GPR55 Receptor Activation by the N-Acyl Dopamine Family Lipids Induces Apoptosis in Cancer Cells via the Nitric Oxide Synthase (nNOS) Over-Stimulation
Abstract
:1. Introduction
2. Results
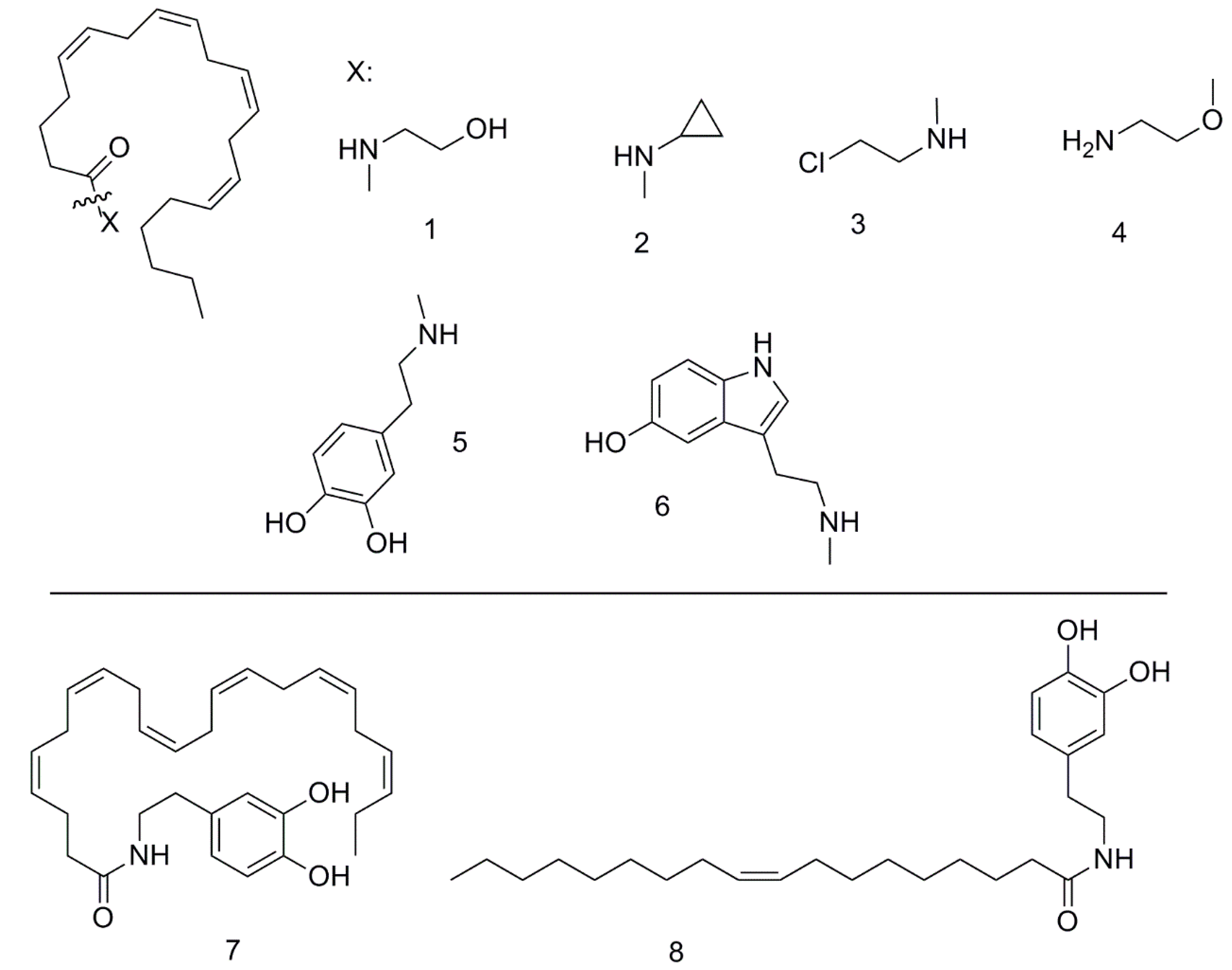
2.1. Chemical Synthesis of Fatty Acid Esters
2.2. Selection of the Most Active Fatty Acid Derivative Family in Cancer Cell Death Induction
2.3. DHA-DA, LPI and AA-EA Docking to the GPR55 Molecule
2.4. GPR55 Knockdown Effect on DHA-DA Cytotoxicity
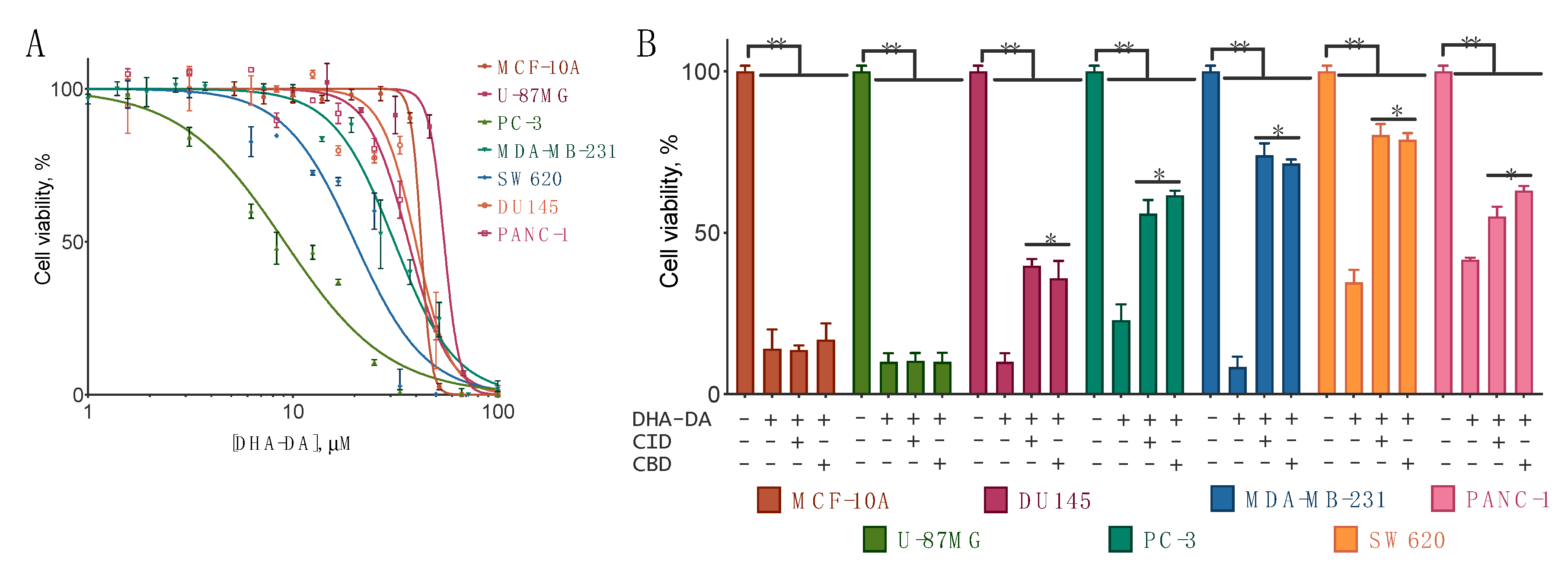
2.5. DHA-DA Cytotoxicity in the Cell Lines with the GPR55 Receptor
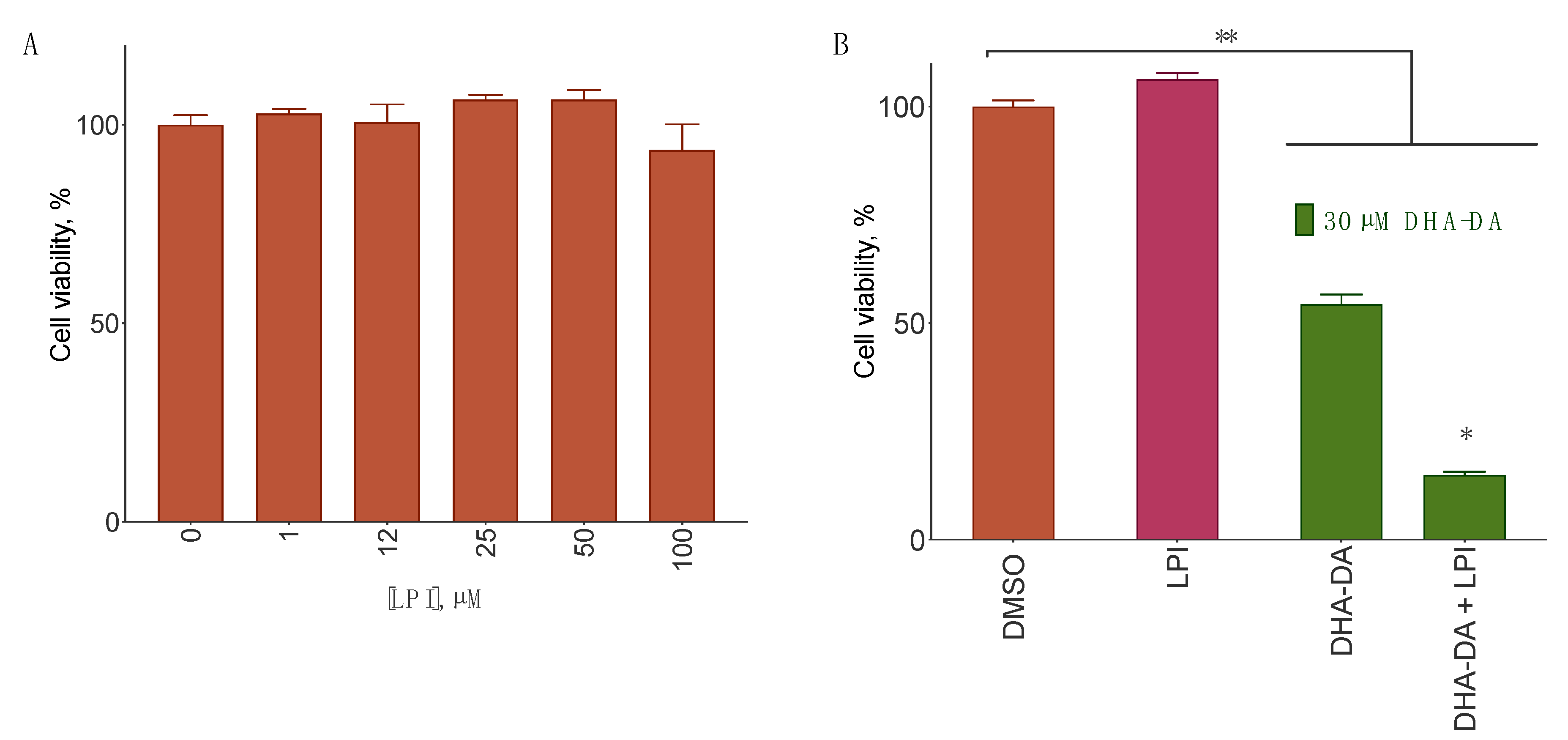
2.6. DHA-DA Interplay with LPI on Cancer Cells
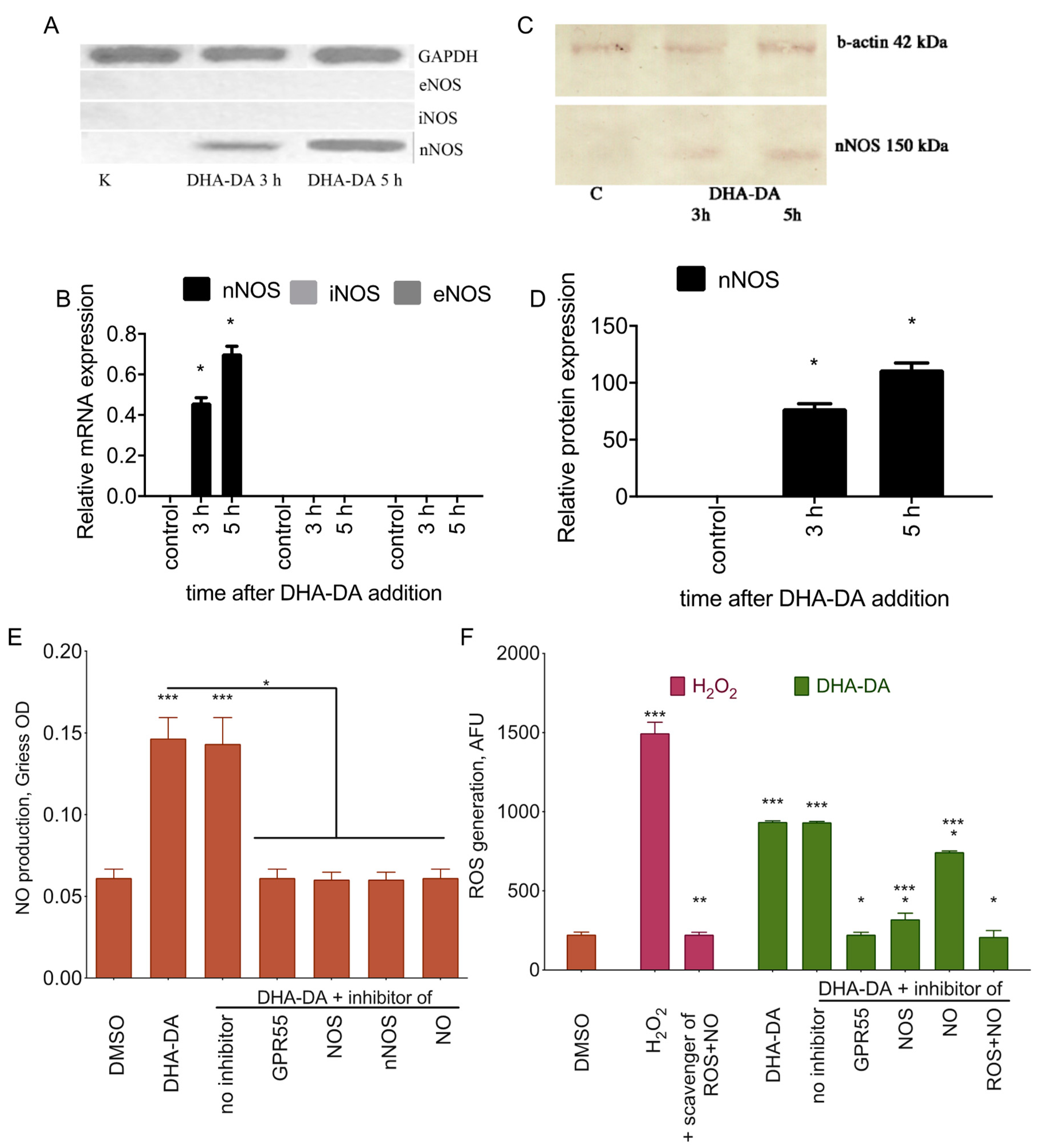
2.7. nNOS-Dependend ROS Production after the GPR55 Activation with DHA-DA during the Apoptosis Induction
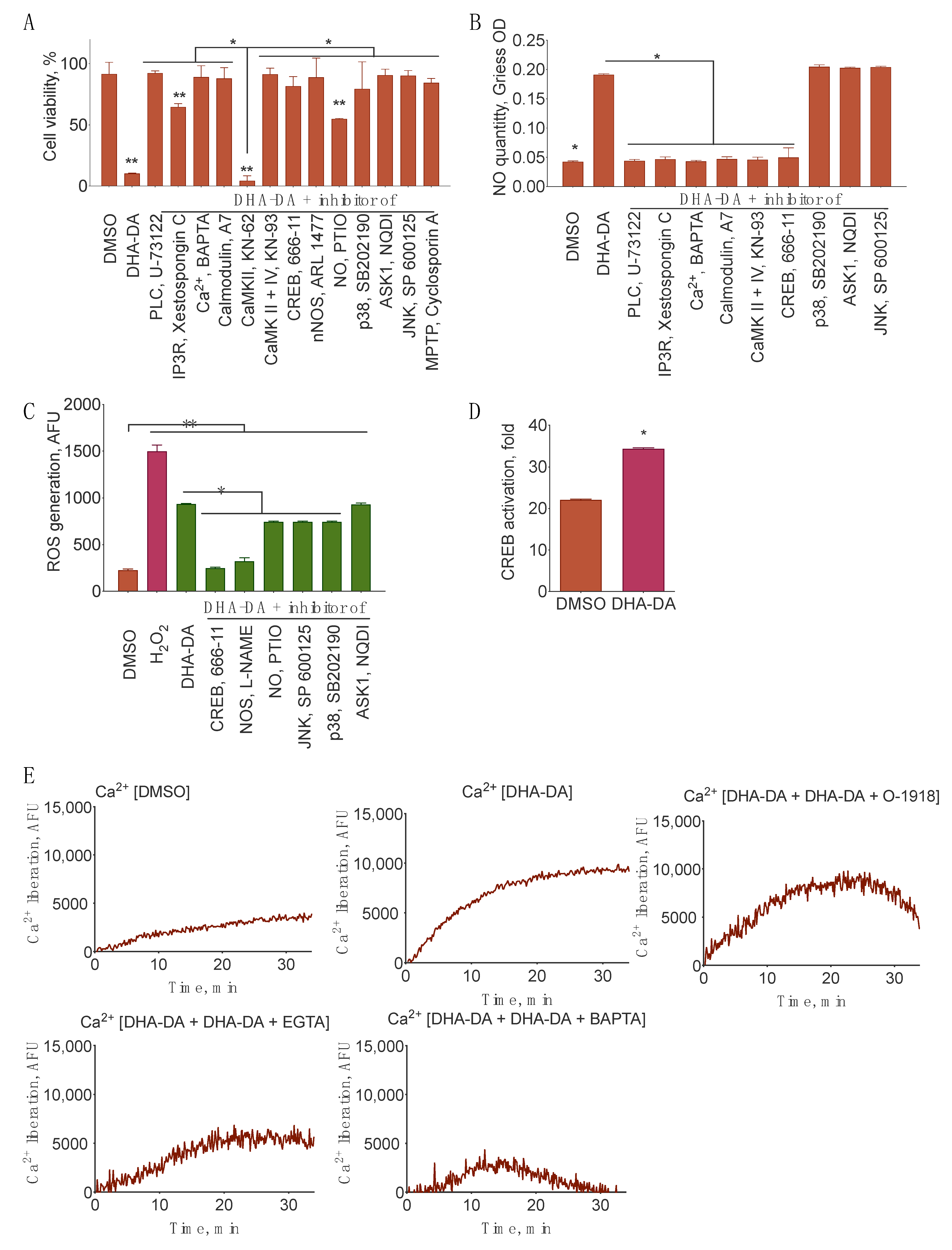
2.8. Signal Transduction from GPR55 to nNOS
3. Discussion
4. Materials and Methods
4.1. Reagents
4.2. Chemical Synthesis
4.3. Cell Culture
4.4. Cytotoxicity, NO, and ROS Generation
4.5. MTT Assay
4.6. ROS Assay
4.7. NO Production Assay
4.8. GPR55 Knockdown
4.9. RNA Isolation and RT-PCR
4.10. Western Blot
4.11. BCA Protein Assay
4.12. Calcium Measurements
4.13. CREB Activation Assay
4.14. Luciferase Activity Detection
4.15. Molecular Docking
4.16. Statistical Procedures
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AA-DA | N-arachidonoyl dopamine |
| OL-DA | N-oleoyl dopamine |
| DHA-DA | N-docosahexaenoyl dopamine |
| NADA | N-acyl dopamine |
| LPI | lysophosphatidylinositol |
| DHEA | N-docosahexaenoyl ethanolamine |
| EREA | N-eicosapentaenoyl ethanolamine |
| VRD | virodhamine |
| AA-CEA | arachidonyl-2′-chloroethylamide |
| AA-CPA | N-arachidonoyl cyclopropylamine |
| AA-5HT | N-arachidonoyl serotonin |
| NOS | NO synthase (i, inducible, e, endothelial, n, neuronal) |
| ROS | reactive oxygen species |
| FAAH | fatty acid amide hydrolase |
| CBD | cannabidiol |
| NADA | N-acyldopamines |
| BCIP | 5-Bromo-4-chloro-3-indolyl phosphate |
| NBT | nitro blue tetrazolium |
| BCA | bicinchoninic acid |
References
- Ross, R.A. The enigmatic pharmacology of GPR55. Trends Pharmacol. Sci. 2009, 30, 156–163. [Google Scholar] [CrossRef] [PubMed]
- DeMorrow, S.; Leyva-Illades, D. Orphan G protein receptor GPR55 as an emerging target in cancer therapy and management. Cancer Manag. Res. 2013, 5, 147. [Google Scholar] [CrossRef] [Green Version]
- Morales, P.; Jagerovic, N. Advances towards the discovery of GPR55 ligands. Curr. Med. Chem. 2016, 23, 2087–2100. [Google Scholar] [CrossRef] [PubMed]
- Piñeiro, R.; Maffucci, T.; Falasca, M. The putative cannabinoid receptor GPR55 defines a novel autocrine loop in cancer cell proliferation. Oncogene 2011, 30, 142–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotsikorou, E.; Madrigal, K.E.; Hurst, D.P.; Sharir, H.; Lynch, D.L.; Heynen-Genel, S.; Milan, L.B.; Chung, T.D.Y.; Seltzman, H.H.; Bai, Y.; et al. Identification of the GPR55 agonist binding site using a novel set of high-potency GPR55 selective ligands. Biochemistry 2011, 50, 5633–5647. [Google Scholar] [CrossRef] [Green Version]
- Singh, N.S.; Bernier, M.; Wainer, I.W. Selective GPR55 antagonism reduces chemoresistance in cancer cells. Pharmacol. Res. 2016, 111, 757–766. [Google Scholar] [CrossRef] [Green Version]
- Huang, L.; Ramirez, J.C.; Frampton, G.A.; Golden, L.E.; Quinn, M.A.; Pae, H.Y.; Horvat, D.; Liang, L.; DeMorrow, S. Anandamide exerts its antiproliferative actions on cholangiocarcinoma by activation of the GPR55 receptor. Lab. Investig. 2011, 91, 1007–1017. [Google Scholar] [CrossRef]
- Moreno, E.; Cavic, M.; Krivokuca, A.; Casadó, V.; Canela, E. The endocannabinoid system as a target in cancer diseases: Are we there yet? Front. Pharmacol. 2019, 10, 339. [Google Scholar] [CrossRef] [Green Version]
- Hart, S.; Fischer, O.M.; Ullrich, A. Cannabinoids induce cancer cell proliferation via tumor necrosis factor α-converting enzyme (TACE/ADAM17)-mediated transactivation of the epidermal growth factor receptor. Cancer Res. 2004, 64, 1943–1950. [Google Scholar] [CrossRef] [Green Version]
- Oka, S.; Nakajima, K.; Yamashita, A.; Kishimoto, S.; Sugiura, T. Identification of GPR55 as a Lysophosphatidylinositol receptor. Biochem. Biophys. Res. Commun. 2007, 362, 928–934. [Google Scholar] [CrossRef]
- Henstidge, C.M.; Balenga, N.A.B.; Ford, L.A.; Ross, R.A.; Waldhoer, M.; Irving, A.J. The GPR55 ligand L-α-lysophosphatidylinositol promotes RhoA-dependent Ca2+ signaling and NFAT activation. FASEB J. 2009, 23, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Kapur, A.; Zhao, P.; Sharir, H.; Bai, Y.; Caron, M.G.; Barak, L.S.; Abood, M.E. Atypical responsiveness of the orphan receptor GPR55 to cannabinoid ligands. J. Biol. Chem. 2009, 284, 29817–29827. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, S.M.; Bisogno, T.; Trevisani, M.; Al-Hayani, A.; De Petrocellis, L.; Fezza, F.; Tognetto, M.; Petros, T.J.; Krey, J.F.; Chu, C.J.; et al. An endogenous capsaicin-like substance with high potency at recombinant and native vanilloid VR1 receptors. Proc. Natl. Acad. Sci. USA 2002, 99, 8400–8405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bisogno, T.; Melck, D.; Bobrov, M.Y.; Gretskaya, N.M.; Bezuglov, V.V.; De Petrocellis, L.; Di Marzo, V. N-Acyl-Dopamines: Novel synthetic CB(1) cannabinoid-receptor ligands and inhibitors of anandamide inactivation with cannabimimetic activity in vitro and in vivo. Biochem. J. 2000, 351, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Navarrete, C.M.; Pérez, M.; de Vinuesa, A.G.; Collado, J.A.; Fiebich, B.L.; Calzado, M.A.; Muñoz, E. Endogenous N-Acyl-Dopamines induce COX-2 expression in brain endothelial cells by stabilizing MRNA through a P38 dependent pathway. Biochem. Pharmacol. 2010, 79, 1805–1814. [Google Scholar] [CrossRef]
- Costa, B.; Bettoni, I.; Petrosino, S.; Comelli, F.; Giagnoni, G.; Di Marzo, V. The dual fatty acid amide hydrolase/TRPV1 blocker, N-Arachidonoyl-Serotonin, relieves carrageenan-induced inflammation and hyperalgesia in mice. Pharmacol. Res. 2010, 61, 537–546. [Google Scholar] [CrossRef]
- Bezuglov, V.V.; Manevich, Y.; Archakov, A.V.; Bobrov, M.Y.; Kuklev, D.V.; Petrukhina, G.N.; Makarov, V.A.; Buznikov, G.A. Artificially functionalized polyenoic fatty acids as new lipid bioregulators. Russ. J. Bioorg. Chem. 1997, 23, 211–220. [Google Scholar]
- Tsuboi, K.; Uyama, T.; Okamoto, Y.; Ueda, N. Endocannabinoids and related N-Acylethanolamines: Biological activities and metabolism. Inflamm. Regen. 2018, 38, 28. [Google Scholar] [CrossRef]
- Witkamp, R. Fatty acids, endocannabinoids and inflammation. Eur. J. Pharmacol. 2016, 785, 96–107. [Google Scholar] [CrossRef]
- Meijerink, J.; Balvers, M.; Witkamp, R. N-Acyl amines of docosahexaenoic acid and other n-3 Polyunsatured fatty acids–From fishy endocannabinoids to potential leads. Br. J. Pharmacol. 2013, 169, 772–783. [Google Scholar] [CrossRef] [Green Version]
- Bisogno, T.; Melck, D.; De Petrocellis, L.; Bobrov, M.Y.; Gretskaya, N.M.; Bezuglov, V.V.; Sitachitta, N.; Gerwick, W.H.; Marzo, V.D. Arachidonoylserotonin and other novel inhibitors of fatty acid amide hydrolase. Biochem. Biophys. Res. Commun. 1998, 248, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Ramer, R.; Schwarz, R.; Hinz, B. Modulation of the endocannabinoid system as a potential anticancer strategy. Front. Pharmacol. 2019, 10, 430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akimov, M.G.; Gretskaya, N.M.; Zinchenko, G.N.; Bezuglov, V.V. Cytotoxicity of endogenous lipids N-Acyl dopamines and their possible metabolic derivatives for human cancer cell lines of different histological origin. Anticancer Res. 2015, 35, 2657–2661. [Google Scholar]
- Watson, J.E.; Kim, J.S.; Das, A. Emerging class of omega-3 fatty acid endocannabinoids & their derivatives. Prostaglandins Other Lipid Mediat. 2019, 143, 106337. [Google Scholar] [CrossRef] [PubMed]
- Rovito, D.; Giordano, C.; Plastina, P.; Barone, I.; De Amicis, F.; Mauro, L.; Rizza, P.; Lanzino, M.; Catalano, S.; Bonofiglio, D.; et al. Omega-3 DHA-and EPA-dopamine conjugates induce PPARγ-dependent breast cancer cell death through autophagy and apoptosis. Biochim. Biophys. Acta 2015, 1850, 2185–2195. [Google Scholar] [CrossRef] [PubMed]
- Rovito, D.; Giordano, C.; Vizza, D.; Plastina, P.; Barone, I.; Casaburi, I.; Lanzino, M.; De Amicis, F.; Sisci, D.; Mauro, L.; et al. Omega-3 PUFA Ethanolamides DHEA and EPEA induce autophagy through PPARγ activation in MCF-7 breast cancer cells. J. Cell. Physiol. 2013, 228, 1314–1322. [Google Scholar] [CrossRef] [PubMed]
- Brown, I.; Cascio, M.G.; Wahle, K.W.J.; Smoum, R.; Mechoulam, R.; Ross, R.A.; Pertwee, R.G.; Heys, S.D. Cannabinoid receptor-dependent and -independent anti-proliferative effects of omega-3 Ethanolamides in androgen receptor-positive and-negative prostate cancer cell lines. Carcinogenesis 2010, 31, 1584–1591. [Google Scholar] [CrossRef] [Green Version]
- de Bus, I.; Witkamp, R.; Zuilhof, H.; Albada, B.; Balvers, M. The role of N-3 PUFA-Derived fatty acid derivatives and their oxygenated metabolites in the modulation of inflammation. Prostaglandins Other Lipid Mediat. 2019, 144, 106351. [Google Scholar] [CrossRef]
- Akimov, M.G.; Ashba, A.M.; Gretskaya, N.M.; Bezuglov, V.V. N-Acyl Dopamines induce apoptosis in PC12 cell line via the GPR55 receptor activation. Dokl. Biochem. Biophys. 2017, 474, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Ashba, A.M.; Akimov, M.G.; Gretskaya, N.M.; Bezuglov, V.V. N-Acyl dopamines induce cell death in PC12 cell line via induction of nitric oxide generation and oxidative stress. Dokl. Biochem. Biophys. 2016, 467, 81–84. [Google Scholar] [CrossRef]
- Akimov, M.G.; Ashba, A.M.; Gretskaya, N.M.; Bezuglov, V.V. Some aspects of the mechanism of cell death induction by the lipids of N-Acyl dopamine family in the PC12 cancer cell line. Anticancer Res. 2014, 34, 5797–5800. [Google Scholar]
- Bau, C.; Middlemiss, P.J.; Hindley, S.; Jiang, S.; Ciccarelli, R.; Caciagli, F.; Diiorio, P.; Werstiuk, E.S.; Rathbone, M.P. Guanosine stimulates neurite outgrowth in PC12 cells via activation of heme oxygenase and cyclic GMP. Purinergic Signal. 2005, 1, 161–172. [Google Scholar] [CrossRef] [Green Version]
- Sheehy, A.M.; Phung, Y.T.; Riemer, R.K.; Black, S.M. Growth factor induction of nitric oxide synthase in rat pheochromocytoma cells. Mol. Brain Res. 1997, 52, 71–77. [Google Scholar] [CrossRef]
- Tamplenizza, M.; Lenardi, C.; Maffioli, E.; Nonnis, S.; Negri, A.; Forti, S.; Sogne, E.; De Astis, S.; Matteoli, M.; Schulte, C.; et al. Nitric oxide synthase mediates PC12 differentiation induced by the surface topography of nanostructured TiO2. J. Nanobiotechnology 2013, 11, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Visnyei, K.; Onodera, H.; Damoiseaux, R.; Saigusa, K.; Petrosyan, S.; De Vries, D.; Ferrari, D.; Saxe, J.; Panosyan, E.H.; Masterman-Smith, M.; et al. A molecular screening approach to identify and characterize inhibitors of glioblastoma stem cells. Mol. Cancer Ther. 2011, 10, 1818–1828. [Google Scholar] [CrossRef] [Green Version]
- Badolato, M.; Carullo, G.; Caroleo, M.C.; Cione, E.; Aiello, F.; Manetti, F. Discovery of 1,4-Naphthoquinones as a new class of antiproliferative agents targeting GPR55. ACS Med. Chem. Lett. 2019, 10, 402–406. [Google Scholar] [CrossRef]
- Tomko, A.; O’Leary, L.; Trask, H.; Achenbach, J.C.; Hall, S.R.; Goralski, K.B.; Ellis, L.D.; Dupré, D.J. Antitumor activity of abnormal cannabidiol and its analog O-1602 in Taxol-resistant preclinical models of breast cancer. Front. Pharmacol. 2019, 10, 1124. [Google Scholar] [CrossRef]
- Bernier, M.; Catazaro, J.; Singh, N.S.; Wnorowski, A.; Boguszewska-Czubara, A.; Jozwiak, K.; Powers, R.; Wainer, I.W. GPR55 Receptor antagonist decreases glycolytic activity in PANC-1 pancreatic cancer cell line and tumor xenografts: GPR55 receptor antagonist. Int. J. Cancer 2017, 141, 2131–2142. [Google Scholar] [CrossRef] [Green Version]
- Uhlen, M.; Fagerberg, L.; Hallstrom, B.M.; Lindskog, C.; Oksvold, P.; Mardinoglu, A.; Sivertsson, A.; Kampf, C.; Sjostedt, E.; Asplund, A.; et al. Tissue-Based map of the human proteome. Science 2015, 347, 1260419. [Google Scholar] [CrossRef]
- Ford, L.A.; Roelofs, A.J.; Anavi-Goffer, S.; Mowat, L.; Simpson, D.G.; Irving, A.J.; Rogers, M.J.; Rajnicek, A.M.; Ross, R.A. A role for L-Alpha-Lysophosphatidylinositol and GPR55 in the modulation of migration, orientation and polarization of human breast cancer cells. Br. J. Pharmacol. 2010, 160, 762–771. [Google Scholar] [CrossRef] [Green Version]
- Hasenoehrl, C.; Feuersinger, D.; Kienzl, M.; Schicho, R. GPR55-Mediated effects in colon cancer cell lines. Med. Cannabis Cannabinoids 2019, 2, 22–28. [Google Scholar] [CrossRef]
- Thomas, A.; Baillie, G.L.; Phillips, A.M.; Razdan, R.K.; Ross, R.A.; Pertwee, R.G. Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro: Cannabinoid antagonism by cannabidiol. Br. J. Pharmacol. 2007, 150, 613–623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costa, B.; Giagnoni, G.; Franke, C.; Trovato, A.E.; Colleoni, M. Vanilloid TRPV1 receptor mediates the Antihyperalgesic effect of the nonpsychoactive cannabinoid, cannabidiol, in a rat model of acute inflammation: Special report. Br. J. Pharmacol. 2004, 143, 247–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, A.J.; Castellano-Pellicena, I.; Haslam, C.P.; Nichols, P.L.; Dowell, S.J. Structure-Activity relationship of the GPR55 antagonist, CID16020046. Pharmacology 2018, 102, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Kargl, J.; Brown, A.J.; Andersen, L.; Dorn, G.; Schicho, R.; Waldhoer, M.; Heinemann, A. A selective antagonist reveals a potential role of G protein-coupled receptor 55 in platelet and endothelial cell function. J. Pharmacol. Exp. Ther. 2013, 346, 54–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomiyama, K.; Funada, M. Cytotoxicity of synthetic cannabinoids on primary neuronal cells of the forebrain: The involvement of cannabinoid CB1 receptors and apoptotic cell death. Toxicol. Appl. Pharmacol. 2014, 274, 17–23. [Google Scholar] [CrossRef]
- Bao, Z.; Dai, X.; Wang, P.; Tao, Y.; Chai, D. Capsaicin induces cytotoxicity in human osteosarcoma MG63 cells through TRPV1-dependent and-independent pathways. Cell Cycle 2019, 18, 1379–1392. [Google Scholar] [CrossRef]
- Redmond, W.J.; Cawston, E.E.; Grimsey, N.L.; Stuart, J.; Edington, A.R.; Glass, M.; Connor, M. Identification of N-Arachidonoyl dopamine as a highly biased ligand at cannabinoid CB1 receptors. Br. J. Pharmacol. 2016, 173, 115–127. [Google Scholar] [CrossRef] [Green Version]
- Trujillo, X.; Ortiz-Mesina, M.; Uribe, T.; Castro, E.; Montoya-Pérez, R.; Urzúa, Z.; Feria-Velasco, A.; Huerta, M. Capsaicin and N-Arachidonoyl-Dopamine (NADA) decrease tension by activating both cannabinoid and vanilloid receptors in fast skeletal muscle fibers of the frog. J. Membr. Biol. 2014, 248, 31–38. [Google Scholar] [CrossRef]
- Ito, K.; Nakazato, T.; Yamato, K.; Miyakawa, Y.; Yamada, T.; Hozumi, N.; Segawa, K.; Ikeda, Y.; Kizaki, M. Induction of apoptosis in leukemic cells by homovanillic acid derivative, capsaicin, through oxidative stress. Cancer Res. 2004, 64, 1071–1078. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.-Y.; Spector, A.A. N-Docosahexaenoylethanolamine: A neurotrophic and neuroprotective metabolite of docosahexaenoic acid. Mol. Asp. Med. 2018, 64, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Meijerink, J.; Poland, M.; Balvers, M.G.J.; Plastina, P.; Lute, C.; Dwarkasing, J.; van Norren, K.; Witkamp, R.F. Inhibition of COX-2-Mediated eicosanoid production plays a major role in the anti-inflammatory effects of the endocannabinoid N-Docosahexaenoylethanolamine (DHEA) in macrophages. Br. J. Pharmacol. 2015, 172, 24–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.; Plastina, P.; Vincken, J.-P.; Jansen, R.; Balvers, M.; ten Klooster, J.P.; Gruppen, H.; Witkamp, R.; Meijerink, J. N-Docosahexaenoyl dopamine, an endocannabinoid-like conjugate of dopamine and the n-3 fatty acid docosahexaenoic acid, attenuates lipopolysaccharide-induced activation of microglia and macrophages via COX-2. ACS Chem. Neurosci. 2017, 8, 548–557. [Google Scholar] [CrossRef] [PubMed]
- Meijerink, J.; Plastina, P.; Vincken, J.-P.; Poland, M.; Attya, M.; Balvers, M.; Gruppen, H.; Gabriele, B.; Witkamp, R.F. The Ethanolamide metabolite of DHA, Docosahexaenoylethanolamine, shows immunomodulating effects in mouse peritoneal and RAW264.7 macrophages: Evidence for a new link between fish oil and inflammation. Br. J. Nutr. 2011, 105, 1798–1807. [Google Scholar] [CrossRef] [Green Version]
- Poland, M.; Ten Klooster, J.P.; Wang, Z.; Pieters, R.; Boekschoten, M.; Witkamp, R.; Meijerink, J. Docosahexaenoyl serotonin, an endogenously formed n-3 fatty acid-serotonin conjugate has anti-inflammatory properties by attenuating IL-23-IL-17 signaling in macrophages. Biochim. Biophys. Acta 2016, 1861, 2020–2028. [Google Scholar] [CrossRef]
- Förstermann, U.; Sessa, W.C. Nitric oxide synthases: Regulation and function. Eur. Heart J. 2012, 33, 829–837. [Google Scholar] [CrossRef] [Green Version]
- Capettini, L.S.A.; Cortes, S.F.; Gomes, M.A.; Silva, G.A.B.; Pesquero, J.L.; Lopes, M.J.; Teixeira, M.M.; Lemos, V.S. Neuronal nitric oxide synthase-derived hydrogen peroxide is a major endothelium-dependent relaxing factor. Am. J. Physiol.-Heart Circ. Physiol. 2008, 295, H2503–H2511. [Google Scholar] [CrossRef] [Green Version]
- Noronha-Dutra, A.A.; Epperlein, M.M.; Woolf, N. Reaction of nitric oxide with hydrogen peroxide to produce potentially cytotoxic singlet oxygen as a model for nitric oxide-mediated killing. FEBS Lett. 1993, 321, 59–62. [Google Scholar] [CrossRef] [Green Version]
- Falasca, M.; Ferro, R. Role of the Lysophosphatidylinositol/GPR55 axis in cancer. Adv. Biol. Regul. 2016, 60, 88–93. [Google Scholar] [CrossRef]
- Deliu, E.; Sperow, M.; Console-Bram, L.; Carter, R.L.; Tilley, D.G.; Kalamarides, D.J.; Kirby, L.G.; Brailoiu, G.C.; Brailoiu, E.; Benamar, K.; et al. The Lysophosphatidylinositol receptor GPR55 modulates pain perception in the periaqueductal gray. Mol. Pharmacol. 2015, 88, 265–272. [Google Scholar] [CrossRef] [Green Version]
- Xu, W.; Liu, L.Z.; Loizidou, M.; Ahmed, M.; Charles, I.G. The role of nitric oxide in cancer. Cell Res. 2002, 12, 311–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laezza, C.; Pagano, C.; Navarra, G.; Pastorino, O.; Proto, M.C.; Fiore, D.; Piscopo, C.; Gazzerro, P.; Bifulco, M. The endocannabinoid system: A target for cancer treatment. Int. J. Mol. Sci. 2020, 21, 747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, S.S.-J.; Bradshaw, H.B.; Benton, V.M.; Chen, J.S.-C.; Huang, S.M.; Minassi, A.; Bisogno, T.; Masuda, K.; Tan, B.; Roskoski, R.; et al. The biosynthesis of N-Arachidonoyl dopamine (NADA), a putative endocannabinoid and endovanilloid, via conjugation of arachidonic acid with dopamine. Prostaglandins Leukot. Essent. Fat. Acids 2009, 81, 291–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akimov, M.G.; Gretskaya, N.M.; Shevchenko, K.V.; Shevchenko, V.P.; Myasoedov, N.F.; Bobrov, M.Y.; Bezuglov, V.V. New aspects of biosynthesis and metabolism of N-Acyldopamines in rat tissues. Russ. J. Bioorg. Chem. 2007, 33, 602–606. [Google Scholar] [CrossRef] [PubMed]
- Hauer, D.; Schelling, G.; Gola, H.; Campolongo, P.; Morath, J.; Roozendaal, B.; Hamuni, G.; Karabatsiakis, A.; Atsak, P.; Vogeser, M.; et al. Plasma concentrations of endocannabinoids and related primary fatty acid amides in patients with post-traumatic stress disorder. PLoS ONE 2013, 8, e62741. [Google Scholar] [CrossRef] [Green Version]
- Chu, C.J.; Huang, S.M.; De Petrocellis, L.; Bisogno, T.; Ewing, S.A.; Miller, J.D.; Zipkin, R.E.; Daddario, N.; Appendino, G.; Di Marzo, V.; et al. N-Oleoyldopamine, a novel endogenous capsaicin-like lipid that produces hyperalgesia. J. Biol. Chem. 2003, 278, 13633–13639. [Google Scholar] [CrossRef] [Green Version]
- Devane, W.; Hanus, L.; Breuer, A.; Pertwee, R.; Stevenson, L.; Griffin, G.; Gibson, D.; Mandelbaum, A.; Etinger, A.; Mechoulam, R. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 1992, 258, 1946–1949. [Google Scholar] [CrossRef]
- Hillard, C.J.; Manna, S.; Greenberg, M.J.; Dicamelli, R.; Ross, R.A.; Stevenson, L.A.; Murphy, V.; Pertwee, R.G.; Campbell, W.B. Synthesis and characterization of potent and selective agonists of the neuronal cannabinoid receptor (CB1). J. Pharmacol. Exp. Ther. 1999, 289, 1427–1433. [Google Scholar]
- Bezuglov, V.; Bobrov, M.; Gretskaya, N.; Gonchar, A.; Zinchenko, G.; Melck, D.; Bisogno, T.; Di Marzo, V.; Kuklev, D.; Rossi, J.-C.; et al. Synthesis and biological evaluation of novel amides of polyunsaturated fatty acids with dopamine. Bioorg. Med. Chem. Lett. 2001, 11, 447–449. [Google Scholar] [CrossRef]
- Bezuglov, V.V.; Archakov, A.V.; Bobrov, M.Y.; Kogteva, G.S.; Manevich, E.M. Serotoninamide of arachidonic acid as an irreversible inhibitor of soybean 15-Lipoxydase. Russ. J. Bioorg. Chem. 1996, 23, 211–220. [Google Scholar]
- Markey, S.P.; Dudding, T.; Wang, T.C.L. Base-and acid-catalyzed interconversions of O-Acyl-and N-Acyl-Ethanolamines: A cautionary note for lipid analyses. J. Lipid Res. 2000, 41, 657–662. [Google Scholar]
- Ottria, R.; Casati, S.; Ciuffreda, P. Optimized synthesis and characterization of N-Acylethanolamines and O-Acylethanolamines, important family of lipid-signalling molecules. Chem. Phys. Lipids 2012, 165, 705–711. [Google Scholar] [CrossRef]
- van de Loosdrecht, A.A.; Beelen, R.H.J.; Ossenkoppele, G.J.; Broekhoven, M.G.; Langenhuijsen, M.M.A.C. A Tetrazolium-Based colorimetric MTT assay to quantitate human monocyte mediated cytotoxicity against leukemic cells from cell lines and patients with Acute Myeloid Leukemia. J. Immunol. Methods 1994, 174, 311–320. [Google Scholar] [CrossRef]
- Akimov, M.G.; Fomina-Ageeva, E.V.; Bezuglov, V.V. Optimization of the procedure of nitrogen oxide quantitation in mammalian cell culture media. Russ. J. Bioorg. Chem. 2015, 41, 63–69. [Google Scholar] [CrossRef]
- Obara, Y.; Ueno, S.; Yanagihata, Y.; Nakahata, N. Lysophosphatidylinositol causes neurite retraction via GPR55, G13 and RhoA in PC12 Cells. PLoS ONE 2011, 6, e24284. [Google Scholar] [CrossRef] [Green Version]
- Ye, J.; Coulouris, G.; Zaretskaya, I.; Cutcutache, I.; Rozen, S.; Madden, T.L. Primer-BLAST: A tool to design target-specific primers for polymerase chain reaction. BMC Bioinform. 2012, 13, 134. [Google Scholar] [CrossRef] [Green Version]
- Smith, P.K.; Krohn, R.I.; Hermanson, G.T.; Mallia, A.K.; Gartner, F.H.; Provenzano, M.D.; Fujimoto, E.K.; Goeke, N.M.; Olson, B.J.; Klenk, D.C. Measurement of protein using bicinchoninic acid. Anal. Biochem. 1985, 150, 76–85. [Google Scholar] [CrossRef]
- O’Boyle, N.M.; Banck, M.; James, C.A.; Morley, C.; Vandermeersch, T.; Hutchison, G.R. Open Babel: An open chemical toolbox. J. Cheminform. 2011, 3, 33. [Google Scholar] [CrossRef] [Green Version]
- Trott, O.; Olson, A.J. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 2010, 31, 455–461. [Google Scholar] [CrossRef] [Green Version]
- Maslova, V.D.; Reshetnikov, R.V.; Bezuglov, V.V.; Lyubimov, I.I.; Golovin, A.V. Supercomputer Simulations of dopamine-derived ligands complexed with cyclooxygenases. Supercomput. Front. Innov. 2018, 5, 98–102. [Google Scholar] [CrossRef]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-Learn: Machine learning in {P}ython. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
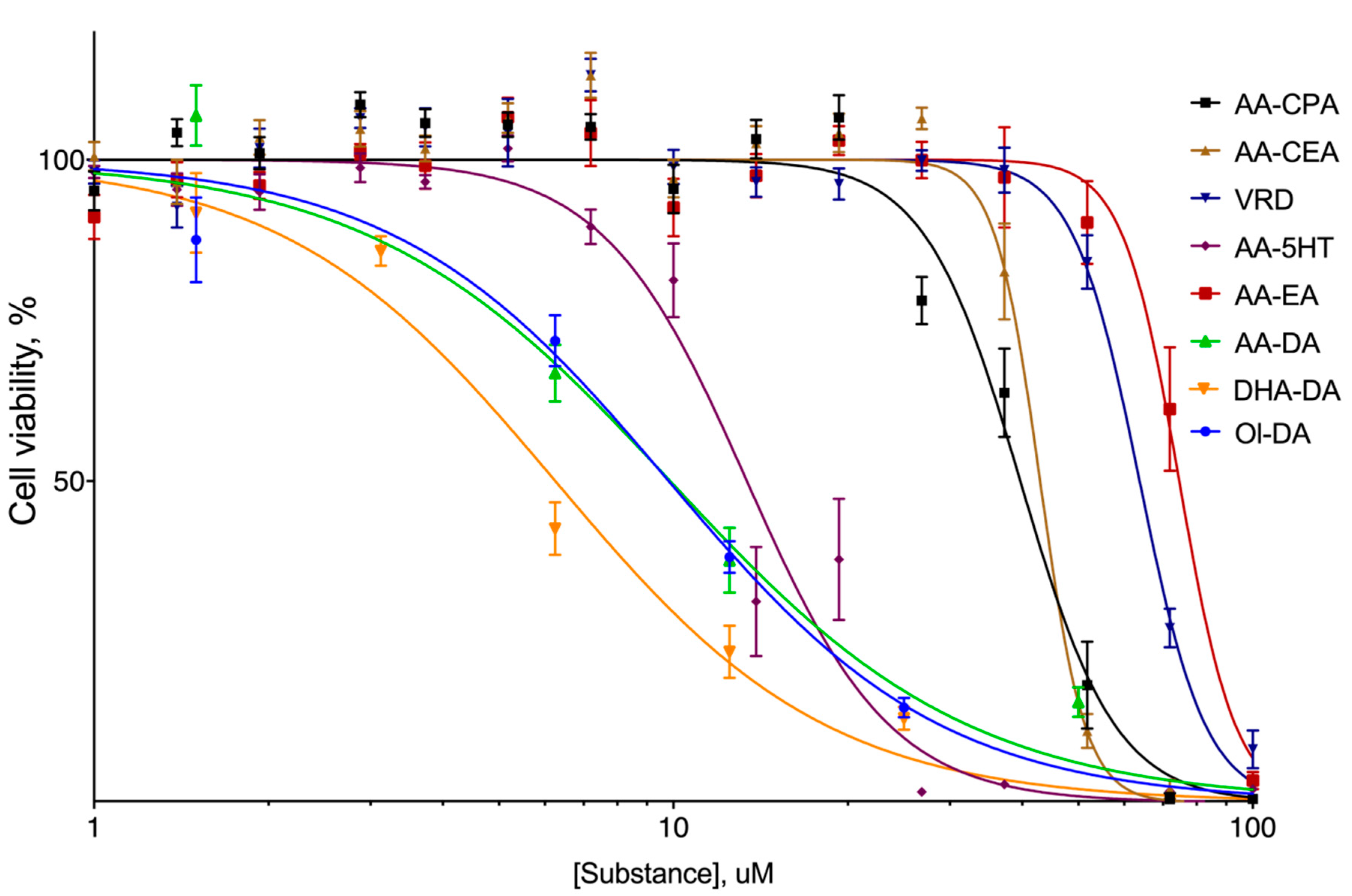



| AA-CEA | AA-CPA | VRD | AA-EA | AA-5HT | DHA-DA | Ol-DA | AA-DA | |
|---|---|---|---|---|---|---|---|---|
| μM, M. (95% Confidence Interval) | ||||||||
| EC50 | 36 (37.93 to 41.50) | 40 (41.49 to 44.42) | 67 (61.88 to 65.72) | 80 (71.14 to 78.15) | 14 (12.53 to 14.33) | 6 (5.434 to 7.224) | 10 (8.635 to 11.05) | 10 (8.035 to 12.46) |
| DHA-DA | AA-EA | LPI | |||
|---|---|---|---|---|---|
| Cluster | Dock Score, kcal/M | Cluster | Dock Score, kcal/M | Cluster | Dock Score, kcal/M |
| Mean ± S.E. | Mean ± S.E. | Mean ± S.E. | |||
| 3 | −8.77 ± 0.03 | 1 | −6.61 ± 0.02 | 3 | −7.76 ± 0.04 |
| 1 | −7.56 ± 0.02 | 3 | −6.6 ± 0.03 | 1 | −7.02 ± 0.03 |
| 5 | −7.37 ± 0.02 | 4 | −6.51 ± 0.02 | 4 | −6.88 ± 0.03 |
| 4 | −7.33 ± 0.04 | 5 | −6.36 ± 0.03 | 5 | −6.82 ± 0.03 |
| 2 | −7.26 ± 0.04 | 2 | −5.8 ± 0.05 | 2 | −6.29 ± 0.03 |
| Cell Line | DHA-DA Cytotoxicity EC50, μM M. (95% C.I.) | DHA-DA Toxicity Change with GPR55 Blockers, Change in % of Cell Viability M. ± S.E. |
|---|---|---|
| MCF-10A | 42 (39.67 to 43.23) | 0 |
| U-87MG | 56 (54.21 to 58.02) | 0 |
| DU145 | 38 (36.20 to 43.39) | +30 ± 2 |
| PC-3 | 9 (8.075 to 10.23) | +32 ± 1 |
| MDA-MB-231 | 30 (29.45 to 33.11) | +70 ± 2 |
| SW620 | 22 (17.79 to 22.59) | +41 ± 1 |
| PANC-1 | 36 (34.90 to 38.51) | +22 ± 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akimov, M.G.; Gamisonia, A.M.; Dudina, P.V.; Gretskaya, N.M.; Gaydaryova, A.A.; Kuznetsov, A.S.; Zinchenko, G.N.; Bezuglov, V.V. GPR55 Receptor Activation by the N-Acyl Dopamine Family Lipids Induces Apoptosis in Cancer Cells via the Nitric Oxide Synthase (nNOS) Over-Stimulation. Int. J. Mol. Sci. 2021, 22, 622. https://doi.org/10.3390/ijms22020622
Akimov MG, Gamisonia AM, Dudina PV, Gretskaya NM, Gaydaryova AA, Kuznetsov AS, Zinchenko GN, Bezuglov VV. GPR55 Receptor Activation by the N-Acyl Dopamine Family Lipids Induces Apoptosis in Cancer Cells via the Nitric Oxide Synthase (nNOS) Over-Stimulation. International Journal of Molecular Sciences. 2021; 22(2):622. https://doi.org/10.3390/ijms22020622
Chicago/Turabian StyleAkimov, Mikhail G., Alina M. Gamisonia, Polina V. Dudina, Natalia M. Gretskaya, Anastasia A. Gaydaryova, Andrey S. Kuznetsov, Galina N. Zinchenko, and Vladimir V. Bezuglov. 2021. "GPR55 Receptor Activation by the N-Acyl Dopamine Family Lipids Induces Apoptosis in Cancer Cells via the Nitric Oxide Synthase (nNOS) Over-Stimulation" International Journal of Molecular Sciences 22, no. 2: 622. https://doi.org/10.3390/ijms22020622
APA StyleAkimov, M. G., Gamisonia, A. M., Dudina, P. V., Gretskaya, N. M., Gaydaryova, A. A., Kuznetsov, A. S., Zinchenko, G. N., & Bezuglov, V. V. (2021). GPR55 Receptor Activation by the N-Acyl Dopamine Family Lipids Induces Apoptosis in Cancer Cells via the Nitric Oxide Synthase (nNOS) Over-Stimulation. International Journal of Molecular Sciences, 22(2), 622. https://doi.org/10.3390/ijms22020622






