Activation of the Complement System on Human Endothelial Cells by Urban Particulate Matter Triggers Inflammation-Related Protein Production
Abstract
1. Introduction
2. Results
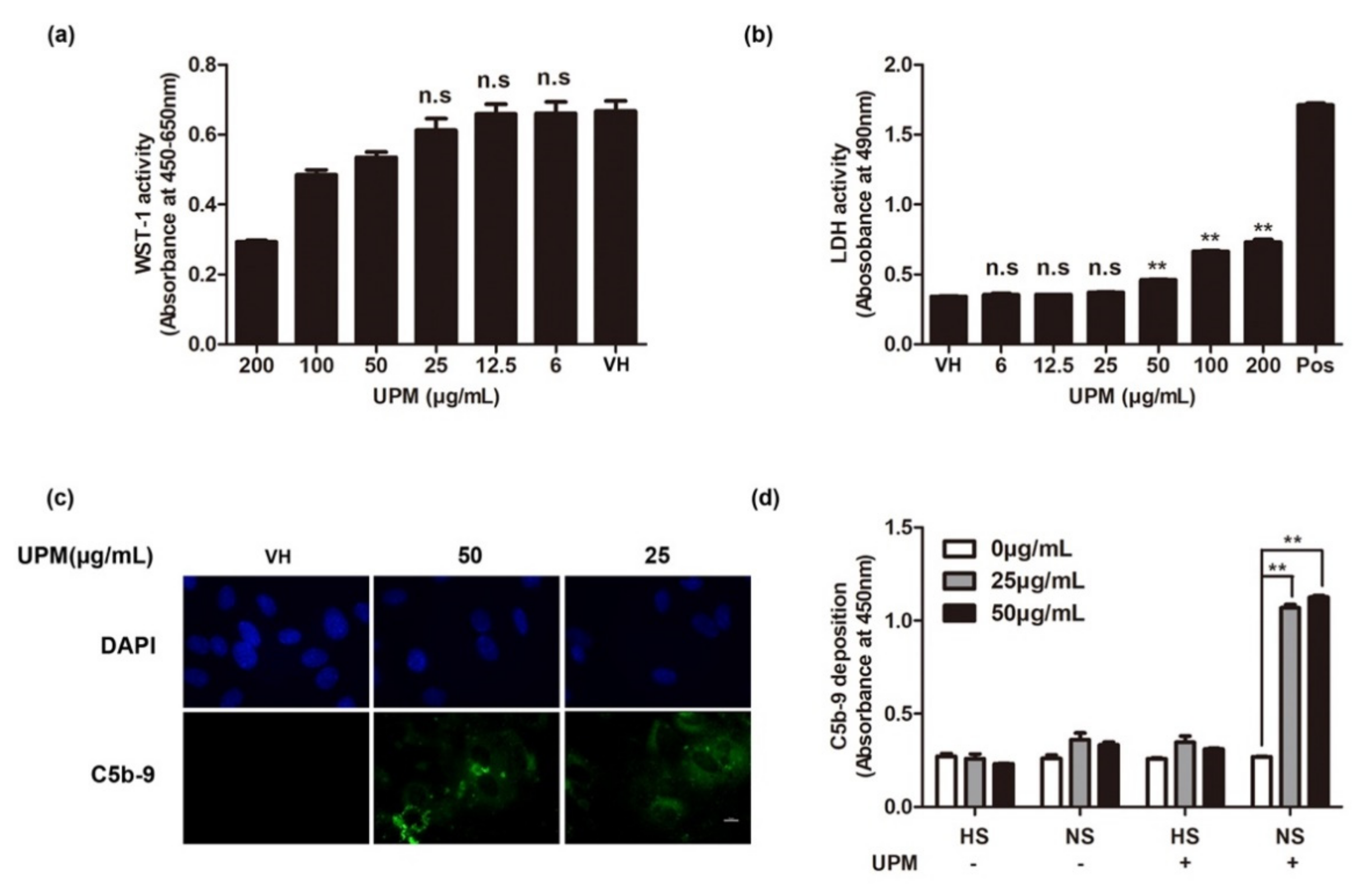
2.1. Effects of UPM on Human Endothelial Cell Viability and Complement Activation
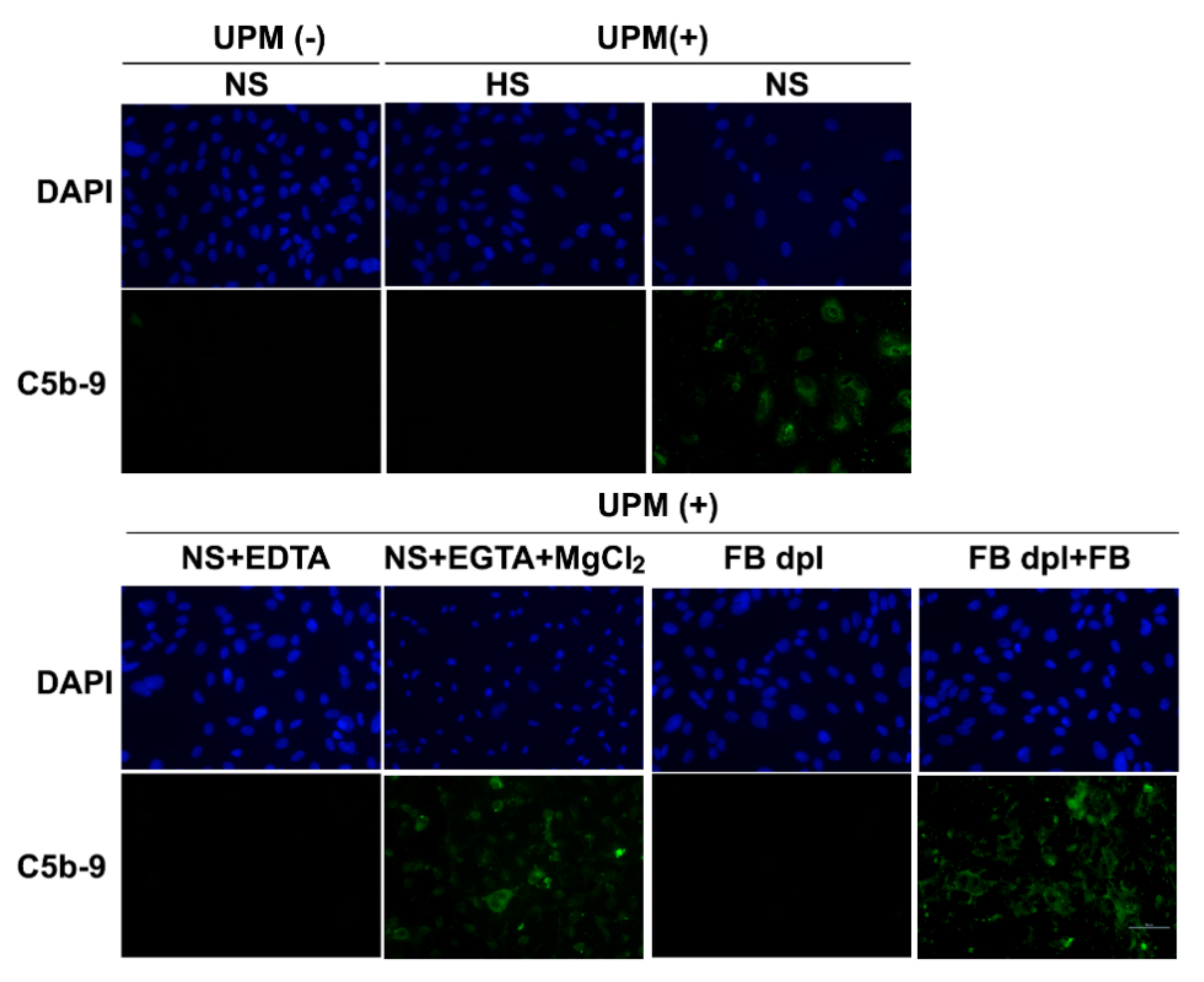
2.2. UPM Activates the Complement System in HUVECs via the Alternative Pathway
2.3. UPM-Mediated Complement Activation of HUVECs Is Associated with ROS But Not Complement Regulatory Proteins
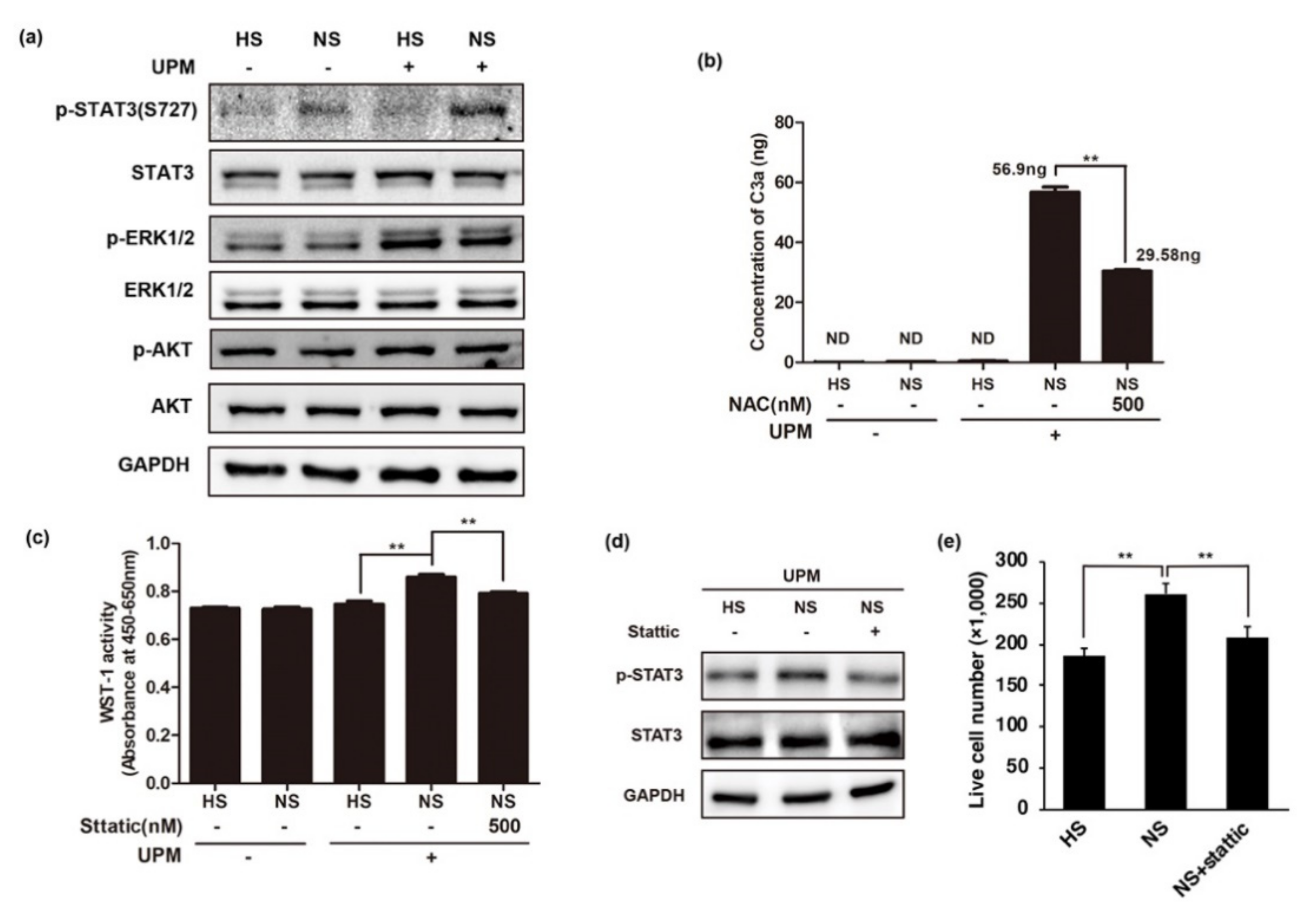
2.4. Cell Viability in Complement-Activated HUVECs Following UPM Treatment
2.5. UPM-Mediated Complement Activation Induces the Phosphorylation of STAT3
2.6. UPM-Mediated Complement Activation Stimulates the Production of Inflammatory Cytokines
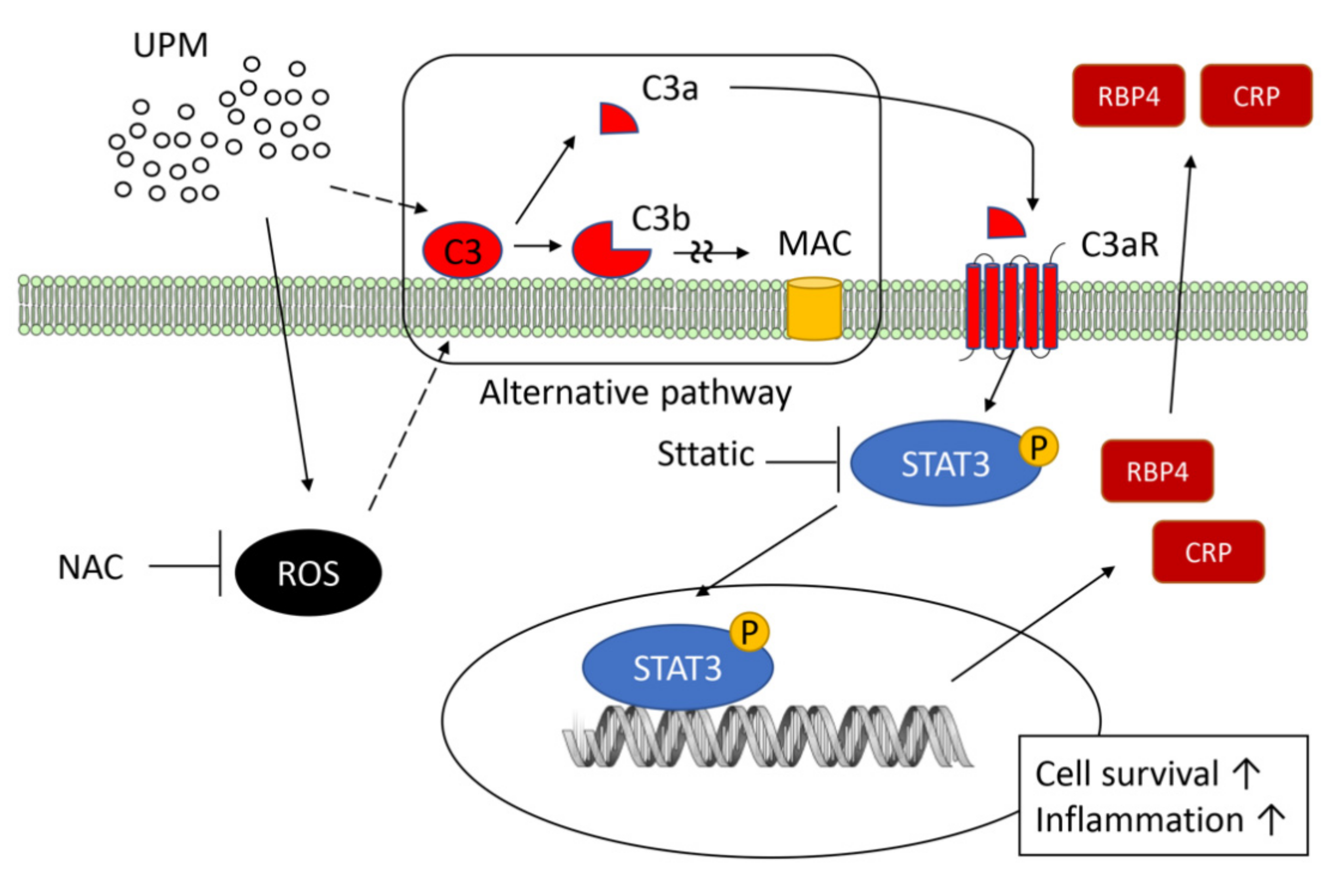
3. Discussion
4. Materials and Methods
4.1. Reagents and Antibodies
4.2. Cell Culture
4.3. Exposure of HUVECs to UPM and Other Inhibitors
4.4. Reverse Transcription Quantitative PCR
4.5. Western Blotting
4.6. Reactive Oxygen Species Measurement
4.7. Enzyme-Linked Immunosorbent Assay
4.8. Detection of C5b-9 Using Cell-Based ELISA
4.9. Flow Cytometric Analysis for C3b-Binding Cells
4.10. Cell Proliferation Assay
4.11. LDH Assay
4.12. Immunofluorescence Assay for the Deposition of C5b-9
4.13. Antibody Array for Cytokine Production
4.14. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dockery, D.W.; Pope, C.A., 3rd. Acute respiratory effects of particulate air pollution. Annu. Rev. Public Health 1994, 15, 107–132. [Google Scholar] [CrossRef] [PubMed]
- Katsouyanni, K.; Touloumi, G.; Spix, C.; Schwartz, J.; Balducci, F.; Medina, S.; Rossi, G.; Wojtyniak, B.; Sunyer, J.; Bacharova, L.; et al. Short-term effects of ambient sulphur dioxide and particulate matter on mortality in 12 European cities: Results from time series data from the APHEA project. Air Pollution and Health: A European Approach. BMJ 1997, 314, 1658–1663. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J. What are people dying of on high air pollution days? Environ. Res. 1994, 64, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Xing, Y.F.; Xu, Y.H.; Shi, M.H.; Lian, Y.X. The impact of PM2.5 on the human respiratory system. J. Thorac. Dis. 2016, 8, E69–E74. [Google Scholar]
- Chen, C.H.; Wu, C.D.; Chiang, H.C.; Chu, D.; Lee, K.Y.; Lin, W.Y.; Yeh, J.I.; Tsai, K.W.; Guo, Y.L. The effects of fine and coarse particulate matter on lung function among the elderly. Sci. Rep. 2019, 9, 14790. [Google Scholar] [CrossRef]
- Hamanaka, R.B.; Mutlu, G.M. Particulate Matter Air Pollution: Effects on the Cardiovascular System. Front. Endocrinol. 2018, 9, 680. [Google Scholar] [CrossRef] [PubMed]
- Sigaux, J.; Biton, J.; Andre, E.; Semerano, L.; Boissier, M.C. Air pollution as a determinant of rheumatoid arthritis. Jt. Bone Spine 2019, 86, 37–42. [Google Scholar] [CrossRef]
- Shimada, A.; Kawamura, N.; Okajima, M.; Kaewamatawong, T.; Inoue, H.; Morita, T. Translocation pathway of the intratracheally instilled ultrafine particles from the lung into the blood circulation in the mouse. Toxicol. Pathol. 2006, 34, 949–957. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Wang, L.; Moreno-Vinasco, L.; Lang, G.D.; Siegler, J.H.; Mathew, B.; Usatyuk, P.V.; Samet, J.M.; Geyh, A.S.; Breysse, P.N.; et al. Particulate matter air pollution disrupts endothelial cell barrier via calpain-mediated tight junction protein degradation. Part Fibre Toxicol. 2012, 9, 35. [Google Scholar] [CrossRef]
- Pope, C.A., 3rd; Bhatnagar, A.; McCracken, J.P.; Abplanalp, W.; Conklin, D.J.; O’Toole, T. Exposure to Fine Particulate Air Pollution Is Associated With Endothelial Injury and Systemic Inflammation. Circ. Res. 2016, 119, 1204–1214. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, H.; He, Y.W. The Complement Receptors C3aR and C5aR Are a New Class of Immune Checkpoint Receptor in Cancer Immunotherapy. Front. Immunol. 2019, 10, 1574. [Google Scholar] [CrossRef] [PubMed]
- Xia, T.; Korge, P.; Weiss, J.N.; Li, N.; Venkatesen, M.I.; Sioutas, C.; Nel, A. Quinones and aromatic chemical compounds in particulate matter induce mitochondrial dysfunction: Implications for ultrafine particle toxicity. Environ. Health Perspect. 2004, 112, 1347–1358. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Yue, P.; Ying, Z.; Cardounel, A.J.; Brook, R.D.; Devlin, R.; Hwang, J.S.; Zweier, J.L.; Chen, L.C.; Rajagopalan, S. Air pollution exposure potentiates hypertension through reactive oxygen species-mediated activation of Rho/ROCK. Arter. Thromb. Vasc. Biol. 2008, 28, 1760–1766. [Google Scholar] [CrossRef] [PubMed]
- Loscalzo, J. Oxidative stress in endothelial cell dysfunction and thrombosis. Pathophysiol. Haemost. Thromb. 2002, 32, 359–360. [Google Scholar] [CrossRef] [PubMed]
- Sena, C.M.; Leandro, A.; Azul, L.; Seica, R.; Perry, G. Vascular Oxidative Stress: Impact and Therapeutic Approaches. Front. Physiol. 2018, 9, 1668. [Google Scholar] [CrossRef]
- Carter, A.M. Complement activation: An emerging player in the pathogenesis of cardiovascular disease. Scientifica 2012, 2012, 402783. [Google Scholar] [CrossRef]
- Lappegard, K.T.; Garred, P.; Jonasson, L.; Espevik, T.; Aukrust, P.; Yndestad, A.; Mollnes, T.E.; Hovland, A. A vital role for complement in heart disease. Mol. Immunol. 2014, 61, 126–134. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gorsuch, W.B.; Chrysanthou, E.; Schwaeble, W.J.; Stahl, G.L. The complement system in ischemia-reperfusion injuries. Immunobiology 2012, 217, 1026–1033. [Google Scholar] [CrossRef] [PubMed]
- Collard, C.D.; Väkevä, A.; Morrissey, M.A.; Agah, A.; Rollins, S.A.; Reenstra, W.R.; Buras, J.A.; Meri, S.; Stahl, G.L. Complement activation after oxidative stress: Role of the lectin complement pathway. Am. J. Pathol. 2000, 156, 1549–1556. [Google Scholar] [CrossRef]
- Williams, J.P.; Pechet, T.T.; Weiser, M.R.; Reid, R.; Kobzik, L.; Moore, F.D., Jr.; Carroll, M.C.; Hechtman, H.B. Intestinal reperfusion injury is mediated by IgM and complement. J. Appl. Physiol. 1999, 86, 938–942. [Google Scholar] [CrossRef]
- Shima, M.; Adachi, M.; Tanaka, T.; Tsunetoshi, Y. Serum complement levels in children in communities with different levels of air pollution in Japan. Arch. Environ. Health 1999, 54, 264–270. [Google Scholar] [CrossRef]
- Hadnagy, W.; Stiller-Winkler, R.; Idel, H. Immunological alterations in sera of persons living in areas with different air pollution. Toxicol. Lett. 1996, 88, 147–153. [Google Scholar] [CrossRef]
- Robbins, R.A.; Nelson, K.J.; Gossman, G.L.; Koyama, S.; Rennard, S.I. Complement activation by cigarette smoke. Am. J. Physiol. 1991, 260 Pt 1, L254–L259. [Google Scholar] [CrossRef]
- Spiller, O.B.; Morgan, B.P. Antibody-independent activation of the classical complement pathway by cytomegalovirus-infected fibroblasts. J. Infect Dis. 1998, 178, 1597–1603. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, M.S.; Jones, T.; Song, D.Y.; Jang, J.H.; Jung, J.U.; Gao, S.J. Exploitation of the complement system by oncogenic Kaposi’s sarcoma-associated herpesvirus for cell survival and persistent infection. PLoS Pathog. 2014, 10, e1004412. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.; Lee, J.S.; Yoo, S.; Lee, M.S. Quantification of complement system activation by measuring C5b-9 cell surface deposition using a cell-ELISA technique. J. Immunol. Methods 2014, 415, 57–62. [Google Scholar] [CrossRef]
- Thurman, J.M.; Holers, V.M. The central role of the alternative complement pathway in human disease. J. Immunol. 2006, 176, 1305–1310. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.W.; Lee, T.L.; Chen, Y.C.; Liang, C.J.; Wang, S.H.; Lue, J.H.; Tsai, J.S.; Lee, S.W.; Chen, S.H.; Yang, Y.F.; et al. PM2.5-induced oxidative stress increases intercellular adhesion molecule-1 expression in lung epithelial cells through the IL-6/AKT/STAT3/NF-kappaB-dependent pathway. Part Fibre Toxicol. 2018, 15, 4. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Carney, D.F.; Hammer, C.H.; Shin, M.L. Nucleated cell killing by complement: Effects of C5b-9 channel size and extracellular Ca2+ on the lytic process. J. Immunol. 1987, 138, 1530–1536. [Google Scholar] [PubMed]
- Koski, C.L.; Ramm, L.E.; Hammer, C.H.; Mayer, M.M.; Shin, M.L. Cytolysis of nucleated cells by complement: Cell death displays multi-hit characteristics. Proc. Natl. Acad. Sci. USA 1983, 80, 3816–3820. [Google Scholar] [CrossRef]
- Jeon, H.; Yoo, S.M.; Choi, H.S.; Mun, J.Y.; Kang, H.G.; Lee, J.; Park, J.; Gao, S.J.; Lee, M.S. Extracellular vesicles from KSHV-infected endothelial cells activate the complement system. Oncotarget 2017, 8, 99841–99860. [Google Scholar] [CrossRef] [PubMed]
- Bouwens van der Vlis, T.A.M.; Kros, J.M.; Mustafa, D.A.M.; van Wijck, R.T.A.; Ackermans, L.; van Hagen, P.M.; van der Spek, P.J. The complement system in glioblastoma multiforme. Acta Neuropathol. Commun. 2018, 6, 91. [Google Scholar] [CrossRef] [PubMed]
- Haynes, T.; Luz-Madrigal, A.; Reis, E.S.; Echeverri Ruiz, N.P.; Grajales-Esquivel, E.; Tzekou, A.; Tsonis, P.A.; Lambris, J.D.; Del Rio-Tsonis, K. Complement anaphylatoxin C3a is a potent inducer of embryonic chick retina regeneration. Nat. Commun. 2013, 4, 2312. [Google Scholar] [CrossRef] [PubMed]
- Hawksworth, O.A.; Coulthard, L.G.; Taylor, S.M.; Wolvetang, E.J.; Woodruff, T.M. Brief report: Complement C5a promotes human embryonic stem cell pluripotency in the absence of FGF2. Stem. Cells 2014, 32, 3278–3284. [Google Scholar] [CrossRef]
- Monsinjon, T.; Gasque, P.; Chan, P.; Ischenko, A.; Brady, J.J.; Fontaine, M.C. Regulation by complement C3a and C5a anaphylatoxins of cytokine production in human umbilical vein endothelial cells. FASEB J. 2003, 17, 1003–1014. [Google Scholar] [CrossRef] [PubMed]
- Markiewski, M.M.; Lambris, J.D. The role of complement in inflammatory diseases from behind the scenes into the spotlight. Am. J. Pathol. 2007, 171, 715–727. [Google Scholar] [CrossRef]
- Collard, C.D.; Agah, A.; Stahl, G.L. Complement activation following reoxygenation of hypoxic human endothelial cells: Role of intracellular reactive oxygen species, NF-kappaB and new protein synthesis. Immunopharmacology 1998, 39, 39–50. [Google Scholar] [CrossRef]
- Collard, C.D.; Vakeva, A.; Bukusoglu, C.; Zund, G.; Sperati, C.J.; Colgan, S.P.; Stahl, G.L. Reoxygenation of hypoxic human umbilical vein endothelial cells activates the classic complement pathway. Circulation 1997, 96, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Trakkides, T.O.; Schafer, N.; Reichenthaler, M.; Kuhn, K.; Brandwijk, R.; Toonen, E.J.M.; Urban, F.; Wegener, J.; Enzmann, V.; Pauly, D. Oxidative Stress Increases Endogenous Complement-Dependent Inflammatory and Angiogenic Responses in Retinal Pigment Epithelial Cells Independently of Exogenous Complement Sources. Antioxidants 2019, 8, 548. [Google Scholar] [CrossRef]
- Liang, S.; Zhang, J.; Ning, R.; Du, Z.; Liu, J.; Batibawa, J.W.; Duan, J.; Sun, Z. The critical role of endothelial function in fine particulate matter-induced atherosclerosis. Part. Fibre. Toxicol. 2020, 17, 61. [Google Scholar] [CrossRef] [PubMed]
- Tedesco, F.; Pausa, M.; Nardon, E.; Introna, M.; Mantovani, A.; Dobrina, A. The cytolytically inactive terminal complement complex activates endothelial cells to express adhesion molecules and tissue factor procoagulant activity. J. Exp. Med. 1997, 185, 1619–1627. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.; Han, S.R.; Lee, S.; Park, S.J.; Kim, J.H.; Yoo, S.M.; Lee, M.S. Activation of the complement system in an osteosarcoma cell line promotes angiogenesis through enhanced production of growth factors. Sci. Rep. 2018, 8, 5415. [Google Scholar] [CrossRef]
- Bora, P.S.; Sohn, J.H.; Cruz, J.M.; Jha, P.; Nishihori, H.; Wang, Y.; Kaliappan, S.; Kaplan, H.J.; Bora, N.S. Role of complement and complement membrane attack complex in laser-induced choroidal neovascularization. J. Immunol. 2005, 174, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Kildsgaard, J.; Hollmann, T.J.; Matthews, K.W.; Bian, K.; Murad, F.; Wetsel, R.A. Cutting edge: Targeted disruption of the C3a receptor gene demonstrates a novel protective anti-inflammatory role for C3a in endotoxin-shock. J. Immunol. 2000, 165, 5406–5409. [Google Scholar] [CrossRef]
- Liu, B.; Wei, L.; Meyerle, C.; Tuo, J.; Sen, H.N.; Li, Z.; Chakrabarty, S.; Agron, E.; Chan, C.C.; Klein, M.L.; et al. Complement component C5a promotes expression of IL-22 and IL-17 from human T cells and its implication in age-related macular degeneration. J. Transl. Med. 2011, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Schraufstatter, I.U.; Trieu, K.; Sikora, L.; Sriramarao, P.; DiScipio, R. Complement c3a and c5a induce different signal transduction cascades in endothelial cells. J. Immunol. 2002, 169, 2102–2110. [Google Scholar] [CrossRef]
- Reiter, Y.; Ciobotariu, A.; Fishelson, Z. Sublytic complement attack protects tumor cells from lytic doses of antibody and complement. Eur. J. Immunol. 1992, 22, 1207–1213. [Google Scholar] [CrossRef]
- Yoo, S.M.; Lee, M.S. Kaposi’s Sarcoma-Associated Herpesvirus and Host Interaction by the Complement System. Pathogens 2020, 9, 260. [Google Scholar] [CrossRef] [PubMed]
- Schindler, R.; Gelfand, J.A.; Dinarello, C.A. Recombinant C5a stimulates transcription rather than translation of interleukin-1 (IL-1) and tumor necrosis factor: Translational signal provided by lipopolysaccharide or IL-1 itself. Blood 1990, 76, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Coulthard, L.G.; Woodruff, T.M. Is the complement activation product C3a a proinflammatory molecule? Re-evaluating the evidence and the myth. J. Immunol. 2015, 194, 3542–3548. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, Y.; Shan, K.; Wang, L.; Qiu, W.; Lu, Y.; Zhao, D.; Zhu, G.; He, F.; Wang, Y. Sublytic C5b-9 induces IL-6 and TGF-beta1 production by glomerular mesangial cells in rat Thy-1 nephritis through p300-mediated C/EBPbeta acetylation. FASEB J. 2014, 28, 1511–1525. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xie, M.; Xia, L.; Yu, T.; He, F.; Zhao, C.; Qiu, W.; Zhao, D.; Liu, Y.; Gong, Y.; et al. Sublytic C5b-9 Induces IL-23 and IL-36a Production by Glomerular Mesangial Cells via PCAF-Mediated KLF4 Acetylation in Rat Thy-1 Nephritis. J. Immunol. 2018, 201, 3184–3198. [Google Scholar] [CrossRef] [PubMed]
- Du Clos, T.W. Function of C-reactive protein. Ann. Med. 2000, 32, 274–278. [Google Scholar] [CrossRef]
- Danesh, J.; Wheeler, J.G.; Hirschfield, G.M.; Eda, S.; Eiriksdottir, G.; Rumley, A.; Lowe, G.D.; Pepys, M.B.; Gudnason, V. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N. Engl. J. Med. 2004, 350, 1387–1397. [Google Scholar] [CrossRef]
- Solini, A.; Santini, E.; Madec, S.; Rossi, C.; Muscelli, E. Retinol-binding protein-4 in women with untreated essential hypertension. Am. J. Hypertens 2009, 22, 1001–1006. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ingelsson, E.; Sundstrom, J.; Melhus, H.; Michaelsson, K.; Berne, C.; Vasan, R.S.; Riserus, U.; Blomhoff, R.; Lind, L.; Arnlov, J. Circulating retinol-binding protein 4, cardiovascular risk factors and prevalent cardiovascular disease in elderly. Atherosclerosis 2009, 206, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Bobbert, T.; Raila, J.; Schwarz, F.; Mai, K.; Henze, A.; Pfeiffer, A.F.; Schweigert, F.J.; Spranger, J. Relation between retinol, retinol-binding protein 4, transthyretin and carotid intima media thickness. Atherosclerosis 2010, 213, 549–551. [Google Scholar] [CrossRef]
- Farjo, K.M.; Farjo, R.A.; Halsey, S.; Moiseyev, G.; Ma, J.X. Retinol-binding protein 4 induces inflammation in human endothelial cells by an NADPH oxidase- and nuclear factor kappa B-dependent and retinol-independent mechanism. Mol. Cell Biol. 2012, 32, 5103–5115. [Google Scholar] [CrossRef]



| Gene | Sense Primer | Anti-Sense Primer |
|---|---|---|
| GAPDH | GGT ATC GTG GAA GGA CTC | GTA GAS GCA GGG ATG ATG |
| CD46 | TTT GAA TGC GAT AAG GGT TT | GAG ACT GGA GGC TTG TAA |
| CD55 | GGC AGT CAA TGG TCA GAT A | GGC ACT CAT ATT CCA CAA C |
| CD59 | AAG AAG GAC CTG TGT AAC TT | GAG TCA CCA GCA GAA GAA |
| Factor H | TGT GGT TAC AAT GGT TGG TCT GAT | GGT AGC ACT GAA CGG AAT TAG GT |
| CRP | CAC TTC TAC ACG GAA CTG | AAT CTC ATT GTC TTG TCT CTT |
| RBP4 | CCC TGC CAA GTT CAA GAT | ACG ATC CAG TGG TCA TCA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, M.S.; Jeon, H.; Yoo, S.-M.; Lee, M.-S. Activation of the Complement System on Human Endothelial Cells by Urban Particulate Matter Triggers Inflammation-Related Protein Production. Int. J. Mol. Sci. 2021, 22, 3336. https://doi.org/10.3390/ijms22073336
Choi MS, Jeon H, Yoo S-M, Lee M-S. Activation of the Complement System on Human Endothelial Cells by Urban Particulate Matter Triggers Inflammation-Related Protein Production. International Journal of Molecular Sciences. 2021; 22(7):3336. https://doi.org/10.3390/ijms22073336
Chicago/Turabian StyleChoi, Myoung Su, Hyungtaek Jeon, Seung-Min Yoo, and Myung-Shin Lee. 2021. "Activation of the Complement System on Human Endothelial Cells by Urban Particulate Matter Triggers Inflammation-Related Protein Production" International Journal of Molecular Sciences 22, no. 7: 3336. https://doi.org/10.3390/ijms22073336
APA StyleChoi, M. S., Jeon, H., Yoo, S.-M., & Lee, M.-S. (2021). Activation of the Complement System on Human Endothelial Cells by Urban Particulate Matter Triggers Inflammation-Related Protein Production. International Journal of Molecular Sciences, 22(7), 3336. https://doi.org/10.3390/ijms22073336






