Molecular Markers of Kidney Transplantation Outcome: Current Omics Tools and Future Developments
Abstract
:1. Introduction
2. What Are Omics-Based Molecular Biomarkers?
3. Molecular Omics before Procurement
3.1. Genomics
3.2. Transcriptomics
3.3. Proteomics
3.4. Metabolomics
4. Molecular Omics after Transplantation
4.1. Genomics
4.2. Transcriptomics
4.3. Proteomics
4.4. Metabolomics
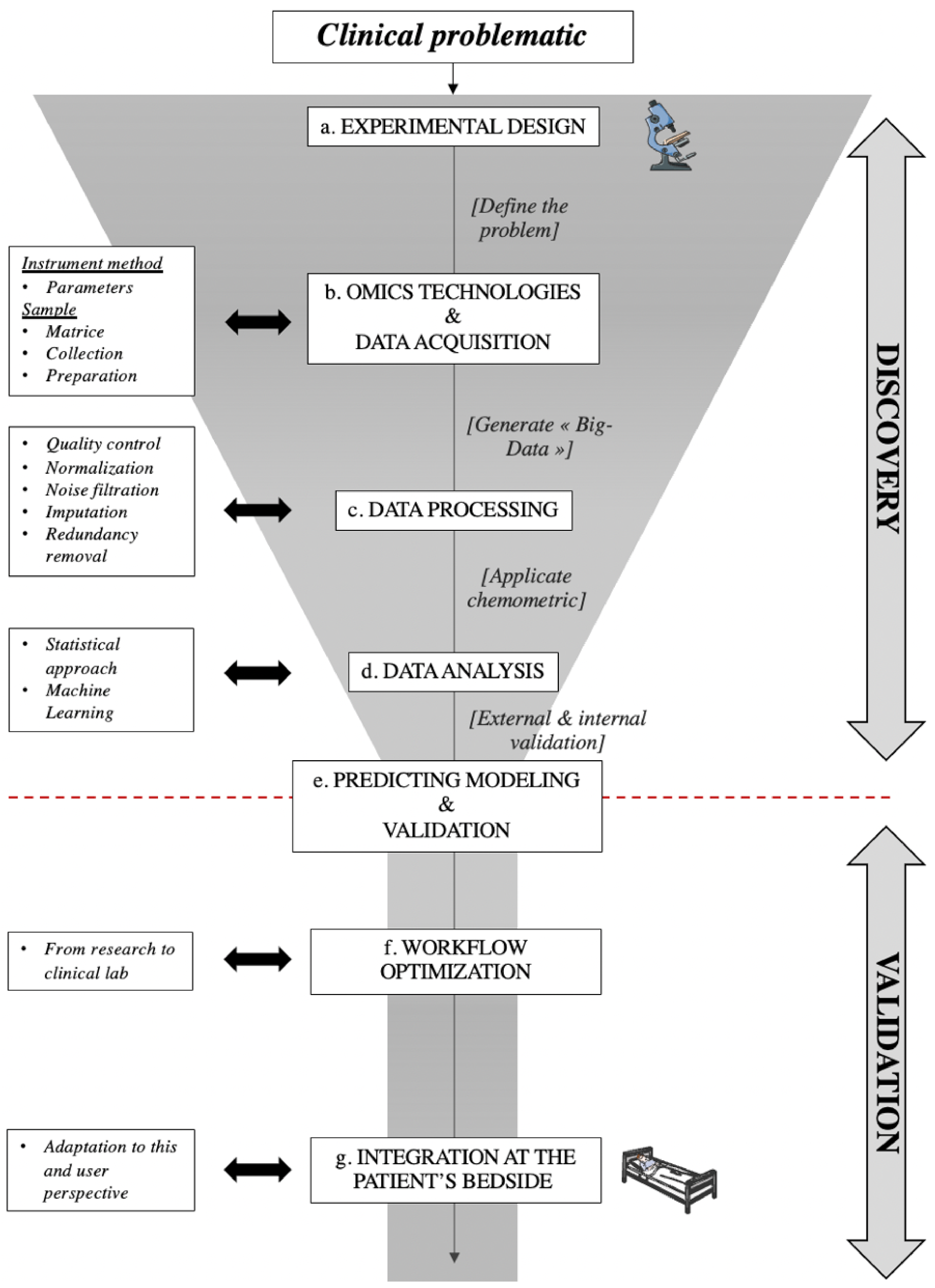
5. Toward an Optimized Use of Omics in Clinical Application: Workflow, Advantages, and Limits
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hariharan, S.; Johnson, C.P.; Bresnahan, B.A.; Taranto, S.E.; McIntosh, M.J.; Stablein, D. Improved Graft Survival after Renal Transplantation in the United States, 1988 to 1996. N. Engl. J. Med. 2000, 342, 605–612. [Google Scholar] [CrossRef]
- Jeon, K.-O.; Son, S.-Y.; Hahm, M.-I.; Kim, S.-I. Quality of Life among End-stage Renal Disease Treatments and Economic Evaluation of Renal Transplantation and Hemodialysis Treatments. J. Korean Soc. Transplant. 2015, 29, 200. [Google Scholar] [CrossRef] [Green Version]
- Williams, W.W.; Taheri, D.; Tolkoff-Rubin, N.; Colvin, R.B. Clinical Role of the Renal Transplant Biopsy. Nat. Rev. Nephrol. 2012, 8, 110–121. [Google Scholar] [CrossRef] [Green Version]
- Christians, U.; Klawitter, J.; Klawitter, J. Biomarkers in Transplantation—Proteomics and Metabolomics. Ther. Drug Monit. 2016, 38, S70–S74. [Google Scholar] [CrossRef] [Green Version]
- Salvadori, M.; Tsalouchos, A. Biomarkers in Renal Transplantation: An Updated Review. WJT 2017, 7, 161. [Google Scholar] [CrossRef]
- Biomarker. Available online: https://www.ema.europa.eu/en/glossary/biomarker (accessed on 2 June 2022).
- Califf, R.M. Biomarker Definitions and Their Applications. Exp. Biol. Med. 2018, 243, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Neagu, M.; Longo, C.; Ribero, S. Omics Landscape in Disease Biomarkers Discovery. Dis. Markers 2016, 2016, 4068252. [Google Scholar] [CrossRef]
- Roth, S.C. What is Genomic Medicine? J. Med. Libr. Assoc. 2019, 107, 442–448. [Google Scholar] [CrossRef]
- Fu, X.-D. Non-Coding RNA: A New Frontier in Regulatory Biology. Natl. Sci. Rev. 2014, 1, 190–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aslam, B.; Basit, M.; Nisar, M.A.; Khurshid, M.; Rasool, M.H. Proteomics: Technologies and Their Applications. J. Chromatogr. Sci. 2017, 55, 182–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, C.H.; Ivanisevic, J.; Siuzdak, G. Metabolomics: Beyond Biomarkers and towards Mechanisms. Nat. Rev. Mol. Cell Biol. 2016, 17, 451–459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Troppmann, C.; Gillingham, K.J.; Benedetti, E.; Almond, P.S.; Gruessner, R.W.G.; Najarian, J.S.; Matas, A.J. Delayed Graft Function, Acute Rejection, and Outcome After Cadaver Renal Transplantation: A Multivariate Analysis. Transplantation 1995, 59, 962–968. [Google Scholar] [CrossRef]
- Lee, A.P.K.; Abramowicz, D. Is the Kidney Donor Risk Index a Step Forward in the Assessment of Deceased Donor Kidney Quality? Nephrol. Dial. Transplant. 2015, 30, 1285–1290. [Google Scholar] [CrossRef] [Green Version]
- Dahmen, M.; Becker, F.; Pavenstädt, H.; Suwelack, B.; Schütte-Nütgen, K.; Reuter, S. Validation of the Kidney Donor Profile Index (KDPI) to Assess a Deceased Donor’s Kidneys’ Outcome in a European Cohort. Sci. Rep. 2019, 9, 11234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Genovese, G.; Friedman, D.J.; Ross, M.D.; Lecordier, L.; Uzureau, P.; Freedman, B.I.; Bowden, D.W.; Langefeld, C.D.; Oleksyk, T.K.; Knob, A.L.U.; et al. Association of Trypanolytic ApoL1 Variants with Kidney Disease in African Americans. Science 2010, 329, 841–845. [Google Scholar] [CrossRef] [Green Version]
- Freedman, B.I.; Pastan, S.O.; Israni, A.K.; Schladt, D.; Julian, B.A.; Gautreaux, M.D.; Hauptfeld, V.; Bray, R.A.; Gebel, H.M.; Kirk, A.D.; et al. APOL1 Genotype and Kidney Transplantation Outcomes from Deceased African American Donors. Transplantation 2016, 100, 194–202. [Google Scholar] [CrossRef]
- Hoffmann, S.; Park, J.; Jacobson, L.M.; Muehrer, R.J.; Lorentzen, D.; Kleiner, D.; Becker, Y.T.; Hullett, D.A.; Mannon, R.; Kirk, A.D.; et al. Donor Genomics Influence Graft Events: The Effect of Donor Polymorphisms on Acute Rejection and Chronic Allograft Nephropathy. Kidney Int. 2004, 66, 1686–1693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, J.; McKnight, A.J.; Döhler, B.; Simmonds, M.J.; Courtney, A.E.; Brand, O.J.; Briggs, D.; Ball, S.; Cockwell, P.; Patterson, C.C.; et al. Donor ABCB1 Variant Associates with Increased Risk for Kidney Allograft Failure. J. Am. Soc. Nephrol. 2012, 23, 1891–1899. [Google Scholar] [CrossRef] [Green Version]
- Hernandez-Fuentes, M.P.; Franklin, C.; Rebollo-Mesa, I.; Mollon, J.; Delaney, F.; Perucha, E.; Stapleton, C.; Borrows, R.; Byrne, C.; Cavalleri, G.; et al. Long- and Short-term Outcomes in Renal Allografts with Deceased Donors: A Large Recipient and Donor Genome-wide Association Study. Am. J. Transplant. 2018, 18, 1370–1379. [Google Scholar] [CrossRef]
- Halloran, P.F.; Einecke, G. Microarrays and Transcriptome Analysis in Renal Transplantation. Nat. Rev. Nephrol. 2006, 2, 2–3. [Google Scholar] [CrossRef] [PubMed]
- Archer, K.J.; Guennel, T. An Application for Assessing Quality of RNA Hybridized to Affymetrix GeneChips. Bioinformatics 2006, 22, 2699–2701. [Google Scholar] [CrossRef] [PubMed]
- Hauser, P.; Schwarz, C.; Mitterbauer, C.; Regele, H.M.; Mühlbacher, F.; Mayer, G.; Perco, P.; Mayer, B.; Meyer, T.W.; Oberbauer, R. Genome-Wide Gene-Expression Patterns of Donor Kidney Biopsies Distinguish Primary Allograft Function. Lab. Investig. 2004, 84, 353–361. [Google Scholar] [CrossRef]
- Mueller, T.F.; Reeve, J.; Jhangri, G.S.; Mengel, M.; Jacaj, Z.; Cairo, L.; Obeidat, M.; Todd, G.; Moore, R.; Famulski, K.S.; et al. The Transcriptome of the Implant Biopsy Identifies Donor Kidneys at Increased Risk of Delayed Graft Function. Am. J. Transplant. 2007, 8, 78–85. [Google Scholar] [CrossRef]
- Mas, V.R.; Archer, K.J.; Yanek, K.; Dumur, C.I.; Capparuccini, M.I.; Mangino, M.J.; King, A.; Gibney, E.M.; Fisher, R.; Posner, M.; et al. Gene Expression Patterns in Deceased Donor Kidneys Developing Delayed Graft Function After Kidney Transplantation. Transplantation 2008, 85, 626–635. [Google Scholar] [CrossRef] [PubMed]
- Mas, V.R.; Scian, M.J.; Archer, K.J.; Suh, J.L.; David, K.G.; Ren, Q.; Gehr, T.W.B.; King, A.L.; Posner, M.P.; Mueller, T.F.; et al. Pretransplant Transcriptome Profiles Identify among Kidneys with Delayed Graft Function Those with Poorer Quality and Outcome. Mol. Med. 2011, 17, 1311–1322. [Google Scholar] [CrossRef]
- Zhang, W.; Yi, Z.; Wei, C.; Keung, K.L.; Sun, Z.; Xi, C.; Woytovich, C.; Farouk, S.; Gallon, L.; Menon, M.C.; et al. Pretransplant Transcriptomic Signature in Peripheral Blood Predicts Early Acute Rejection. JCI Insight 2019, 4, e127543. [Google Scholar] [CrossRef] [Green Version]
- Snoeijs, M.G.J.; Pulinx, B.; van Dieijen-Visser, M.P.; Buurman, W.A.; van Heurn, L.W.E.; Wodzig, W.K.W.H. Characterization of the Perfusate Proteome of Human Donor Kidneys. Ann. Clin. Biochem. 2013, 50, 140–146. [Google Scholar] [CrossRef]
- Koo, T.Y.; Jeong, J.C.; Lee, Y.; Ko, K.-P.; Lee, K.-B.; Lee, S.; Park, S.J.; Park, J.B.; Han, M.; Lim, H.J.; et al. Pre-Transplant Evaluation of Donor Urinary Biomarkers Can Predict Reduced Graft Function After Deceased Donor Kidney Transplantation. Medicine 2016, 95, e3076. [Google Scholar] [CrossRef] [PubMed]
- Gagnebin, Y.; Pezzatti, J.; Lescuyer, P.; Boccard, J.; Ponte, B.; Rudaz, S. Combining the Advantages of Multilevel and Orthogonal Partial Least Squares Data Analysis for Longitudinal Metabolomics: Application to Kidney Transplantation. Anal. Chim. Acta 2020, 1099, 26–38. [Google Scholar] [CrossRef]
- Kvietkauskas, M.; Zitkute, V.; Leber, B.; Strupas, K.; Stiegler, P.; Schemmer, P. The Role of Metabolomics in Current Concepts of Organ Preservation. IJMS 2020, 21, 6607. [Google Scholar] [CrossRef]
- Loupy, A.; Aubert, O.; Orandi, B.J.; Naesens, M.; Bouatou, Y.; Raynaud, M.; Divard, G.; Jackson, A.M.; Viglietti, D.; Giral, M.; et al. Prediction System for Risk of Allograft Loss in Patients Receiving Kidney Transplants: International Derivation and Validation Study. BMJ 2019, 366, l4923. [Google Scholar] [CrossRef] [Green Version]
- Raynaud, M.; Aubert, O.; Divard, G.; Reese, P.P.; Kamar, N.; Yoo, D.; Chin, C.-S.; Bailly, É.; Buchler, M.; Ladrière, M.; et al. Dynamic Prediction of Renal Survival among Deeply Phenotyped Kidney Transplant Recipients Using Artificial Intelligence: An Observational, International, Multicohort Study. Lancet Digit. Health 2021, 3, e795–e805. [Google Scholar] [CrossRef]
- Pahl, E.S.; Street, W.N.; Johnson, H.J.; Reed, A.I. A Predictive Model for Kidney Transplant Graft Survival Using Machine Learning. Comput. Sci. Inf. Technol. CSIT 2020, 10, 99–108. [Google Scholar] [CrossRef]
- Montero, N.; Codina, S.; Cruzado, J.M. Prediction Scores for Risk of Allograft Loss in Patients Receiving Kidney Transplants: Nil Satis Nisi Optimum. Clin. Kidney J. 2020, 13, 745–748. [Google Scholar] [CrossRef]
- Oetting, W.S.; Dorr, C.; Remmel, R.P.; Matas, A.J.; Israni, A.K.; Jacobson, P.A. Concepts of Genomics in Kidney Transplantation. Curr. Transpl. Rep. 2017, 4, 116–123. [Google Scholar] [CrossRef]
- Sarwal, M.; Chua, M.-S.; Kambham, N.; Hsieh, S.-C.; Satterwhite, T.; Masek, M.; Salvatierra, O. Molecular Heterogeneity in Acute Renal Allograft Rejection Identified by DNA Microarray Profiling. N. Engl. J. Med. 2003, 349, 125–138. [Google Scholar] [CrossRef] [Green Version]
- O’Connell, P.J.; Zhang, W.; Menon, M.C.; Yi, Z.; Schröppel, B.; Gallon, L.; Luan, Y.; Rosales, I.A.; Ge, Y.; Losic, B.; et al. Biopsy Transcriptome Expression Profiling to Identify Kidney Transplants at Risk of Chronic Injury: A Multicentre, Prospective Study. Lancet 2016, 388, 983–993. [Google Scholar] [CrossRef] [Green Version]
- Dorr, C.R.; Oetting, W.S.; Jacobson, P.A.; Israni, A.K. Genetics of Acute Rejection after Kidney Transplantation. Transpl. Int. 2018, 31, 263–277. [Google Scholar] [CrossRef] [Green Version]
- O’Brien, R.P.; Phelan, P.J.; Conroy, J.; O’Kelly, P.; Green, A.; Keogan, M.; O’Neill, D.; Jennings, S.; Traynor, C.; Casey, J.; et al. A Genome-Wide Association Study of Recipient Genotype and Medium-Term Kidney Allograft Function. Clin. Transplant. 2013, 27, 379–387. [Google Scholar] [CrossRef]
- Li, B.; Hartono, C.; Ding, R.; Sharma, V.K.; Ramaswamy, R.; Qian, B.; Serur, D.; Mouradian, J.; Schwartz, J.E.; Suthanthiran, M. Noninvasive Diagnosis of Renal-Allograft Rejection by Measurement of Messenger RNA for Perforin and Granzyme B in Urine. N. Engl. J. Med. 2001, 344, 947–954. [Google Scholar] [CrossRef]
- Mueller, T.F.; Einecke, G.; Reeve, J.; Sis, B.; Mengel, M.; Jhangri, G.S.; Bunnag, S.; Cruz, J.; Wishart, D.; Meng, C.; et al. Microarray Analysis of Rejection in Human Kidney Transplants Using Pathogenesis-Based Transcript Sets. Am. J. Transplant. 2007, 7, 2712–2722. [Google Scholar] [CrossRef]
- The PLOS Medicine Staff Correction: The KSORT Assay to Detect Renal Transplant Patients at High Risk for Acute Rejection: Results of the Multicenter AART Study. PLoS Med. 2015, 12, e1001790. [CrossRef] [Green Version]
- Roedder, S.; Sigdel, T.; Salomonis, N.; Hsieh, S.; Dai, H.; Bestard, O.; Metes, D.; Zeevi, A.; Zeevi, A.; Gritsch, A.; et al. The KSORT Assay to Detect Renal Transplant Patients at High Risk for Acute Rejection: Results of the Multicenter AART Study. PLoS Med. 2014, 11, e1001759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Loon, E.; Giral, M.; Anglicheau, D.; Lerut, E.; Dubois, V.; Rabeyrin, M.; Brouard, S.; Roedder, S.; Spigarelli, M.G.; Rabant, M.; et al. Diagnostic Performance of KSORT, a Blood-based MRNA Assay for Noninvasive Detection of Rejection after Kidney Transplantation: A Retrospective Multicenter Cohort Study. Am. J. Transplant. 2021, 21, 740–750. [Google Scholar] [CrossRef]
- Kumar, J.; Contrepois, K.; Snyder, M.; Grimm, P.C.; Moudgil, A.; Smith, J.M.; Bobrowski, A.E.; Verghese, P.S.; Hooper, D.; Ingulli, E.; et al. Design and Methods of the Validating Injury to the Renal Transplant Using Urinary Signatures (VIRTUUS) Study in Children. Transplant. Direct 2021, 7, e791. [Google Scholar] [CrossRef]
- Rabant, M.; Amrouche, L.; Lebreton, X.; Aulagnon, F.; Benon, A.; Sauvaget, V.; Bonifay, R.; Morin, L.; Scemla, A.; Delville, M.; et al. Urinary C-X-C Motif Chemokine 10 Independently Improves the Noninvasive Diagnosis of Antibody–Mediated Kidney Allograft Rejection. JASN 2015, 26, 2840–2851. [Google Scholar] [CrossRef] [Green Version]
- Suhail, S.M. Significance of Urinary Proteome Pattern in Renal Allograft Recipients. J. Transplant. 2014, 2014, 139361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stanimirova, I.; Banasik, M.; Ząbek, A.; Dawiskiba, T.; Kościelska-Kasprzak, K.; Wojtowicz, W.; Krajewska, M.; Janczak, D.; Młynarz, P. Serum Metabolomics Approach to Monitor the Changes in Metabolite Profiles Following Renal Transplantation. Sci. Rep. 2020, 10, 17223. [Google Scholar] [CrossRef]
- Banon-Maneus, E.; Quintana, L.F.; Campistol, J.M. Urinary Proteomics and Renal Transplantation. In Kidney Transplantation–New Perspectives; Trzcinska, M., Ed.; InTech: London, UK, 2011; ISBN 978-953-307-684-3. [Google Scholar]
- Kim, M.; Tagkopoulos, I. Data Integration and Predictive Modeling Methods for Multi-Omics Datasets. Mol. Omics 2018, 14, 8–25. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Sarwal, M.M. Computational Models for Transplant Biomarker Discovery. Front. Immunol. 2015, 6, 458. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Lu, Y.; Guo, Y.; Cao, H.; Wang, Q.; Shui, W. Comprehensive Evaluation of Untargeted Metabolomics Data Processing Software in Feature Detection, Quantification and Discriminating Marker Selection. Anal. Chim. Acta 2018, 1029, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, S.L.C. Experimental Design. In Reference Module in Chemistry, Molecular Sciences and Chemical Engineering; Elsevier: Amsterdam, The Netherlands, 2018; p. 9780124095472144000. ISBN 978-0-12-409547-2. [Google Scholar]
- Fernandez-Delgado, M. Do We Need Hundreds of Classifiers to Solve Real World Classification Problems? J. Mach. Learn. Res. 2014, 15, 3133–3181. [Google Scholar]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G. Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD): The TRIPOD Statement. BMC Med. 2015, 13, 1. [Google Scholar] [CrossRef] [Green Version]
- Bohra, R.; Klepacki, J.; Klawitter, J.; Klawitter, J.; Thurman, J.M.; Christians, U. Proteomics and Metabolomics in Renal Transplantation-Quo Vadis? Transpl. Int. 2013, 26, 225–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaboré, R.; Haller, M.C.; Harambat, J.; Heinze, G.; Leffondré, K. Risk Prediction Models for Graft Failure in Kidney Transplantation: A Systematic Review. Nephrol. Dial. Transplant. 2017, 32, ii68–ii76. [Google Scholar] [CrossRef] [Green Version]
- Sautenet, B.; Tong, A.; Manera, K.; Chapman, J.; Warrens, A.; Rosenbloom, D.; Wong, G.; Gill, J.; Rostaing, L.; Josephson, M.; et al. Développement d’un consensus sur les critères de jugement à utiliser dans les essais de transplantation rénale: Une enquête Delphi internationale basée sur l’opinion partagée des patients, aidants et professionnels de santé. Néphrol. Thér. 2017, 13, 289. [Google Scholar] [CrossRef]
- Dharnidharka, V.R.; Malone, A. Biomarkers to Detect Rejection after Kidney Transplantation. Pediatr. Nephrol. 2018, 33, 1113–1122. [Google Scholar] [CrossRef]
- Weiss, R.H.; Kim, K. Metabolomics in the Study of Kidney Diseases. Nat. Rev. Nephrol. 2012, 8, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Cristoferi, I.; Giacon, T.A.; Boer, K.; van Baardwijk, M.; Neri, F.; Campisi, M.; Kimenai, H.J.A.N.; Clahsen-van Groningen, M.C.; Pavanello, S.; Furian, L.; et al. The Applications of DNA Methylation as a Biomarker in Kidney Transplantation: A Systematic Review. Clin. Epigenet. 2022, 14, 20. [Google Scholar] [CrossRef] [PubMed]
- Shen, Z.; Lin, J.; Teng, J.; Zhuang, Y.; Zhang, H.; Wang, C.; Zhang, Y.; Ding, X.; Zhang, X. Association of Urinary Ionomic Profiles and Acute Kidney Injury and Mortality in Patients after Cardiac Surgery. J. Thorac. Cardiovasc. Surg. 2020, 159, 918–926. [Google Scholar] [CrossRef]
- Khatri, P.; Sarwal, M.M.; Butte, A.J. Applications of Translational Bioinformatics in Transplantation. Clin. Pharm. Ther. 2011, 90, 323–327. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Predictive Model Approach | Markers, Molecules, Roles | Sample Type | Performance | Limitation | Ref. |
|---|---|---|---|---|---|
| KDPI | Age, height, weight, last serum creatinine, history of diabetes, hypertension, HCV-infection, ethnicity, and the cause of death | Blood | Prediction of graft failure (AUC 0.6) | Not validated in European cohorts, low c statistics | [14,15] |
| Genomics | APOL1 polymorphism, involved in the formation of most cholesteryl esters in plasma and also promotes efflux of cholesterol from cells | Blood | Significantly associated with worse outcome (p < 0.0001), now integrated to KDPI | Limited to patient of african descent | [16,17] |
| Polymorphisms of TGF-β and CCR5, role in inflammation | Blood | no consistent association with acute rejection | Small cohorts | [18] | |
| Transcriptomics | 48 mRNA coding for cell communication, apoptosis, inflammation | Biospy | correlation with risk of graft failure | Limited number of samples | [19] |
| Molecular pannel of 1051 transcripts; overexpression of molecules related to inflammation (immunoglobulins), collagens, integrins, chemokines, Toll-like receptor signaling, antigen processing and presentation and renal injury; underexpression of markers of transport, glucose, fatty acid and amino acid metabolism | Biospy | Many molecules differentiated between organs from deceased donors vs. living donors (adjusted p-value <0.01) | Small cohorts and short duration of follow-up | [20] | |
| 36 candidate genes, chief among which IGFBP5 and CSNK2A2 (cell cycle/growth); RASGRP3 (signal transduction); CD83, BCL3, MX1, TNFRSF1B (immune response); ENPP4, GBA3 (metabolism) | Biospy | Significantly associated with stratification of graft performance in correlation with recipient’s DGF (p < 0.001) | Small cohorts | [21] | |
| Molecular pannel associated with antigen processing and presentation via MHC class I/II, T-cell–mediated cytotoxicity, allograft rejection/graft versus host disease, antigen processing and presentation and cell adhesion molecules. Top molecules were HLA-G, HLA-E, HLA-DRB1, HLA-DRA, HLA-DPB1, HLA-DPA1, HLA-DQB1, HLA-DQA1, HLA-B, HLA-C, HLA-DMA, PSMB8, PSME1, HSP90AB1, and PRDX1 | Biospy | Significantly associated with DGF severity (p < 0.001) | Small cohorts | [22] | |
| 23-gene transcriptional signature associated with NK and CD8+ T cell activation, among which Granzyme B, FGFBP2, NKG7, Perforin 1, Fas Ligand, CD8A, CCR5, coagulation factor XII | Blood | Risk score associated with acute cellular rejection after 6 months, antibody-mediated rejection and/or de novo donor-specific antibodies, and graft loss (AUC 0.89) | No standardization | [23] | |
| Proteomics | Predictive model using Neutrophil gelatinase-associated lipocalin (NGAL) and L-type fatty acid binding protein (L-FABP) | Urine | Prediction of reduced graft function (AUC 0.8) | Small cohorts | [24] |
| Metabolomics | 266 plasma metabolites building ANOVA multiblock OPLS models, the main molecules being azelaic acid, creatinine, kynurenic acid, kynurenine, indoxyl sulfate and tryptophan | Blood | Significantly associated with rejection (p < 0.005) | Data interpretation and small cohorts | [25] |
| Review on metabolomics investigation during perfusion for the heart, lung, kidney and liver. Biomarkers molecules mainly associated with energy metabolim (ATP → Pi, Krebs cycle intermediates, lactate), glycogenolysis, amino acids metabolism, | Measurable association with graft quality | Small cohorts | [26] |
| Predictive model approach | Markers, Molecules, Roles | Sample Type | Performance | Limitation | Ref |
|---|---|---|---|---|---|
| Genomics | Pannel of 13 genes : MET, ST5 and KAAG1 (tumor development or suppression); RNF149, ASB15, KLH13 (ubiquitination and proteasome) ; TGIF1, SPRY4, WNT9A, RXRA and FJX1 (developmental or growth pathways such as NOTCH/Wnt or RAR); CHCHD10 and SERINC5 (energy and membrane repair) | Biopsy | Prediction of the development of fibrosis at 1 year (AUC 0.9) | No validation yet, clinical trial ongoing | [36] |
| Polymorphism of several genes such as CYP3A5 (involved in drug metabolisation, among which tacrolimus), CCR5, FOXP3 and other genes involved in inflammation and immune response (interleukines, chemokines, TLR pathway, innate and adaptative immunity mediators); TGF b, VEGF and other mediators of fibrosis. | Biopsy | Several variants are predictors of long-term allograft function (p = 0.004) | Very small sample set (24 specimens) | [37] | |
| Transcriptomics | Non-invasive urinary cell mRNAs Granzyme B, Perforin, Cyclophilin B, all related to the immune system and inflammation | Urine | Significantly associated with acute rejection (p < 0.001) | Small cohort | [38] |
| The kSORT pannel: 17-gene transcriptional signature to predict acute rejection DUSP1, CFLAR, ITGAX, NAMPT, MAPK9, PSEN1, RYBP, NKTR, SLC25A37, CEACAM4, RARA, RXRA, EPOR, GZMK, and RHEB) together with 18S ribosomal RNA as housekeeping gene. This signature is mainly directed at defining the type and intensity of the inflammatory response | Blood | Prediction of Acute Rejection (AUC = 0.93) | No validation on an independent sample set. Indeed, an independant study showed that adding kSORT to classical clinical variables (eGFR, Proteinuria, DSA) did not increase their diagnostic performance [39] | [40,41] | |
| The VIRTUUS panel: 3 genes (18S-normalized CD3ε, CXCL10 mRNA, and 18S ribosomal RNA) associated with inflammation and immune response | Blood | No result yet | This is a design & method presentation of an ongoing clinical trial | [42] | |
| Proteomics | Urinary levels of CXCL9 and CXCL10 proteins, both linked to inflammation signaling | Urine | Prediction of T cell-mediated rejection (TCMR) and antibody-mediated rejection (ABMR) (AUC: 0.75 and 0.83 respectively) | Prospective cohort study | [43] |
| Metabolomics | None significant studies |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lepoittevin, M.; Kerforne, T.; Pellerin, L.; Hauet, T.; Thuillier, R. Molecular Markers of Kidney Transplantation Outcome: Current Omics Tools and Future Developments. Int. J. Mol. Sci. 2022, 23, 6318. https://doi.org/10.3390/ijms23116318
Lepoittevin M, Kerforne T, Pellerin L, Hauet T, Thuillier R. Molecular Markers of Kidney Transplantation Outcome: Current Omics Tools and Future Developments. International Journal of Molecular Sciences. 2022; 23(11):6318. https://doi.org/10.3390/ijms23116318
Chicago/Turabian StyleLepoittevin, Maryne, Thomas Kerforne, Luc Pellerin, Thierry Hauet, and Raphael Thuillier. 2022. "Molecular Markers of Kidney Transplantation Outcome: Current Omics Tools and Future Developments" International Journal of Molecular Sciences 23, no. 11: 6318. https://doi.org/10.3390/ijms23116318
APA StyleLepoittevin, M., Kerforne, T., Pellerin, L., Hauet, T., & Thuillier, R. (2022). Molecular Markers of Kidney Transplantation Outcome: Current Omics Tools and Future Developments. International Journal of Molecular Sciences, 23(11), 6318. https://doi.org/10.3390/ijms23116318








