Cell Viability Assessment Using Fluorescence Vital Dyes and Confocal Microscopy in Evaluating Freezing and Thawing Protocols Used in Cryopreservation of Allogeneic Venous Grafts
Abstract
1. Introduction
2. Results
2.1. Immediate Post-Thaw Cell Viability
2.2. Evaluation of Changes of the Post-Thaw Cell Viability in Time
2.2.1. Slow Thawing Protocol
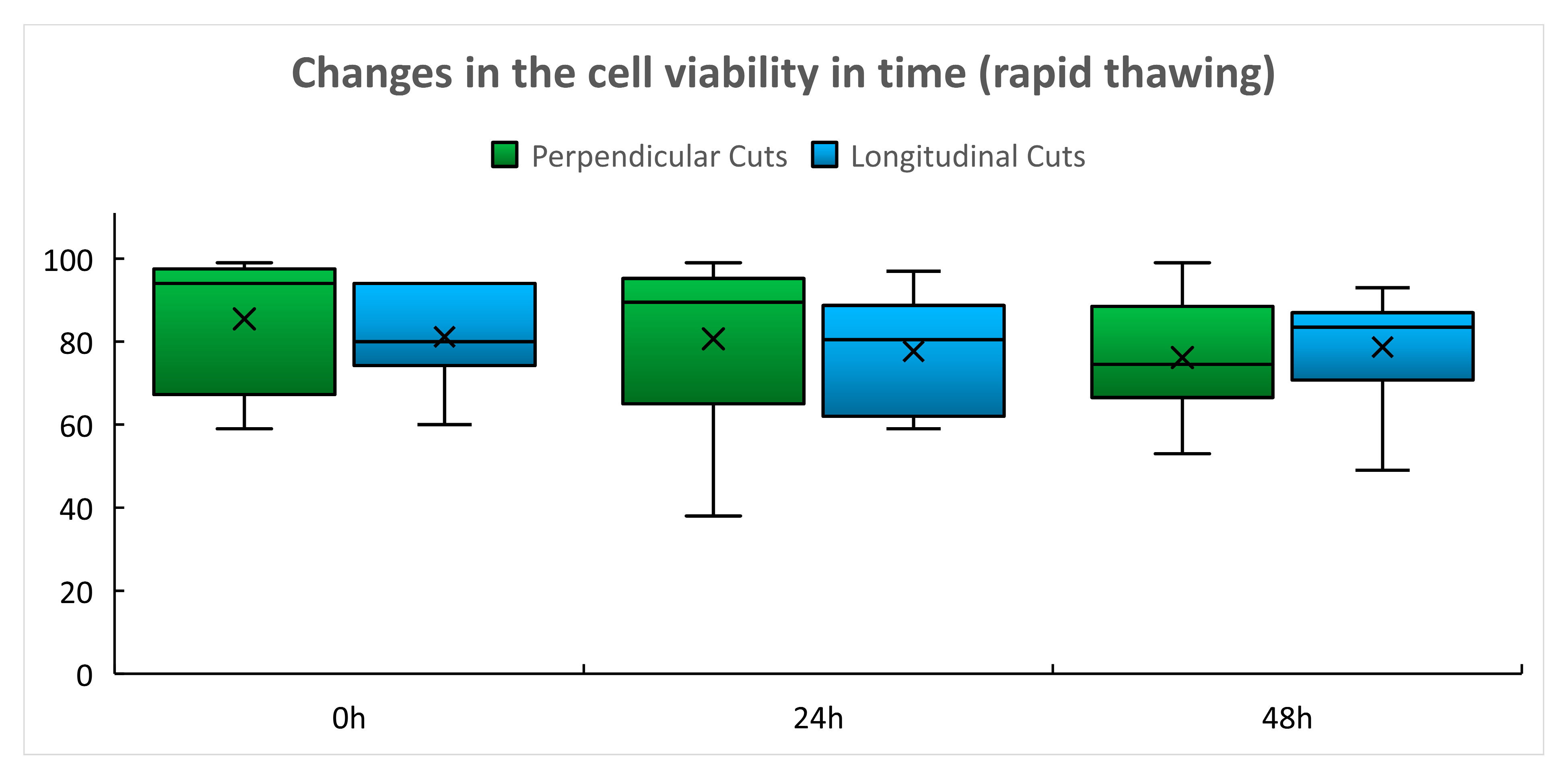
2.2.2. Rapid Thawing Protocol
3. Discussion
4. Methods
4.1. Vascular Tissue Harvest and Cryopreservation
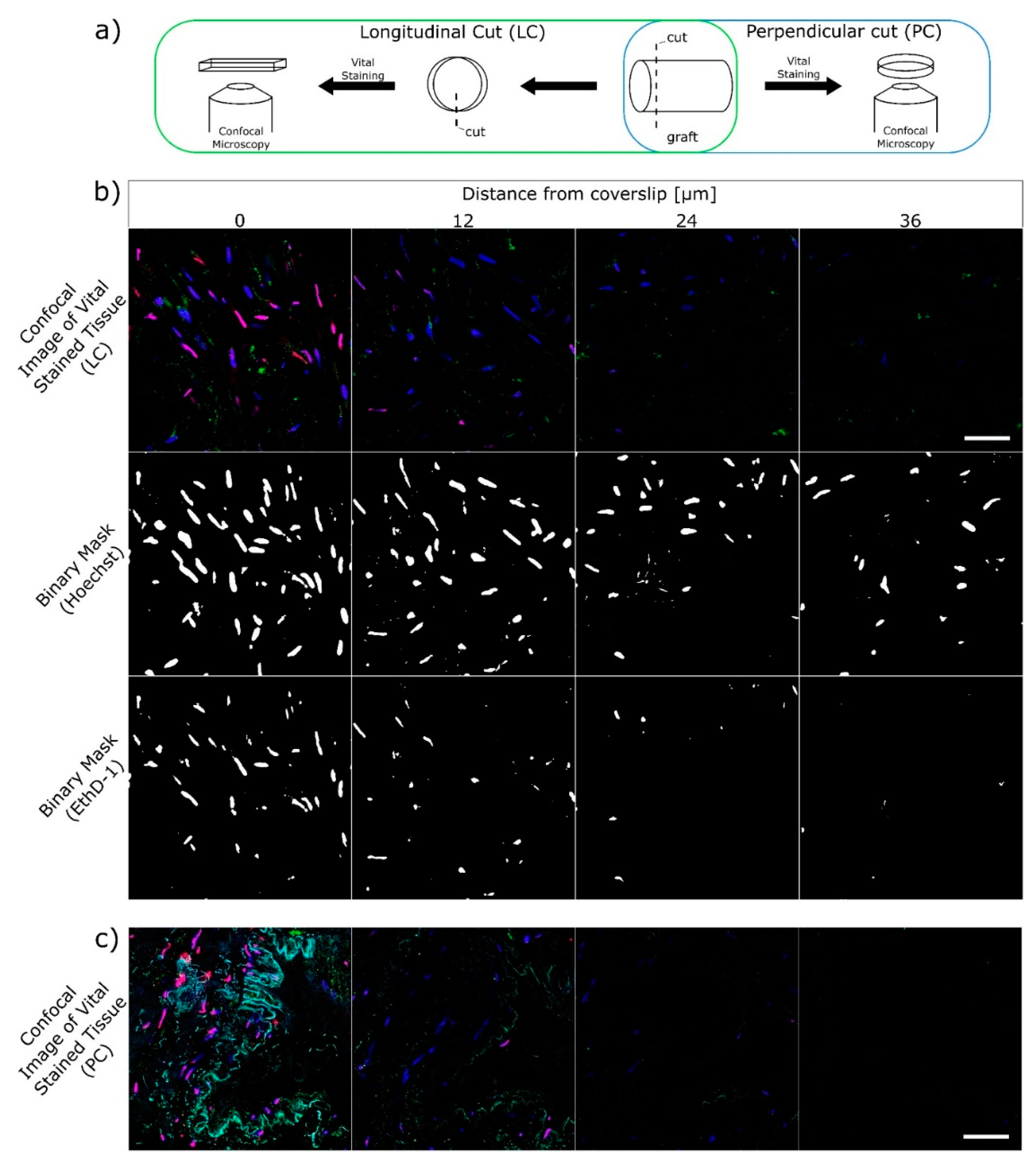
4.2. Processing of the Graft Samples for Viability Assays
- Substance Hoechst 33258 (blue in Figure 4b,c; Sigma Aldrich, St. Louis, MO, USA) Nuclear stain that permeates cells regardless of the membrane status. Excitation 405 nm, emission 420–475 nm.
- Acetoxymethyl calcein (green in Figure 4b,c; Thermo Fisher Scientific, Waltham, MA, USA). Proof of the enzymatic activity. Esterase turns acetoxymethyl calcein to calcein. Excitation 488 nm, emission 500–550 nm. In this study, the enzymatic activity was not evaluated.
- Ethidium homodimer (EthD-1, red in Figure 4b,c; Thermo Fisher Scientific, Waltham, MA, USA). Nuclear stain that permeates through damaged cell membranes, thus cells with EthD-1 stained nuclei were evaluated as non-viable. Excitation 561 nm, emission 585–650 nm.
4.3. Statistical Evaluation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Berz, D.; McCormack, E.M.; Winer, E.S.; Colvin, G.A.; Quesenberry, P.J. Cryopreservation of hematopoietic stem cells. Am. J. Hematol. 2007, 82, 463–472. [Google Scholar] [CrossRef]
- Baust, J.M.; Corwin, W.; Snyder, K.K.; Van Buskirk, R.; Baust, J.G. Cryopreservation: Evolution of Molecular Based Strategies. Adv. Exp. Med. Biol. 2016, 951, 13–29. [Google Scholar] [CrossRef]
- Cosentino, L.; Corwin, W.; Baust, J.; Diaz-Mayoral, N.; Cooley, H.; Shao, W.; van Buskirk, R. Preliminary Report: Evaluation of Storage Conditions and Cryococktails during Peripheral Blood Mononuclear Cell Cryopreservation. Cell Preserv. Technol. 2007, 5, 189–204. [Google Scholar] [CrossRef]
- Jandova, M.; Sponer, P.; Vokurkova, D.; Bauer, P.O.; Filipova, A.; Filip, S.; Mericka, P. New Cryopreservation Technology of hMSCs: First Preclinical Results Using DMSO-containing Medium. Cryoletters 2020, 41, 50–56. [Google Scholar]
- Johnson, S.; Rabinovitch, P.S. Ex Vivo Imaging of Excised Tissue Using Vital Dyes and Confocal Microscopy. Curr. Protoc. Cytom. 2012, 61, 9.39.1–9.39.18. [Google Scholar] [CrossRef] [PubMed]
- Baust, J.M.; Snyder, K.K.; VanBuskirk, R.G.; Baust, J.G. Changing Paradigms in Biopreservation. Biopreserv. Biobank. 2009, 7, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Baust, J.M.; Campbell, L.H.; Harbell, J. Best practices for cryopreserving, thawing, recovering, and assessing cells. In Vitro Cell. Dev. Biol.-Anim. 2017, 53, 855–871. [Google Scholar] [CrossRef]
- Baust, J.M.; Vogel, M.J.; Van Buskirk, R. A Molecular Basis of Cryopreservation Failure and Its Modulation to Improve Cell Survival. Cell Transplant. 2001, 10, 561–571. [Google Scholar] [CrossRef]
- Heng, B.C.; Clément, M.V.; Cao, T. Caspase Inhibitor Z-VAD-FMK Enhances the Freeze-Thaw Survival Rate of Human Embryonic Stem Cells. Biosci. Rep. 2007, 27, 257–264. [Google Scholar] [CrossRef]
- Savitskaya, M.A.; Onishchenko, G.E. Apoptosis in cryopreserved eukaryotic cells. Biochemistry 2016, 81, 445–452. [Google Scholar] [CrossRef]
- Searle, J.; Kerr, J.F.; Bishop, C.J. Necrosis and apoptosis: Distinct modes of cell death with fundamentally different significance. Pathol. Annu. 1982, 17, 229–259. [Google Scholar]
- Měřička, P.; Straková, H.; Lánská, M.; Vokurková, D.; Pecka, M.; Bláha, M.; Žák, P.; Jebavý, L. Testing of cryopreserved concentrates at infusion leads to standardization of engraftment in autologous blood progenitor cell transplantation. In Proceedings of the 23th IIR International Congress of Refrigeration, Prague, Czech Republic, 20–26 August 2011; Čermák, R., Ed.; Volume 23, p. 3609. [Google Scholar]
- Morgenstern, D.A.; Ahsan, G.; Brocklesby, M.; Ings, S.; Balsa, C.; Veys, P.; Brock, P.; Anderson, J.; Amrolia, P.; Goulden, N.; et al. Post-thaw viability of cryopreserved peripheral blood stem cells (PBSC) does not guarantee functional activity: Important implications for quality assurance of stem cell transplant programmes. Br. J. Haematol. 2016, 174, 942–951. [Google Scholar] [CrossRef]
- Wats, M.; Ings, S.; Balsa, C. Failure of cryopreserved peripheral blood stem cells to ensure engraftment resolved by functional assays but not by post-thaw viability. Cryoletters 2020, 41, 158–159. [Google Scholar]
- Schneider, M.; Stamm, C.; Brockbank, K.G.M.; Stock, U.A.; Seifert, M. The choice of cryopreservation method affects immune compatibility of human cardiovascular matrices. Sci. Rep. 2017, 7, 17027. [Google Scholar] [CrossRef]
- Matia, I.; Lodererova, A.; Adamec, M. Delayed administration of FK 506 is sufficient to suppress acute rejection changes after aortal transplantation in rats. Transpl. Int. 2007, 20, 371–380. [Google Scholar] [CrossRef]
- Jonas, S.; Matia, I.; Fellmer, P.; Splith, K.; Varga, M.; Adamec, M.; Kämmerer, I.; Feldbrügge, L.; Krenzien, F.; Hau, H.-M.; et al. Immunosuppressive protocol with delayed use of low-dose tacrolimus after aortic transplantation suppresses donor-specific anti-MHC class I and class II antibody production in rats. Ann. Transplant. 2014, 19, 225–232. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Spunda, R.; Hruby, J.; Mericka, P.; Mlcek, M.; Pecha, O.; Splith, K.; Schmelzle, M.; Krenzien, F.; Lindner, J.; Matia, I.; et al. Immunosuppressive protocols with tacrolimus after cryopreserved aortal allotransplantation in rats. PLoS ONE 2018, 13, e0201984. [Google Scholar] [CrossRef]
- Hruby, J.; Spunda, R.; Mericka, P.; Mlcek, M.; Pecha, O.; Splith, K.; Schmelzle, M.; Krenzien, F.; Lindner, J.; Spacek, M.; et al. Influence of the new standardized clinical cryopreservation/slow thawing protocol on immunogenicity of arterial allografts in rats. PLoS ONE 2020, 15, e0230234. [Google Scholar] [CrossRef] [PubMed]
- Spacek, M.; Měřička, P.; Janoušek, L.; Štádler, P.; Adamec, M.; Vlachovský, R.; Guňka, I.; Navrátil, P.; Thieme, F.; Špunda, R.; et al. Current vascular allograft procurement, cryopreservation and transplantation techniques in the Czech Republic. Adv. Clin. Exp. Med. 2019, 28, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.J.; Weegman, B.P.; Baicu, S.C.; Giwa, S.E. New Approaches to Cryopreservation of Cells, Tissues, and Organs. Transfus. Med. Hemother. 2019, 46, 197–215. [Google Scholar] [CrossRef] [PubMed]
- Pegg, D.E.; Wusteman, M.C.; Boylan, S. Fractures in Cryopreserved Elastic Arteries. Cryobiology 1997, 34, 183–192. [Google Scholar] [CrossRef]
- Hunt, C.; Song, Y.; Bateson, E.; Pegg, D. Fractures in Cryopreserved Arteries. Cryobiology 1994, 31, 506–515. [Google Scholar] [CrossRef]
- Novotny, R.; Slizova, D.; Hlubocký, J.; Krs, O.; Spatenka, J.; Burkert, J.; Fiala, R.; Mitas, P.; Mericka, P.; Spacek, M.; et al. Cryopreserved human aortic root allografts arterial wall: Structural changes occurring during thawing. PLoS ONE 2017, 12, e0175007. [Google Scholar] [CrossRef]
- Fellmer, P.T.; Matia, I.; Jonas, S. Arterielle Homografts in der Gefäßchirurgie—Idealer Gefäßersatz bei aortalen Gefäßprotheseninfektionen?! [Arterial allografts in vascular surgery—Best choice in cases of aortic graft infection?!]. Zent. Chir. 2013, 138, 530–535. [Google Scholar] [CrossRef]
- Hwang, S.; Bae, J.H.; Kim, I.-O.; Hong, J.-J. Current vascular allograft procurement, cryopreservation and transplantation techniques in the Asan Medical Center Tissue Bank. Ann. Liver Transplant. 2021, 1, 79–85. [Google Scholar] [CrossRef]
- Goffin, Y.A.; Van Hoeck, B.; Jashari, R.; Soots, G.; Kalmar, P. Banking of cryopreserved heart valves in Europe: Assessment of a 10-year operation in the European Homograft Bank (EHB). J. Heart Valve Dis. 2000, 9, 207–214. [Google Scholar]
- Jashari, R.; Van Hoeck, B.; Ngakam, R.; Goffin, Y.; Fan, Y. Banking of cryopreserved arterial allografts in Europe: 20 years of operation in the European Homograft Bank (EHB) in Brussels. Cell Tissue Bank. 2013, 14, 589–599. [Google Scholar] [CrossRef] [PubMed]
- Awan, M.; Buriak, I.; Fleck, R.; Fuller, B.; Goltsev, A.; Kerby, J.; Lowdell, M.; Mericka, P.; Petrenko, A.; Petrenko, Y.; et al. Dimethyl sulfoxide: A central player since the dawn of cryobiology, is efficacy balanced by toxicity? Regen. Med. 2020, 15, 1463–1491. [Google Scholar] [CrossRef] [PubMed]
- European Commission. EU Tissue and Cell Product Compendium. Available online: webgate.ec.europa.eu/eucoding/reports/te/index.xhtml (accessed on 8 April 2015).
- Měřička, P.; Špaček, M.; Janoušek, L.; Dvořáček, L.; Štádler, P.; Vlachovský, R.; Guňka, I.; Honegrová, B.; Brandejs, D.; Štěrba, L.; et al. Cryopreservation of vascular grafts for clinical use: Retrospective analysis of pre-freezing factors with potential impact on the quality and safety of vascular transplantations. Cryobiology 2015, 71, 546–547. [Google Scholar] [CrossRef]
- Van Kats, J.P.; Van Tricht, C.; Van Dijk, A.; Van Der Schans, M.; Bogaerdt, A.V.D.; Petit, P.L.; Bogers, A.J. Microbiological examination of donated human cardiac tissue in heart valve banking. Eur. J. Cardio-Thorac. Surg. 2010, 37, 163–169. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Špaček, M.; Měřička, P.; Janoušek, L.; Dalecká, M.; Benda, A.; Krs, O.; Slížová, D.; Špunda, R.; Hrubý, J.; Matia, I.; et al. Comparison of Different Thawing Protocols in Human Cryopreserved Venous Grafts. Ann. Vasc. Surg. 2020, 64, 347–354. [Google Scholar] [CrossRef] [PubMed]


| Slow Thawing-PC | Slow Thawing LC | Rapid Thawing PC | Rapid Thawing LC | |
|---|---|---|---|---|
| Mean | 87.70 | 74.5 | 85.5 | 81.2 |
| SD | 11.30 | 13.7 | 16.7 | 12.6 |
| Median | 91.03 | 79.0 | 94.0 | 80.0 |
| PC 24 h Culture | LC 24 h Culture | PC 48 h Culture * | LC 48 h Culture | |
|---|---|---|---|---|
| Mean | 90.0 | 83.3 | 56.7 | 75.5 |
| SD | 5.9 | 20.9 | 23.7 | 15.2 |
| Median | 92.0 | 93.5 | 53.0 | 81.0 |
| PC 24 h Culture | LC 24 h Culture | PC 48 h Culture | LC 48 h culture | |
|---|---|---|---|---|
| Mean | 80.7 | 77.7 | 76.2 | 78.7 |
| SD | 22.6 | 14.6 | 15.5 | 15.3 |
| Median | 89.5 | 80.5 | 74.5 | 83.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Měřička, P.; Janoušek, L.; Benda, A.; Lainková, R.; Sabó, J.; Dalecká, M.; Prokšová, P.; Salmay, M.; Špunda, R.; Pecha, O.; et al. Cell Viability Assessment Using Fluorescence Vital Dyes and Confocal Microscopy in Evaluating Freezing and Thawing Protocols Used in Cryopreservation of Allogeneic Venous Grafts. Int. J. Mol. Sci. 2021, 22, 10653. https://doi.org/10.3390/ijms221910653
Měřička P, Janoušek L, Benda A, Lainková R, Sabó J, Dalecká M, Prokšová P, Salmay M, Špunda R, Pecha O, et al. Cell Viability Assessment Using Fluorescence Vital Dyes and Confocal Microscopy in Evaluating Freezing and Thawing Protocols Used in Cryopreservation of Allogeneic Venous Grafts. International Journal of Molecular Sciences. 2021; 22(19):10653. https://doi.org/10.3390/ijms221910653
Chicago/Turabian StyleMěřička, Pavel, Libor Janoušek, Aleš Benda, Radka Lainková, Ján Sabó, Markéta Dalecká, Petra Prokšová, Myroslav Salmay, Rudolf Špunda, Ondřej Pecha, and et al. 2021. "Cell Viability Assessment Using Fluorescence Vital Dyes and Confocal Microscopy in Evaluating Freezing and Thawing Protocols Used in Cryopreservation of Allogeneic Venous Grafts" International Journal of Molecular Sciences 22, no. 19: 10653. https://doi.org/10.3390/ijms221910653
APA StyleMěřička, P., Janoušek, L., Benda, A., Lainková, R., Sabó, J., Dalecká, M., Prokšová, P., Salmay, M., Špunda, R., Pecha, O., Jandová, M., Gregor, J., Štěrba, L., Špaček, M., & Lindner, J. (2021). Cell Viability Assessment Using Fluorescence Vital Dyes and Confocal Microscopy in Evaluating Freezing and Thawing Protocols Used in Cryopreservation of Allogeneic Venous Grafts. International Journal of Molecular Sciences, 22(19), 10653. https://doi.org/10.3390/ijms221910653






