metabolic impact of nonalcoholic steatohepatitis in obese patients with type 2 diabetes. Diabetes Care 2016, 39, 632–638. [Google Scholar] [CrossRef]
- Bril, F.; Lomonaco, R.; Orsak, B.; Ortiz-Lopez, C.; Webb, A.; Tio, F.; Hecht, J.; Cusi, K. Relationship between disease severity, hyperinsulinemia, and impaired insulin clearance in patients with nonalcoholic steatohepatitis. Hepatology 2014, 59, 2178–2187. [Google Scholar] [CrossRef]
- Nangami, G.N.; Watson, K.; Parker-Johnson, K.; Okereke, K.O.; Sakwe, A.; Thompson, P.; Frimpong, N.; Ochieng, J. Fetuin-A (α2HS-glycoprotein) is a serum chemo-attractant that also promotes invasion of tumor cells through Matrigel. Biochem. Biophys. Res. Commun. 2013, 438, 660–665. [Google Scholar] [CrossRef]
- Auberger, P.; Falquerho, L.; Contreres, J.O.; Pages, G.; Le Cam, G.; Rossi, B.; Le Cam, A. Characterization of a natural inhibitor of the insulin receptor tyrosine kinase: cDNA cloning, purification, and anti-mitogenic activity. Cell 1989, 58, 631–640. [Google Scholar] [CrossRef]
- Kalabay, L.; Mathur, S.; Bobin, S.; Arnaud, P. Electrophoretic and isoelectric focusing analysis of human recombinant alpha2-HS glycoprotein produced in insect cells: Analysis of the post-translational events. Electrophoresis 1996, 17, 529–532. [Google Scholar] [CrossRef]
- Matsui, I.; Hamano, T.; Mikami, S.; Fujii, N.; Takabatake, Y.; Nagasawa, Y.; Kawada, N.; Ito, T.; Rakugi, H.; Imai, E.; et al. Fully phosphorylated fetuin-A forms a mineral complex in the serum of rats with adenine-induced renal failure. Kidney Int. 2009, 75, 915–928. [Google Scholar] [CrossRef]
- Mori, K.; Emoto, M.; Inaba, M. Fetuin-A: A multifunctional protein. Recent Pat. Endocr. Metab. Immune Drug Discov. 2011, 5, 124–146. [Google Scholar] [CrossRef]
- Trepanowski, J.F.; Mey, J.; Varady, K.A. Fetuin-A: A novel link between obesity and related complications. Int. J. Obes. 2015, 39, 734–741. [Google Scholar] [CrossRef]
- Ou, H.-Y.; Yang, Y.; Wu, H.-T.; Wu, J.-S.; Lu, F.-H.; Chang, C. Serum fetuin-A concentrations are elevated in subjects with impaired glucose tolerance and newly diagnosed type 2 diabetes. Clin. Endocrinol. 2011, 75, 450–455. [Google Scholar] [CrossRef]
- Ix, J.H.; Shlipak, M.G.; Brandenburg, V.M.; Ali, S.; Ketteler, M.; Whooley, M.A. Association between human fetuin-A and the metabolic syndrome. Circulation 2006, 113, 1760–1767. [Google Scholar] [CrossRef]
- Aroner, S.A.; St-Jules, D.E.; Mukamal, K.J.; Katz, R.; Shlipak, M.G.; Criqui, M.H.; Kestenbaum, B.; Siscovick, D.S.; De Boer, I.H.; Jenny, N.S.; et al. Fetuin-A, glycemic status, and risk of cardiovascular disease: The multi-ethnic study of atherosclerosis. Atherosclerosis 2016, 248, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Stefan, N.; Hennige, A.M.; Staiger, H.; Machann, J.; Schick, F.; Kröber, S.M.; Machicao, F.; Fritsche, A.; Häring, H.U. Alpha2-Heremans-Schmid glycoprotein/ fetuin-A is associated with insulin resistance and fat accumulation in the liver in humans. Diabetes Care 2006, 29, 853–857. [Google Scholar] [CrossRef]
- Stefan, N.; Häring, H.-U. The role of hepatokines in metabolism. Nat. Rev. Endocrinol. 2013, 9, 144–152. [Google Scholar] [CrossRef]
- Lebensztejn, D.M.; Białokoz-Kalinowska, I.; Kłusek-Oksiuta, M.; Tarasów, E.; Wojtkowska, M.; Kaczmarski, M. Serum fetuin A concentration is elevated in children with nonalcoholic fatty liver disease. Adv. Med. Sci. 2014, 59, 81–84. [Google Scholar] [CrossRef]
- Reinehr, T.; Roth, C.L. Fetuin-A and its relation to metabolic syndrome and fatty liver disease in obese children before and after weight loss. J. Clin. Endocrinol. Metab. 2008, 93, 4479–4485. [Google Scholar] [CrossRef]
- Ou, H.-Y.; Yang, Y.-C.; Wu, H.-T.; Wu, J.-S.; Lu, F.-H.; Chang, C.-J. Increased fetuin-A concentrations in impaired glucose tolerance with or without nonalcoholic fatty liver disease, but not impaired fasting glucose. J. Clin. Endocrinol. Metab. 2012, 97, 4717–4723. [Google Scholar] [CrossRef]
- Huang, Y.; Huang, X.; Ding, L.; Wang, P.; Peng, K.; Chen, Y.; Dai, M.; Zhang, D.; Xu, M.; Bi, Y.; et al. Serum fetuin-A associated with fatty liver index, early indicator of nonalcoholic fatty liver disease. Medicine 2015, 94, e1517. [Google Scholar] [CrossRef]
- Thompson, D.S.; Tennant, I.A.; Soares, D.P.; Osmond, C.; Byrne, C.D.; Forrester, T.E.; Boyne, M. Nonalcoholic fatty liver disease in nonobese subjects of African origin has atypical metabolic characteristics. J. Endocr. Soc. 2019, 3, 2051–2063. [Google Scholar] [CrossRef]
- Cui, Z.; Xuan, R.; Yang, Y. Serum fetuin A level is associated with nonalcoholic fatty liver disease in Chinese population. Oncotarget 2017, 8, 107149–107156. [Google Scholar] [CrossRef][Green Version]
- Sato, M.; Kamada, Y.; Takeda, Y.; Kida, S.; Ohara, Y.; Fujii, H.; Akita, M.; Mizutani, K.; Yoshida, Y.; Yamada, M.; et al. Fetuin-A negatively correlates with liver and vascular fibrosis in nonalcoholic fatty liver disease subjects. Liver Int. 2014, 35, 925–935. [Google Scholar] [CrossRef]
- Yilmaz, Y.; Yonal, O.; Kurt, R.; Ari, F.; Oral, A.Y.; Celikel, C.A.; Korkmaz, S.; Ulukaya, E.; Ozdogan, O.; Imeryuz, N.; et al. Serum fetuin-A/α2HS-glycoprotein levels in patients with nonalcoholic fatty liver disease: Relation with liver fibrosis. Ann. Clin. Biochem. Int. J. Lab. Med. 2010, 47, 549–553. [Google Scholar] [CrossRef]
- Haukeland, J.W.; Dahl, T.B.; Yndestad, A.; Gladhaug, I.P.; Løberg, E.M.; Haaland, T.; Konopski, Z.; Wium, C.; Aasheim, E.T.; Johansen, O.E.; et al. Fetuin-A in nonalcoholic fatty liver disease: In vivo and in vitro studies. Eur. J. Endocrinol. 2012, 166, 503–510. [Google Scholar] [CrossRef]
- Ou, H.-Y.; Wu, H.-T.; Hung, H.-C.; Yang, Y.-C.; Wu, J.-S.; Chang, C.-J. Endoplasmic reticulum stress induces the expression of fetuin-A to develop insulin resistance. Endocrinology 2012, 153, 2974–2984. [Google Scholar] [CrossRef]
- Çelebi, G.; Genc, H.; Gurel, H.; Sertoglu, E.; Kara, M.; Tapan, S.; Acikel, C.; Karslioglu, Y.; Ercin, C.N.; Dogru, T. The relationship of circulating fetuin-A with liver histology and biomarkers of systemic inflammation in nondiabetic subjects with nonalcoholic fatty liver disease. Saudi J. Gastroenterol. 2015, 21, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Kahraman, A.; Sowa, J.-P.; Schlattjan, M.; Sydor, S.; Pronadl, M.; Wree, A.; Beilfuss, A.; Kilicarslan, A.; Altinbaş, A.; Bechmann, L.P.; et al. Fetuin-A mRNA expression is elevated in NASH compared with NAFL patients. Clin. Sci. 2013, 125, 391–400. [Google Scholar] [CrossRef]
- Rametta, R.; Ruscica, M.; Dongiovanni, P.; Macchi, C.; Fracanzani, A.L.; Steffani, L.; Fargion, S.; Magni, P.; Valenti, L. Hepatic steatosis and PNPLA3 I148M variant are associated with serum fetuin-A independently of insulin resistance. Eur. J. Clin. Investig. 2014, 44, 627–633. [Google Scholar] [CrossRef]
- Von Loeffelholz, C.; Horn, P.; Birkenfeld, A.; Claus, R.; Metzing, B.; Döcke, S.; Jahreis, G.; Heller, R.; Hoppe, S.; Stockmann, M.; et al. Fetuin A is a predictor of liver fat in preoperative patients with nonalcoholic fatty liver disease. J. Investig. Surg. 2016, 29, 266–274. [Google Scholar] [CrossRef]
- Pampanini, V.; Inzaghi, E.; Germani, D.; Alterio, A.; Puglianiello, A.; Alisi, A.; Nobili, V.; Cianfarani, S. Serum fetuin-A levels in obese children with biopsy proven nonalcoholic fatty liver disease. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Peter, A.; Kovarova, M.; Staiger, H.; Machann, J.; Schick, F.; Königsrainer, A.; Königsrainer, I.; Schleicher, E.; Fritsche, A.; Häring, H.-U.; et al. The hepatokines fetuin-A and fetuin-B are upregulated in the state of hepatic steatosis and may differently impact on glucose homeostasis in humans. Am. J. Physiol. Metab. 2018, 314, E266–E273. [Google Scholar] [CrossRef]
- Kaushik, S.V.; Plaisance, E.P.; Kim, T.; Huang, E.Y.; Mahurin, A.J.; Grandjean, P.W.; Mathews, S.T. Extended-release niacin decreases serum fetuin-A concentrations in individuals with metabolic syndrome. Diabetes/Metab. Res. Rev. 2009, 25, 427–434. [Google Scholar] [CrossRef]
- Stenvinkel, P.; Wang, K.; Qureshi, A.R.; Axelsson, J.; Pecoits-Filho, R.; Gao, P.; Barany, P.; Lindholm, B.; Jogestrand, T.; Heimberger, O.; et al. Low fetuin-A levels are associated with cardiovascular death: Impact of variations in the gene encoding fetuin. Kidney Int. 2005, 67, 2383–2392. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, C.; Heiss, A.; Schwarz, A.; Westenfeld, R.; Ketteler, M.; Floege, J.; Müller-Esterl, W.; Schinke, T.; Jahnen-Dechent, W. The serum protein α2–Heremans-Schmid glycoprotein/fetuin-A is a systemically acting inhibitor of ectopic calcification. J. Clin. Investig. 2003, 112, 357–366. [Google Scholar] [CrossRef]
- Westenfeld, R.; Schäfer, C.; Krüger, T.; Haarmann, C.; Schurgers, L.J.; Reutelingsperger, C.; Ivanovski, O.; Drueke, T.B.; Massy, Z.A.; Ketteler, M.; et al. Fetuin-A protects against atherosclerotic calcification in CKD. J. Am. Soc. Nephrol. 2009, 20, 1264–1274. [Google Scholar] [CrossRef] [PubMed]
- Ford, M.L.; Tomlinson, L.A.; Smith, E.R.; Rajkumar, C.; Holt, S.G. Fetuin-A is an independent determinant of change of aortic stiffness over 1 year in non-diabetic patients with CKD stages 3 and 4. Nephrol. Dial. Transplant. 2010, 25, 1853–1858. [Google Scholar] [CrossRef]
- Ketteler, M.; Bongartz, P.; Westenfeld, R.; Wildberger, J.E.; Mahnken, A.H.; Böhm, R.; Metzger, T.; Wanner, C.; Jahnen-Dechent, W.; Floege, J. Association of low fetuin-A (AHSG) concentrations in serum with cardiovascular mortality in patients on dialysis: A cross-sectional study. Lancet 2003, 361, 827–833. [Google Scholar] [CrossRef]
- Adams, L.A.; Waters, O.R.; Knuiman, M.W.; Elliott, R.R.; Olynyk, J.K. NAFLD as a risk factor for the development of diabetes and the metabolic syndrome: An eleven-year follow-up study. Am. J. Gastroenterol. 2009, 104, 861–867. [Google Scholar] [CrossRef]
- Shulman, G.I. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease. N. Engl. J. Med. 2014, 371, 1131–1141. [Google Scholar] [CrossRef]
- Jensen, M.K.; Bartz, T.M.; Mukamal, K.J.; Djoussé, L.; Kizer, J.R.; Tracy, R.P.; Zieman, S.J.; Rimm, E.B.; Siscovick, D.S.; Shlipak, M.; et al. Fetuin-A, type 2 diabetes, and risk of cardiovascular disease in older adults: The cardiovascular health study. Diabetes Care 2012, 36, 1222–1228. [Google Scholar] [CrossRef]
- Laughlin, G.A.; Cummins, K.M.; Wassel, C.L.; Daniels, L.B.; Ix, J.H. The Association of fetuin-A with cardiovascular disease mortality in older community-dwelling adults: The rancho bernardo study. J. Am. Coll. Cardiol. 2012, 59, 1688–1696. [Google Scholar] [CrossRef]
- Sun, Q.; Jiménez, M.C.; Townsend, M.K.; Rimm, E.B.; Manson, J.E.; Albert, C.; Rexrode, K.M. Plasma levels of fetuin-A and risk of coronary heart disease in US women: The nurses’ health study. J. Am. Heart Assoc. 2014, 3, e000939. [Google Scholar] [CrossRef]
- Caglar, K.; Yilmaz, M.I.; Saglam, M.; Cakir, E.; Kilic, S.; Sonmez, A.; Eyileten, T.; Yenicesu, M.; Oguz, Y.; Tasar, M.; et al. Serum fetuin-A concentration and endothelial dysfunction in chronic kidney disease. Nephron 2008, 108, c233–c240. [Google Scholar] [CrossRef] [PubMed]
- Hruska, K.A.; Mathew, S.; Lund, R.J.; Memon, I.; Saab, G. The pathogenesis of vascular calcification in the chronic kidney disease mineral bone disorder: The links between bone and the vasculature. Semin. Nephrol. 2009, 29, 156–165. [Google Scholar] [CrossRef][Green Version]
- Weikert, C.; Stefan, N.; Schulze, M.B.; Pischon, T.; Berger, K.; Joost, H.-G.; Häring, H.-U.; Boeing, H.; Fritsche, A. Plasma fetuin-A levels and the risk of myocardial infarction and ischemic stroke. Circulation 2008, 118, 2555–2562. [Google Scholar] [CrossRef]
- Vörös, K.; Gráf, L., Jr.; Prohászka, Z.; Gráf, L.; Szenthe, P.; Kaszás, E.; Böröcz, Z.; Cseh, K.; Kalabay, L. Serum fetuin-A in metabolic and inflammatory pathways in patients with myocardial infarction. Eur. J. Clin. Investig. 2011, 41, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Brix, J.M.; Stingl, H.; Höllerl, F.; Schernthaner, G.H.; Kopp, H.-P.; Schernthaner, G. Elevated fetuin-A concentrations in morbid obesity decrease after dramatic weight loss. J. Clin. Endocrinol. Metab. 2010, 95, 4877–4881. [Google Scholar] [CrossRef]
- Mori, K.; Emoto, M.; Araki, T.; Yokoyama, H.; Teramura, M.; Lee, E.; Motoyama, K.; Koyama, H.; Shoji, T.; Inaba, M.; et al. Association of serum fetuin-A with carotid arterial stiffness. Clin. Endocrinol. 2006, 66, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Haglund, Å.C.; Ek, B.; Ek, P. Phosphorylation of human plasma α2-Heremans‒Schmid glycoprotein (human fetuin) in vivo. Biochem. J. 2001, 357, 437–445. [Google Scholar] [CrossRef]
- Dogru, T.; Genc, H.; Tapan, S.; Aslan, F.; Ercin, C.N.; Ors, F.; Kara, M.; Sertoglu, E.; Karslioglu, Y.; Bagci, S.; et al. Plasma fetuin-A is associated with endothelial dysfunction and subclinical atherosclerosis in subjects with nonalcoholic fatty liver disease. Clin. Endocrinol. 2013, 78, 712–717. [Google Scholar] [CrossRef]
- Ballestri, S.; Meschiari, E.; Baldelli, E.; Musumeci, F.E.; Romagnoli, D.; Trenti, T.; Zennaro, R.G.; Lonardo, A.; Loria, P. Relationship of serum fetuin-A levels with coronary atherosclerotic burden and NAFLD in patients undergoing elective coronary angiography. Metab. Syndr. Relat. Disord. 2013, 11, 289–295. [Google Scholar] [CrossRef]
- Nascimbeni, F.; Romagnoli, D.; Ballestri, S.; Baldelli, E.; Lugari, S.; Sirotti, V.; Giampaoli, V.; Lonardo, A. Do nonalcoholic fatty liver disease and fetuin-A play different roles in symptomatic coronary artery disease and peripheral arterial disease? Diseases 2018, 6, 17. [Google Scholar] [CrossRef]
- Zhao, Z.-W.; Lin, C.-G.; Wu, L.-Z.; Luo, Y.-K.; Fan, L.; Dong, X.-F.; Zheng, H. Serum fetuin-A levels are associated with the presence and severity of coronary artery disease in patients with type 2 diabetes. Biomarkers 2013, 18, 160–164. [Google Scholar] [CrossRef]
- Herrmann, M.; Babler, A.; Moshkova, I.; Gremse, F.; Kiessling, F.; Kusebauch, U.; Nelea, V.; Kramann, R.; Moritz, R.L.; McKee, M.D.; et al. Lumenal calcification and microvasculopathy in fetuin-A-deficient mice lead to multiple organ morbidity. PLoS ONE 2020, 15, e0228503. [Google Scholar] [CrossRef]
| Author (Reference) | Study Population | Diagnosis of NAFLD | Fetuin-A Levels in NAFLD (Compared to Controls) | Association of Fetuin-A with NAFLD |
|---|---|---|---|---|
| Lebensztejn et al. [38] | 45 obese children with NAFLD and 30 controls | US | Higher | None |
| Reinehr et al. [39] | 36 obese children with NAFLD and 14 controls | US | Higher | None |
| Ou HY et al. [40] | 255 subjects with NAFLD and 255 controls | US | Higher | None |
| Huang et al. [41] | 5219 middle-aged and elderly subjects | US | NE | Positive |
| Cui et al. [43] | 79 subjects with NAFLD and 79 controls | US | Lower | Positive |
| Sato et al. [44] | 295 subjects with NAFLD | US | NE | Negative |
| Thompson et al. [42] | 78 subjects with NAFLD | CT | NE | None |
| Yilmaz et al. [45] | 99 subjects with NAFLD and 75 controls | Liver bx | Higher | Positive |
| Haukeland et al. [46] | 111 subjects with NAFLD and 131 controls | Liver bx | Higher | Positive |
| Ou et al. [47] | 90 subjects with NAFLD and 90 controls | Liver bx | Higher | NE |
| Celebi et al. [48] | 105 subjects with NAFLD | Liver bx | NE | None |
| Kahraman et al. [49] | 108 morbidly obese subjects with NAFLD and 10 controls | Liver bx | NS | Negative |
| Rametta et al. [50] | 137 subjects with NAFLD and 260 controls | Liver bx | Higher | Positive |
| Von Loeffelholz et al. [51] | 58 subjects with NAFLD | Liver bx | NE | Positive |
| Pampanini et al. [52] | 160 subjects with NAFLD and 23 controls | US and Liver bx | Higher | None |
| Author (Reference) | Study Population | Study Design | CVD Risk Assessment | Association of Fetuin-A with CVD Risk |
|---|---|---|---|---|
| Jensen et al. [62] | 3810 older subjects | Prospective | CVD event or CVD death | Negative |
| Laughlin et al. [63] | 1688 women | Prospective | CVD event or CVD death | Negative |
| Sun et al. [64] | 466 patients with IS | Prospective | IS | None |
| Caglar et al. [65] | 198 nondiabetic patients with CKD | Retrospective | FMD and cIMT | Positive |
| Zhao et al. [75] | 241 patients with T2D | Retrospective | Coronary angiography | Positive |
| Weikert et al. [67] | 227 patients with MI and 168 patients with IS | Prospective | MI or IS | Positive |
| Vörös et al. [68] | 171 patients with CVD and 81 controls | Cross-sectional | Biomarkers of ED | Positive |
| Mori et al. [70] | 141 healthy subjects | Cross-sectional | Carotid arterial stiffness | Positive |
| Sato et al. [44] | 295 subjects with NAFLD | Cross-sectional | cIMT | Negative |
| Dogru et al. [72] | 115 subjects with NAFLD | Cross-sectional | Biomarkers of ED and cIMT | Positive |
| Ballestri et al. [73] | 70 subjects with and without CVD | Cross-sectional | Coronary angiography | Negative |
| Nascimbeni et al. [74] | 45 patients with CVD and 104 patients with PAD | Cross-sectional | CAD PAD | Positive |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dogru, T.; Kirik, A.; Gurel, H.; Rizvi, A.A.; Rizzo, M.; Sonmez, A. The Evolving Role of Fetuin-A in Nonalcoholic Fatty Liver Disease: An Overview from Liver to the Heart. Int. J. Mol. Sci. 2021, 22, 6627. https://doi.org/10.3390/ijms22126627
Dogru T, Kirik A, Gurel H, Rizvi AA, Rizzo M, Sonmez A. The Evolving Role of Fetuin-A in Nonalcoholic Fatty Liver Disease: An Overview from Liver to the Heart. International Journal of Molecular Sciences. 2021; 22(12):6627. https://doi.org/10.3390/ijms22126627
Chicago/Turabian StyleDogru, Teoman, Ali Kirik, Hasan Gurel, Ali A. Rizvi, Manfredi Rizzo, and Alper Sonmez. 2021. "The Evolving Role of Fetuin-A in Nonalcoholic Fatty Liver Disease: An Overview from Liver to the Heart" International Journal of Molecular Sciences 22, no. 12: 6627. https://doi.org/10.3390/ijms22126627
APA StyleDogru, T., Kirik, A., Gurel, H., Rizvi, A. A., Rizzo, M., & Sonmez, A. (2021). The Evolving Role of Fetuin-A in Nonalcoholic Fatty Liver Disease: An Overview from Liver to the Heart. International Journal of Molecular Sciences, 22(12), 6627. https://doi.org/10.3390/ijms22126627







