Telomere Distribution in Human Sperm Heads and Its Relation to Sperm Nuclear Morphology: A New Marker for Male Factor Infertility?
Abstract
:1. Introduction
2. Results
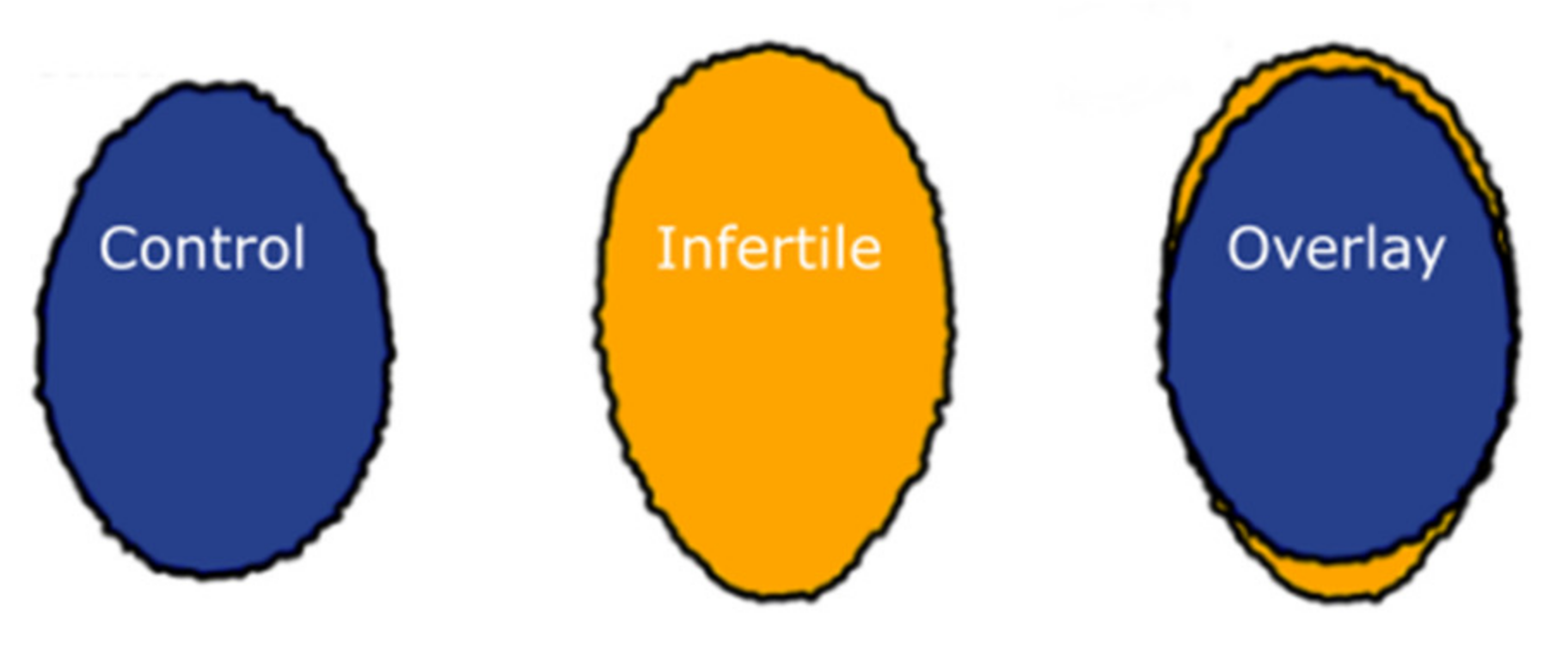
2.1. Nuclei from Infertile Men Have Altered Shape and Size
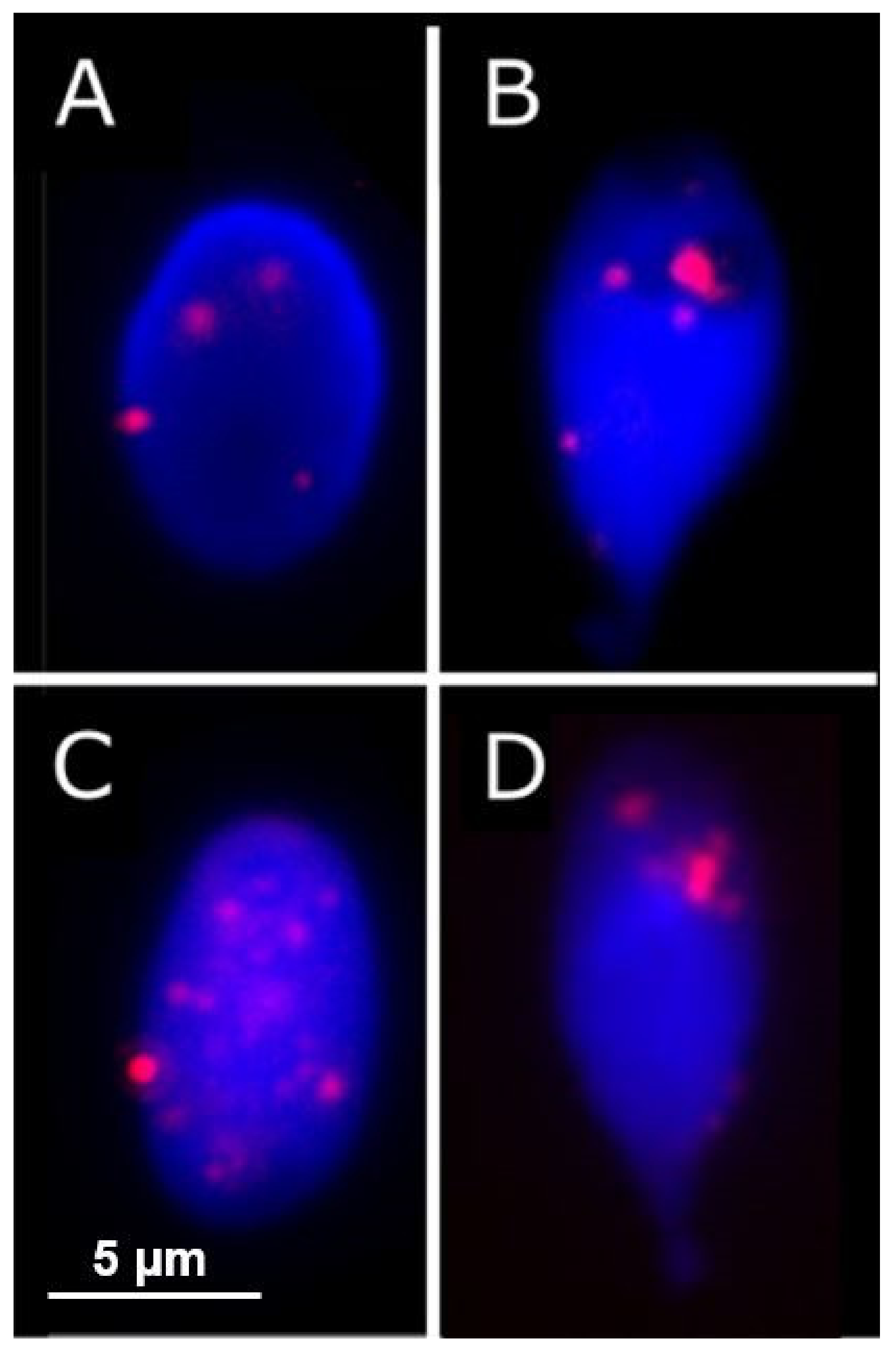
2.2. Greater Number of Telomere Signals Observed in Infertile Cohort
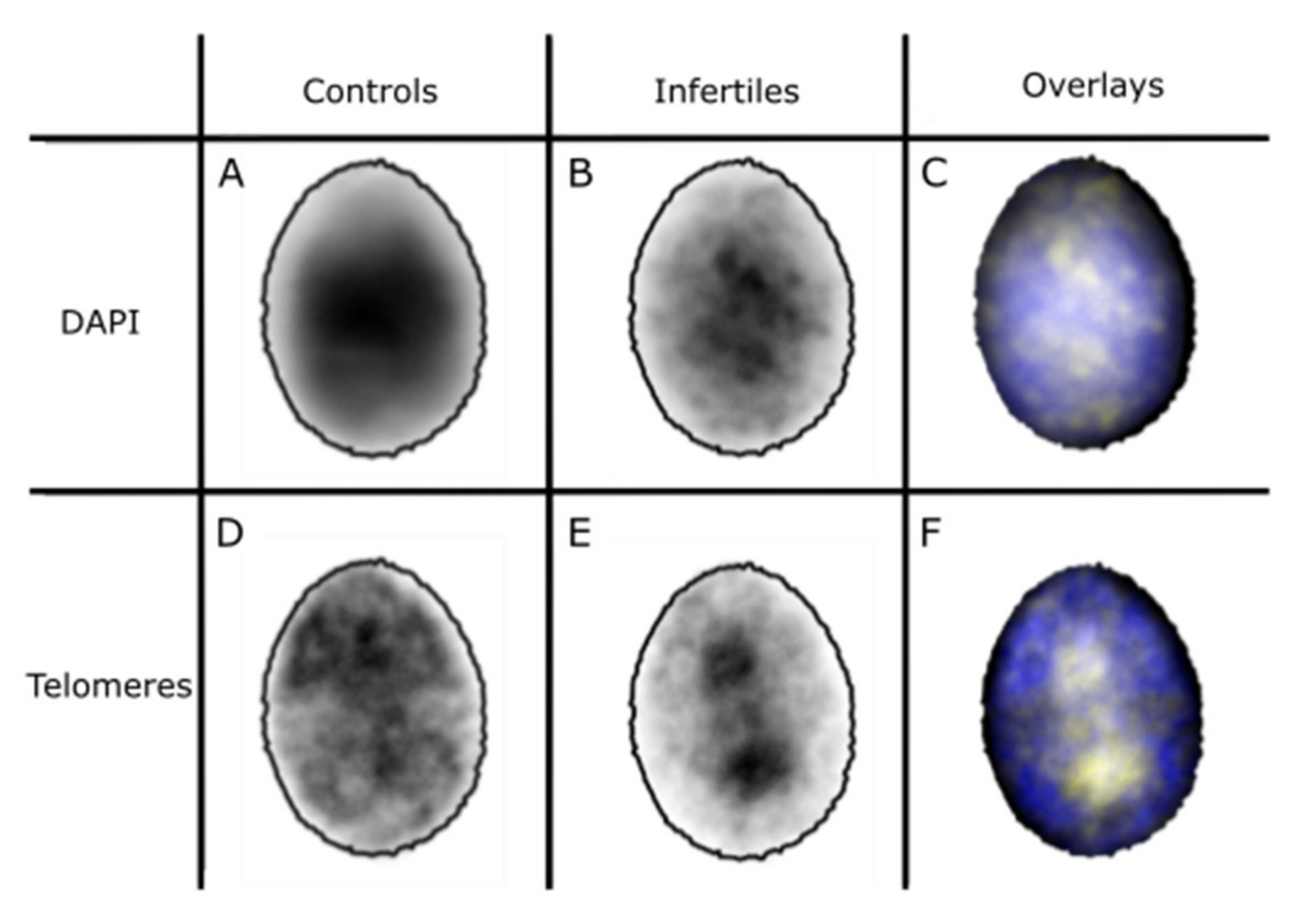
2.3. 3D Distribution of Telomeres
3. Discussion
4. Materials and Methods
4.1. Semen Samples
4.2. Telomeres and FISH
4.3. 2D Telomere Distribution in Fertile vs. Infertile Males
4.4. 3D Telomere Distribution in Infertile vs. Control Cohorts
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ray, P.F.; Toure, A.; Metzler-Guillemain, C.; Mitchell, M.J.; Arnoult, C.; Coutton, C. Genetic abnormalities leading to qualitative de-fects of sperm morphology or function. Clin. Genet. 2017, 91, 217–232. [Google Scholar] [CrossRef]
- Ribas-Maynou, J.; Benet, J. Single and Double Strand Sperm DNA Damage: Different Reproductive Effects on Male Fertility. Genes 2019, 10, 105. [Google Scholar] [CrossRef] [Green Version]
- Cho, C.-L.; Agarwal, A. Role of sperm DNA fragmentation in male factor infertility: A systematic review. Arab. J. Urol. 2018, 16, 21–34. [Google Scholar] [CrossRef] [Green Version]
- Bracke, A.; Peeters, K.; Punjabi, U.; Hoogewijs, D.; Dewilde, S. A search for molecular mechanisms underlying male idiopathic in-fertility. In Reproductive BioMedicine Online; Elsevier Ltd.: Amsterdam, The Netherlands, 2018; Volume 36, pp. 327–339. [Google Scholar]
- Fice, H.E.; Robaire, B. Telomere Dynamics throughout Spermatogenesis. Genes 2019, 10, 525. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, K.; Sivapalan, G.; Gibbons, N.; Tempest, H.; Griffin, D.K. The genetic basis of infertility. Reproduction 2003, 126, 13–25. [Google Scholar] [CrossRef] [PubMed]
- Griffin, D.K.; A Finch, K. The genetic and cytogenetic basis of male infertility. Hum. Fertil. 2005, 8, 19–26. [Google Scholar] [CrossRef]
- Jennings, C.; Powell, D. Genome organisation in the murine sperm nucleus. Zygote 1995, 3, 123–131. [Google Scholar] [CrossRef]
- Zalensky, A.O.; Allen, M.J.; Kobayashi, A.; Zalenskaya, I.A.; Balhorn, R.; Bradbury, E.M. Well-defined genome architecture in the hu-man sperm nucleus. Chromosoma 1995, 103, 577–590. [Google Scholar] [CrossRef]
- Zalensky, A.O.; Breneman, J.W.; Zalenskaya, I.A.; Brinkley, B.R.; Bradbury, E.M. Organization of centromeres in the decondensed nuclei of mature human sperm. Chromosoma 1993, 102, 509–518. [Google Scholar] [CrossRef] [PubMed]
- Solov’eva, L.; Svetlova, M.; Bodinski, D.; Zalensky, A.O. Nature of telomere dimers and chromosome looping in human sperma-tozoa. Chromosome Res. 2004, 12, 817–823. [Google Scholar] [CrossRef] [Green Version]
- Sotolongo, B.; Huang, T.T.F.; Isenberger, E.; Ward, W.S. An Endogenous Nuclease in Hamster, Mouse, and Human Spermatozoa Cleaves DNA into Loop-Sized Fragments. J. Androl. 2005, 26, 272–280. [Google Scholar] [CrossRef]
- Ward, W.S.; Kimura, Y.; Yanagimachi, R. An Intact Sperm Nuclear Matrix May Be Necessary for the Mouse Paternal Genome to Participate in Embryonic Development1. Biol. Reprod. 1999, 60, 702–706. [Google Scholar] [CrossRef] [Green Version]
- Zalenskaya, I.A.; Bradbury, E.; Zalensky, A.O. Chromatin Structure of Telomere Domain in Human Sperm. Biochem. Biophys. Res. Commun. 2000, 279, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.Y.; Bisig, C.G.; Conrad, M.N.; Ditamo, Y.; de Almeida, L.P.; Dresser, M.E.; Pezza, R.J.; Lee, C.Y.; Bisig, C.G.; Conrad, M.N.; et al. Telomere-led meiotic chromosome movements: Recent update in structure and function. Nucleus 2020, 11, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Rocca, M.S.; Foresta, C.; Ferlin, A. Telomere length: Lights and shadows on their role in human reproduction. Biol. Reprod. 2018, 100, 305–317. [Google Scholar] [CrossRef] [PubMed]
- Zalenskaya, I.A.; Zalensky, A.O. Non-random positioning of chromosomes in human sperm nuclei. Chromosome Res. 2004, 12, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Mudrak, O.; Tomilin, N.; Zalensky, A. Chromosome architecture in the decondensing human sperm nucleus. J. Cell Sci. 2005, 118, 4541–4550. [Google Scholar] [CrossRef] [Green Version]
- Luetjens, C.M.; Payne, C.; Schatten, G. Non-random chromosome positioning in human sperm and sex chromosome anomalies following intracytoplasmic sperm injection. Lancet 1999, 353, 1240. [Google Scholar] [CrossRef]
- Hazzouri, M.; Rousseaux, S.; Mongelard, F.; Usson, Y.; Pelletier, R.; Faure, A.K.; Vourc’h, C.; Sele, B. Genome organization in the human sperm nu-cleus studied by FISH and confocal microscopy. Mol. Reprod. Dev. 2000, 55, 307–315. [Google Scholar] [CrossRef]
- Foster, H.; Abeydeera, L.R.; Griffin, D.K.; Bridger, J. Non-random chromosome positioning in mammalian sperm nuclei, with migration of the sex chromosomes during late spermatogenesis. J. Cell Sci. 2005, 118, 1811–1820. [Google Scholar] [CrossRef] [Green Version]
- Pereira, C.D.; Serrano, J.B.; Martins, F.; da Cruz e Silva, O.A.B.; Rebelo, S. Nuclear envelope dynamics during mammalian spermato-genesis: New insights on male fertility. Biol. Rev. 2019, 94, 1195–1219. [Google Scholar] [CrossRef]
- Wykes, S.M.; Krawetz, S.A. The Structural Organization of Sperm Chromatin. J. Biol. Chem. 2003, 278, 29471–29477. [Google Scholar] [CrossRef] [Green Version]
- Finch, K.; Fonseka, K.; Abogrein, A.; Ioannou, D.; Handyside, A.; Thornhill, A.; Hickson, N.; Griffin, D. Nuclear organization in human sperm: Preliminary evidence for altered sex chromosome centromere position in infertile males. Hum. Reprod. 2008, 23, 1263–1270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olszewska, M.; Wiland, E.; Kurpisz, M. Positioning of chromosome 15, 18, X and Y centromeres in sperm cells of fertile individ-uals and infertile patients with increased level of aneuploidy. Chromosome Res. 2008, 16, 875–890. [Google Scholar] [CrossRef] [PubMed]
- Perdrix, A.; Rives, N. Motile sperm organelle morphology examination (MSOME) and sperm head vacuoles: State of the art in 2013. Hum. Reprod. Update 2013, 19, 527–541. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alladin, N.; Moskovtsev, S.I.; Russell, H.; Kenigsberg, S.; Lulat, A.G.-M.; Librach, C.L. The three-dimensional image analysis of the chromocenter in motile and immotile human sperm. Syst. Biol. Reprod. Med. 2013, 59, 146–152. [Google Scholar] [CrossRef]
- Wiland, E.; Olszewska, M.; Kurpisz, M. Interindividual differences and alterations in the topology of chromosomes in human sperm nuclei of fertile donors and carriers of reciprocal translocations. Chromosome Res. 2008, 16, 291–305. [Google Scholar] [CrossRef] [PubMed]
- Ioannou, D.; Griffin, D.K. Nanotechnology and molecular cytogenetics: The future has not yet arrived. Nano Rev. 2010, 1. [Google Scholar] [CrossRef]
- Ellis, P.J.I.; Griffin, D.K. Form from Function, Order from Chaos in Male Germline Chromatin. Genes 2020, 11, 210. [Google Scholar] [CrossRef] [Green Version]
- Champroux, A.; Damon-Soubeyrand, C.; Goubely, C.; Bravard, S.; Henry-Berger, J.; Guiton, R.; Saez, F.; Drevet, J.; Kocer, A. Nuclear Integrity but Not To-pology of Mouse Sperm Chromosome is Affected by Oxidative DNA Damage. Genes 2018, 9, 501. [Google Scholar] [CrossRef] [Green Version]
- Wiland, E.; Fraczek, M.; Olszewska, M.; Kurpisz, M. Topology of chromosome centromeres in human sperm nuclei with high levels of DNA damage. Sci. Rep. 2016, 6, 31614. [Google Scholar] [CrossRef] [Green Version]
- Bisht, S.; Dada, R. Oxidative stress: Major executioner in disease pathology, role in sperm DNA damage and preventive strate-gies. Front Biosci. 2017, 9, 420–447. [Google Scholar]
- Ioannou, D.; Griffin, D. Male Fertility, Chromosome Abnormalities, and Nuclear Organization. Cytogenet. Genome Res. 2010, 133, 269–279. [Google Scholar] [CrossRef] [PubMed]
- Gillies, E.A.; Cannon, R.M.; Green, R.B.; Pacey, A.A. Hydrodynamic propulsion of human sperm. J. Fluid Mech. 2009, 625, 445. [Google Scholar] [CrossRef] [Green Version]
- Skinner, B.M.; Rathje, C.C.; Bacon, J.; Johnson, E.E.P.; Larson, E.L.; Kopania, E.E.K.; Good, J.M.; Yousafzai, G.; Affara, N.A.; Ellis, P.J.I. A high-throughput method for unbiased quan-titation and categorization of nuclear morphology. Biol. Reprod. 2019, 100, 1250–1260. [Google Scholar] [CrossRef] [Green Version]
- Franco, J.G.; Baruffi, R.L.R.; Mauri, A.L.; Petersen, C.G.; A Oliveira, J.B.; Vagnini, L. Significance of large nuclear vacuoles in human spermatozoa: Implications for ICSI. Reprod. Biomed. Online 2008, 17, 42–45. [Google Scholar] [CrossRef]
- Cremer, T.; Cremer, C. Chromosome territories, nuclear architecture and gene regulation in mammalian cells. Nat. Rev. Genet. 2001, 2, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Voldgorn, Y.I.; Adilgereeva, E.P.; Nekrasov, E.D.; Lavrov, A.V. Cultivation and Differentiation Change Nuclear Localization of Chromosome Centromeres in Human Mesenchymal Stem Cells. PLoS ONE 2015, 10, e0118350. [Google Scholar] [CrossRef]
- Wiblin, A.E.; Cui, W.; Clark, J.A.; Bickmore, W.A. Distinctive nuclear organisation of centromeres and regions involved in pluripo-tency in human embryonic stem cells. J. Cell Sci. 2005, 118, 3861–3868. [Google Scholar] [CrossRef] [Green Version]
- Kuroda, M.; Tanabe, H.; Yoshida, K.; Oikawa, K.; Saito, A.; Kiyuna, T.; Mizusawa, H.; Mukai, K. Alteration of chromosome positioning during adipocyte differentiation. J. Cell Sci. 2004, 117, 5897–5903. [Google Scholar] [CrossRef] [Green Version]
- Mewborn, S.K.; Puckelwartz, M.J.; Abuisneineh, F.; Fahrenbach, J.P.; Zhang, Y.; MacLeod, H.; Dellefave, L.; Pytel, P.; Selig, S.; Labno, C.M.; et al. Altered Chromosomal Positioning, Compaction, and Gene Expression with a Lamin A/C Gene Mutation. PLoS ONE 2010, 5, e14342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ioannou, D.; Meershoek, E.J.; Christopikou, D.; Ellis, M.; Thornhill, A.R.; Griffin, D.K. Nuclear organisation of sperm remains remarkably unaffected in the presence of defective spermatogenesis. Chromosome Res. 2011, 19, 741–753. [Google Scholar] [CrossRef] [Green Version]
- Schulz, K.N.; Harrison, M.M. Mechanisms regulating zygotic genome activation. Nat. Rev. Genet. 2019, 20, 221–234. [Google Scholar] [CrossRef]
- Svoboda, P. Mammalian zygotic genome activation. Semin. Cell Dev. Biol. 2018, 84, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Baur, J.; Zou, Y.; Shay, J.W.; Wright, W.E. Telomere Position Effect in Human Cells. Science 2001, 292, 2075–2077. [Google Scholar] [CrossRef]
- Blasco, M.A. The epigenetic regulation of mammalian telomeres. Nat. Rev. Genet. 2007, 8, 299–309. [Google Scholar] [CrossRef]
- Palladino, F.; Laroche, T.; Gilson, E.; Axelrod, A.; Pillus, L.; Gasser, S. SIR3 and SIR4 proteins are required for the positioning and integrity of yeast telomeres. Cell 1993, 75, 543–555. [Google Scholar] [CrossRef]
- Dada, R.; Kumar, M.; Jesudasan, R.; Fernández, J.L.; Gosálvez, J.; Agarwal, A. Epigenetics and its role in male infertility. J. Assist. Reprod. Genet. 2012, 29, 213–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitamura, A.; Miyauchi, N.; Hamada, H.; Hiura, H.; Chiba, H.; Okae, H.; Sato, A.; John, R.; Arima, T. Epigenetic alterations in sperm associated with male infertility. Congenit. Anomalies 2015, 55, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Urdinguio, R.G.; Bayón, G.F.; Dmitrijeva, M.; Toraño, E.G.; Bravo, C.; Fraga, M.F.; Bassas, L.; Larriba, S.; Fernández, A.F. Aberrant DNA methylation patterns of sper-matozoa in men with unexplained infertility. Hum. Reprod. 2015, 30, 1014–1028. [Google Scholar] [CrossRef] [Green Version]
- Aston, K.I.; Uren, P.J.; Jenkins, T.G.; Horsager, A.; Cairns, B.R.; Smith, A.D.; Carrell, D.T. Aberrant sperm DNA methylation predicts male fertil-ity status and embryo quality. Fertil. Steril. 2015, 104, 1388–1397.e5. [Google Scholar] [CrossRef]
- Montjean, D.; Zini, A.; Ravel, C.; Belloc, S.; Dalleac, A.; Copin, H.; Boyer, P.; McElreavey, K.; Benkhalifa, M. Sperm global DNA methylation level: Association with semen parameters and genome integrity. Androl. 2015, 3, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Moskovtsev, S.I.; Willis, J.; White, J.; Mullen, J.B.M. Sperm DNA Damage: Correlation to Severity of Semen Abnormalities. Urology 2009, 74, 789–793. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A. Role of sperm chromatin abnormalities and DNA damage in male infertility. Hum. Reprod. Update 2003, 9, 331–345. [Google Scholar] [CrossRef] [Green Version]
- Evenson, D.P.; Jost, L.K.; Marshall, D.; Zinaman, M.J.; Clegg, E.; Purvis, K.; De Angelis, P.; Claussen, O.P. Utility of the sperm chromatin structure assay as a diagnostic and prognostic tool in the human fertility clinic. Hum. Reprod. 1999, 14, 1039–1049. [Google Scholar] [CrossRef]
- Evenson, D.P.; Larson, K.L.; Jost, L.K. Sperm Chromatin Structure Assay: Its Clinical Use for Detecting Sperm DNA Fragmentation in Male Infertility and Comparisons with Other Techniques. J. Androl. 2002, 23, 25–43. [Google Scholar] [CrossRef]
- Biron-Shental, T.; Wiser, A.; Hershko-Klement, A.; Markovitch, O.; Amiel, A.; Berkovitch, A. Sub-fertile sperm cells exemplify telo-mere dysfunction. J. Assist. Reprod. Genet. 2018, 35, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Fernández, J.L.; Muriel, L.; Rivero, M.T.; Goyanes, V.; Vazquez, R.; Alvarez, J.G. The sperm chromatin dispersion test: A simple method for the determination of sperm DNA fragmentation. J. Androl. 2003, 24, 59–66. [Google Scholar]
- Tanemura, K.; Ogura, A.; Cheong, C.; Gotoh, H.; Matsumoto, K.; Sato, E.; Hayashi, Y.; Lee, H.-W.; Kondo, T. Dynamic rearrangement of telomeres during sper-matogenesis in mice. Dev. Biol. 2005, 281, 196–207. [Google Scholar] [CrossRef] [Green Version]
- Wright, W.E.; Piatyszek, M.A.; Rainey, W.E.; Byrd, W.; Shay, J.W. Telomerase activity in human germline and embryonic tissues and cells. Dev. Genet. 1996, 18, 173–179. [Google Scholar] [CrossRef]
- Turner, S.; Wong, H.P.; Rai, J.; Hartshorne, G.M. Telomere lengths in human oocytes, cleavage stage embryos and blastocysts. Mol. Hum. Reprod. 2010, 16, 685–694. [Google Scholar] [CrossRef] [Green Version]
- Wright, D.L. Characterization of telomerase activity in the human oocyte and preimplantation embryo. Mol. Hum. Reprod. 2001, 7, 947–955. [Google Scholar] [CrossRef] [Green Version]
- Allsopp, R.C.; Vaziri, H.; Patterson, C.; Goldstein, S.; Younglai, E.V.; Futcher, A.B.; Greider, C.W.; Harley, C.B. Telomere length predicts replicative capacity of human fibroblasts. Proc. Natl. Acad. Sci. USA 1992, 89, 10114–10118. [Google Scholar] [CrossRef] [Green Version]
- Baird, D.M.; Britt-Compton, B.; Rowson, J.; Amso, N.; Gregory, L.; Kipling, D. Telomere instability in the male germline. Hum. Mol. Genet. 2005, 15, 45–51. [Google Scholar] [CrossRef] [Green Version]
- Cooke, H.; Smith, B. Variability at the Telomeres of the Human X/Y Pseudoautosomal Region. Cold Spring Harb. Symp. Quant. Biol. 1986, 51, 213–219. [Google Scholar] [CrossRef]
- De Lange, T.; Shiue, L.; Myers, R.M.; Cox, D.R.; Naylor, S.L.; Killery, A.M.; Varmus, H.E. Structure and variability of human chromosome ends. Mol. Cell Biol. 1990, 10, 518–527. [Google Scholar] [CrossRef] [Green Version]
- Kimura, M.; Cherkas, L.F.; Kato, B.S.; Demissie, S.; Hjelmborg, J.B.; Brimacombe, M.; Cupples, A.; Hunkin, J.L.; Gardner, J.P.; Lu, X.; et al. Offspring’s Leukocyte Telomere Length, Paternal Age, and Telomere Elongation in Sperm. PLoS Genet. 2008, 4, e37. [Google Scholar] [CrossRef] [Green Version]
- Vasilopoulos, E.; Fragkiadaki, P.; Kalliora, C.; Fragou, D.; Docea, A.O.; Vakonaki, E.; Tsoukalas, D.; Calina, D.; Buga, A.M.; Georgiadis, G.; et al. The association of female and male infer-tility with telomere length (Review). Int. J. Mol. Med. 2019, 44, 375–389. [Google Scholar]
- Turner, S.; Hartshorne, G.M. Telomere lengths in human pronuclei, oocytes and spermatozoa. Mol. Hum. Reprod. 2013, 19, 510–518. [Google Scholar] [CrossRef]
- Ichikawa, Y.; Nishimura, Y.; Kurumizaka, H.; Shimizu, M. Nucleosome organization and chromatin dynamics in telomeres. Biomol. Concepts 2015, 6, 67–75. [Google Scholar] [CrossRef]
- Skinner, B.M.; Bacon, J.; Rathje, C.C.; Larson, E.L.; Kopania, E.E.K.; Good, J.M.; Affara, N.A.; Ellis, P.J.I. Automated Nuclear Cartography Reveals Con-served Sperm Chromosome Territory Localization across 2 Million Years of Mouse Evolution. Genes 2019, 10, 109. [Google Scholar] [CrossRef] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018; Available online: http://www.R-project.org/ (accessed on 9 July 2021).
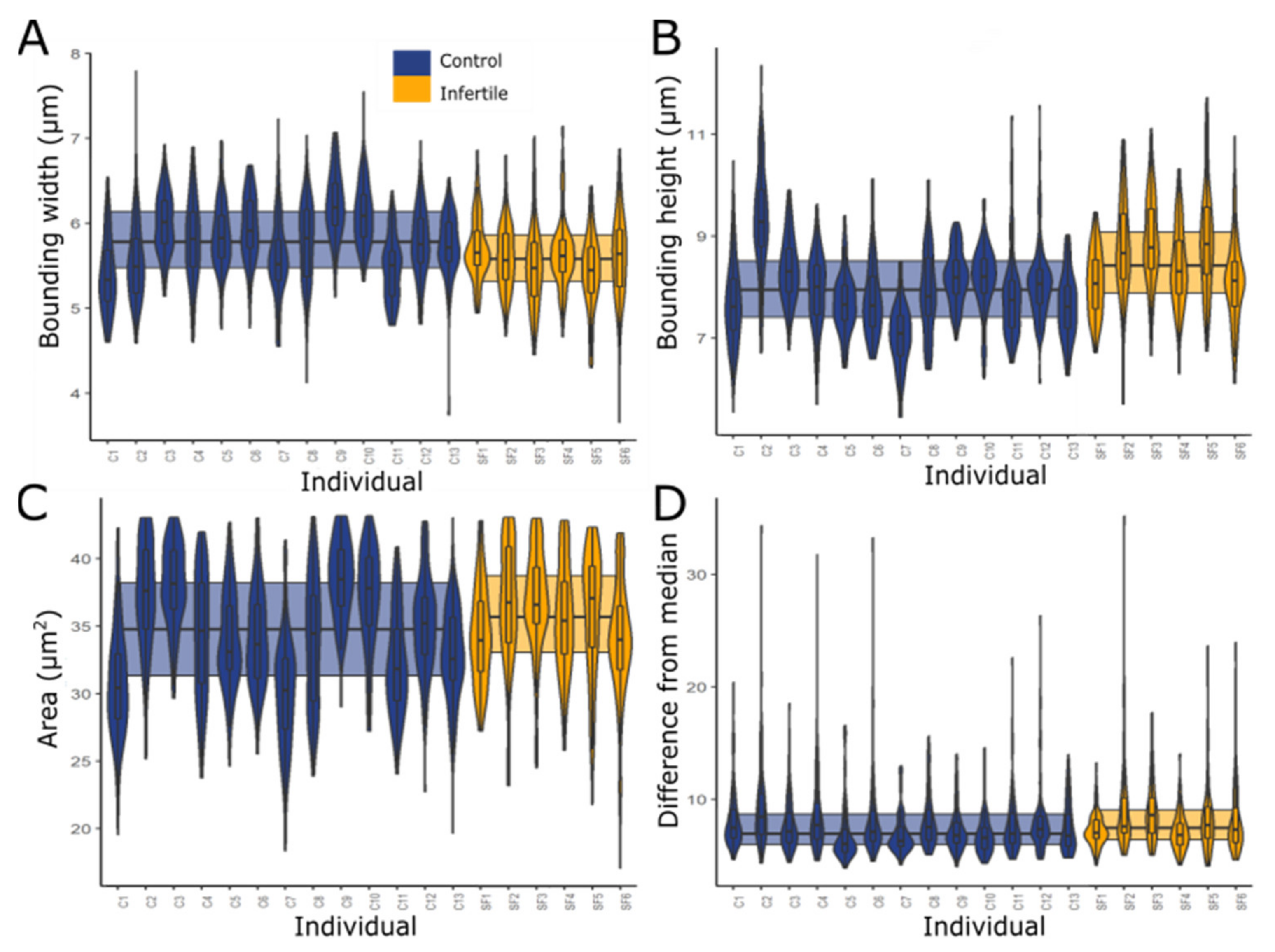


| Parameter | Controls | Infertiles | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean ± SD | Mean ± SEM | Mean | Standard Deviation | Mean ± SD | Mean ± SEM | |
| Bounding width (µm) | 5.77 | 0.492 | 5.280–6.263 | 5.754–5.786 | 5.58 | 0.456 | 5.122–6.034 | 5.559–5.601 |
| Bounding height (µm) | 8.00 | 0.937 | 7.066–8.940 | 7.970–8.030 | 8.51 | 0.953 | 7.553–9.458 | 8.466–8.554 |
| Area (µm2) | 34.45 | 4.616 | 29.831–39.063 | 34.300–34.600 | 35.45 | 4.415 | 31.033–39.863 | 35.246–35.654 |
| Difference from median | 7.96 | 3.085 | 4.874–11.045 | 7.860–8.060 * | 8.19 | 3.081 | 5.108–11.270 | 8.048–8.332 * |
| Patient Number | Concentration (×106/mL) | Motility (%) | Progressive Motility (%) | % Normal Forms |
|---|---|---|---|---|
| 1 | 20 | 20 | 10 | 5 |
| 2 | 0.8 | 0 | 0 | 5 |
| 3 | 18 | 20 | 5 | 2 |
| 4 | 2 | 5 | 0 | 5 |
| 5 | 2 | 10 | 5 | 8 |
| 6 | 60 | 45 | 25 | 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Turner, K.J.; Watson, E.M.; Skinner, B.M.; Griffin, D.K. Telomere Distribution in Human Sperm Heads and Its Relation to Sperm Nuclear Morphology: A New Marker for Male Factor Infertility? Int. J. Mol. Sci. 2021, 22, 7599. https://doi.org/10.3390/ijms22147599
Turner KJ, Watson EM, Skinner BM, Griffin DK. Telomere Distribution in Human Sperm Heads and Its Relation to Sperm Nuclear Morphology: A New Marker for Male Factor Infertility? International Journal of Molecular Sciences. 2021; 22(14):7599. https://doi.org/10.3390/ijms22147599
Chicago/Turabian StyleTurner, Kara J., Eleanor M. Watson, Benjamin M. Skinner, and Darren K. Griffin. 2021. "Telomere Distribution in Human Sperm Heads and Its Relation to Sperm Nuclear Morphology: A New Marker for Male Factor Infertility?" International Journal of Molecular Sciences 22, no. 14: 7599. https://doi.org/10.3390/ijms22147599







