Elevated Alpha 1(I) to Alpha 2(I) Collagen Ratio in Dermal Fibroblasts Possibly Contributes to Fibrosis in Systemic Sclerosis
Abstract
:1. Introduction
2. Results
2.1. The Ratio of α1(I) and α2(I) Collagen Is Increased in SSc Dermal Fibroblasts
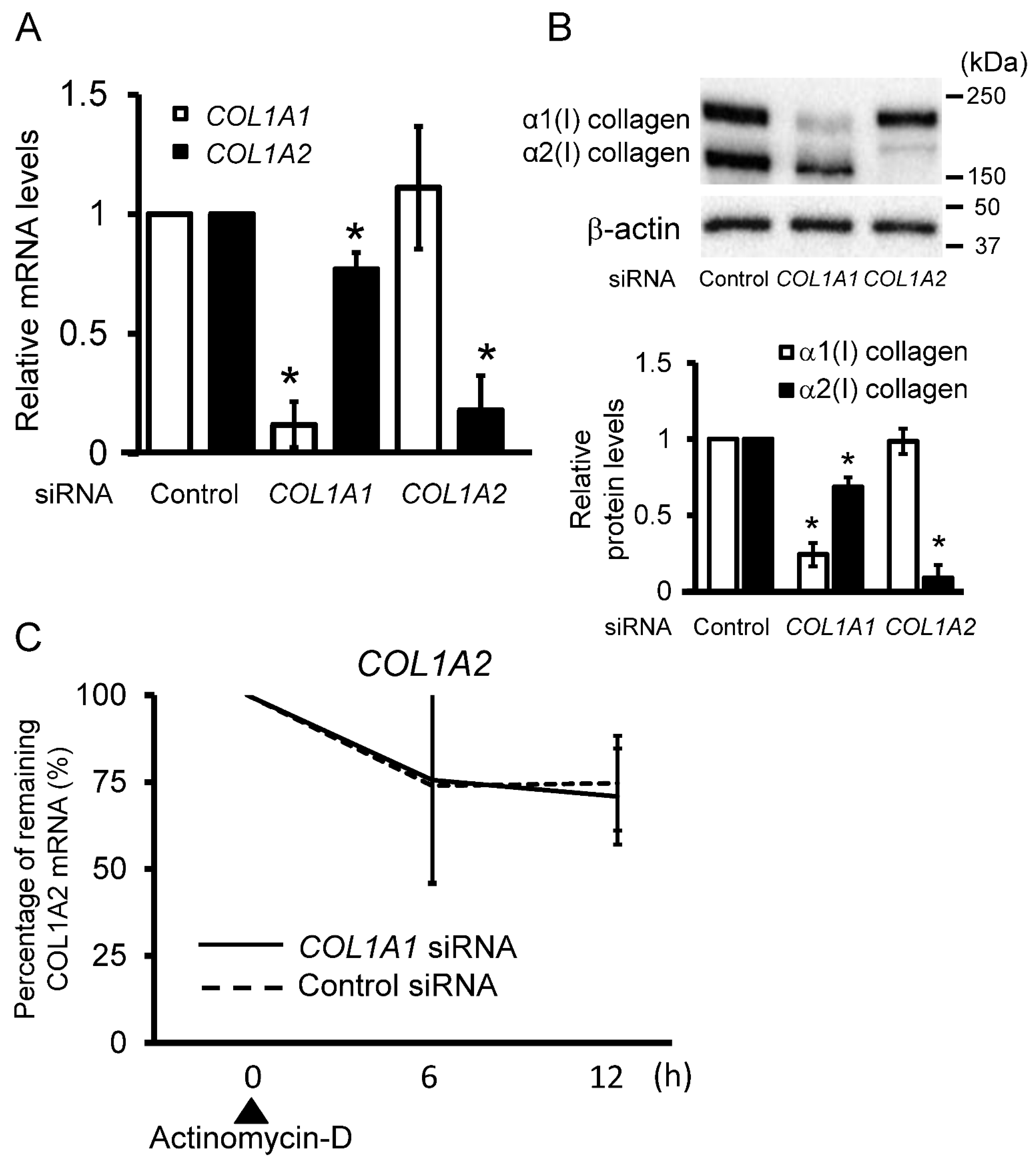
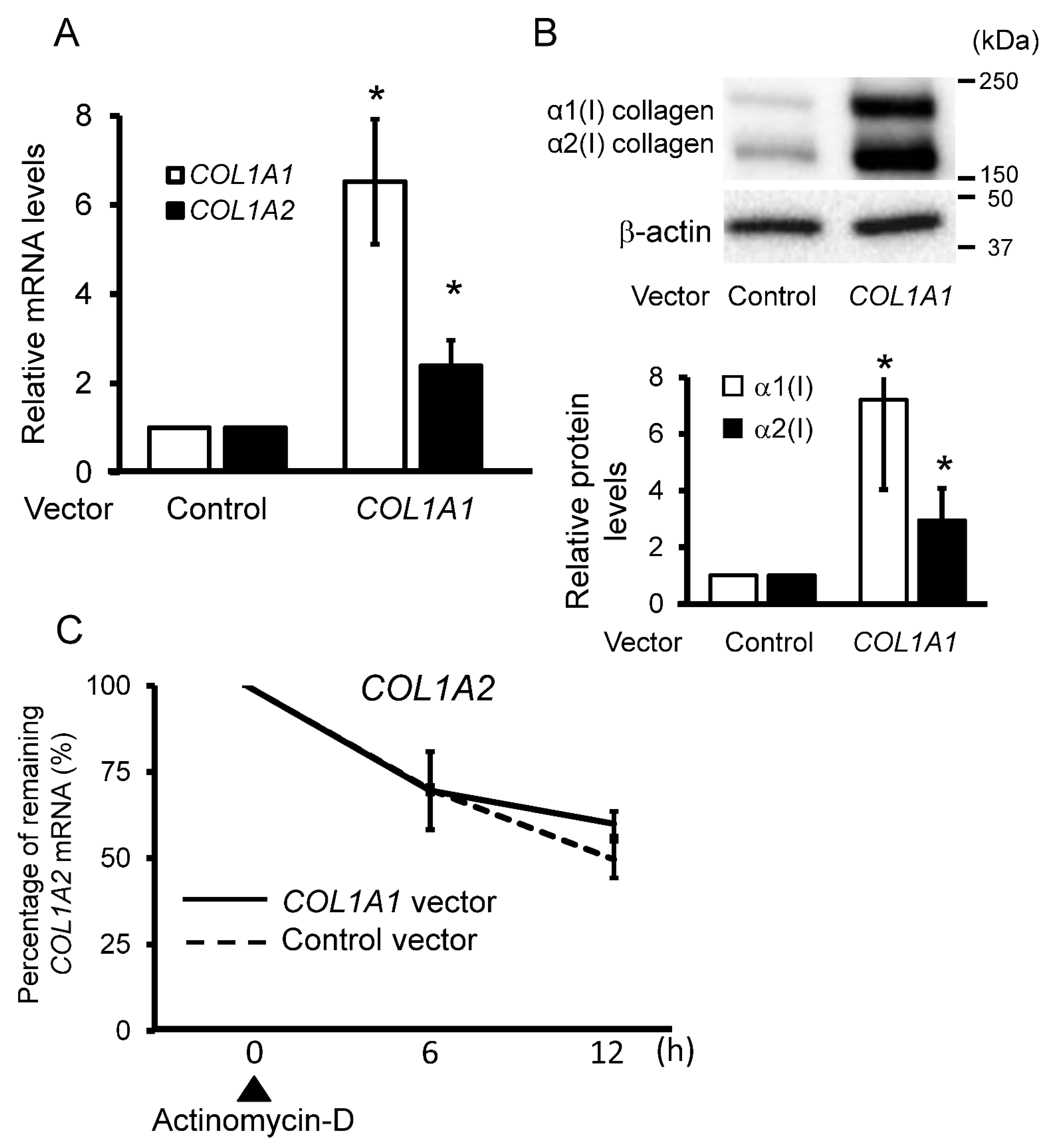
2.2. Forced Expression of α1(I) Collagen Affects α2(I) Collagen Expression in Control Dermal Fibroblasts
2.3. Local Administration of COL1A1 siRNA Attenuates Skin Fibrosis in a Bleomycin-Induced SSc Mouse Model
3. Discussion
4. Materials and Methods
4.1. Reagents
4.2. Cell Cultures
4.3. RNA Extraction, Reverse Transcription, and PCR Analysis of RNA Expression
4.4. Immunoblotting
4.5. Transient Transfection
4.6. Lentiviral Gene Transfer
4.7. Mice
4.8. Bleomycin Treatment in Mice
4.9. Measurement of Collagen Production in Mouse Skin
4.10. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ECM | extracellular matrix |
| siRNA | small interfering RNA |
| SSc | systemic sclerosis |
| TGF-β | transforming growth factor-β |
References
- Korn, J. Immunologic aspects of scleroderma. Curr. Opin. Rheumatol. 1989, 1, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Mauch, C.; Kreig, T. Fibroblast-matrix interactions and their role in the pathogenesis of fibrosis. Rheum. Dis. Clin. N. Am. 1990, 16, 93–107. [Google Scholar] [CrossRef]
- Trojanowska, M.; LeRoy, E.C.; Eckes, B.; Krieg, T. Pathogenesis of fibrosis: Type 1 collagen and the skin. J. Mol. Med. 1998, 76, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Roberts, A.B.; Sporn, M.B.; Assoian, R.K.; Smith, J.M.; Roche, N.S.; Wakefield, L.M.; Heine, U.I.; Liotta, L.A.; Falanga, V.; Kehrl, J.H.; et al. Transforming growth factor type beta: Rapid induction of fibrosis and angiogenesis in vivo and stimulation of collagen formation in vitro. Proc. Natl. Acad. Sci. USA 1986, 83, 4167–4171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberts, A.B.; Heine, U.I.; Flanders, K.C.; Sporn, M.B. Transforming growth factor-beta. Major role in regulation of extracellular matrix. Ann. N. Y. Acad. Sci. 1990, 580, 225–232. [Google Scholar] [CrossRef]
- Ihn, H. Autocrine TGF-beta signaling in the pathogenesis of systemic sclerosis. J. Dermatol. Sci. 2008, 49, 103–113. [Google Scholar] [CrossRef]
- Kivirikko, K.I. Collagen biosynthesis: A mini-review cluster. Matrix Biol. 1998, 16, 355–356. [Google Scholar] [CrossRef]
- Huerre, C.; Junien, C.; Weil, D.; Chu, M.L.; Morabito, M.; Van Cong, N.; Myers, J.C.; Foubert, C.; Gross, M.S.; Prockop, D.J.; et al. Human type I procollagen genes are located on different chromosomes. Proc. Natl. Acad. Sci. USA 1982, 79, 6627–6630. [Google Scholar] [CrossRef] [Green Version]
- Yamada, Y.; Mudryj, M.; de Crombrugghe, B. A uniquely conserved regulatory signal is found around the translation initiation site in three different collagen genes. J. Biol. Chem. 1983, 258, 14914–14919. [Google Scholar] [CrossRef]
- Fleischmajer, R.; Damiano, V.; Nedwich, A. Scleroderma and the subcutaneous tissue. Science 1971, 171, 1019–1021. [Google Scholar] [CrossRef]
- Moinzadeh, P.; Agarwal, P.; Bloch, W.; Orteu, C.; Hunzelmann, N.; Eckes, B.; Krieg, T. Systemic sclerosis with multiple nodules: Characterization of the extracellular matrix. Arch. Dermatol. Res. 2013, 305, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Fleischmajer, R.; Gay, S.; Perlish, J.S.; Cesarini, J.P. Immunoelectron microscopy of type III collagen in normal and scleroderma skin. J. Investig. Dermatol. 1980, 75, 189–191. [Google Scholar] [CrossRef] [PubMed]
- Rice, L.M.; Padilla, C.M.; McLaughlin, S.R.; Mathes, A.; Ziemek, J.; Goummih, S.; Nakerakanti, S.; York, M.; Farina, G.; Whitfield, M.L.; et al. Fresolimumab treatment decreases biomarkers and improves clinical symptoms in systemic sclerosis patients. J. Clin. Investig. 2015, 125, 2795–2807. [Google Scholar] [CrossRef]
- Xiao, R.; Liu, F.Y.; Luo, J.Y.; Yang, X.J.; Wen, H.Q.; Su, Y.W.; Yan, K.L.; Li, Y.P.; Liang, Y.S. Effect of small interfering RNA on the expression of connective tissue growth factor and type I and III collagen in skin fibroblasts of patients with systemic sclerosis. Br. J. Dermatol. 2006, 155, 1145–1153. [Google Scholar] [CrossRef] [PubMed]
- Pannu, J.; Gardner, H.; Shearstone, J.R.; Smith, E.; Trojanowska, M. Increased levels of transforming growth factor beta receptor type I and up-regulation of matrix gene program: A model of scleroderma. Arthritis Rheum. 2006, 54, 3011–3021. [Google Scholar] [CrossRef] [PubMed]
- Morris, E.; Chrobak, I.; Bujor, A.; Hant, F.; Mummery, C.; Ten Dijke, P.; Trojanowska, M. Endoglin promotes TGF-beta/Smad1 signaling in scleroderma fibroblasts. J. Cell Physiol. 2011, 226, 3340–3348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bujor, A.M.; Pannu, J.; Bu, S.; Smith, E.A.; Muise-Helmericks, R.C.; Trojanowska, M. Akt blockade downregulates collagen and upregulates MMP1 in human dermal fibroblasts. J. Investig. Dermatol. 2008, 128, 1906–1914. [Google Scholar] [CrossRef] [Green Version]
- Honda, N.; Jinnin, M.; Kajihara, I.; Makino, T.; Makino, K.; Masuguchi, S.; Fukushima, S.; Okamoto, Y.; Hasegawa, M.; Fujimoto, M.; et al. TGF-beta-mediated downregulation of microRNA-196a contributes to the constitutive upregulated type I collagen expression in scleroderma dermal fibroblasts. J. Immunol. 2012, 188, 3323–3331. [Google Scholar] [CrossRef] [Green Version]
- Bailey, A.J.; Knott, L. Molecular changes in bone collagen in osteoporosis and osteoarthritis in the elderly. Exp. Gerontol. 1999, 34, 337–351. [Google Scholar] [CrossRef]
- Mann, V.; Hobson, E.E.; Li, B.; Stewart, T.L.; Grant, S.F.; Robins, S.P.; Aspden, R.M.; Ralston, S.H. A COL1A1 Sp1 binding site polymorphism predisposes to osteoporotic fracture by affecting bone density and quality. J. Clin. Investig. 2001, 107, 899–907. [Google Scholar] [CrossRef] [Green Version]
- Pucci-Minafra, I.; Andriolo, M.; Basirico, L.; Alessandro, R.; Luparello, C.; Buccellato, C.; Garbelli, R.; Minafra, S. Absence of regular alpha2(I) collagen chains in colon carcinoma biopsy fragments. Carcinogenesis 1998, 19, 575–584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McBride, D.J., Jr.; Choe, V.; Shapiro, J.R.; Brodsky, B. Altered collagen structure in mouse tail tendon lacking the alpha 2(I) chain. J. Mol. Biol. 1997, 270, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Misof, K.; Landis, W.J.; Klaushofer, K.; Fratzl, P. Collagen from the osteogenesis imperfecta mouse model (oim) shows reduced resistance against tensile stress. J. Clin. Investig. 1997, 100, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, A.S.; Meyers, D.F.; Page, R.C.; Welgus, H.G. Action of mammalian collagenases on type I trimer collagen. Coll. Relat. Res. 1984, 4, 289–296. [Google Scholar] [CrossRef]
- Makareeva, E.; Han, S.; Vera, J.C.; Sackett, D.L.; Holmbeck, K.; Phillips, C.L.; Visse, R.; Nagase, H.; Leikin, S. Carcinomas contain a matrix metalloproteinase-resistant isoform of type I collagen exerting selective support to invasion. Cancer Res. 2010, 70, 4366–4374. [Google Scholar] [CrossRef] [Green Version]
- Dzobo, K.; Leaner, V.D.; Parker, M.I. Feedback regulation of the alpha2(1) collagen gene via the Mek-Erk signaling pathway. IUBMB Life 2012, 64, 87–98. [Google Scholar] [CrossRef]
- Van Rooij, E.; Sutherland, L.B.; Thatcher, J.E.; DiMaio, J.M.; Naseem, R.H.; Marshall, W.S.; Hill, J.A.; Olson, E.N. Dysregulation of microRNAs after myocardial infarction reveals a role of miR-29 in cardiac fibrosis. Proc. Natl. Acad. Sci. USA 2008, 105, 13027–13032. [Google Scholar] [CrossRef] [Green Version]
- Verma, U.N.; Surabhi, R.M.; Schmaltieg, A.; Becerra, C.; Gaynor, R.B. Small interfering RNAs directed against beta-catenin inhibit the in vitro and in vivo growth of colon cancer cells. Clin. Cancer Res. 2003, 9, 1291–1300. [Google Scholar]
- Takeshita, F.; Minakuchi, Y.; Nagahara, S.; Honma, K.; Sasaki, H.; Hirai, K.; Teratani, T.; Namatame, N.; Yamamoto, Y.; Hanai, K.; et al. Efficient delivery of small interfering RNA to bone-metastatic tumors by using atelocollagen in vivo. Proc. Natl. Acad. Sci. USA 2005, 102, 12177–12182. [Google Scholar] [CrossRef] [Green Version]
- Whitehead, K.A.; Langer, R.; Anderson, D.G. Knocking down barriers: Advances in siRNA delivery. Nat. Rev. Drug Discov. 2009, 8, 129–138. [Google Scholar] [CrossRef]
- Wang, J.C.; Lai, S.; Guo, X.; Zhang, X.; de Crombrugghe, B.; Sonnylal, S.; Arnett, F.C.; Zhou, X. Attenuation of fibrosis in vitro and in vivo with SPARC siRNA. Arthritis Res. Ther. 2010, 12, R60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vollmann, E.H.; Cao, L.; Amatucci, A.; Reynolds, T.; Hamann, S.; Dalkilic-Liddle, I.; Cameron, T.O.; Hossbach, M.; Kauffman, K.J.; Mir, F.F.; et al. Identification of Novel Fibrosis Modifiers by In Vivo siRNA Silencing. Mol. Ther. Nucleic Acids 2017, 7, 314–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ihn, H.; LeRoy, E.C.; Trojanowska, M. Oncostatin M stimulates transcription of the human alpha2(I) collagen gene via the Sp1/Sp3-binding site. J. Biol. Chem. 1997, 272, 24666–24672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakashima, T.; Jinnin, M.; Yamane, K.; Honda, N.; Kajihara, I.; Makino, T.; Masuguchi, S.; Fukushima, S.; Okamoto, Y.; Hasegawa, M.; et al. Impaired IL-17 signaling pathway contributes to the increased collagen expression in scleroderma fibroblasts. J. Immunol. 2012, 188, 3573–3583. [Google Scholar] [CrossRef] [Green Version]
- Kudo, H.; Jinnin, M.; Asano, Y.; Trojanowska, M.; Nakayama, W.; Inoue, K.; Honda, N.; Kajihara, I.; Makino, K.; Fukushima, S.; et al. Decreased interleukin-20 expression in scleroderma skin contributes to cutaneous fibrosis. Arthritis Rheumatol. 2014, 66, 1636–1647. [Google Scholar] [CrossRef] [Green Version]
- Makino, K.; Jinnin, M.; Hirano, A.; Yamane, K.; Eto, M.; Kusano, T.; Honda, N.; Kajihara, I.; Makino, T.; Sakai, K.; et al. The downregulation of microRNA let-7a contributes to the excessive expression of type I collagen in systemic and localized scleroderma. J. Immunol. 2013, 190, 3905–3915. [Google Scholar] [CrossRef] [Green Version]
- Kitamura, T.; Koshino, Y.; Shibata, F.; Oki, T.; Nakajima, H.; Nosaka, T.; Kumagai, H. Retrovirus-mediated gene transfer and expression cloning: Powerful tools in functional genomics. Exp. Hematol. 2003, 31, 1007–1014. [Google Scholar] [CrossRef]
- Miyoshi, H.; Blomer, U.; Takahashi, M.; Gage, F.H.; Verma, I.M. Development of a self-inactivating lentivirus vector. J. Virol. 1998, 72, 8150–8157. [Google Scholar] [CrossRef] [Green Version]
- Tahara-Hanaoka, S.; Sudo, K.; Ema, H.; Miyoshi, H.; Nakauchi, H. Lentiviral vector-mediated transduction of murine CD34(−) hematopoietic stem cells. Exp. Hematol. 2002, 30, 11–17. [Google Scholar] [CrossRef]
- Egashira, S.; Jinnin, M.; Ajino, M.; Shimozono, N.; Okamoto, S.; Tasaki, Y.; Hirano, A.; Ide, M.; Kajihara, I.; Aoi, J.; et al. Chronic sun exposure-related fusion oncogenes EGFR-PPARGC1A in cutaneous squamous cell carcinoma. Sci. Rep. 2017, 7, 12654. [Google Scholar] [CrossRef] [Green Version]
- Takei, Y.; Kadomatsu, K.; Yuzawa, Y.; Matsuo, S.; Muramatsu, T. A small interfering RNA targeting vascular endothelial growth factor as cancer therapeutics. Cancer Res. 2004, 64, 3365–3370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruzehaji, N.; Avouac, J.; Elhai, M.; Frechet, M.; Frantz, C.; Ruiz, B.; Distler, J.H.; Allanore, Y. Combined effect of genetic background and gender in a mouse model of bleomycin-induced skin fibrosis. Arthritis Res. Ther. 2015, 17, 145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takahashi, T.; Asano, Y.; Ichimura, Y.; Toyama, T.; Taniguchi, T.; Noda, S.; Akamata, K.; Tada, Y.; Sugaya, M.; Kadono, T.; et al. Amelioration of tissue fibrosis by toll-like receptor 4 knockout in murine models of systemic sclerosis. Arthritis Rheumatol. 2015, 67, 254–265. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Shin, M.Y.; Suh, S.H.; Park, S. Lyso-globotriaosylceramide downregulates KCa3.1 channel expression to inhibit collagen synthesis in fibroblasts. Biochem. Biophys. Res. Commun. 2015, 468, 883–888. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sawamura, S.; Makino, K.; Ide, M.; Shimada, S.; Kajihara, I.; Makino, T.; Jinnin, M.; Fukushima, S. Elevated Alpha 1(I) to Alpha 2(I) Collagen Ratio in Dermal Fibroblasts Possibly Contributes to Fibrosis in Systemic Sclerosis. Int. J. Mol. Sci. 2022, 23, 6811. https://doi.org/10.3390/ijms23126811
Sawamura S, Makino K, Ide M, Shimada S, Kajihara I, Makino T, Jinnin M, Fukushima S. Elevated Alpha 1(I) to Alpha 2(I) Collagen Ratio in Dermal Fibroblasts Possibly Contributes to Fibrosis in Systemic Sclerosis. International Journal of Molecular Sciences. 2022; 23(12):6811. https://doi.org/10.3390/ijms23126811
Chicago/Turabian StyleSawamura, Soichiro, Katsunari Makino, Maho Ide, Shuichi Shimada, Ikko Kajihara, Takamitsu Makino, Masatoshi Jinnin, and Satoshi Fukushima. 2022. "Elevated Alpha 1(I) to Alpha 2(I) Collagen Ratio in Dermal Fibroblasts Possibly Contributes to Fibrosis in Systemic Sclerosis" International Journal of Molecular Sciences 23, no. 12: 6811. https://doi.org/10.3390/ijms23126811





