Chronic Prostatitis/Chronic Pelvic Pain Syndrome Leads to Impaired Semen Parameters, Increased Sperm DNA Fragmentation and Unfavorable Changes of Sperm Protamine mRNA Ratio
Abstract
:1. Introduction
2. Results
2.1. Basic Semen Parameters, Biochemical Parameters and Inflammatory Parameters
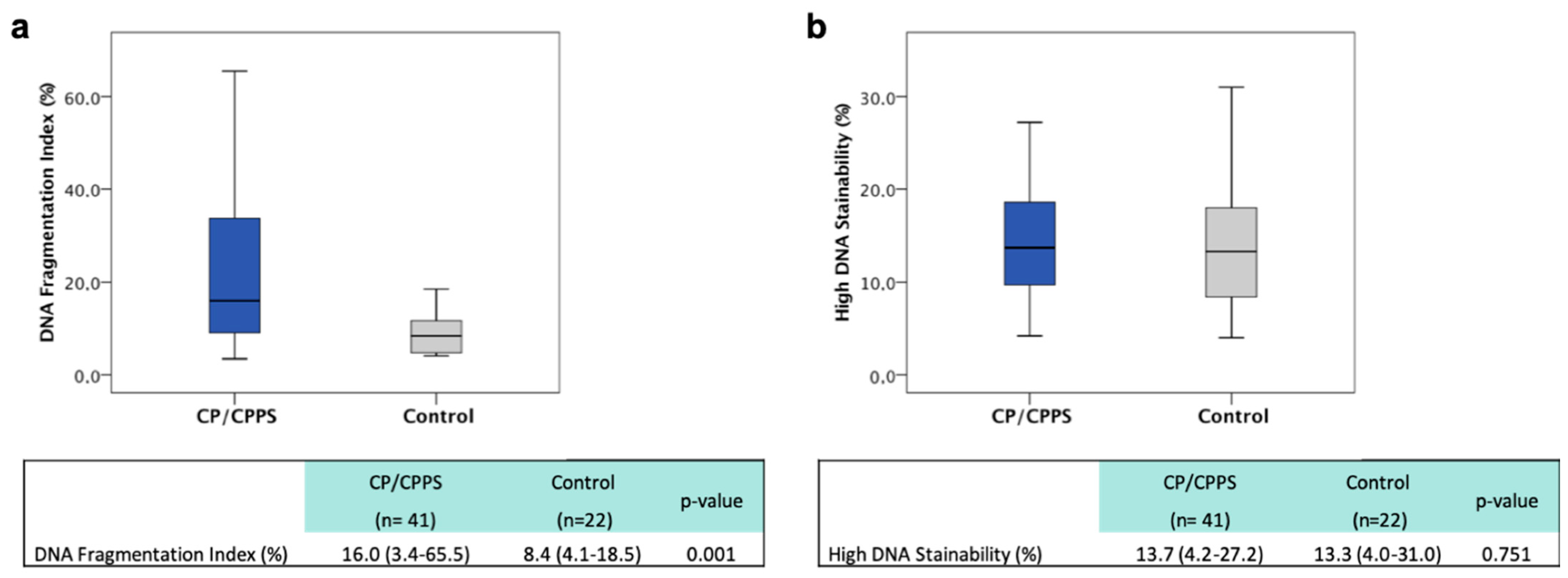
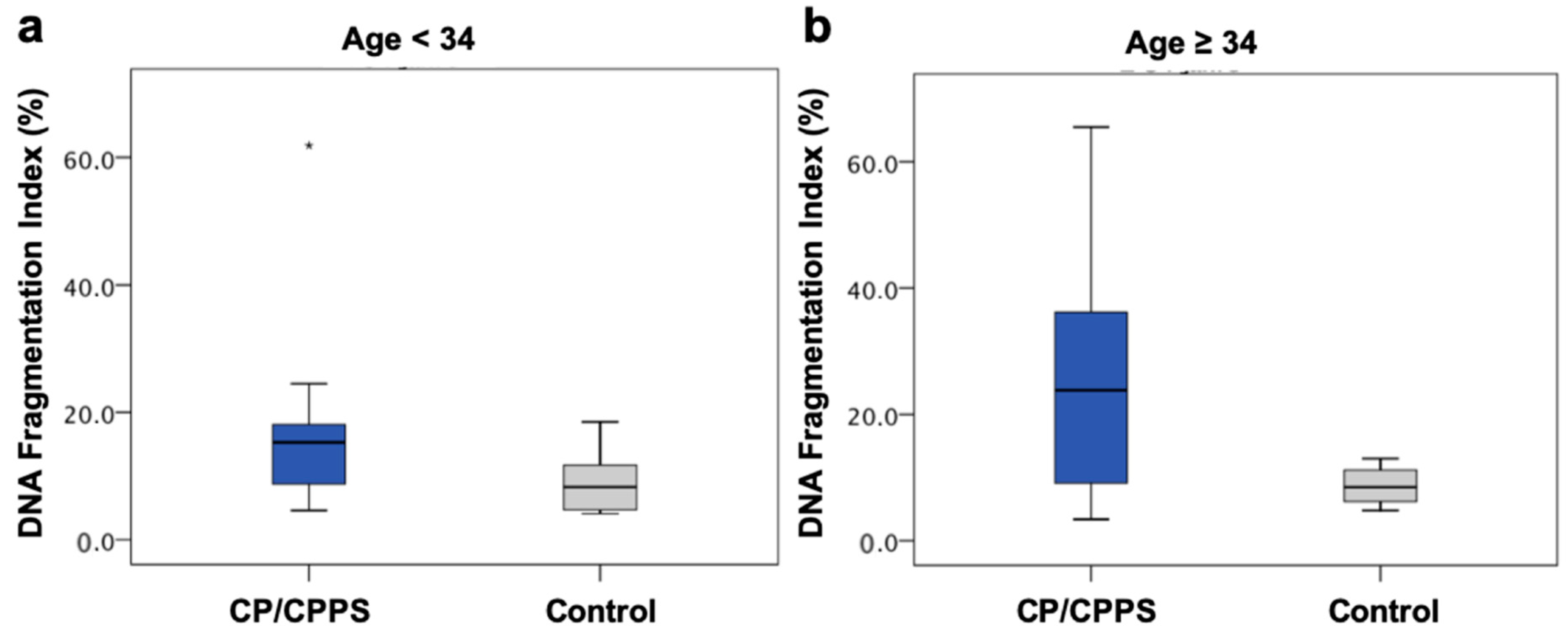
2.2. Sperm DNA Fragmentation
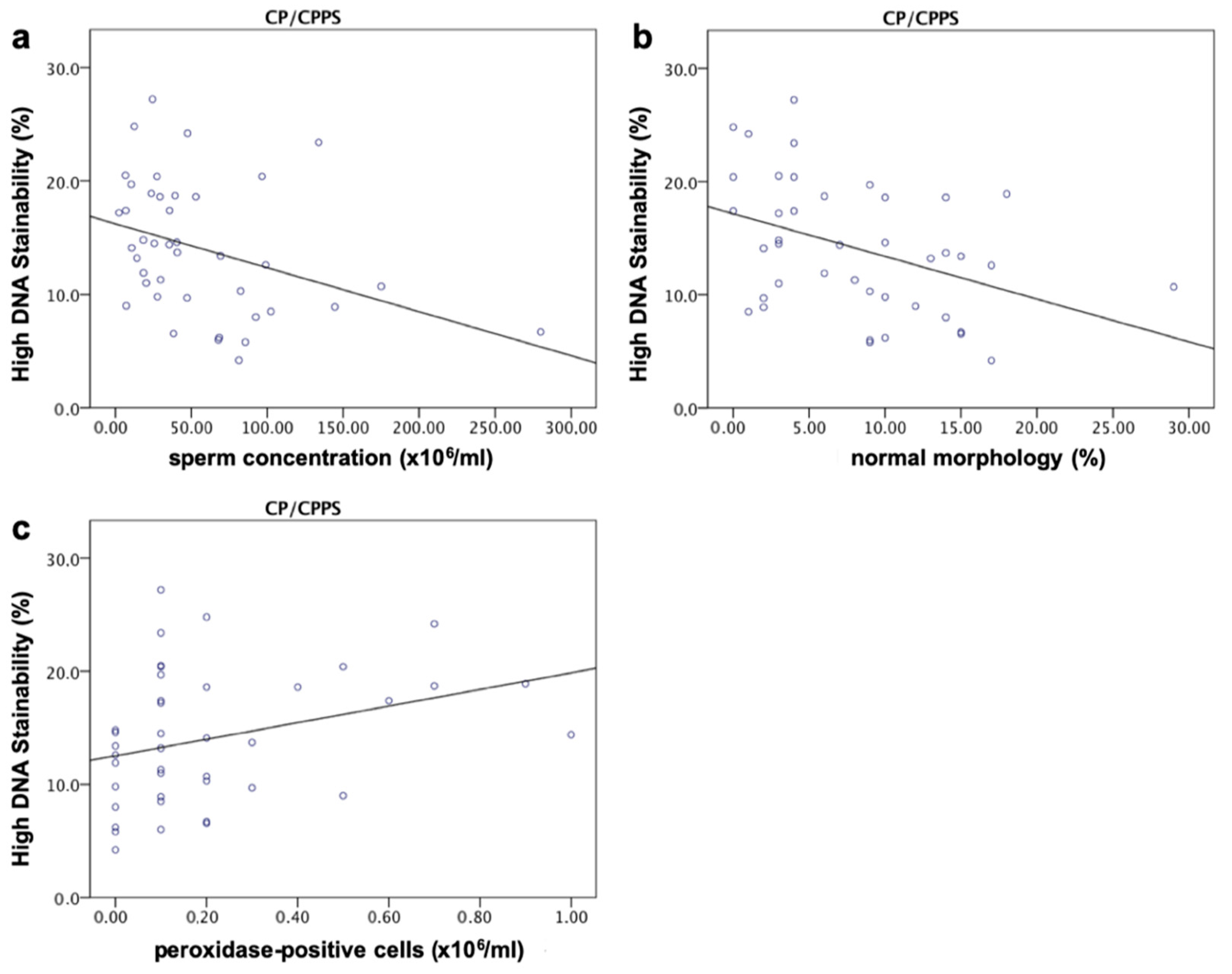
2.3. High DNA Stainability
2.4. Sperm Protamine mRNA Ratio
2.5. DFI, HDS, Protamine mRNA Ratio and Inflammatory Parameters
2.6. Basic Semen Parameters, DFI, HDS, Protamine mRNA Ratio and UPOINTS
3. Discussion
3.1. CP/CPPS and Conventional Semen Parameters
3.2. Biochemical Parameters
3.3. CP/CPPS and Sperm DNA Fragmentation
3.4. CP/CPPS and HDS
3.5. CP/CPPS and Sperm Protamine mRNA Ratio
3.6. Inflammatory Parameters and DFI, HDS, P1/P2 mRNA Ratio
4. Materials and Methods
4.1. Sample Acquisition
4.2. Semen Analysis
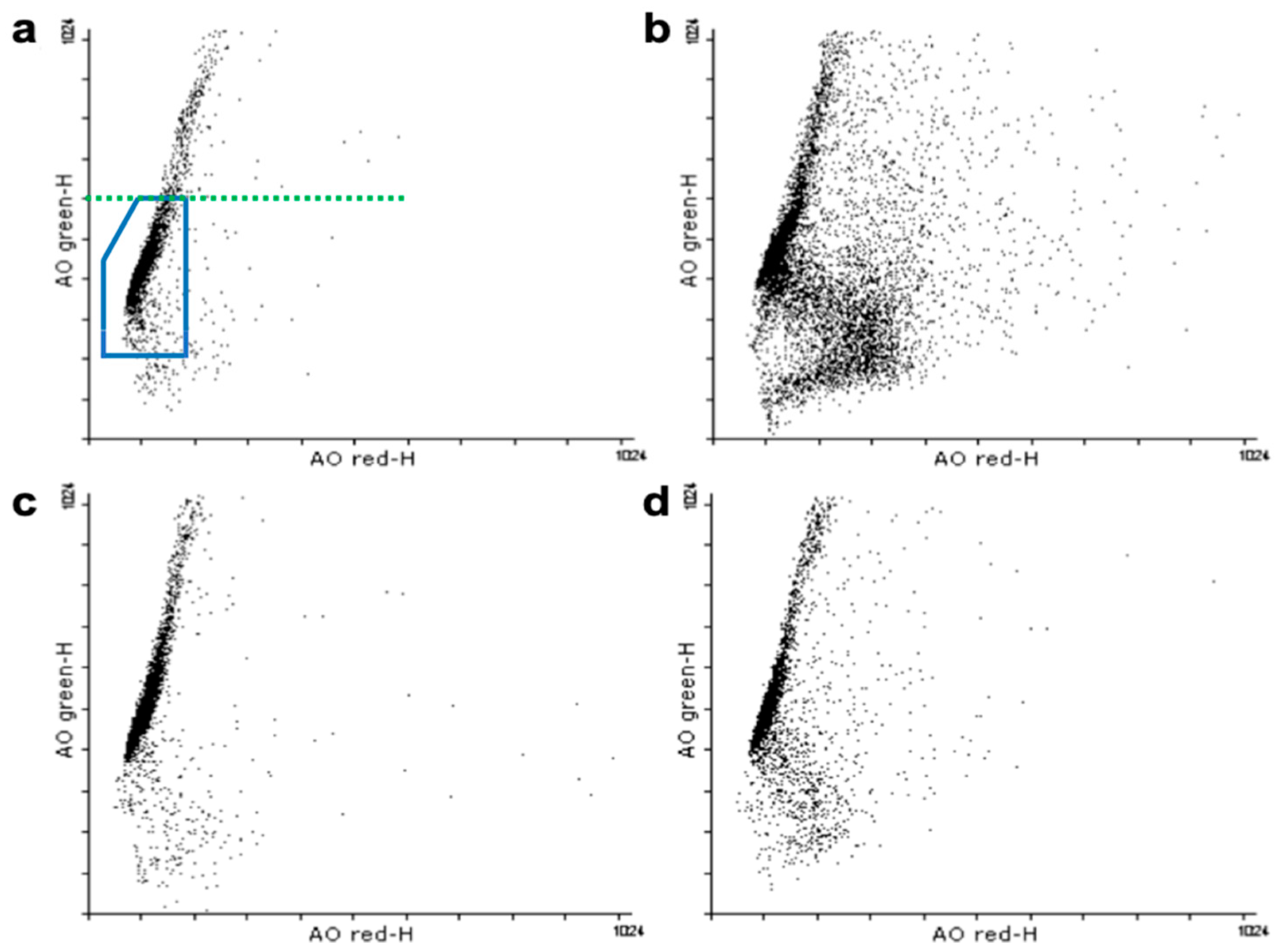
4.3. Sperm Chromatin Structure Assay (SCSA)
4.4. RNA Isolation, cDNA Synthesis and RT-qPCR
4.5. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Schaeffer, A.J. Epidemiology and Evaluation of Chronic Pelvic Pain Syndrome in Men. Int. J. Antimicrob. Agents 2008, 31 (Suppl. 1), 108–111. [Google Scholar] [CrossRef]
- Collins, M.M.; Stafford, R.S.; O’Leary, M.P.; Barry, M.J. How Common Is Prostatitis? A National Survey of Physician Visits. J. Urol. 1998, 159, 1224–1228. [Google Scholar] [CrossRef]
- Krieger, J.N.; Nyberg, L.; Nickel, J.C. NIH Consensus Definition and Classification of Prostatitis. JAMA 1999, 282, 236–237. [Google Scholar] [CrossRef]
- Schneider, H.; Ludwig, M.; Weidner, W.; Brähler, E. Experience with Different Questionnaires in the Management of Patients with CP/CPPS: GPSS, IPSS and NIH-CPSI. World J. Urol. 2003, 21, 116–118. [Google Scholar] [CrossRef]
- Shoskes, D.A.; Nickel, J.C.; Dolinga, R.; Prots, D. Clinical Phenotyping of Patients With Chronic Prostatitis/Chronic Pelvic Pain Syndrome and Correlation With Symptom Severity. Urology 2009, 73, 538–542. [Google Scholar] [CrossRef]
- Magri, V.; Wagenlehner, F.; Perletti, G.; Schneider, S.; Marras, E.; Naber, K.G.; Weidner, W. Use of the UPOINT Chronic Prostatitis/Chronic Pelvic Pain Syndrome Classification in European Patient Cohorts: Sexual Function Domain Improves Correlations. J. Urol. 2010, 184, 2339–2345. [Google Scholar] [CrossRef]
- Nickel, J.C.; Shoskes, D. Phenotypic Approach to the Management of Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Curr. Urol. Rep. 2009, 7, 132–137. [Google Scholar] [CrossRef]
- Magri, V.; Marras, E.; Restelli, A.; Wagenlehner, F.M.E.; Perletti, G. Multimodal Therapy for Category III Chronic Prostatitis/Chronic Pelvic Pain Syndrome in UPOINTS Phenotyped Patients. Exp. Ther. Med. 2015, 9, 658–666. [Google Scholar] [CrossRef] [Green Version]
- Condorelli, R.A.; Russo, G.I.; Calogero, A.E.; Morgia, G.; La Vignera, S. Chronic Prostatitis and Its Detrimental Impact on Sperm Parameters: A Systematic Review and Meta-Analysis. J. Endocrinol. Investig. 2017, 40, 1209–1218. [Google Scholar] [CrossRef]
- Schagdarsurengin, U.; Teuchert, L.M.; Hagenkötter, C.; Nesheim, N.; Dansranjavin, T.; Schuppe, H.C.; Gies, S.; Pilatz, A.; Weidner, W.; Wagenlehner, F.M.E. Chronic Prostatitis Affects Male Reproductive Health and Is Associated with Systemic and Local Epigenetic Inactivation of C-X-C Motif Chemokine 12 Receptor C-X-C Chemokine Receptor Type 4. Urol. Int. 2017, 98, 89–101. [Google Scholar] [CrossRef]
- Aitken, R.J.; De Iuliis, G.N. On the Possible Origins of DNA Damage in Human Spermatozoa. Mol. Hum. Reprod. 2009, 16, 3–13. [Google Scholar] [CrossRef] [Green Version]
- González-Marín, C.; Gosálvez, J.; Roy, R. Types, Causes, Detection and Repair of DNA Fragmentation in Animal and Human Sperm Cells. Int. J. Mol. Sci. 2012, 13, 14026–14052. [Google Scholar] [CrossRef] [Green Version]
- Cho, C.L.; Agarwal, A. Role of Sperm DNA Fragmentation in Male Factor Infertility: A Systematic Review. Arab J. Urol. 2018, 16, 21–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aitken, R.J.; Bakos, H.W. Should We Be Measuring DNA Damage in Human Spermatozoa? New Light on an Old Question. Hum. Reprod. 2021, 36, 1175–1185. [Google Scholar] [CrossRef]
- Evenson, D.; Jost, L. Sperm Chromatin Structure Assay Is Useful for Fertility Assessment. Methods Cell Sci. 2000, 22, 169–189. [Google Scholar] [CrossRef] [PubMed]
- Evenson, D.P. The Sperm Chromatin Structure Assay (SCSA®) and Other Sperm DNA Fragmentation Tests for Evaluation of Sperm Nuclear DNA Integrity as Related to Fertility. Anim. Reprod. Sci. 2016, 169, 56–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evenson, D.P. Evaluation of Sperm Chromatin Structure and DNA Strand Breaks Is an Important Part of Clinical Male Fertility Assessment. Transl. Androl. Urol. 2017, 6, 495–500. [Google Scholar] [CrossRef] [Green Version]
- Rex, A.S.; Aagaard, J.; Fedder, J. DNA Fragmentation in Spermatozoa: A Historical Review. Andrology 2017, 5, 622–630. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evenson, D.P.; Jost, L.K.; Marshall, D.; Zinaman, M.J.; Clegg, E.; Purvis, K.; Angelis, P. Utility of the Sperm Chromatin Structure Assay as a Diagnostic and Prognostic Tool in the Human Fertility Clinic. Hum. Reprod. 1999, 14, 1039–1049. [Google Scholar] [CrossRef]
- Baldi, E.; Muratori, M. Genetic Damage in Human Spermatozoa. In Advances in Experimental Medicine and Biology; Springer: New York, NY, USA, 2014. [Google Scholar]
- Evenson, D.P.; Wixon, R. Meta-Analysis of Sperm DNA Fragmentation Using the Sperm Chromatin Structure Assay. Reprod. Biomed. Online 2006, 12, 466–472. [Google Scholar] [CrossRef]
- Steger, K.; Balhorn, R. Sperm Nuclear Protamines: A Checkpoint to Control Sperm Chromatin Quality. Anat. Histol. Embryol. 2018, 47, 273–279. [Google Scholar] [CrossRef] [Green Version]
- Steger, K.; Wilhelm, J.; Konrad, L.; Stalf, T.; Greb, R.; Diemer, T.; Kliesch, S.; Bergmann, M.; Weidner, W. Both Protamine-1 to Protamine-2 MRNA Ratio and Bcl2 MRNA Content in Testicular Spermatids and Ejaculated Spermatozoa Discriminate between Fertile and Infertile Men. Hum. Reprod. 2008, 23, 11–16. [Google Scholar] [CrossRef] [Green Version]
- Rogenhofer, N.; Dansranjavin, T.; Schorsch, M.; Spiess, A.; Wang, H.; von Schonfeldt, V.; Cappallo-Obermann, H.; Baukloh, V.; Yang, H.; Paradowska, A.; et al. The Sperm Protamine MRNA Ratio as a Clinical Parameter to Estimate the Fertilizing Potential of Men Taking Part in an ART Programme. Hum. Reprod. 2013, 28, 969–978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ni, K.; Spiess, A.-N.; Schuppe, H.-C.; Steger, K. The Impact of Sperm Protamine Deficiency and Sperm DNA Damage on Human Male Fertility: A Systematic Review and Meta-Analysis. Andrology 2016, 4, 789–799. [Google Scholar] [CrossRef]
- Rogenhofer, N.; Ott, J.; Pilatz, A.; Wolf, J.; Thaler, C.J.; Windischbauer, L.; Schagdarsurengin, U.; Steger, K.; Von Schönfeldt, V. Unexplained Recurrent Miscarriages Are Associated with an Aberrant Sperm Protamine MRNA Content. Hum. Reprod. 2017, 32, 1574–1582. [Google Scholar] [CrossRef]
- World Health Organization; Department of Reproductive Health and Research. WHO Laboratory Manual for the Examination and Processing of Human Sperm, 5th ed.; World Health Organization: Geneva, Switzerland, 2010; p. 9. [Google Scholar]
- Marconi, M.; Pilatz, A.; Wagenlehner, F.; Diemer, T.; Weidner, W. Impact of Infection on the Secretory Capacity of the Male Accessory Glands. Int. Braz. J. Urol. 2009, 35, 299–308. [Google Scholar] [CrossRef] [Green Version]
- Rusz, A.; Pilatz, A.; Wagenlehner, F.; Linn, T.; Diemer, T.; Schuppe, H.C.; Lohmeyer, J.; Hossain, H.; Weidner, W. Influence of Urogenital Infections and Inflammation on Semen Quality and Male Fertility. World J. Urol. 2012, 30, 23–30. [Google Scholar] [CrossRef]
- Fu, W.; Zhou, Z.; Liu, S.; Li, Q.; Yao, J.; Li, W.; Yan, J. The Effect of Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) on Semen Parameters in Human Males: A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e94991. [Google Scholar] [CrossRef]
- Pilatz, A.; Boecker, M.; Schuppe, H.C.; Diemer, T.; Wagenlehner, F. Infektionen Und Infertilität. Urologe 2016, 55, 883–889. [Google Scholar] [CrossRef] [PubMed]
- Menkveld, R.; Holleboom, C.A.G.; Rhemrev, J.P.T. Measurement and Significance of Sperm Morphology. Asian J. Androl. 2011, 13, 59–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abu Hassan Abu, D.; Franken, D.R.; Hoffman, B.; Henkel, R. Accurate Sperm Morphology Assessment Predicts Sperm Function. Andrologia 2012, 44 (Suppl. 1), 571–577. [Google Scholar] [CrossRef] [PubMed]
- Diemer, T.; Huwe, P.; Ludwig, M.; Hauck, E.W.; Weidner, W. Urogenital Infection and Sperm Motility. Andrologia 2003, 35, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Henkel, R.; Offor, U.; Fisher, D. The Role of Infections and Leukocytes in Male Infertility. Andrologia 2021, 53. [Google Scholar] [CrossRef] [PubMed]
- Orhan, I.; Onur, R.; Ilhan, N.; Ardiçoglu, A. Seminal Plasma Cytokine Levels in the Diagnosis of Chronic Pelvic Pain Syndrome. Int. J. Urol. 2001, 8, 495–499. [Google Scholar] [CrossRef] [Green Version]
- Lampiao, F.; du Plessis, S.S. TNF-α and IL-6 Affect Human Sperm Function by Elevating Nitric Oxide Production. Reprod. Biomed. Online 2008, 17, 628–631. [Google Scholar] [CrossRef]
- Kopa, Z.; Wenzel, J.; Papp, G.K.; Haidl, G. Role of Granulocyte Elastase and Interleukin-6 in the Diagnosis of Male Genital Tract Inflammation. Andrologia 2005, 37, 188–194. [Google Scholar] [CrossRef]
- Eggert-Kruse, W.; Boit, R.; Rohr, G.; Aufenanger, J.; Hund, M.; Strowitzki, T. Relationship of Seminal Plasma Interleukin (IL)-8 and IL-6 with Semen Quality. Hum. Reprod. 2001, 16, 517–528. [Google Scholar] [CrossRef] [Green Version]
- Walczak-Jedrzejowska, R.; Wolski, J.K.; Slowikowska-Hilczer, J. The Role of Oxidative Stress and Antioxidants in Male Fertility. Cent. Eur. J. Urol. 2013, 66, 60–67. [Google Scholar] [CrossRef] [Green Version]
- Ludwig, M.; Vidal, A.; Diemer, T.; Pabst, W.; Failing, K.; Weidner, W. Seminal Secretory Capacity of the Male Accessory Sex Glands in Chronic Pelvic Pain Syndrome (CPPS)/Chronic Prostatitis with Special Focus on the New Prostatitis Classification. Eur. Urol. 2002, 42, 24–28. [Google Scholar] [CrossRef]
- Moazenchi, M.; Totonchi, M.; Salman Yazdi, R.; Hratian, K.; Mohseni Meybodi, M.A.; Ahmadi Panah, M.; Chehrazi, M.; Mohseni Meybodi, A. The Impact of Chlamydia Trachomatis Infection on Sperm Parameters and Male Fertility: A Comprehensive Study. Int. J. STD AIDS 2018, 29, 466–473. [Google Scholar] [CrossRef]
- Ni, K.; Steger, K.; Yang, H.; Wang, H.; Hu, K.; Chen, B. Sperm Protamine MRNA Ratio and DNA Fragmentation Index Represent Reliable Clinical Biomarkers for Men with Varicocele after Microsurgical Varicocele Ligation. J. Urol. 2014, 192, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Evgeni, E.; Charalabopoulos, K.; Asimakopoulos, B. Human Sperm DNA Fragmentation and Its Correlation with Conventional Semen Parameters. J. Reprod. Infertil. 2014, 15, 2–14. [Google Scholar] [PubMed]
- Raheem, O.A.; Walsh, T.J. Clinical Utility of Sperm DNA Fragmentation Testing: Practice Recommendations Based on Clinical Scenarios. Transl. Androl. Urol. 2017, 6 (Suppl. 4), S322–S323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Da Costa, R.; Redmann, K.; Schlatt, S. Simultaneous Detection of Sperm Membrane Integrity and DNA Fragmentation by Flow Cytometry: A Novel and Rapid Tool for Sperm Analysis. Andrology 2021. [Google Scholar] [CrossRef] [PubMed]
- Schulte, R.T.; Ohl, D.A.; Sigman, M.; Smith, G.D. Sperm DNA Damage in Male Infertility: Etiologies, Assays, and Outcomes. J. Assist. Reprod. Genet. 2010, 27, 3–12. [Google Scholar] [CrossRef] [Green Version]
- Potts, J.M.; Pasqualotto, F.F. Seminal Oxidative Stress in Patients with Chronic Prostatitis. Andrologia 2003, 35, 304–308. [Google Scholar] [CrossRef]
- Kullisaar, T.; Türk, S.; Punab, M.; Mändar, R. Oxidative Stress-Cause or Consequence of Male Genital Tract Disorders? Prostate 2012, 72, 977–983. [Google Scholar] [CrossRef]
- Evenson, D.P.; Wixon, R. Clinical Aspects of Sperm DNA Fragmentation Detection and Male Infertility. Theriogenology 2006, 65, 979–991. [Google Scholar] [CrossRef]
- Lewis, S.E.M.; Aitken, R.J.; Conner, S.J.; De Iuliis, G.; Evenson, D.P.; Henkel, R.; Giwercman, G.A.; Gharagozloo, P. The Impact of Sperm DNA Damage in Assisted Conception and beyond: Recent Advances in Diagnosis and Treatment. Reprod. Biomed. Online 2013, 27, 325–337. [Google Scholar] [CrossRef] [Green Version]
- Virro, M.R.; Larson-Cook, K.L.; Evenson, D.P. Sperm Chromatin Structure Assay (SCSA®) Parameters Are Related to Fertilization, Blastocyst Development, and Ongoing Pregnancy in in Vitro Fertilization and Intracytoplasmic Sperm Injection Cycles. Fertil. Steril. 2004, 81, 1289–1295. [Google Scholar] [CrossRef]
- Simon, L.; Castillo, J.; Oliva, R.; Lewis, S.E.M. Relationships between Human Sperm Protamines, DNA Damage and Assisted Reproduction Outcomes. Reprod. Biomed. Online 2011, 23, 724–734. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeyad, A.; Hamad, M.F.; Hammadeh, M.E. The Effects of Bacterial Infection on Human Sperm Nuclear Protamine P1/P2 Ratio and DNA Integrity. Andrologia 2018, 50, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, J.G.; Sharma, R.K.; Ollero, M.; Saleh, R.A.; Lopez, M.C.; Thomas, A.J.; Evenson, D.P.; Agarwal, A. Increased DNA Damage in Sperm from Leukocytospermic Semen Samples as Determined by the Sperm Chromatin Structure Assay. Fertil. Steril. 2002, 78, 319–329. [Google Scholar] [CrossRef]
- Nickel, J.C.; Nyberg, L.M.; Hennenfent, M. Research Guidelines for Chronic Prostatitis: Consensus Report from the First National Institutes of Health International Prostatitis Collaborative Network. Urology 1999, 54, 229–233. [Google Scholar] [CrossRef]
- Weidner, W.; Naber, K.G. Prostatitis-Syndrom: Konsensus Der 6. Internationalen Konsultation in Paris 2005. Aktuelle Urol. 2006, 37, 269–271. [Google Scholar] [CrossRef] [PubMed]
- Hochreiter, W.; Ludwig, M.; Weidner, W.; Wagenlehner, F.; Naber, K.; Eremenco, S.; Arnold, B. National Institutes of Health NIH)-Chronic Prostatitis Symptom Index Deutsche Version. Der Urol. Ausg. A 2001, 40, 16–17. [Google Scholar] [CrossRef]
- Magistro, G.; Wagenlehner, F.M.E.; Grabe, M.; Weidner, W.; Stief, C.G.; Nickel, J.C. Contemporary Management of Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Eur. Urol. 2016, 69, 286–297. [Google Scholar] [CrossRef]
- Xiao, J.; Ren, L.; Lv, H.; Ding, Q.; Lou, S.; Zhang, W.; Dong, Z. Atypical Microorganisms in Expressed Prostatic Secretion from Patients with Chronic Prostatitis/Chronic Pelvic Pain Syndrome: Microbiological Results from a Case-Control Study. Urol. Int. 2013, 91, 410–416. [Google Scholar] [CrossRef]
- Pilatz, A.; Hossain, H.; Kaiser, R.; Mankertz, A.; Schüttler, C.G.; Domann, E.; Schuppe, H.C.; Chakraborty, T.; Weidner, W.; Wagenlehner, F. Acute Epididymitis Revisited: Impact of Molecular Diagnostics on Etiology and Contemporary Guideline Recommendations. Eur. Urol. 2015, 68, 428–435. [Google Scholar] [CrossRef]
- Ludwig, M.; Steltz, C.; Huwe, P.; Schäffer, R.; Altmannsberger, M.; Weidner, W. Immunocytological analysis of leukocyte subpopulations in urine specimens before and after prostatic massage. Eur. Urol. 2001, 39, 277–282. [Google Scholar] [CrossRef]


| Parameter | CP/CPPS | Control | p-Value | WHO 2010 [27] Lower Reference Limit */Consensus Threshold Values |
|---|---|---|---|---|
| Volume (mL) | 2.3 (0.6–7.4) | 3.5 (1.1–5.0) | 0.046 | 1.5 * |
| pH | 7.8 (7.2–9.0) | 8.3 (7.8–8.7) | <0.001 | 7.2 * |
| Total sperm number (×106/ejaculate) | 81.2 (4.3–896.0) | 132.1 (42.0–725.2) | 0.139 | 39 * |
| Sperm concentration (×106/mL) | 38.3 (2.4–280.0) | 44.8 (12.0–148.0) | 0.545 | 15 * |
| Total motility (%) | 62.0 (5.0–89.0) | 75.5 (55.0–88.0) | <0.001 | 40 * |
| Progressive motility (%) | 53.0 (3.0–69.0) | 64.5 (42.0–84.0) | <0.001 | 32 * |
| Immotile sperm (%) | 37.0 (11.0–95.0) | 24.5 (12.0–45.0) | <0.001 | N/A |
| Normal morphology (%) | 8.0 (0.0–29.0) | 14.0 (4.0–31.0) | 0.001 | 4 * |
| Head defects (%) | 79.0 (51.0–100.0) | 69.0 (48.0–91.0) | 0.003 | N/A |
| Mid-piece defects (%) | 4.0 (1.0–22.0) | 53.0 (33.0–74.0) | <0.001 | N/A |
| Tail defects (%) | 51.0 (20.0–89.0) | 21.0 (7.0–36.0) | <0.001 | N/A |
| Vitality (%) | 61.0 (34.0–82.0) | 86.5 (73.0–97.0) | <0.001 | 58 * |
| Peroxidase-positive cells (×106/mL) | 0.1 (0.0–1.0) | 0.0 (0.0–1.5) | 0.011 | <1 |
| Immature germ cells (×106/mL) | 0.56 (0.0–22.4) | 0.0 (0.0–2.29) | 0.005 | N/A |
| Fructose (µmol/ejaculate) | 42.2 (9.1–158.0) | 45.8 (9.8–116.6) | 0.462 | ≥13 |
| Glucosidase (mU/ejaculate) | 40.6 (4.1–242.0) | 40.4 (19.6–134.8) | 0.713 | ≥20 |
| Zinc (µmol/ejaculate) | 6.6 (1.3–40.8) | 10.3 (4.0–24.5) | 0.066 | ≥2.4 |
| Elastase (ng/mL) | 37 (10–1191) | 31.5 (10–415) | 0.674 | <250 |
| IL-8 (pg/mL) | 3503 (956–21,524) | 1679.5 (458–20,226) | 0.004 | N/A |
| CP/CPPS (%) (n = 41) | Control (%) (n = 22) | |||
|---|---|---|---|---|
| Median age in years (range) | 40 (22–62) | 29.5 (20–41) | ||
| Children | 0 | 41.5 | 86.4 | |
| 1 | 14.6 | 4.5 | ||
| 2 | 19.5 | 9.1 | ||
| ≥3 | 14.6 | 0 | ||
| no data | 9.8 | - | ||
| Currently trying to conceive | yes | 12.2 | 22.7 | |
| no | 41.5 | 77.3 | ||
| no data | 46.3 | - | ||
| ART | yes | 2.4 | 0 | |
| no | 43.9 | 100 | ||
| no data | 53.7 | - | ||
| Smoking | yes | 22.0 | 9.1 | |
| no | 68.3 | 90.9 | ||
| no data | 9.8 | - | ||
| Alcohol | yes | rarely | 14.6 | 31.8 |
| occasionally | 22 | 45.5 | ||
| frequently | 14.6 | 22.7 | ||
| no | 36.6 | 0 | ||
| no data | 12.2 | - | ||
| Drug use | yes | 2.4 | 9.1 | |
| no | 46.3 | 90.9 | ||
| no data | 51.2 | - | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berg, E.; Houska, P.; Nesheim, N.; Schuppe, H.-C.; Pilatz, A.; Fijak, M.; Manthey, M.; Steger, K.; Wagenlehner, F.; Schagdarsurengin, U. Chronic Prostatitis/Chronic Pelvic Pain Syndrome Leads to Impaired Semen Parameters, Increased Sperm DNA Fragmentation and Unfavorable Changes of Sperm Protamine mRNA Ratio. Int. J. Mol. Sci. 2021, 22, 7854. https://doi.org/10.3390/ijms22157854
Berg E, Houska P, Nesheim N, Schuppe H-C, Pilatz A, Fijak M, Manthey M, Steger K, Wagenlehner F, Schagdarsurengin U. Chronic Prostatitis/Chronic Pelvic Pain Syndrome Leads to Impaired Semen Parameters, Increased Sperm DNA Fragmentation and Unfavorable Changes of Sperm Protamine mRNA Ratio. International Journal of Molecular Sciences. 2021; 22(15):7854. https://doi.org/10.3390/ijms22157854
Chicago/Turabian StyleBerg, Elena, Petr Houska, Nils Nesheim, Hans-Christian Schuppe, Adrian Pilatz, Monika Fijak, Marc Manthey, Klaus Steger, Florian Wagenlehner, and Undraga Schagdarsurengin. 2021. "Chronic Prostatitis/Chronic Pelvic Pain Syndrome Leads to Impaired Semen Parameters, Increased Sperm DNA Fragmentation and Unfavorable Changes of Sperm Protamine mRNA Ratio" International Journal of Molecular Sciences 22, no. 15: 7854. https://doi.org/10.3390/ijms22157854
APA StyleBerg, E., Houska, P., Nesheim, N., Schuppe, H.-C., Pilatz, A., Fijak, M., Manthey, M., Steger, K., Wagenlehner, F., & Schagdarsurengin, U. (2021). Chronic Prostatitis/Chronic Pelvic Pain Syndrome Leads to Impaired Semen Parameters, Increased Sperm DNA Fragmentation and Unfavorable Changes of Sperm Protamine mRNA Ratio. International Journal of Molecular Sciences, 22(15), 7854. https://doi.org/10.3390/ijms22157854






