Plasminogen Receptors and Fibrinolysis
Abstract
1. Introduction
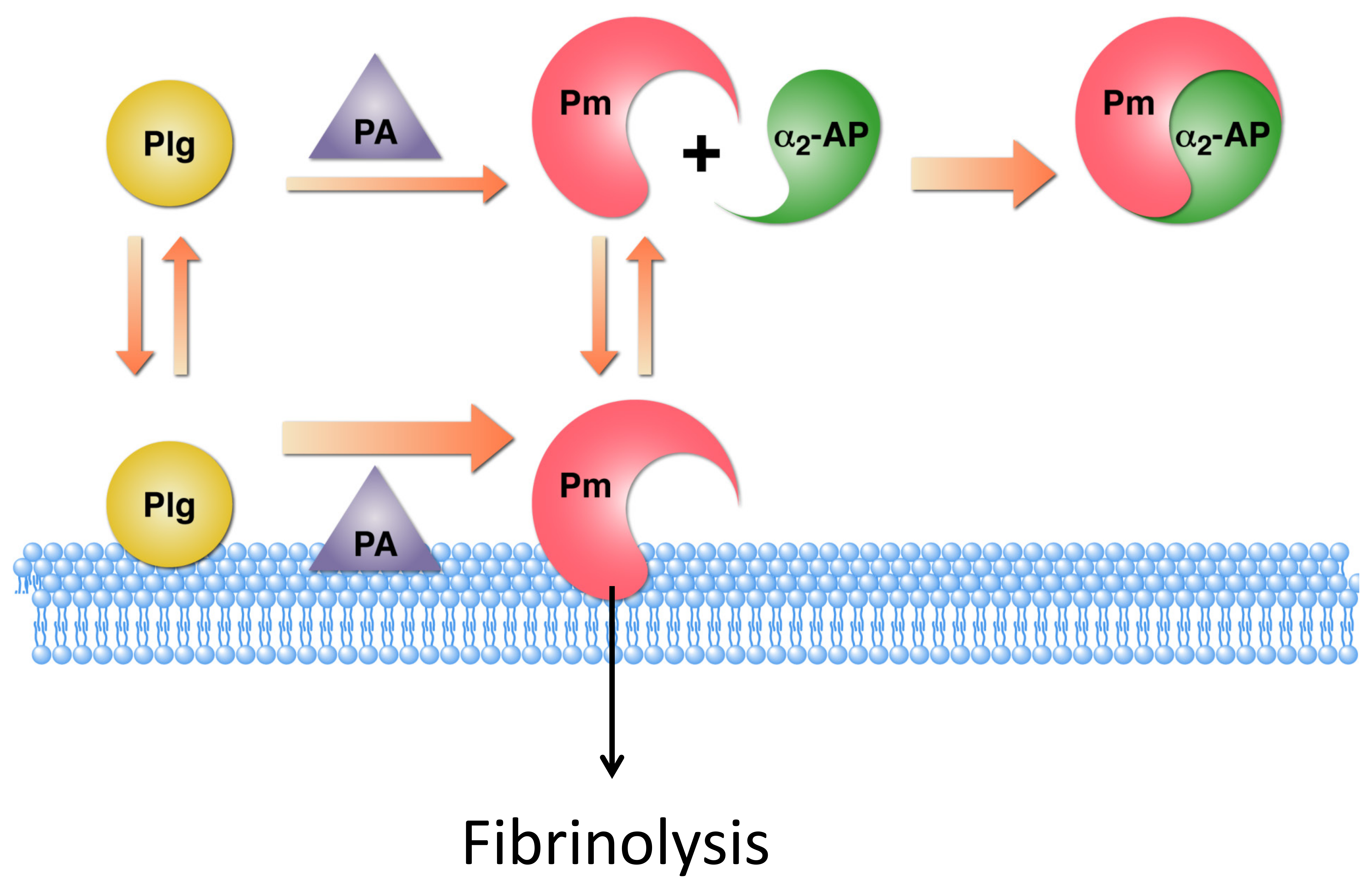
2. Similarities in Plasminogen Activation on Fibrin and on Cell Surfaces
3. Cellular Plasminogen Receptors
4. Intravascular Fibrinolysis
5. Immune Cell Recruitment in the Inflammatory Response
6. Wound Healing
7. Lactation
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Miles, L.A.; Plow, E.F. Binding and activation of plasminogen on the platelet surface. J. Biol. Chem. 1985, 260, 4303–4311. [Google Scholar] [CrossRef]
- Miles, L.A.; Parmer, R.J. Plasminogen receptors: The first quarter century. Semin. Thromb. Hemost. 2013, 39, 329–337. [Google Scholar] [CrossRef]
- Miles, L.A.; Lighvani, S.; Baik, N.; Parmer, C.M.; Khaldoyanidi, S.; Mueller, B.M.; Parmer, R.J. New insights into the role of Plg-RKT in macrophage recruitment. Int. Rev. Cell Mol. Biol. 2014, 309, 259–302. [Google Scholar]
- Hoylaerts, M.; Rijken, D.C.; Lijnen, H.R.; Collen, D. Kinetics of the activation of plasminogen by human tissue plasminogen activator. J. Biol. Chem. 1982, 257, 2912–2919. [Google Scholar] [CrossRef]
- Miles, L.A.; Dahlberg, C.M.; Plow, E.F. The cell-binding domains of plasminogen and their function in plasma. J. Biol. Chem. 1988, 263, 11928–11934. [Google Scholar] [CrossRef]
- Félez, J.; Miles, L.A.; Fábregas, P.; Jardi, M.; Plow, E.F.; Lijnen, R.H. Characterization of cellular binding sites and interactive regions within reactants required for enhancement of plasminogen activation by tPA on the surface of leukocytic cells. Thromb. Haemost. 1996, 76, 577–584. [Google Scholar] [CrossRef]
- Miles, L.A.; Andronicos, N.M.; Chen, E.I.; Baik, N.; Bai, H.; Parmer, C.M.; Lighvani, S.; Nangia, S.; Kiosses, W.B.; Kamps, M.P.; et al. Identification of the Novel Plasminogen Receptor, Plg-RKT in Proteomics—Human Diseases and Protein Functions; IntechOpen Limited: London, UK, 2011. [Google Scholar] [CrossRef][Green Version]
- Gong, Y.; Kim, S.O.; Felez, J.; Grella, D.K.; Castellino, F.J.; Miles, L.A. Conversion of glu-plasminogen to lys-plasminogen is necessary for optimal stimulation of plasminogen activation on the endothelial cell surface. J. Biol. Chem. 2001, 276, 19078–19083. [Google Scholar] [CrossRef] [PubMed]
- Miles, L.A.; Castellino, F.J.; Gong, Y. Critical role for conversion of glu-plasminogen to Lys-plasminogen for optimal stimulation of plasminogen activation on cell surfaces. Trends Cardiovasc. Med. 2003, 13, 21–30. [Google Scholar] [CrossRef]
- Zhang, L.; Gong, Y.; Grella, D.K.; Castellino, F.J.; Miles, L.A. Endogenous plasmin converts Glu-plasminogen to Lys-plasminogen on the monocytoid cell surface. J. Thromb. Haemost. 2003, 1, 1264–1270. [Google Scholar] [CrossRef]
- Han, J.; Baik, N.; Kim, K.H.; Yang, J.M.; Han, G.W.; Gong, Y.; Jardi, M.; Castellino, F.J.; Felez, J.; Parmer, R.J.; et al. Monoclonal antibodies detect receptor-induced binding sites in Glu-plasminogen. Blood 2011, 118, 1653–1662. [Google Scholar] [CrossRef] [PubMed]
- Plow, E.F.; Freaney, D.E.; Plescia, J.; Miles, L.A. The plasminogen system and cell surfaces: Evidence for plasminogen and urokinase receptors on the same cell type. J. Cell Biol. 1986, 103, 2411–2420. [Google Scholar] [CrossRef] [PubMed]
- Hall, S.W.; Humphries, J.E.; Gonias, S.L. Inhibition of cell surface receptor-bound plasmin by a2-antiplasmin and a2-macroglobulin. J. Biol. Chem. 1991, 266, 12329–12336. [Google Scholar] [CrossRef]
- Lu, B.G.; Sofian, T.; Law, R.H.; Coughlin, P.B.; Horvath, A.J. Contribution of conserved lysine residues in the alpha2-antiplasmin C terminus to plasmin binding and inhibition. J. Biol. Chem. 2011, 286, 24544–24552. [Google Scholar] [CrossRef] [PubMed]
- Andronicos, N.M.; Chen, E.I.; Baik, N.; Bai, H.; Parmer, C.M.; Kiosses, W.B.; Kamps, M.P.; Yates, J.R., III; Parmer, R.J.; Miles, L.A. Proteomics-based discovery of a novel, structurally unique, and developmentally regulated plasminogen receptor, Plg-RKT, a major regulator of cell surface plasminogen activation. Blood 2010, 115, 1319–1330. [Google Scholar] [CrossRef] [PubMed]
- Miles, L.A.; Dahlberg, C.M.; Plescia, J.; Felez, J.; Kato, K.; Plowz, E.F. Role of cell-surface lysines in plasminogen binding to cells: Identification of alpha-Enolase as a candidate plasminogen receptor. Biochemistry 1991, 30, 1682–1691. [Google Scholar] [CrossRef] [PubMed]
- Redlitz, A.; Fowler, B.J.; Plow, E.F.; Miles, L.A. The role of an enolase-related molecule in plasminogen binding to cells. Eur. J. Biochem. 1995, 227, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Hembrough, T.A.; Vasudevan, J.; Allietta, M.M.; Glass, W.F.; Gonias, S.L. A cytokeratin 8-like protein with plasminogen-binding activity is present on the external surfaces of hepatocytes, HepG2 cells and breast carcinoma cell lines. J. Cell Sci. 1995, 108, 1071–1082. [Google Scholar] [PubMed]
- Hembrough, T.A.; Kralovich, K.R.; Li, L.; Gonias, S.L. Cytokeratin 8 released by breast carcinoma cells in vitro binds plasminogen and tissue-type plasminogen activator and promotes plasminogen activation. Biochem. J. 1996, 317, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Kassam, G.; Le, B.H.; Choi, K.S.; Kang, H.M.; Fitzpatrick, S.L.; Louie, P.; Waisman, D.M. The p11 subunit of the annexin II tetramer plays a key role in the stimulation of t-PA-dependent plasminogen activation. Biochemistry 1998, 37, 16958–16966. [Google Scholar] [CrossRef] [PubMed]
- Herren, T.; Burke, T.A.; Das, R.; Plow, E.F. Identification of histone H2B as a regulated plasminogen receptor. Biochemistry 2006, 45, 9463–9474. [Google Scholar] [CrossRef]
- Hawley, S.B.; Tamura, T.; Miles, L.A. Purification, cloning, and characterization of a profibrinolytic plasminogen-binding protein, TIP49a. J. Biol. Chem. 2001, 276, 179–186. [Google Scholar] [CrossRef]
- Dudani, A.K.; Ganz, P.R. Endothelial cell surface actin serves as a binding site for plasminogen, tissue plasminogen activator and lipoprotein(a). Br. J. Haematol. 1996, 95, 168–178. [Google Scholar] [CrossRef] [PubMed]
- Miles, L.A.; Andronicos, N.M.; Baik, N.; Parmer, R.J. Cell-surface actin binds plasminogen and modulates neurotransmitter release from catecholaminergic cells. J. Neurosci. 2006, 26, 13017–13024. [Google Scholar] [CrossRef]
- Briens, A.; Bardou, I.; Lebas, H.; Miles, L.A.; Parmer, R.J.; Vivien, D.; Docagne, F. Astrocytes regulate the balance between plasminogen activation and plasmin clearance via cell-surface actin. Cell Discov. 2017, 3. [Google Scholar] [CrossRef]
- Fan, Z.; Larson, P.J.; Bognacki, J.; Raghunath, P.N.; Tomaszewski, J.E.; Kuo, A.; Canziani, G.; Chaiken, I.; Cines, D.B.; Higazi, A.A. Tissue factor regulates plasminogen binding and activation. Blood 1998, 91, 1987–1998. [Google Scholar] [CrossRef] [PubMed]
- Miles, L.A.; Dahlberg, C.M.; Levin, E.G.; Plow, E.F. Gangliosides interact directly with plasminogen and urokinase and may mediate binding of these components to cells. Biochemistry 1989, 280, 9337–9343. [Google Scholar] [CrossRef] [PubMed]
- Miles, L.A.; Ginsberg, M.H.; White, J.G.; Plow, E.F. Plasminogen interacts with human platelets through two distinct mechanisms. J. Clin. Invest. 1986, 77, 2001–2009. [Google Scholar] [CrossRef]
- Pluskota, E.; Soloviev, D.A.; Bdeir, K.; Cines, D.B.; Plow, E.F. Integrin alphaMbeta2 orchestrates and accelerates plasminogen activation and fibrinolysis by neutrophils. J. Biol. Chem. 2004, 279, 18063–18072. [Google Scholar] [CrossRef]
- Lishko, V.K.; Novokhatny, V.V.; Yakubenko, V.P.; Prokvolit, S.H.V.; Ugarova, T.P. Characterization of plasminogen as an adhesive ligand for integrins {alpha}M{beta}2 (Mac-1) and {alpha}5{beta}1(VLA-5). Blood 2004, 104, 719–726. [Google Scholar] [CrossRef] [PubMed]
- Parkkinen, J.; Raulo, E.; Merenmies, J.; Nolo, R.; Kajander, E.O.; Baumann, M.; Rauvala, H. Amphoterin, the 30-kDa protein in a family of HMG1-type polypeptides. Enhanced expression in transformed cells, leading edge localization, and interactions with plasminogen activation. J. Biol. Chem. 1993, 268, 19726–19738. [Google Scholar] [CrossRef]
- Kanalas, J.J.; Makker, S.P. Identification of the rat Heymann nephritis autoantigen (GP330) as a receptor site for plasminogen. J. Biol. Chem. 1991, 266, 10825–10829. [Google Scholar] [CrossRef]
- Miles, L.A.; Plow, E.F.; Waisman, D.M.; Parmer, R.J. Plasminogen receptors. J. Biomed. Biotechnol. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Ling, Q.; Jacovina, A.T.; Deora, A.; Febbraio, M.; Simantov, R.; Silverstein, R.L.; Hempstead, B.; Mark, W.H.; Hajjar, K.A. Annexin II regulates fibrin homeostasis and neoangiogenesis in vivo. J. Clin. Invest. 2004, 113, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Surette, A.P.; Madureira, P.A.; Phipps, K.D.; Miller, V.A.; Svenningsson, P.; Waisman, D.M. Regulation of fibrinolysis by S100A10 in vivo. Blood 2011, 118, 3172–3181. [Google Scholar] [CrossRef]
- Miles, L.A.; Baik, N.; Lighvani, S.; Khaldoyanidi, S.; Varki, N.M.; Bai, H.; Mueller, B.M.; Parmer, R.J. Deficiency of plasminogen receptor, Plg-RKT, causes defects in plasminogen binding and inflammatory macrophage recruitment in vivo. J. Thromb. Haemost. 2017, 15, 155–612. [Google Scholar] [CrossRef]
- Das, R.; Burke, T.; Plow, E.F. Histone H2B as a functionally important plasminogen receptor on macrophages. Blood 2007, 110, 3763–3772. [Google Scholar] [CrossRef] [PubMed]
- Wygrecka, M.; Marsh, L.M.; Morty, R.E.; Henneke, I.; Guenther, A.; Lohmeyer, J.; Markart, P.; Preissner, K.T. Enolase-1 promotes plasminogen-mediated recruitment of monocytes to the acutely inflamed lung. Blood 2009, 113, 5588–5598. [Google Scholar] [CrossRef] [PubMed]
- Bugge, T.H.; Flick, M.J.; Daugherty, C.C.; Degen, J.L. Plasminogen deficiency causes severe thrombosis but is compatible with development and reproducton. Genes. Dev. 1995, 9, 794–807. [Google Scholar] [CrossRef]
- Ploplis, V.A.; Carmeliet, P.; Vazirzadeh, S.; Van, V.I.; Moons, L.; Plow, E.F.; Collen, D. Effects of disruption of the plasminogen gene on thrombosis, growth, and health in mice. Circulation 1995, 92, 2585–2593. [Google Scholar] [CrossRef] [PubMed]
- Madureira, P.A.; Surette, A.P.; Phipps, K.D.; Taboski, M.A.; Miller, V.A.; Waisman, D.M. The role of the annexin A2 heterotetramer in vascular fibrinolysis. Blood 2011, 118, 4789–4797. [Google Scholar] [CrossRef]
- Puisieux, A.; Ji, J.; Ozturk, M. Annexin II up-regulates cellular levels of p11 protein by a post-translational mechanisms. Biochem. J. 1996, 313, 51–55. [Google Scholar] [CrossRef]
- Zobiack, N.; Rescher, U.; Ludwig, C.; Zeuschner, D.; Gerke, V. The annexin 2/S100A10 complex controls the distribution of transferrin receptor-containing recycling endosomes. Mol. Biol. Cell. 2003, 14, 4896–4908. [Google Scholar] [CrossRef]
- He, K.L.; Deora, A.B.; Xiong, H.; Ling, Q.; Weksler, B.B.; Niesvizky, R.; Hajjar, K.A. Endothelial cell annexin A2 regulates polyubiquitination and degradation of its binding partner S100A10/p. J. Biol. Chem. 2008, 283, 19192–19200. [Google Scholar] [CrossRef]
- Hou, Y.; Yang, L.; Mou, M.; Hou, Y.; Zhang, A.; Pan, N.; Qiang, R.; Wei, L.; Zhang, N. Annexin A2 regulates the levels of plasmin, S100A10 and Fascin in L5178Y cells. Cancer Invest. 2008, 26, 809–815. [Google Scholar] [CrossRef]
- Whyte, C.S.; Morrow, G.B.; Baik, N.; Booth, N.A.; Jalal, M.M.; Parmer, R.J.; Miles, L.A.; Mutch, N.J. Exposure of plasminogen and the novel plasminogen receptor, Plg-RKT, on activated human and murine platelets. Blood 2020. [Google Scholar] [CrossRef]
- Bavil, A.A.; Hayes, S.; Goretzki, L.; Kroger, M.; Anders, J.; Hendriks, R. Convenient and versatile subcellular extraction procedure, that facilitates classical protein expression profiling and functional protein analysis. Proteomics 2004, 4, 1397–1405. [Google Scholar] [CrossRef]
- Ploplis, V.A.; French, E.L.; Carmeliet, P.; Collen, D.; Plow, E.F. Plasminogen deficiency differentially affects recruitment of inflammatory cell populations in mice. Blood 1998, 91, 2005–2009. [Google Scholar] [CrossRef] [PubMed]
- Plow, E.F.; Ploplis, V.A.; Busuttil, S.; Carmeliet, P.; Collen, D. A role of plasminogen in atherosclerosis and restenosis models in mice. Thromb. Haemost. 1999, 82, 4–7. [Google Scholar] [PubMed]
- Busuttil, S.J.; Ploplis, V.A.; Castellino, F.J.; Tang, L.; Eaton, J.W.; Plow, E.F. A central role for plasminogen in the inflammatory response to biomaterials. J. Thromb. Haemost. 2004, 2, 1798–1805. [Google Scholar] [CrossRef]
- Vago, J.P.; Sugimoto, M.A.; Lima, K.M.; Lima, N.G.L.; Baik, N.; Teixeira, M.M.; Perretti, M.; Parmer, R.J.; Miles, L.A.; Sousa, L.P. Plasminogen and the Plasminogen Receptor, Plg-RKT, Regulate Macrophage Phenotypic, and Functional Changes. Front. Immunol. 2019, 10, 1458. [Google Scholar] [CrossRef]
- Silva, L.M.; Lum, A.G.; Tran, C.; Shaw, M.W.; Gao, Z.; Flick, M.J.; Moutsopoulos, N.M.; Bugge, T.H.; Mullins, E.S. Plasmin-mediated fibrinolysis enables macrophage migration in a murine model of inflammation. Blood 2019, 134, 291–303. [Google Scholar] [CrossRef]
- Motley, M.P.; Madsen, D.H.; Jurgensen, H.J.; Spencer, D.E.; Szabo, R.; Holmbeck, K.; Flick, M.; Lawrence, D.A.; Castellino, F.J.; Weigert, R.; et al. A CCR2 macrophage endocytic pathway mediates extravascular fibrin clearance in vivo. Blood 2016, 127, 1085–1096. [Google Scholar] [CrossRef]
- Swaisgood, C.M.; Schmitt, D.; Eaton, D.; Plow, E.F. In vivo regulation of plasminogen function by plasma carboxypeptidase B. J. Clin. Invest. 2002, 110, 1275–1282. [Google Scholar] [CrossRef]
- Lighvani, S.; Baik, N.; Diggs, J.E.; Khaldoyanidi, S.; Parmer, R.J.; Miles, L.A. Regulation of macrophage migration by a novel plasminogen receptor Plg-RKT. Blood 2011, 118, 5622–5630. [Google Scholar] [CrossRef]
- Connell, P.A.; Surette, A.P.; Liwski, R.S.; Svenningsson, P.; Waisman, D.M. S100A10 regulates plasminogen-dependent macrophage invasion. Blood 2010, 116, 1136–1146. [Google Scholar] [CrossRef]
- Thaler, B.; Baik, N.; Hohensinner, P.J.; Baumgartner, J.; Panzenbock, A.; Stojkovic, S.; Demyanets, S.; Huk, I.; Kaun, R.G.; Kaun, C.; et al. Differential expression of Plg-RKT and its effects on migration of proinflammatory monocyte and macrophage subsets. Blood 2019, 134, 561–567. [Google Scholar] [CrossRef]
- Gong, Y.; Hart, E.; Shchurin, A.; Plow, H.J. Inflammatory macrophage migration requires MMP-9 activation by plasminogen in mice. J. Clin. Invest. 2008, 118, 3012–3024. [Google Scholar] [CrossRef]
- Rose, L.F.; Chan, R.K. The Burn Wound Microenvironment. Adv. Wound Care 2016, 5, 106–118. [Google Scholar] [CrossRef]
- Hettiaratchy, S.; Dziewulski, P. ABC of burns: Pathophysiology and types of burns. BMJ 2004, 328, 1427–1429. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, D.J.; Mahan, J.T. Keratinocyte migration and the extracellular matrix. J. Invest. Dermatol. 1988, 90, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Mingers, A.M.; Heimburger, N.; Zeitler, P.; Kreth, H.W.; Schuster, V. Homozygous type I plasminogen deficiency. Semin. Thromb. Hemost. 1997, 23, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Schuster, V.; Mingers, A.M.; Seidenspinner, S.; Nüssgens, Z.; Pukrop, T.; Kreth, H.W. Homozygous mutations in the plasminogen gene of two unrelated girls with ligneous conjunctivitis. Blood 1997, 90, 958–966. [Google Scholar] [CrossRef]
- Klammt, J.; Kobelt, L.; Aktas, D.; Durak, I.; Gokbuget, A.; Hughes, Q.; Irkec, M.; Kurtulus, I.; Lapi, E.; Mechoulam, H.; et al. Identification of three novel plasminogen (PLG) gene mutations in a series of 23 patients with low PLG activity. Thromb. Haemost. 2011, 105, 454–460. [Google Scholar] [CrossRef]
- Shapiro, A.D.; Nakar, C.; Parker, J.M.; Albert, G.R.; Moran, J.E.; Thibaudeau, K.; Thukral, N.; Hardesty, B.M.; Laurin, P.; Sandset, P.M. Plasminogen replacement therapy for the treatment of children and adults with congenital plasminogen deficiency. Blood 2018, 131, 1301–1310. [Google Scholar] [CrossRef] [PubMed]
- Rouatbi, A.; Chebbi, A.; Bouguila, H. Ligneous conjunctivitis due to plasminogen deficit: Diagnostic and therapeutic approach. With literature review. J. Fr. Ophtalmol. 2018, 41, 916–919. [Google Scholar] [CrossRef] [PubMed]
- Schuster, V.; Hugle, B.; Tefs, K. Plasminogen deficiency. J. Thromb. Haemost. 2007, 5, 2315–2322. [Google Scholar] [CrossRef]
- Romer, J.; Bugge, T.H.; Pyke, C.; Lund, L.R.; Flick, M.J.; Degen, J.L.; Dano, K. Impaired wound healing in mice with a disrupted plasminogen gene. Nat. Med. 1996, 2, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Creemers, E.; Cleutjens, J.; Smits, J.; Heymans, S.; Moons, L.; Collen, D.; Daemen, M.; Carmeliet, P. Disruption of the plasminogen gene in mice abolishes wound healing after myocardial infarction. Am. J. Pathol. 2000, 156, 1865–1873. [Google Scholar] [CrossRef]
- Eriksson, P.O.; Li, J.; Ny, T.; Hellstrom, S. Spontaneous development of otitis media in plasminogen-deficient mice. Int. J. Med. Microbiol. 2006, 296. [Google Scholar] [CrossRef]
- Li, J.; Eriksson, P.O.; Hansson, A.; Hellstrom, S.; Ny, T. Plasmin/plasminogen is essential for the healing of tympanic membrane perforations. Thromb. Haemost. 2006, 96, 512–519. [Google Scholar] [CrossRef]
- Sulniute, R.; Lindh, T.; Wilczynska, M.; Li, J.; Ny, T. Plasmin is essential in preventing periodontitis in mice. Am. J. Pathol. 2011, 179. [Google Scholar] [CrossRef] [PubMed]
- Sulniute, R.; Shen, Y.; Guo, Y.Z.; Fallah, M.; Ahlskog, N.; Ny, L.; Rakhimova, O.; Broden, J.; Boija, H.; Moghaddam, A.; et al. Plasminogen is a critical regulator of cutaneous wound healing. Thromb. Haemost. 2016, 115, 1001–1009. [Google Scholar] [CrossRef]
- Fallah, M.; Viklund, E.; Bäckman, A.; Brodén, J.; Lundskog, B.; Johansson, M.; Blomquist, M.; Wilczynska, M.; Ny, T. Plasminogen is a master regulator and a potential drug candidate for the healing of radiation wounds. Cell Death Dis. 2020, 11, 201. [Google Scholar] [CrossRef]
- Bugge, T.H.; Kombrinck, K.W.; Flick, M.J.; Daugherty, C.C.; Danton, M.J.S.; Degen, J.L. Loss of fibrinogen rescues mice from the pleiotropic effects of plasminogen deficiency. Cell 1996, 87, 709–719. [Google Scholar] [CrossRef]
- Shen, Y.; Guo, Y.; Mikus, P.; Sulniute, R.; Wilczynska, M.; Ny, T.; Li, J. Plasminogen is a key proinflammatory regulator that accelerates the healing of acute and diabetic wounds. Blood 2012, 119, 5879–5887. [Google Scholar] [CrossRef] [PubMed]
- Syrovets, T.; Jendrach, M.; Rohwedder, A.; Schule, A.; Simmet, T. Plasmin-induced expression of cytokines and tissue factor in human monocytes involves AP-1 and IKKbeta-mediated NF-kappaB activation. Blood 2001, 97, 3941–3950. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Laumonnier, Y.; Syrovets, T.; Simmet, T. Plasmin triggers cytokine induction in human monocyte-derived macrophages. Arter. Thromb. Vasc. Biol. 2007, 27, 1383–1389. [Google Scholar] [CrossRef]
- Syrovets, T.; Lunov, O.; Simmet, T. Plasmin as a proinflammatory cell activator. J. Leukoc. Biol. 2012, 92, 509–519. [Google Scholar] [CrossRef]
- Ny, L.; Parmer, R.J.; Shen, Y.; Holmberg, S.; Baik, N.; Bäckman, A.; Broden, J.; Wilczynska, M.; Ny, T.; Miles, L.A. The plasminogen receptor, Plg-R(KT), plays a role in inflammation and fibrinolysis during cutaneous wound healing in mice. Cell Death Dis. 2020, 11, 1054. [Google Scholar] [CrossRef]
- Lund, L.R.; Bjorn, S.F.; Sternlicht, M.D.; Nielsen, B.S.; Solberg, H.; Usher, P.A.; Osterby, R.; Christensen, I.J.; Stephens, R.W.; Bugge, T.H.; et al. Lactational competence and involution of the mouse mammary gland require plasminogen. Development 2000, 127, 4481–4492. [Google Scholar]
- Green, K.A.; Nielsen, B.S.; Castellino, F.J.; Romer, J.; Lund, L.R. Lack of plasminogen leads to milk stasis and premature mammary gland involution during lactation. Dev. Biol. 2006, 299, 164–175. [Google Scholar] [CrossRef] [PubMed]
- Miles, L.A.; Baik, N.; Bai, H.; Makarenkova, H.P.; Kiosses, W.B.; Krajewski, S.; Castellino, F.J.; Valenzuela, A.; Varki, N.M.; Mueller, B.M.; et al. The Plasminogen Receptor Plg-RKT, is Essential for Mammary Lobuloalveolar Development, Lactation. J. Thromb. Haemost. 2018, 16, 919–932. [Google Scholar] [CrossRef] [PubMed]
- Bharadwaj, A.G.; Dahn, M.L.; Liu, R.Z.; Colp, P.; Thomas, L.N.; Holloway, R.W.; Marignani, P.A.; Too, C.K.; Barnes, P.J.; Godbout, R.; et al. S100A10 Has a Critical Regulatory Function in Mammary Tumor Growth and Metastasis: Insights Using MMTV-PyMT Oncomice and Clinical Patient Sample Analysis. Cancers (Basel) 2020, 12. [Google Scholar] [CrossRef] [PubMed]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miles, L.A.; Ny, L.; Wilczynska, M.; Shen, Y.; Ny, T.; Parmer, R.J. Plasminogen Receptors and Fibrinolysis. Int. J. Mol. Sci. 2021, 22, 1712. https://doi.org/10.3390/ijms22041712
Miles LA, Ny L, Wilczynska M, Shen Y, Ny T, Parmer RJ. Plasminogen Receptors and Fibrinolysis. International Journal of Molecular Sciences. 2021; 22(4):1712. https://doi.org/10.3390/ijms22041712
Chicago/Turabian StyleMiles, Lindsey A., Lina Ny, Malgorzata Wilczynska, Yue Shen, Tor Ny, and Robert J. Parmer. 2021. "Plasminogen Receptors and Fibrinolysis" International Journal of Molecular Sciences 22, no. 4: 1712. https://doi.org/10.3390/ijms22041712
APA StyleMiles, L. A., Ny, L., Wilczynska, M., Shen, Y., Ny, T., & Parmer, R. J. (2021). Plasminogen Receptors and Fibrinolysis. International Journal of Molecular Sciences, 22(4), 1712. https://doi.org/10.3390/ijms22041712





