Evaluation of the Influence of Adalimumab on the Expression Profile of Leptin-Related Genes and Proteins in Keratinocytes Treated with Lipopolysaccharide A
Abstract
:1. Introduction
2. Results
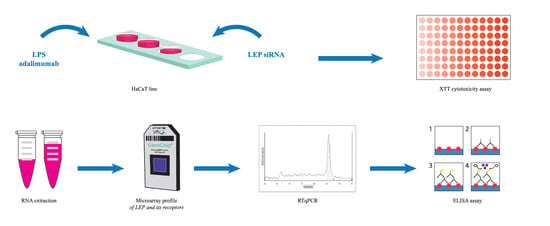
2.1. LPS and Adalimumab XTT Cytotoxicity Assay
2.2. Assessment of Caspases-3, -8 and -9 Activity in the HaCaT Cell Line Treated with Adalimumab after Inducing Inflammation by LPS
2.3. Expression Profile of Leptin-Related Genes in HaCaT Culture Exposed to LPS, LPS and Adalimumab and in a Control Culture as Determined by Microarray, RTqPCR
2.4. The Level of Leptin (Protein) in Keratinocytes Exposed to LPS, and Adalimumab in Comparison with the Control Culture
2.5. RNA Interference Analysis
3. Discussion
4. Materials and Methods
4.1. Cell Culture
4.2. XTT Cytotoxicity Assay
4.3. Caspases-3, 8, and -9 Activity
4.4. RNA Extraction
4.5. Microarray Profile of Leptin-Related Genes
- Synthesis of double-stranded cDNA on the matrix of the ribonucleic extracts.
- Adding the poly-A control and First Strand Master Mix to the total RNA, and next incubating it for 2 h at 42 °C.
- Adding the Second Strand Master Mix to the reaction mixture and next incubating it for 1 h at 16 °C and next for 10 min at 65 °C.
- Synthesis of biotinyl mRNA and incubation for 16 h at 40 °C.
- Labeling mRNA with biotin and purifying,
- Hybridization of mRNA specimens with microarray probes.
- Reading of the hybridization signal and data analysis.
4.6. Real-Time Quantitative Reverse Transcription Reaction
4.7. Changes in the Concentration of Leptin
4.8. RNA Interference
4.9. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| RTqPCR | Real-time quantitative reverse transcription reaction |
| RNA | Ribonucleic acid |
| LPS | Lipopolysaccharide A |
| STAT | Signal transducer and activator of transcription |
| TNF-α | Tumor necrosis factor alfa |
| XTT | (2,3-Bis-(2-Methoxy-4-Nitro-5-Sulfophenyl)-2H-Tetrazolium-5-Carboxanilide) |
| ELISA | Enzyme-linked immunoassay |
| siRNA | Small interfering RNA |
| ACTB | β-actin |
| LEPROT | Leptin overlapping transcript |
| LEPROTL1 | Leptin receptor overlapping transcript-like 1 |
| LEPR | Leptin receptor |
| LEP | Leptin |
| MAPK | mitogen-activated protein kinase |
| IMQ | Imiquimod |
References
- Sáinz, N.; Barrenetxe, J.; Moreno-Aliaga, M.J.; Martínez, J.A. Leptin resistance and diet-induced obesity: Central and peripheral actions of leptin. Metabolism 2015, 64, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Park, H.-K.; Ahima, R.S. Physiology of leptin: Energy homeostasis, neuroendocrine function and metabolism. Metabolism 2015, 64, 24–34. [Google Scholar] [CrossRef] [Green Version]
- Münzberg, H.; Morrison, C.D. Structure, production and signaling of leptin. Metabolism 2015, 64, 13–23. [Google Scholar] [CrossRef] [Green Version]
- Crujeiras, A.B.; Carreira, M.C.; Cabia, B.; Andrade, S.; Amil, M.; Casanueva, F.F. Leptin resistance in obesity: An epigenetic landscape. Life Sci. 2015, 140, 57–63. [Google Scholar] [CrossRef]
- Izquierdo, A.G.; Crujeiras, A.B.; Casanueva, F.F.; Carreira, M.C. Leptin, obesity, and leptin resistance: Where are we 25 years later? Nutrients 2019, 11, 2704. [Google Scholar] [CrossRef] [Green Version]
- Perego, L.; Pizzocri, P.; Corradi, D.; Maisano, F.; Paganelli, M.; Fiorina, P.; Barbieri, M.; Morabito, A.; Paolisso, G.; Folli, F.; et al. Circulating leptin correlates with left ventricular mass in morbid (grade III) obesity before and after weight loss induced by bariatric surgery: A potential role for leptin in mediating human left ventricular hypertrophy. J. Clin. Endocrinol. Metab. 2005, 90, 4087–4093. [Google Scholar] [CrossRef]
- Poetsch, M.S.; Strano, A.; Guan, K. Role of Leptin in Cardiovascular Diseases. Front Endocrinol. 2020, 11, 354. [Google Scholar] [CrossRef]
- Han, T.J.; Xu, H.Z.; Li, J.S.; Geng, L.Y.; Li, X.Y.; Zhou, X.X.; Wang, X. Leptin and its receptor in glucose metabolism of T cell lymphoma. Oncol. Lett. 2018, 16, 5838–5846. [Google Scholar] [CrossRef] [PubMed]
- Martín-González, J.; Pérez-Pérez, A.; Cabanillas-Balsera, D.; Vilariño-García, T.; Sánchez-Margalet, V.; Segura-Egea, J.J. Leptin stimulates DMP-1 and DSPP expression in human dental pulp via MAPK 1/3 and PI3K signaling pathways. Arch. Oral Biol. 2019, 98, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Yang, L.; Zeng, Z.; Feng, Y.; Wang, X.; Wu, X.; Luo, H.; Zhang, J.; Pakvasa, M.; Wagstaff, W.; et al. Leptin potentiates BMP9-induced osteogenic differentiation of mesenchymal stem cells through the activation of JAK/STAT signaling. Stem Cells Dev. 2020, 29, 498–510. [Google Scholar] [CrossRef] [PubMed]
- Cortese, L.; Terrazzano, G.; Pelagalli, A. Leptin and immunological profile in obesity and its associated diseases in dogs. Int. J. Mol. Sci. 2019, 20, 2392. [Google Scholar] [CrossRef] [Green Version]
- Zheng, H.; Zhang, X.; Castillo, E.F.; Luo, Y.; Liu, M.; Yang, X.O. Leptin enhances TH2 and ILC2 responses in allergic airway disease. J. Biol. Chem. 2016, 291, 22043–22052. [Google Scholar] [CrossRef] [Green Version]
- Kong, Y.; Zhang, S.; Wu, R.; Su, X.; Peng, D.; Zhao, M.; Su, Y. New insights into different adipokines in linking the pathophysiology of obesity and psoriasis. Lipids Health Dis. 2019, 18, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.; Krueger, J.G. Highly effective new treatments for psoriasis target the IL-23/Type 17 T cell auto-immune axis. Annu. Rev. Med. 2017, 68, 255–269. [Google Scholar] [CrossRef]
- Hamminga, E.A.; Van Der Lely, A.J.; Neumann, H.A.; Thio, H.B. Chronic inflammation in psoriasis and obesity: Implication for therapy. Med. Hypotheses 2006, 67, 768–773. [Google Scholar] [CrossRef]
- Cerman, A.A.; Bozkurt, S.; Sav, A.; Tulunay, A.; Elbaşı, M.O.; Ergun, T. Serum leptin levels, skin leptin and leptin receptor expression in psoriasis. Br. J. Dermatol. 2008, 159, 820–826. [Google Scholar] [CrossRef]
- Chen, J.; Xie, Z.; Bin, Z. The Association Between Serum Leptin Levels and Cardiovascular Events in Pa-tients with Rheumatoid Arthritis. Lab. Med. 2021, 52, 86–92. [Google Scholar] [CrossRef]
- Szepietowski, J.; Adamski, Z.; Chodorowska, G.; Kaszuba, A.; Placek, W.; Rudnicka, L.; Reich, A. Leczenie łuszczycy-rekomendacje ekspertów Polskiego Towarzystwa Dermatologicznego. Część II: Łuszczyca umiarkowana do ciężkiej. Dermatol. Rev. 2014, 101, 455–472. [Google Scholar] [CrossRef]
- Adwent, I.; Grabarek, B.O.; Kojs-Mrożkiewicz, M.; Brus, R.; Staszkiewicz, R.; Plewka, A.; Stasiowski, M.; Lyssek-Boroń, A. The Influence of Adalimumab and Cyclosporine A on the Expression Profile of the Genes Related to TGFβ Signaling Pathways in Keratinocyte Cells Treated with Lipopolysaccharide A. Mediat. Inflamm. 2020, 2020, 3821279. [Google Scholar] [CrossRef]
- Malakou, L.S.; Gargalionis, A.N.; Piperi, C.; Papadavid, E.; Papavassiliou, A.G.; Basdra, E.K. Molecular mechanisms of mechanotransduction in psoriasis. J. Transl. Med. 2018, 6, 1–11. [Google Scholar] [CrossRef]
- Tan, Y.; Qi, Q.; Lu, C.; Niu, X.; Bai, Y.; Jiang, C.; Wang, Y.; Zhou, Y.; Lu, A.; Xiao, C. Cytokine imbalance as a common mechanism in both psoriasis and rheumatoid arthritis. Mediat. Inflamm. 2017, 2017, 2405291. [Google Scholar] [CrossRef]
- Wolk, K.; Sabat, R. Adipokines in psoriasis: An important link between skin inflammation and metabolic alterations. Rev. Endocr. Metab. Disord. 2016, 17, 305–317. [Google Scholar] [CrossRef]
- Rajappa, M.; Rathika, S.; Munisamy, M.; Chandrashekar, L.; Thappa, D.M. Effect of treatment with methotrexate and coal tar on adipokine levels and indices of insulin resistance and sensitivity in patients with psoriasis vulgaris. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Robati, R.M.; Partovi-Kia, M.; Haghighatkhah, H.R.; Younespour, S.; Abdollahimajd, F. Increased serum leptin and resistin levels and increased carotid intima-media wall thickness in patients with psoriasis: Is psoriasis associated with atherosclerosis? J. Am. Acad. Dermatol. 2014, 71, 642–648. [Google Scholar] [CrossRef]
- Ehsani, A.H.; Mortazavi, H.; Balighi, K.; Hosseini, M.S.; Azizpour, A.; Hejazi, S.P.; Goodarzi, A.; Darvari, S.B. Changes in body mass index and lipid profile in psoriatic patients after treatment with standard protocol of infliximab. Acta Med. Iran. 2016, 54, 570–575. [Google Scholar] [PubMed]
- Hwang, J.; Yoo, J.A.; Yoon, H.; Han, T.; Yoon, J.; An, S.; Cho, J.Y.; Lee, J. The Role of Leptin in the Association between Obesity and Psoriasis. Biomol. Ther. 2021, 29, 11–21. [Google Scholar] [CrossRef]
- Kumthekar, A.; Ogdie, A. Obesity and Psoriatic Arthritis: A Narrative Review. Rheumatol. Ther. 2020, 7, 447–456. [Google Scholar] [CrossRef]
- Baran, A.; Flisiak, I.; Jaroszewicz, J.; Swiderska, M. Serum adiponectin and leptin levels in psoriatic patients according to topical treatment. J. Dermatol. Treat. 2015, 26, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.H.; Lin, C.F.; Alalaiwe, A.; Yang, S.C.; Fang, J.Y. Apoptotic or antiproliferative activity of natural products against keratinocytes for the treatment of psoriasis. Int. J. Mol. Sci. 2019, 20, 2558. [Google Scholar] [CrossRef] [Green Version]
- Baliwag, J.; Barnes, D.H.; Johnston, A. Cytokines in psoriasis. Cytokine 2015, 73, 342–350. [Google Scholar] [CrossRef] [Green Version]
- Ogawa, E.; Sato, Y.; Minagawa, A.; Okuyama, R. Pathogenesis of psoriasis and development of treatment. J. Dermatol. 2018, 45, 264–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schön, M.P.; Erpenbeck, L. The interleukin-23/interleukin-17 axis links adaptive and innate immunity in psoriasis. Front. Immunol. 2018, 9, 1323. [Google Scholar] [CrossRef] [Green Version]
- Julien, O.; Wells, J.A. Caspases and their substrates. Cell Death Differ. 2017, 24, 1380. [Google Scholar] [CrossRef] [PubMed]
- McArthur, K.; Kile, B.T. Apoptotic caspases: Multiple or mistaken identities? Trends Cell Biol. 2018, 28, 475–493. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Liu, S.; Wang, Y.; Dai, W.; Zou, H.; Wang, S.; Zhang, J.; Pan, J. Salinomycin effectively eliminates cancer stem-like cells and obviates hepatic metastasis in uveal melanoma. Mol. Cancer 2019, 18, 159. [Google Scholar] [CrossRef]
- Kaźmierczuk, A.; Kiliańska, Z.M. Rola białek szoku cieplnego w apoptozie komórek. Role of heat shock proteins in cell apoptosis. Post. Hig Med. Dosw 2010, 64, 273–283. [Google Scholar]
- Shen, C.; Van Assche, G.; Rutgeerts, P.; Ceuppens, J.L. Caspase activation and apoptosis induction by adalimumab: Demonstration in vitro and in vivo in a chimeric mouse model. Inflamm. Bowel Dis. 2006, 12, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Paula, Á.C.D.; Ávila, M.P.D.; Isaac, D.L.C.; Salustiano, R.; Lima, A.P.D.; Mello, F.M.; Pereira, F.D.; Silva, P.H.; Lacerda, E.D.P.S. Cytotoxicity and genotoxicity of intravitreal adalimumab administration in rabbit retinal cells. Arq. Bras. Oftalmol. 2015, 78, 89–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wcisło-Dziadecka, D.; Simka, K.; Kaźmierczak, A.; Kruszniewska-Rajs, C.; Gola, J.; Grabarek, B.; Hybiak, J.; Grillon, C.; Mazurek, U.; Łos, M.J. Psoriasis treatment changes the expression profile of selected caspases and their regulatory MicroRNAs. Cell Physiol. Biochem. 2018, 50, 525–537. [Google Scholar] [CrossRef]
- Grabarek, B.; Wcislo-Dziadecka, D.; Gola, J.; Kruszniewska-Rajs, C.; Brzezinska-Wcislo, L.; Zmarzly, N.; Mazurek, U. Changes in the expression profile of Jak/Stat signaling pathway genes and miRNAs regulating their expression under the adalimumab therapy. Curr. Pharm. Biotech. 2018, 19, 556–565. [Google Scholar] [CrossRef]
- Reinartz, J.; Bechtel, M.J.; Kramer, M.D. Tumor necrosis factor-alpha-induced apoptosis in a human keratinocyte cell line (HaCaT) is counteracted by transforming growth factor-alpha. Exp. Cell Res. 1996, 228, 334–340. [Google Scholar] [CrossRef]
- Udommethaporn, S.; Tencomnao, T.; McGowan, E.M.; Boonyaratanakornkit, V. Assessment of anti-TNF-α activities in keratinocytes expressing inducible TNF-α: A novel tool for anti-TNF-α drug screening. PLoS ONE 2016, 11, e0159151. [Google Scholar] [CrossRef]
- Gojniczek, K.; Jurzak, M.; Boryka, M.; Garncarczyk, A. Keratosis of the epidermis as an effect of keratinocyte proliferation, differentiation and apoptosis. Pol. J. Cosmetol. 2007, 10, 146–155. [Google Scholar]
- Lee, M.; Lee, E.; Jin, S.H.; Ahn, S.; Kim, S.O.; Kim, J.; Choi, D.; Lim, K.-M.; Lee, S.-T.; Noh, M. Leptin regulates the pro-inflammatory response in human epidermal keratinocytes. Arch. Dermatol. Res. 2018, 310, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Stjernholm, T.; Ommen, P.; Langkilde, A.; Johansen, C.; Iversen, L.; Rosada, C.; Stenderup, K. Leptin deficiency in mice counteracts imiquimod (IMQ)-induced psoriasis-like skin inflammation while leptin stimulation induces inflammation in human keratinocytes. Exp. Dermatol. 2017, 26, 338–345. [Google Scholar] [CrossRef]
- Emílio-Silva, M.T.; Rodrigues, V.P.; Bueno, G.; Ohara, R.; Martins, M.G.; Horta-Júnior, J.A.; Branco, L.G.; Rocha, L.R.; Hiruma-Lima, C.A. Hypothermic Effect of Acute Citral Treatment during LPS-induced Systemic Inflammation in Obese Mice: Reduction of Serum TNF-α and Leptin Levels. Biomolecules 2020, 10, 1454. [Google Scholar] [CrossRef] [PubMed]
- Brunet, M.; Van Gelder, T.; Åsberg, A.; Haufroid, V.; Hesselink, D.A.; Langman, L.; Lemaitre, F.; Marquet, P.; Seger, C.; Shipkova, M.; et al. Therapeutic drug monitoring of tacrolimus-personalized therapy: Second consensus report. Ther. Drug Monit. 2019, 41, 261–307. [Google Scholar] [CrossRef]
- Cordeiro, R.C.; Chaves Filho, A.J.M.; Gomes, N.S.; Tomaz, V.D.S.; Medeiros, C.D.; Queiroz, A.I.D.G.; Maes, M.; Macedo, D.S.; Carvalho, A.F. Leptin prevents lipopolysaccharide-induced depressive-like behaviors in mice: Involvement of dopamine receptors. Front. Psychiatry 2019, 10, 125. [Google Scholar] [CrossRef]
- Hernández, J.L.; López-Mejías, R.; Blanco, R.; Pina, T.; Ruiz, S.; Sierra, I.; Corrales, A. Association of trabecular bone score with inflammation and adiposity in patients with psoriasis: Effect of adalimumab therapy. J. Osteoporos. 2016, 2016, 5747852. [Google Scholar] [CrossRef]
- Kyriakou, A.; Patsatsi, A.; Sotiriadis, D.; Goulis, D.G. Effects of treatment for psoriasis on circulating levels of leptin, adiponectin and resistin: A systematic review and meta-analysis. Br. J. Dermatol. 2018, 179, 273–281. [Google Scholar] [CrossRef]
- Türkeş, C. Investigation of potential paraoxonase-I inhibitors by kinetic and molecular docking studies: Chemotherapeutic drugs. Protein Pept. Lett. 2019, 26, 392–402. [Google Scholar] [CrossRef] [PubMed]
- Voloshyna, I.; Mounessa, J.; Carsons, S.E.; Reiss, A.B. Effect of inhibition of interleukin-12/23 by ustekinumab on the expression of leptin and leptin receptor in human THP-1 macrophages. Clin. Exp. Dermatol. 2016, 41, 308–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chuang, S.Y.; Lin, C.H.; Sung, C.T.; Fang, J.Y. Murine models of psoriasis and their usefulness for drug discovery. Expert Opin. Drug Discov. 2018, 13, 551–562. [Google Scholar] [CrossRef]
- Bocheńska, K.; Smolińska, E.; Moskot, M.; Jakóbkiewicz-Banecka, J.; Gabig-Cimińska, M. Models in the research process of psoriasis. Int. J. Mol. Sci. 2017, 18, 2514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Souza Xavier Costa, N.; Ribeiro Júnior, G.; dos Santos Alemany, A.A.; Belotti, L.; Zati, D.H.; Frota Cavalcante, M.; Matera Veras, M.; Ribeiro, S.; Kallás, E.G.; Nascimento Saldiva, P.H.; et al. Early and late pulmonary effects of nebulized LPS in mice: An acute lung injury model. PLoS ONE 2017, 12, e0185474. [Google Scholar] [CrossRef] [Green Version]





| mRNA | ID | Microarray | RTqPCR | ||||||
|---|---|---|---|---|---|---|---|---|---|
| LPS | LPS + Adalimumab | LPS | LPS + Adalimumab | ||||||
| H-8 vs. C | H-2 vs. C | H-8 vs. C | H-24 vs. C | H-8 vs. C | H-2 vs. C | H-8 vs. C | H-24 vs. C | ||
| LEP | 207092_at | +8.77 a | −2.96 b | −3.98 b | −3.01 b | +7.74 a | −2.41 b | −3.49 b | −3.55 b |
| LEPROT | 202377_at 202378_s_at | +6.08 a | −2.14 b | −2.18 b | −2.54 b | +6.14 a | −2.36 b | −2.41 b | −1.98 b |
| LEPROTL1 | 202594_at 202595_s_at | +5.01 a | +2.36 b | −1.98 b | −2.04 b | +5.89 a | +2.14 b | −2.03 b | −2.43 b |
| LEPR | 209894_at 209959_at 211167_s_at 211354_s_at 211355_x_at 211356_x_at | +4.18 a | −3.55 b | −3.10 b | −2.11 b | +4.22 a | −3.64 b | −2.74 b | −1.56 b |
| mRNA | Nucleotide Sequence |
|---|---|
| LEP | Forward 5′-GAAGACCACATCCACACACG-3′ Reverse 5′-AGCTCAGCCAGACCCATCTA-3′ |
| LEPROT | Forward 5′-GCTTGGAGAGGCAGATAACG-3′ Reverse ′-AATGTCCTGGGTCCAGAGTG-3′ |
| LEPROTL1 | Forward 5′-TGCAATGTGGGAAGAAATGA-3′ Reverse 5′-AAGGAGGAAGCAGAGGAAGG-3′ |
| LEPR | Forward 5′-ACAGTCCCTTTGTGGGTCAG-3′ Reverse 5′-TATCCGAGCTCCAGCGTACT-3′ |
| ACTB | Forward 5′-TCACCCACACTGTGCCCATCTACGA-3′ Reverse 5′-CAGCGGAACCGCTCATTGCCAATGG-3′ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grabarek, B.O.; Kasela, T.; Adwent, I.; Zawidlak-Węgrzyńska, B.; Brus, R. Evaluation of the Influence of Adalimumab on the Expression Profile of Leptin-Related Genes and Proteins in Keratinocytes Treated with Lipopolysaccharide A. Int. J. Mol. Sci. 2021, 22, 1595. https://doi.org/10.3390/ijms22041595
Grabarek BO, Kasela T, Adwent I, Zawidlak-Węgrzyńska B, Brus R. Evaluation of the Influence of Adalimumab on the Expression Profile of Leptin-Related Genes and Proteins in Keratinocytes Treated with Lipopolysaccharide A. International Journal of Molecular Sciences. 2021; 22(4):1595. https://doi.org/10.3390/ijms22041595
Chicago/Turabian StyleGrabarek, Beniamin Oskar, Tomasz Kasela, Iwona Adwent, Barbara Zawidlak-Węgrzyńska, and Ryszard Brus. 2021. "Evaluation of the Influence of Adalimumab on the Expression Profile of Leptin-Related Genes and Proteins in Keratinocytes Treated with Lipopolysaccharide A" International Journal of Molecular Sciences 22, no. 4: 1595. https://doi.org/10.3390/ijms22041595
APA StyleGrabarek, B. O., Kasela, T., Adwent, I., Zawidlak-Węgrzyńska, B., & Brus, R. (2021). Evaluation of the Influence of Adalimumab on the Expression Profile of Leptin-Related Genes and Proteins in Keratinocytes Treated with Lipopolysaccharide A. International Journal of Molecular Sciences, 22(4), 1595. https://doi.org/10.3390/ijms22041595