Predicting Antigenic Peptides from Rocio Virus NS1 Protein for Immunodiagnostic Testing Using Immunoinformatics and Molecular Dynamics Simulation
Abstract
:1. Introduction
2. Results
2.1. ROCV NS1 Has High Amino Acid Identity with Other Flaviviruses
2.2. Predicted Protein Characteristics and Structural Features of ROCV NS1
2.3. Peptide Candidate as a Potential Antigen Suitable for Immunodiagnostic Tests
2.4. Physicochemical Properties of the p_ROCV2 Peptide
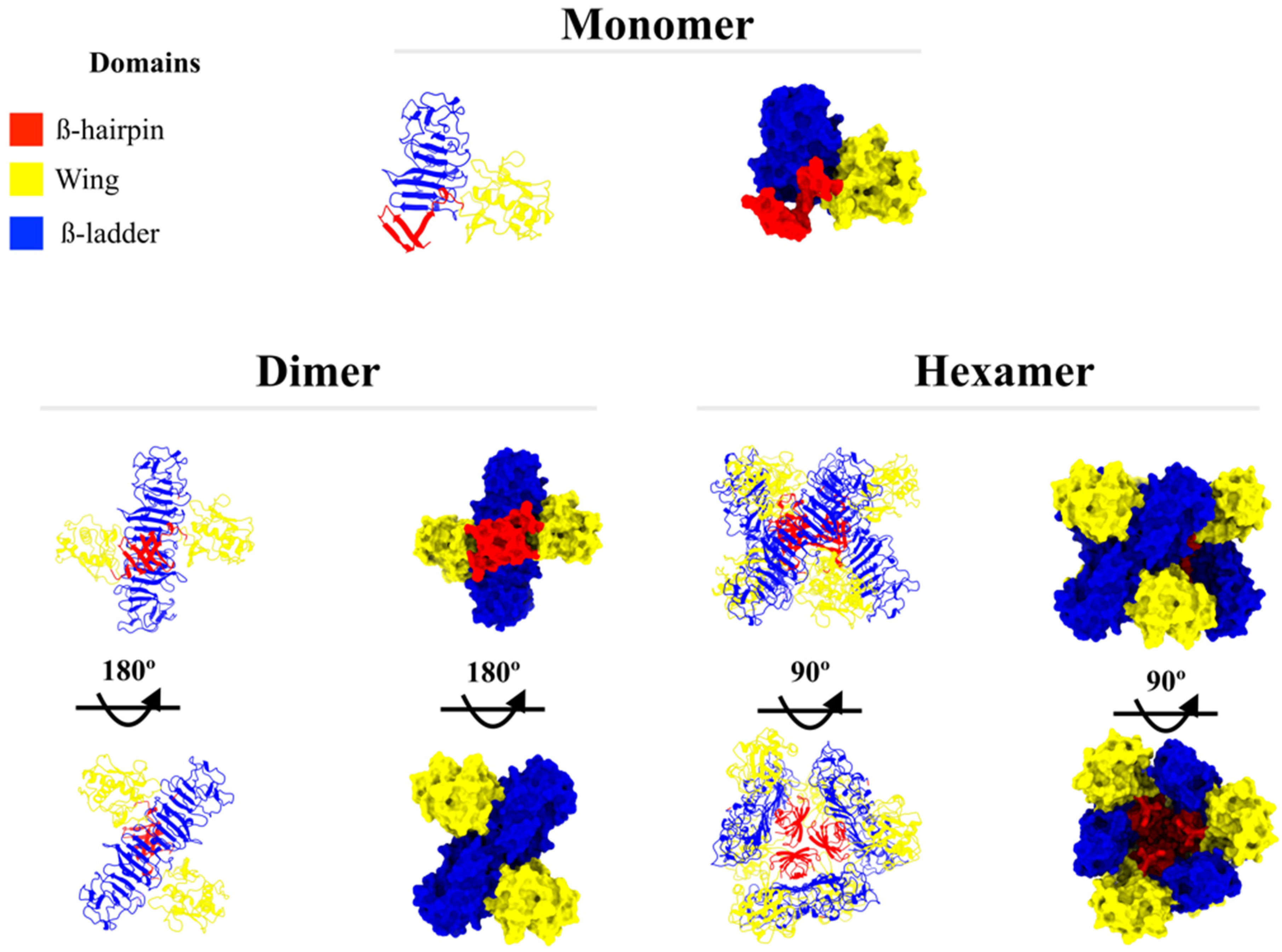
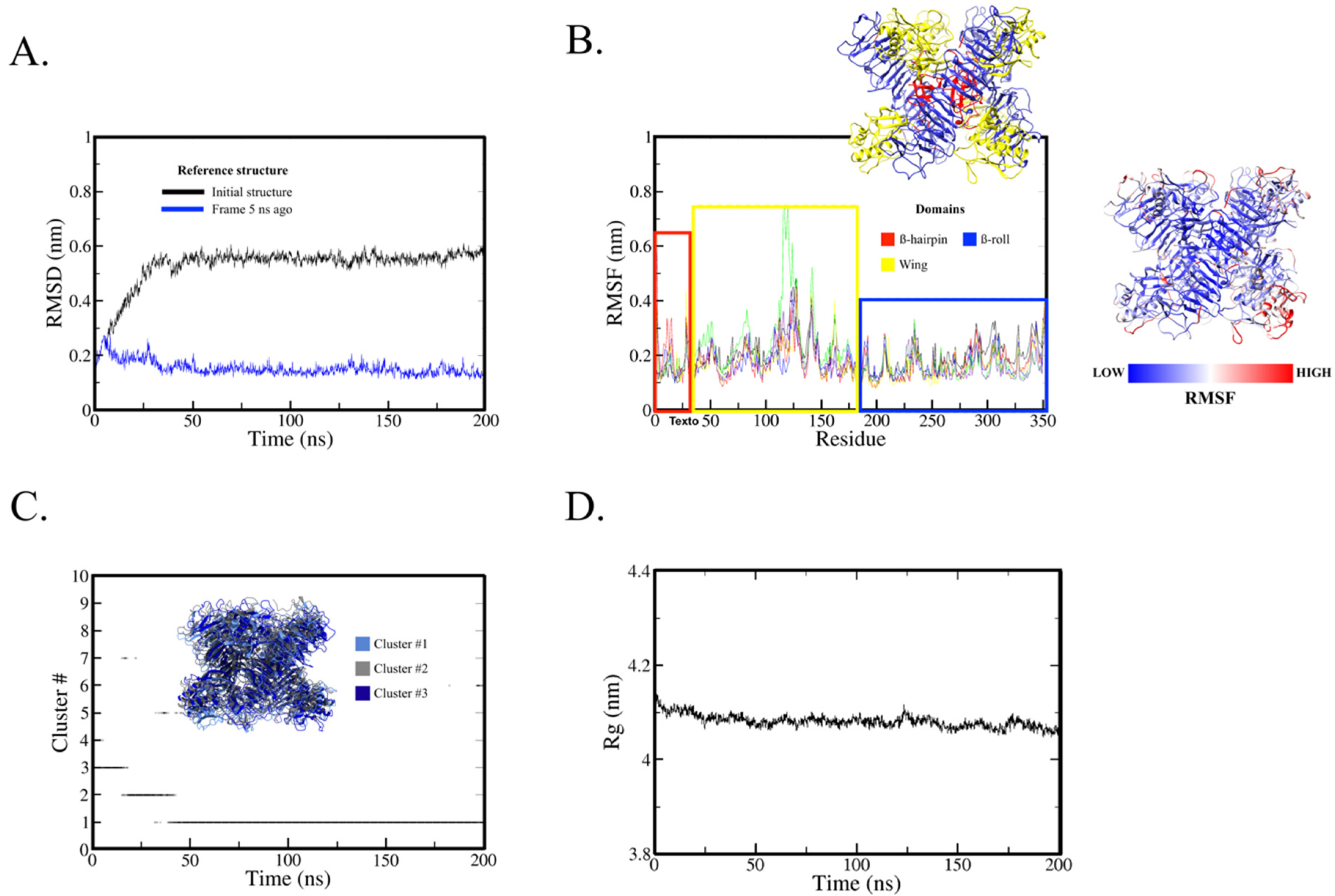
2.5. Tri-Dimensional ROCV NS1 Hexamer Protein and Immunogenic Peptide Analyses
3. Discussion
4. Materials and Methods
4.1. Sequence Retrieval
4.2. Predicting Physicochemical Properties of Protein
4.3. Predicting Antigenicity and Linear B-Cell Epitopes
4.4. Predicting Physicochemical Properties of the Epitopes
4.5. NS1 Hexamer Modeling
4.6. Molecular Dynamics Simulation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tiriba, A.C.; Miziara, A.M.; Lorenço, R.; Costa, C.R.B.; Costa, C.S.; Pinto, G.H. Encefalite Humana Primária Epidêmica Por Arbovírus Observada No Litoral Sul Do Estado de São Paulo. Rev. Assoc. Med. Brasil 1976, 22, 415–420. [Google Scholar]
- Saivish, M.V.; Gomes da Costa, V.; de Lima Menezes, G.; Alves da Silva, R.; Dutra da Silva, G.C.; Moreli, M.L.; Sacchetto, L.; Pacca, C.C.; Vasilakis, N.; Nogueira, M.L. Rocio Virus: An Updated View on an Elusive Flavivirus. Viruses 2021, 13, 2293. [Google Scholar] [CrossRef]
- Saivish, M.V.; da Costa, V.G.; Rodrigues, R.L.; Féres, V.C.R.; Montoya-Diaz, E.; Moreli, M.L. Detection of Rocio Virus SPH 34675 during Dengue Epidemics, Brazil, 2011–2013. Emerg. Infect. Dis. 2020, 26, 797–799. [Google Scholar] [CrossRef]
- Lopes, O.D.S.; Coimbra, T.L.M.; Sacchetta, L.D.A.; Calisher, C.H. Emergence of a new arbovirus disease in Brazil: I. isolation and characterization of the etiologic agent, Rocio virus. Am. J. Epidemiol. 1978, 107, 444–449. [Google Scholar] [CrossRef]
- Iversson, L.B. Aspectos da epidemia de encefalite por arbovirus na região do Vale do Ribeira, S. Paulo, Brasil, no período de 1975 a 1978. Rev. Saúde Pública 1980, 14, 9–35. [Google Scholar] [CrossRef]
- Pauvolid-Corrêa, A.; Campos, Z.; Juliano, R.; Velez, J.; Nogueira, R.M.R.; Komar, N. Serological Evidence of Widespread Circulation of West Nile Virus and Other Flaviviruses in Equines of the Pantanal, Brazil. PLoS Negl. Trop. Dis. 2014, 8, e2706. [Google Scholar] [CrossRef] [Green Version]
- Silva, J.R.; Romeiro, M.F.; de Souza, W.M.; Munhoz, T.D.; Borges, G.P.; Soares, O.A.B.; de Campos, C.H.C.; Machado, R.Z.; Silva, M.L.C.R.; Faria, J.L.M.; et al. A Saint Louis Encephalitis and Rocio Virus Serosurvey in Brazilian Horses. Rev. Soc. Bras. Med. Trop. 2014, 47, 414–417. [Google Scholar] [CrossRef] [Green Version]
- Straatmann, A.; Santos-Torres, S.; Vasconcelos, P.F.C.; Travassos da Rosa, A.P.A.; Rodrigues, S.G.; Tavares-Neto, J. Evidências sorológicas da circulação do arbovírus Rocio (Flaviviridae) na Bahia. Rev. Soc. Bras. Med. Trop. 1997, 30, 511–515. [Google Scholar] [CrossRef] [Green Version]
- Tanaka, H.; Weigl, D.R.; de Souza Lopes, O. The Replication of Rocio Virus in Brain Tissue of Suckling Mice. Study by Electron Microscopy. Arch. Virol. 1983, 78, 309–314. [Google Scholar] [CrossRef]
- Setoh, Y.X.; Amarilla, A.A.; Peng, N.Y.; Slonchak, A.; Periasamy, P.; Figueiredo, L.T.M.; Aquino, V.H.; Khromykh, A.A. Full Genome Sequence of Rocio Virus Reveal Substantial Variations from the Prototype Rocio Virus SPH 34675 Sequence. Arch. Virol. 2018, 163, 255–258. [Google Scholar] [CrossRef]
- Tsai, C.-L.; Sun, D.-S.; Su, M.-T.; Lien, T.-S.; Chen, Y.-H.; Lin, C.-Y.; Huang, C.-H.; King, C.-C.; Li, C.-R.; Chen, T.-H.; et al. Suppressed Humoral Immunity Is Associated with Dengue Nonstructural Protein NS1-Elicited Anti-Death Receptor Antibody Fractions in Mice. Sci. Rep. 2020, 10, 6294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shukla, A.; Rastogi, M.; Singh, S.K. Zika Virus NS1 Suppresses the Innate Immune Responses via MiR-146a in Human Microglial Cells. Int. J. Biol. Macromol. 2021, 193, 2290–2296. [Google Scholar] [CrossRef] [PubMed]
- Avirutnan, P.; Hauhart, R.E.; Somnuke, P.; Blom, A.M.; Diamond, M.S.; Atkinson, J.P. Binding of Flavivirus Nonstructural Protein NS1 to C4b Binding Protein Modulates Complement Activation. J. Immunol. 2011, 187, 424–433. [Google Scholar] [CrossRef]
- Ci, Y.; Liu, Z.-Y.; Zhang, N.-N.; Niu, Y.; Yang, Y.; Xu, C.; Yang, W.; Qin, C.-F.; Shi, L. Zika NS1–Induced ER Remodeling Is Essential for Viral Replication. J. Cell Biol. 2020, 219, e201903062. [Google Scholar] [CrossRef] [PubMed]
- Scaturro, P.; Cortese, M.; Chatel-Chaix, L.; Fischl, W.; Bartenschlager, R. Dengue Virus Non-Structural Protein 1 Modulates Infectious Particle Production via Interaction with the Structural Proteins. PLoS Pathog. 2015, 11, e1005277. [Google Scholar] [CrossRef]
- Roldán, J.S.; Cassola, A.; Castillo, D.S. Development of a Novel NS1 Competitive Enzyme-Linked Immunosorbent Assay for the Early Detection of Zika Virus Infection. PLoS ONE 2021, 16, e0256220. [Google Scholar] [CrossRef]
- Lorch, M.S.; Collado, M.S.; Argüelles, M.H.; Rota, R.P.; Spinsanti, L.I.; Lozano, M.E.; Goñi, S.E. Production of Recombinant NS1 Protein and Its Possible Use in Encephalitic Flavivirus Differential Diagnosis. Protein Expr. Purif. 2019, 153, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-J.; Cho, Y.; Kang, H.J.; Choi, H.; Han, K.R.; Chong, C.K.; Kim, Y.B. Identification of Peptide Based B-Cell Epitopes in Zika Virus NS1. Biochem. Biophys. Res. Commun. 2018, 505, 1010–1014. [Google Scholar] [CrossRef]
- Kumarasamy, V.; Wahab, A.H.A.; Chua, S.K.; Hassan, Z.; Chem, Y.K.; Mohamad, M.; Chua, K.B. Evaluation of a Commercial Dengue NS1 Antigen-Capture ELISA for Laboratory Diagnosis of Acute Dengue Virus Infection. J. Virol. Methods 2007, 140, 75–79. [Google Scholar] [CrossRef]
- Zainah, S.; Wahab, A.H.A.; Mariam, M.; Fauziah, M.K.; Khairul, A.H.; Roslina, I.; Sairulakhma, A.; Kadimon, S.S.; Jais, M.S.M.; Chua, K.B. Performance of a Commercial Rapid Dengue NS1 Antigen Immunochromatography Test with Reference to Dengue NS1 Antigen-Capture ELISA. J. Virol. Methods 2009, 155, 157–160. [Google Scholar] [CrossRef]
- Castro-Jorge, L.A.; Machado, P.R.L.; Fávero, C.A.; Borges, M.C.; Passos, L.M.R.; de Oliveira, R.M.; Fonseca, B.A.L. Clinical Evaluation of the NS1 Antigen-Capture ELISA for Early Diagnosis of Dengue Virus Infection in Brazil. J. Med. Virol. 2010, 82, 1400–1405. [Google Scholar] [CrossRef] [PubMed]
- Murphy, N.; Macchiaverna, N.P.; Victoria Cardinal, M.; Bhattacharyya, T.; Mertens, P.; Zeippen, N.; Gustin, Y.; Gilleman, Q.; Gürtler, R.E.; Miles, M.A. Lineage-Specific Rapid Diagnostic Tests Can Resolve Trypanosoma Cruzi TcII/V/VI Ecological and Epidemiological Associations in the Argentine Chaco. Parasit. Vectors 2019, 12, 424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, M.; Malik, S.S.; Vergis, J.; Ramanjeneya, S.; Sahu, R.; Pathak, R.; Yadav, J.P.; Dhaka, P.; Barbuddhe, S.B.; Rawool, D.B. Development of the Com1 Synthetic Peptide-Based Latex Agglutination Test (LAT) and Its Comparative Evaluation with Commercial Indirect-ELISA for Sero-Screening of Coxiellosis in Cattle. J. Microbiol. Methods 2019, 162, 83–85. [Google Scholar] [CrossRef] [PubMed]
- Guevarra, L.A., Jr.; Boado, K.J.O.; Ceñidoza, F.B.B.; Imbao, M.R.L.M.; Sia, M.J.G.; Dalmacio, L.M.M. A Synthetic Peptide Analog of in Silico-Predicted Immunogenic Epitope Unique to Dengue Virus Serotype 2 NS1 Antigen Specifically Binds Immunoglobulin G Antibodies Raised in Rabbits. Microbiol. Immunol. 2020, 64, 153–161. [Google Scholar] [CrossRef]
- Köhler, H.; Liebler-Tenorio, E.; Hughes, V.; Stevenson, K.; Bakker, D.; Willemsen, P.; Bay, S.; Ganneau, C.; Biet, F.; Vordermeier, H.M. Interferon-γ Response of Mycobacterium Avium Subsp. Paratuberculosis Infected Goats to Recombinant and Synthetic Mycobacterial Antigens. Front. Vet. Sci. 2021, 8, 645251. [Google Scholar] [CrossRef]
- Middleton, S.; Steinbach, S.; Coad, M.; McGill, K.; Brady, C.; Duignan, A.; Wiseman, J.; Gormley, E.; Jones, G.J.; Vordermeier, H.M. A Molecularly Defined Skin Test Reagent for the Diagnosis of Bovine Tuberculosis Compatible with Vaccination against Johne’s Disease. Sci. Rep. 2021, 11, 2929. [Google Scholar] [CrossRef]
- Polvere, I.; Parrella, A.; Casamassa, G.; D’Andrea, S.; Tizzano, A.; Cardinale, G.; Voccola, S.; Porcaro, P.; Stilo, R.; Vito, P.; et al. Seroprevalence of Anti-SARS-CoV-2 IgG and IgM among Adults over 65 Years Old in the South of Italy. Diagnostics 2021, 11, 483. [Google Scholar] [CrossRef]
- Arumugam, S.; Nayak, S.; Williams, T.; di Santa Maria, F.S.; Guedes, M.S.; Chaves, R.C.; Linder, V.; Marques, A.R.; Horn, E.J.; Wong, S.J.; et al. A Multiplexed Serologic Test for Diagnosis of Lyme Disease for Point-of-Care Use. J. Clin. Microbiol. 2019, 57, e01142-19. [Google Scholar] [CrossRef]
- Prado, I.C.; Mendes, V.G.; Souza, A.L.A.; Dutra, R.F.; De-Simone, S.G. Electrochemical Immunosensor for Differential Diagnostic of Wuchereria Bancrofti Using a Synthetic Peptide. Biosens. Bioelectron. 2018, 113, 9–15. [Google Scholar] [CrossRef]
- Gomara, M.J.; Haro, I. Synthetic Peptides for the Immunodiagnosis of Human Diseases. Curr. Med. Chem. 2007, 14, 531–546. [Google Scholar] [CrossRef]
- Genus: Flavivirus-Flaviviridae-Positive-Sense RNA Viruses-ICTV. Available online: https://talk.ictvonline.org/ictv-reports/ictv_online_report/positive-sense-rna-viruses/w/flaviviridae/360/genus-flavivirus (accessed on 16 May 2022).
- Kolaskar, A.S.; Tongaonkar, P.C. A Semi-Empirical Method for Prediction of Antigenic Determinants on Protein Antigens. FEBS Lett. 1990, 276, 172–174. [Google Scholar] [CrossRef] [Green Version]
- Jameson, B.A.; Wolf, H. The Antigenic Index: A Novel Algorithm for Predicting Antigenic Determinants. Bioinformatics 1988, 4, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Prediction of Sequential Antigenic Regions in Proteins-Welling-1985-FEBS Letters-Wiley Online Library. Available online: https://febs.onlinelibrary.wiley.com/doi/abs/10.1016/0014-5793%2885%2980374-4?sid=nlm%3Apubmed (accessed on 25 May 2022).
- Wessel, A.W.; Doyle, M.P.; Engdahl, T.B.; Rodriguez, J.; Crowe, J.E.; Diamond, M.S. Human Monoclonal Antibodies against NS1 Protein Protect against Lethal West Nile Virus Infection. mBio 2021, 12, e02440-21. [Google Scholar] [CrossRef] [PubMed]
- Modhiran, N.; Song, H.; Liu, L.; Bletchly, C.; Brillault, L.; Amarilla, A.A.; Xu, X.; Qi, J.; Chai, Y.; Cheung, S.T.M.; et al. A Broadly Protective Antibody That Targets the Flavivirus NS1 Protein. Science 2021, 371, 190–194. [Google Scholar] [CrossRef]
- Lai, Y.-C.; Chuang, Y.-C.; Liu, C.-C.; Ho, T.-S.; Lin, Y.-S.; Anderson, R.; Yeh, T.-M. Antibodies Against Modified NS1 Wing Domain Peptide Protect Against Dengue Virus Infection. Sci. Rep. 2017, 7, 6975. [Google Scholar] [CrossRef]
- Lopes, O.D.S.; Sacchetta, L.D.A.; Coimbra, T.L.M.; Pinto, G.H.; Glasser, C.M. Emergence of a new arbovirus disease in brazil: II. epidemiologic studies on 1975 epidemic. Am. J. Epidemiol. 1978, 108, 394–401. [Google Scholar] [CrossRef]
- Casseb, A.R.; Cruz, A.V.; Jesus, I.S.; Chiang, J.O.; Martins, L.C.; Silva, S.P.; Henriques, D.F.; Casseb, L.M.; Vasconcelos, P.F.C. Seroprevalence of Flaviviruses Antibodies in Water Buffaloes (Bubalus Bubalis) in Brazilian Amazon. J. Venom. Anim. Toxins Trop. Dis. 2014, 20, 9. [Google Scholar] [CrossRef] [Green Version]
- Carpio, K.L.; Barrett, A.D.T. Flavivirus NS1 and Its Potential in Vaccine Development. Vaccines 2021, 9, 622. [Google Scholar] [CrossRef]
- Rastogi, M.; Sharma, N.; Singh, S.K. Flavivirus NS1: A Multifaceted Enigmatic Viral Protein. Virol. J. 2016, 13, 131. [Google Scholar] [CrossRef] [Green Version]
- Kam, Y.-W.; Leite, J.A.; Amrun, S.N.; Lum, F.-M.; Yee, W.-X.; Bakar, F.A.; Eng, K.E.; Lye, D.C.; Leo, Y.-S.; Chong, C.-Y.; et al. ZIKV-Specific NS1 Epitopes as Serological Markers of Acute Zika Virus Infection. J. Infect. Dis. 2019, 220, 203–212. [Google Scholar] [CrossRef]
- Mora-Cárdenas, E.; Aloise, C.; Faoro, V.; Gašper, N.K.; Korva, M.; Caracciolo, I.; D’Agaro, P.; Avšič-Županc, T.; Marcello, A. Comparative Specificity and Sensitivity of NS1-Based Serological Assays for the Detection of Flavivirus Immune Response. PLoS Negl. Trop. Dis. 2020, 14, e0008039. [Google Scholar] [CrossRef] [PubMed]
- Salarpour, A.; Toroghi, R.; Nikbakht Brujeni, G.; Momayez, R. In Silico Prediction of Linear B-Cell Epitopes for S1 Protein of Two Iranian 793/B Isolates and Their Changes after 90 Serial Passaging. Vet. Res. Forum 2020, 11, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Moeini, H.; Afridi, S.Q.; Donakonda, S.; Knolle, P.A.; Protzer, U.; Hoffmann, D. Linear B-Cell Epitopes in Human Norovirus GII.4 Capsid Protein Elicit Blockade Antibodies. Vaccines 2021, 9, 52. [Google Scholar] [CrossRef] [PubMed]
- Siañez-Estrada, L.I.; Rivera-Benítez, J.F.; Rosas-Murrieta, N.H.; Reyes-Leyva, J.; Santos-López, G.; Herrera-Camacho, I. Immunoinformatics Approach for Predicting Epitopes in HN and F Proteins of Porcine Rubulavirus. PLoS ONE 2020, 15, e0239785. [Google Scholar] [CrossRef]
- de Paiva Conte, F.; Tinoco, B.C.; Chaves, T.S.; de Oliveira, R.C.; Mansur, J.F.; Mohana-Borges, R.; de Lemos, E.R.S.; da Costa Neves, P.C.; Rodrigues-da-Silva, R.N. Identification and Validation of Specific B-Cell Epitopes of Hantaviruses Associated to Hemorrhagic Fever and Renal Syndrome. PLoS Negl. Trop. Dis. 2019, 13, e0007915. [Google Scholar] [CrossRef] [Green Version]
- Almeida, M.A.; Almeida-Paes, R.; Guimarães, A.J.; Valente, R.H.; de Almeida Soares, C.M.; Zancopé-Oliveira, R.M. Immunoproteomics Reveals Pathogen’s Antigens Involved in Homo Sapiens–Histoplasma Capsulatum Interaction and Specific Linear B-Cell Epitopes in Histoplasmosis. Front. Cell. Infect. Microbiol. 2020, 10, 591121. [Google Scholar] [CrossRef]
- Frontiers | Antibody Responses Against Plasmodium Vivax TRAP Recombinant and Synthetic Antigens in Naturally Exposed Individuals From the Brazilian Amazon | Immunology. Available online: https://www.frontiersin.org/articles/10.3389/fimmu.2019.02230/full (accessed on 28 May 2022).
- Campos, M.P.; Figueiredo, F.B.; Morgado, F.N.; dos Santos Renzetti, A.R.; de Souza, S.M.M.; Pereira, S.A.; Rodrigues-Da-Silva, R.N.; Lima-Junior, J.D.C.; De Luca, P.M. Leishmania Infantum Virulence Factor A2 Protein: Linear B-Cell Epitope Mapping and Identification of Three Main Linear B-Cell Epitopes in Vaccinated and Naturally Infected Dogs. Front. Immunol. 2018, 9, 1690. [Google Scholar] [CrossRef]
- Fontes, S.d.S.; Maia, F.d.M.; Ataides, L.S.; Conte, F.P.; Lima-Junior, J.d.C.; Rozental, T.; da Silva Assis, M.R.; Júnior, A.A.P.; Fernandes, J.; de Lemos, E.R.S.; et al. Identification of Immunogenic Linear B-Cell Epitopes in C. Burnetii Outer Membrane Proteins Using Immunoinformatics Approaches Reveals Potential Targets of Persistent Infections. Pathogens 2021, 10, 1250. [Google Scholar] [CrossRef]
- Zargaran, F.N.; Akya, A.; Rezaeian, S.; Ghadiri, K.; Lorestani, R.C.; Madanchi, H.; Safaei, S.; Rostamian, M. B Cell Epitopes of Four Fimbriae Antigens of Klebsiella Pneumoniae: A Comprehensive In Silico Study for Vaccine Development. Int. J. Pept. Res. Ther. 2021, 27, 875–886. [Google Scholar] [CrossRef]
- Feodorova, V.A.; Lyapina, A.M.; Khizhnyakova, M.A.; Zaitsev, S.S.; Saltykov, Y.V.; Motin, V.L. Yersinia Pestis Antigen F1 but Not LcrV Induced Humoral and Cellular Immune Responses in Humans Immunized with Live Plague Vaccine—Comparison of Immunoinformatic and Immunological Approaches. Vaccines 2020, 8, 698. [Google Scholar] [CrossRef]
- Kalkanlı Taş, S.; Kırkık, D.; Öztürk, K.; Tanoğlu, A. Determination of B- and T- Cell Epitopes for Helicobacter Pylori CagPAI: An in Silico Approach. Turk. J. Gastroenterol. 2020, 31, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Han, K.; Huang, X.; Zhang, L.; Wang, H.; Liu, N.; Tian, Y.; Liu, Q.; Yang, J.; Liu, Y.; et al. Screening and Identification of B-Cell Epitopes within Envelope Protein of Tembusu Virus. Virol. J. 2018, 15, 142. [Google Scholar] [CrossRef] [PubMed]
- Palanisamy, N.; Lennerstrand, J. Computational Prediction of Usutu Virus E Protein B Cell and T Cell Epitopes for Potential Vaccine Development. Scand. J. Immunol. 2017, 85, 350–364. [Google Scholar] [CrossRef] [Green Version]
- Nadugala, M.N.; Premaratne, P.H.; Goonasekara, C.L. Systematic Bioinformatic Approach for Prediction of Linear B-Cell Epitopes on Dengue E and PrM Protein. Adv. Bioinforma. 2016, 2016, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabrejee, S.; Hossain, M.M. In Silico Approach To Design a B-Cell Epitope Based Vaccine Target Against Yellow Fever Virus. Bangladesh J. Microbiol. 2018, 35, 27–35. [Google Scholar] [CrossRef]
- Slathia, P.S.; Sharma, P. A Common Conserved Peptide Harboring Predicted T and B Cell Epitopes in Domain III of Envelope Protein of Japanese Encephalitis Virus and West Nile Virus for Potential Use in Epitope Based Vaccines. Comp. Immunol. Microbiol. Infect. Dis. 2019, 65, 238–245. [Google Scholar] [CrossRef]
- Amrun, S.N.; Yee, W.-X.; Abu Bakar, F.; Lee, B.; Kam, Y.-W.; Lum, F.-M.; Tan, J.J.; Lim, V.W.; Watthanaworawit, W.; Ling, C.; et al. Novel Differential Linear B-Cell Epitopes to Identify Zika and Dengue Virus Infections in Patients. Clin. Transl. Immunol. 2019, 8, e1066. [Google Scholar] [CrossRef] [Green Version]
- Freire, M.C.L.C.; Pol-Fachin, L.; Coêlho, D.F.; Viana, I.F.T.; Magalhães, T.; Cordeiro, M.T.; Fischer, N.; Loeffler, F.F.; Jaenisch, T.; Franca, R.F.; et al. Mapping Putative B-Cell Zika Virus NS1 Epitopes Provides Molecular Basis for Anti-NS1 Antibody Discrimination between Zika and Dengue Viruses. ACS Omega 2017, 2, 3913–3920. [Google Scholar] [CrossRef] [Green Version]
- Manikandan, M.; Prabu, S.; Rajeswari, K.; Kamaraj, R.; Krishnan, S. In Silico Prediction of B-Cell Epitopes of Dengue Virus–A Reverse Vaccinology Approach. J. Appl. Pharm. Sci. 2020, 10, 77–85. [Google Scholar] [CrossRef]
- Biering, S.B.; Akey, D.L.; Wong, M.P.; Brown, W.C.; Lo, N.T.N.; Puerta-Guardo, H.; Tramontini Gomes de Sousa, F.; Wang, C.; Konwerski, J.R.; Espinosa, D.A.; et al. Structural Basis for Antibody Inhibition of Flavivirus NS1–Triggered Endothelial Dysfunction. Science 2021, 371, 194–200. [Google Scholar] [CrossRef]
- Chung, K.M.; Nybakken, G.E.; Thompson, B.S.; Engle, M.J.; Marri, A.; Fremont, D.H.; Diamond, M.S. Antibodies against West Nile Virus Nonstructural Protein NS1 Prevent Lethal Infection through Fc γ Receptor-Dependent and -Independent Mechanisms. J. Virol. 2006, 80, 1340–1351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wessel, A.W.; Kose, N.; Bombardi, R.G.; Roy, V.; Chantima, W.; Mongkolsapaya, J.; Edeling, M.A.; Nelson, C.A.; Bosch, I.; Alter, G.; et al. Antibodies Targeting Epitopes on the Cell-Surface Form of NS1 Protect against Zika Virus Infection during Pregnancy. Nat. Commun. 2020, 11, 5278. [Google Scholar] [CrossRef] [PubMed]
- Akey, D.L.; Brown, W.C.; Dutta, S.; Konwerski, J.; Jose, J.; Jurkiw, T.J.; DelProposto, J.; Ogata, C.M.; Skiniotis, G.; Kuhn, R.J.; et al. Flavivirus NS1 Structures Reveal Surfaces for Associations with Membranes and the Immune System. Science 2014, 343, 881–885. [Google Scholar] [CrossRef] [Green Version]
- Akey, D.L.; Brown, W.C.; Jose, J.; Kuhn, R.J.; Smith, J.L. Structure-Guided Insights on the Role of NS1 in Flavivirus Infection. BioEssays 2015, 37, 489–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nair, D.T.; Singh, K.; Siddiqui, Z.; Nayak, B.P.; Rao, K.V.S.; Salunke, D.M. Epitope Recognition by Diverse Antibodies Suggests Conformational Convergence in an Antibody Response. J. Immunol. 2002, 168, 2371–2382. [Google Scholar] [CrossRef] [Green Version]
- Influence of Protein Flexibility and Peptide Conformation on Reactivity of Monoclonal Anti-Peptide Antibodies with a Protein Alpha-Helix. | PNAS. Available online: https://www.pnas.org/doi/abs/10.1073/pnas.84.23.8568 (accessed on 25 May 2022).
- Prediction of Protein Antigenic Determinants from Amino Acid Sequences. | PNAS. Available online: https://www.pnas.org/doi/10.1073/pnas.78.6.3824?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed (accessed on 25 May 2022).
- Kyte, J.; Doolittle, R.F. A Simple Method for Displaying the Hydropathic Character of a Protein. J. Mol. Biol. 1982, 157, 105–132. [Google Scholar] [CrossRef] [Green Version]
- Parker, J.M.R.; Guo, D.; Hodges, R.S. New Hydrophilicity Scale Derived from High-Performance Liquid Chromatography Peptide Retention Data: Correlation of Predicted Surface Residues with Antigenicity and x-Ray-Derived Accessible Sites. Biochemistry 1986, 25, 5425–5432. [Google Scholar] [CrossRef]
- Emini, E.A.; Hughes, J.V.; Perlow, D.S.; Boger, J. Induction of Hepatitis A Virus-Neutralizing Antibody by a Virus-Specific Synthetic Peptide. J. Virol. 1985, 55, 836–839. [Google Scholar] [CrossRef] [Green Version]
- Karplus, P.A.; Schulz, G.E. Prediction of Chain Flexibility in Proteins. Naturwissenschaften 1985, 72, 212–213. [Google Scholar] [CrossRef]
- B-Cell Epitopes (DNASTAR)-User Guide to Protean 3D-17.2. Available online: https://www.dnastar.com/manuals/protean3d/17.2/en/topic/b-cell-epitopes-neoclone (accessed on 25 May 2022).
- Ponomarenko, J.; Bui, H.-H.; Li, W.; Fusseder, N.; Bourne, P.E.; Sette, A.; Peters, B. ElliPro: A New Structure-Based Tool for the Prediction of Antibody Epitopes. BMC Bioinformatics 2008, 9, 514. [Google Scholar] [CrossRef] [Green Version]
- Doytchinova, I.A.; Flower, D.R. VaxiJen: A Server for Prediction of Protective Antigens, Tumour Antigens and Subunit Vaccines. BMC Bioinformatics 2007, 8, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frontiers | Antigenic Peptide Prediction From E6 and E7 Oncoproteins of HPV Types 16 and 18 for Therapeutic Vaccine Design Using Immunoinformatics and MD Simulation Analysis | Immunology. Available online: https://www.frontiersin.org/articles/10.3389/fimmu.2018.03000/full (accessed on 25 May 2022).
- Gasteiger, E.; Hoogland, C.; Gattiker, A.; Duvaud, S.; Wilkins, M.R.; Appel, R.D.; Bairoch, A. Protein Identification and Analysis Tools on the ExPASy Server. In The Proteomics Protocols Handbook; Walker, J.M., Ed.; Humana Press: Totowa, NJ, USA, 2005; pp. 571–607. ISBN 978-1-58829-343-5. [Google Scholar]
- Yang, J.; Zhang, Y. I-TASSER Server: New Development for Protein Structure and Function Predictions. Nucleic Acids Res. 2015, 43, 174–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tovchigrechko, A.; Vakser, I.A. GRAMM-X Public Web Server for Protein–Protein Docking. Nucleic Acids Res. 2006, 34, W310–W314. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Qi, J.; Haywood, J.; Shi, Y.; Gao, G.F. Zika Virus NS1 Structure Reveals Diversity of Electrostatic Surfaces among Flaviviruses. Nat. Struct. Mol. Biol. 2016, 23, 456–458. [Google Scholar] [CrossRef]
- Olsson, M.H.M.; Søndergaard, C.R.; Rostkowski, M.; Jensen, J.H. PROPKA3: Consistent Treatment of Internal and Surface Residues in Empirical p K a Predictions. J. Chem. Theory Comput. 2011, 7, 525–537. [Google Scholar] [CrossRef]
- Abraham, M.J.; Murtola, T.; Schulz, R.; Páll, S.; Smith, J.C.; Hess, B.; Lindahl, E. GROMACS: High Performance Molecular Simulations through Multi-Level Parallelism from Laptops to Supercomputers. SoftwareX 2015, 1–2, 19–25. [Google Scholar] [CrossRef] [Green Version]
- Hess, B.; Bekker, H.; Berendsen, H.J.C.; Fraaije, J.G.E.M. LINCS: A Linear Constraint Solver for Molecular Simulations. J. Comput. Chem. 1997, 18, 1463–1472. [Google Scholar] [CrossRef]
- Miyamoto, S.; Kollman, P.A. Settle: An Analytical Version of the SHAKE and RATTLE Algorithm for Rigid Water Models. J. Comput. Chem. 1992, 13, 952–962. [Google Scholar] [CrossRef]
- Berendsen, H.J.C.; Postma, J.P.M.; van Gunsteren, W.F.; DiNola, A.; Haak, J.R. Molecular Dynamics with Coupling to an External Bath. J. Chem. Phys. 1984, 81, 3684–3690. [Google Scholar] [CrossRef] [Green Version]
- Hutter, J. Car-Parrinello Molecular Dynamics: Car-Parrinello Molecular Dynamics. Wiley Interdiscip. Rev. Comput. Mol. Sci. 2012, 2, 604–612. [Google Scholar] [CrossRef]
- Hockney, R.W.; Goel, S.P.; Eastwood, J.W. Quiet High-Resolution Computer Models of a Plasma. J. Comput. Phys. 1974, 14, 148–158. [Google Scholar] [CrossRef]
- Daura, X.; Gademann, K.; Jaun, B.; Seebach, D.; van Gunsteren, W.F.; Mark, A.E. Peptide Folding: When Simulation Meets Experiment. Angew. Chem. Int. Ed. 1999, 38, 236–240. [Google Scholar] [CrossRef]
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C.; Couch, G.S.; Greenblatt, D.M.; Meng, E.C.; Ferrin, T.E. UCSF Chimera-a Visualization System for Exploratory Research and Analysis. J. Comput. Chem. 2004, 25, 1605–1612. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C.; Meng, E.C.; Couch, G.S.; Croll, T.I.; Morris, J.H.; Ferrin, T.E. UCSF CHIMERAX: Structure Visualization for Researchers, Educators, and Developers. Protein Sci. 2021, 30, 70–82. [Google Scholar] [CrossRef]
- Rodrigues, R.L.; Menezes, G.D.L.; Saivish, M.V.; Costa, V.G.D.; Pereira, M.; Moreli, M.L.; Silva, R.A.D. Prediction of MAYV Peptide Antigens for Immunodiagnostic Tests by Immunoinformatics and Molecular Dynamics Simulations. Sci. Rep. 2019, 9, 13339. [Google Scholar] [CrossRef]


| Prediction Items | Prediction Results (Location of Deduced Peptides) |
|---|---|
| Antigenicity: Jameson–Wolf, DNASTAR Protean 3D | 1–4, 11–17, 24–25, 28–42, 49–54, 59–62, 106–109, 118–119, 136–146, 171–177, 189–191, 203–209, 220–224, 235–241, 249–273, 279–289, 291–295, 302–309, 313, 316–318, 320, 324–328, 335–345 |
| Antigenicity: Welling, DNASTAR Protean 3D | 26, 30–40, 44–48, 51, 61–62, 66, 72–73, 89, 91, 94–104, 145, 168, 170–174, 191–197, 210, 213, 250–261, 264, 295–301, 303, 341–342, 349–353 |
| B-cell epitopes: high antigenic regions, DNASTAR Protean 3D | 2–5, 10, 12–14, 16, 21–23, 26, 34–36, 40–41, 48–51, 53, 71–76, 78, 80–83, 88–91, 99, 101–102, 111, 113–118, 124–127, 134–137, 140, 147, 149–150, 153–164, 169–171, 174, 176–185, 187–191, 193–199, 201–205, 215–216, 220–228, 232–241, 247–249, 252–253, 260–266, 270–271, 273–278, 280, 282–283, 302–305, 309–310, 312–313, 315–320, 328–330, 341–342, 352 |
| ElliPro antibody epitope prediction (IEDB) | 1–23, 47–55, 73–87, 104–132, 139–147, 205–210, 230–241, 279–297, 299–320, 337–351 |
| Bepipred linear epitope prediction (IEDB) | 25–41, 93–131, 137–150, 173–178, 228–240, 248–275, 281–282, 290–317, 319–319, 339–349 |
| ABCpred prediction server | 2–18, 16–32, 25–41, 50–66, 93–109, 107–123, 118–134, 124–140, 138–154, 159–175, 182–198, 193–209, 204–220, 219–235, 229–245, 248–264, 273–289, 306–322, 314–330, 329–345 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saivish, M.V.; Menezes, G.d.L.; Costa, V.G.d.; Silva, G.C.D.d.; Marques, R.E.; Nogueira, M.L.; Silva, R.A.D. Predicting Antigenic Peptides from Rocio Virus NS1 Protein for Immunodiagnostic Testing Using Immunoinformatics and Molecular Dynamics Simulation. Int. J. Mol. Sci. 2022, 23, 7681. https://doi.org/10.3390/ijms23147681
Saivish MV, Menezes GdL, Costa VGd, Silva GCDd, Marques RE, Nogueira ML, Silva RAD. Predicting Antigenic Peptides from Rocio Virus NS1 Protein for Immunodiagnostic Testing Using Immunoinformatics and Molecular Dynamics Simulation. International Journal of Molecular Sciences. 2022; 23(14):7681. https://doi.org/10.3390/ijms23147681
Chicago/Turabian StyleSaivish, Marielena Vogel, Gabriela de Lima Menezes, Vivaldo Gomes da Costa, Gislaine Celestino Dutra da Silva, Rafael Elias Marques, Maurício Lacerda Nogueira, and Roosevelt Alves Da Silva. 2022. "Predicting Antigenic Peptides from Rocio Virus NS1 Protein for Immunodiagnostic Testing Using Immunoinformatics and Molecular Dynamics Simulation" International Journal of Molecular Sciences 23, no. 14: 7681. https://doi.org/10.3390/ijms23147681
APA StyleSaivish, M. V., Menezes, G. d. L., Costa, V. G. d., Silva, G. C. D. d., Marques, R. E., Nogueira, M. L., & Silva, R. A. D. (2022). Predicting Antigenic Peptides from Rocio Virus NS1 Protein for Immunodiagnostic Testing Using Immunoinformatics and Molecular Dynamics Simulation. International Journal of Molecular Sciences, 23(14), 7681. https://doi.org/10.3390/ijms23147681








