Matrix Metalloproteinases in Dental and Periodontal Tissues and Their Current Inhibitors: Developmental, Degradational and Pathological Aspects
Abstract
:1. Introduction
2. MMPs Grouping and Substrate
3. MMPs and Enamel
4. MMPs and Dentine
5. MMPs and Dental Caries
6. MMPs in Pulpal and Periapical Lesions
7. MMPs and Hybrid Layer Degradation
8. MMPs and Periodontal Tissues
9. MMPs in Orthodontic Tooth Movement
10. MMP Inhibitors
10.1. Chlorhexidine
10.2. Fluorinated Products
10.3. Tetracyclines
11. Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cerdà-Costa, N.; Gomis-Rüth, F.X. Architecture and function of metallopeptidase catalytic domains. Protein Sci. 2014, 23, 123–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Velden, V.H.; Hulsmann, A.R. Peptidases: Structure, function and modulation of peptide-mediated effects in the human lung. Clin. Exp. Allergy 1999, 29, 445–456. [Google Scholar] [CrossRef] [PubMed]
- Frantz, C.; Stewart, K.M.; Weaver, V.M. The extracellular matrix at a glance. J. Cell Sci. 2010, 123, 4195–4200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, A.; Bahuguna, R. Role of matrix metalloproteinases in dental caries, pulp and periapical inflammation: An overview. J. Oral Biol. Craniofac. Res. 2015, 5, 212–218. [Google Scholar] [CrossRef] [Green Version]
- Lu, P.; Takai, K.; Weaver, V.M.; Werb, Z. Extracellular Matrix Degradation and Remodeling in Development and Disease. Cold Spring Harbor Perspect. Biol. 2011, 1, a005058. [Google Scholar] [CrossRef]
- Ra, H.-J.; Parks, W.C. Control of matrix metalloproteinase catalytic activity. Matrix Biol. 2007, 26, 587–596. [Google Scholar] [CrossRef] [Green Version]
- Schiegnitz, E.; Kämmerer, P.; Schön, H.; Gülle, C.; Berres, M.; Sagheb, K.; Al-Nawas, B. The matrix metalloproteinase and insulin-like growth factor system in oral cancer–A prospective clinical study. OncoTargets Ther. 2017, 10, 5099–5105. [Google Scholar] [CrossRef] [Green Version]
- Sternlicht, M.D.; Werb, Z. How Matrix Metalloproteinases Regulate Cell Behavior. Annu. Rev. Cell Dev. Biol. 2001, 17, 463–516. [Google Scholar] [CrossRef] [Green Version]
- Laronha, H.; Caldeira, J. Structure and Function of Human Matrix Metalloproteinases. Cells 2020, 9, 1076. [Google Scholar] [CrossRef]
- Boelen, G.-J.; Boute, L.; D’Hoop, J.; Ezeldeen, M.; Lambrichts, I.; Opdenakker, G. Matrix metalloproteinases and inhibitors in dentistry. Clin. Oral Investig. 2019, 23, 2823–2835. [Google Scholar] [CrossRef]
- Cao, J.; Zucker, S. Introduction to the MMP and TIMP families (structures, substrates) and an overview of diseases where MMPs have been incriminated. Biol. Chem. Matrix Met. 2010, 41, 271–290. [Google Scholar]
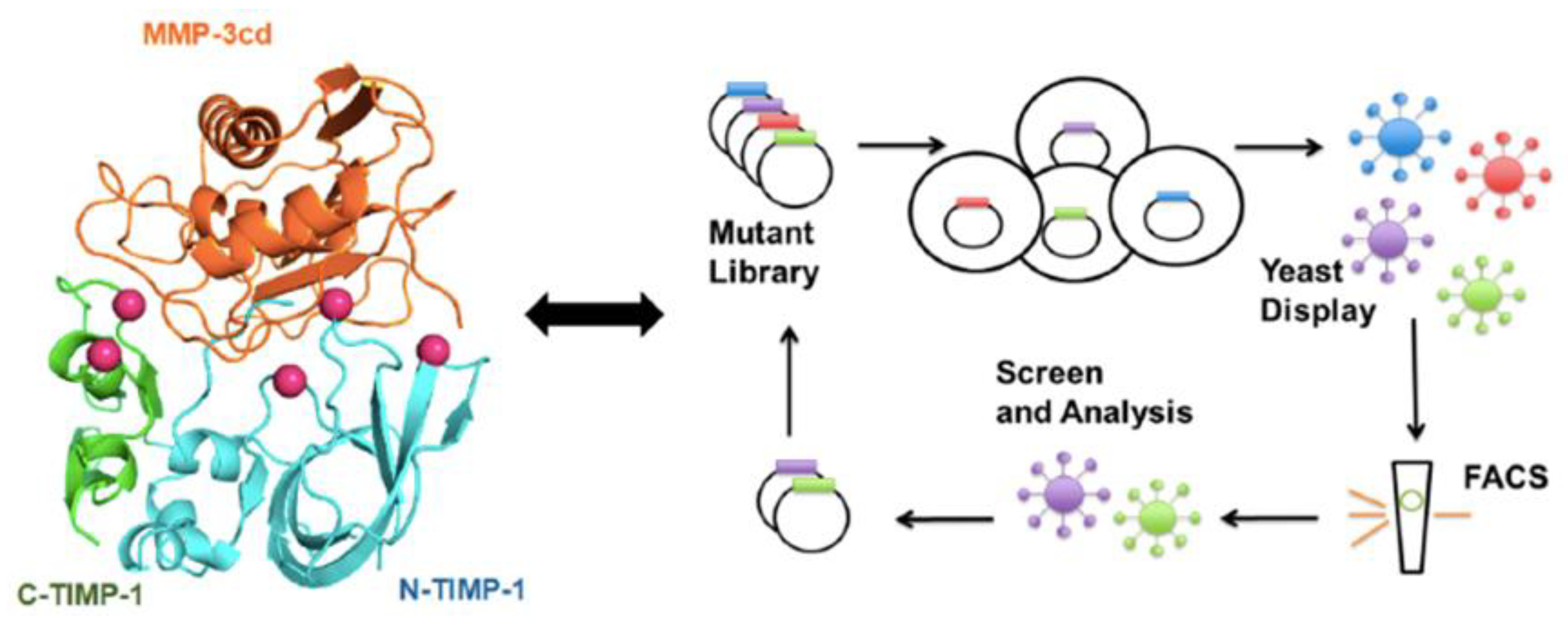
- Raeeszadeh-Sarmazdeh, M.; Do, L.D.; Hritz, B.G. Metalloproteinases and Their Inhibitors: Potential for the Development of New Therapeutics. Cells 2020, 9, 1313. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, D.; Morrison, C.J.; Overall, C.M. Matrix metalloproteinases: What do they not do? New substrates and biological roles identified by murine models and proteomics. Biochim. Biophys. Acta (BBA) Mol. Cell Res. 2010, 1803, 39–54. [Google Scholar] [CrossRef] [Green Version]
- Mazzoni, A.; Tjäderhane, L.; Checchi, V.; Di Lenarda, R.; Salo, T.; Tay, F.R.; Pashley, D.H.; Breschi, L. Role of Dentin MMPs in Caries Progression and Bond Stability. J. Dent. Res. 2015, 94, 241–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Checchi, V.; Maravic, T.; Bellini, P.; Generali, L.; Consolo, U.; Breschi, L.; Mazzoni, A. The Role of Matrix Metalloproteinases in Periodontal Disease. Int. J. Environ. Res. Public Health 2020, 17, 4923. [Google Scholar] [CrossRef]
- Chen, M.; Zeng, J.; Yang, Y.; Wu, B. Diagnostic biomarker candidates for pulpitis revealed by bioinformatics analysis of merged microarray gene expression datasets. BMC Oral Health 2020, 20, 279. [Google Scholar] [CrossRef] [PubMed]
- De Morais, E.F.; Pinheiro, J.C.; Leite, R.B.; Santos, P.P.A.; Barboza, C.A.G.; Freitas, R.A. Matrix metalloproteinase-8 levels in periodontal disease patients: A systematic review. J. Periodont. Res. 2018, 53, 156–163. [Google Scholar] [CrossRef] [PubMed]
- El Gezawi, M.; Wölfle, U.C.; Haridy, R.; Fliefel, R.; Kaisarly, D. Remineralization, Regeneration, and Repair of Natural Tooth Structure: Influences on the Future of Restorative Dentistry Practice. ACS Biomater. Sci. Eng. 2019, 5, 4899–4919. [Google Scholar] [CrossRef]
- Matuszczak, E.; Cwalina, I.; Tylicka, M.; Wawrzyn, K.; Nowosielska, M.; Sankiewicz, A.; Ołdak, Ł.; Gorodkiewicz, E.; Hermanowicz, A. Levels of Selected Matrix Metalloproteinases—MMP-1, MMP-2 and Fibronectin in the Saliva of Patients Planned for Endodontic Treatment or Surgical Extraction. J. Clin. Med. 2020, 9, 3971. [Google Scholar] [CrossRef]
- Pereira Prado, V.; Asquino, N.; Apellaniz, D.; Bueno Rossy, L.; Tapia, G.; Bologna Molina, R. Metalloproteinases (MMPs) of the extracellular matrix in dentistry. In Odontoestomatologia; Springer: Berlin/Heidelberg, Germany, 2016; Volume 18, pp. 19–28. [Google Scholar]
- Sambandam, V.; Neelakantan, P. Matrix metalloproteinases (mmp) in restorative dentistry and endodontics. J. Clin. Pediatr. Dent. 2014, 39, 57–59. [Google Scholar] [CrossRef]
- Tjäderhane, L.; Buzalaf, M.A.R.; Carrilho, M.; Chaussain, C. Matrix Metalloproteinases and Other Matrix Proteinases in Relation to Cariology: The Era of ‘Dentin Degradomics’. Caries Res. 2015, 49, 193–208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Moraes, I.Q.S.; do Nascimento, T.G.; da Silva, A.T.; de Lira, L.M.S.S.; Parolia, A.; de Porto, I.C.C.M. Inhibition of matrix metalloproteinases: A troubleshooting for dentin adhesion. Restor. Dent. Endodont. 2020, 45, e31. [Google Scholar] [CrossRef] [PubMed]
- Klein, T.; Bischoff, R. Physiology and pathophysiology of matrix metalloproteases. Amino Acids 2011, 41, 271–290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, G. Riding the metalloproteinase roller coaster. J. Biol. Chem. 2017, 292, 7708–7718. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vartak, D.G.; Gemeinhart, R.A. Matrix metalloproteases: Underutilized targets for drug delivery. J. Drug Target. 2007, 15, 1–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bartlett, J.D.; Beniash, E.; Lee, D.H.; Smith, C.E. Decreased mineral content in MMP-20 null mouse enamel is prominent during the maturation stage. J. Dent. Res. 2004, 83, 909–913. [Google Scholar] [CrossRef] [PubMed]
- Khaddam, M. Role of EMMPRIN and MMPs in Tooth Development, Dental Caries and Pulp-Dentin Regeneration (Rôle d’EMMPRIN et MMPS dans le Développement Dentaire, la Carie Dentaire et la Régénération Pulpo-Dentinaire). Ph.D. Thesis, Université René Descartes, Paris, France, 2014. [Google Scholar]
- Vasconcelos, K.R.; Arid, J.; Evangelista, S.; Oliveira, S.; Dutra, A.L.; Silva, L.A.B.; Segato, R.A.B.; Vieira, A.R.; Nelson-Filho, P.; Küchler, E.C. MMP13 Contributes to Dental Caries Associated with Developmental Defects of Enamel. Caries Res. 2019, 53, 441–446. [Google Scholar] [CrossRef]
- Sandoval, N.G.; Nayra, S.L.; Bautz, W.G.; Gama-de-Souza, L.N.; Karla, L.C. Matrix Metalloproteinase 2: A Possible Role inTooth Development and Eruption. Odovtos-Int. J. Dent. Sci. 2019, 21, 41–51. [Google Scholar] [CrossRef]
- Gomes, J.R.; Omar, N.F.; Dos Santos Neves, J.; Narvaes, E.A.; Novaes, P.D. Increase of MT1-MMP, TIMP-2 and Ki-67 proteins in the odontogenic region of the rat incisor post-shortening procedure. J. Mol. Histol. 2010, 41, 333–341. [Google Scholar] [CrossRef]
- Goldberg, M.; Kulkarni, A.B.; Young, M.; Boskey, A. Dentin: Structure, composition and mineralization. Front. Biosci. 2011, 3, 711–735. [Google Scholar] [CrossRef]
- Baranova, J.; Büchner, D.; Götz, W.; Schulze, M.; Tobiasch, E. Tooth Formation: Are the Hardest Tissues of Human Body Hard to Regenerate? Int. J. Mol. Sci. 2020, 21, 4031. [Google Scholar] [CrossRef] [PubMed]
- Chaussain, C.; Boukpessi, T.; Khaddam, M.; Tjaderhane, L.; George, A.; Menashi, S. Dentin matrix degradation by host matrix metalloproteinases: Inhibition and clinical perspectives toward regeneration. Front. Physiol. 2013, 4, 308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuan, G.; Chen, L.; Feng, J.; Yang, G.; Ni, Q.; Xu, X.; Wan, C.; Lindsey, M.; Donly, K.J.; MacDougall, M.; et al. Dentin Sialoprotein is a Novel Substrate of Matrix Metalloproteinase 9 in vitro and in vivo. Sci. Rep. 2017, 7, 42449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gobbi, P.; Maravic, T.; Comba, A.; Mazzitelli, C.; Mancuso, E.; Falconi, M.; Breschi, L.; Mazzoni, A. Biochemical and immunohistochemical analysis of tissue inhibitor of metalloproteinases-1 in human sound dentin. Clin. Oral Investig. 2021, 25, 5067–5075. [Google Scholar] [CrossRef]
- Chaussain-Miller, C.; Fioretti, F.; Goldberg, M.; Menashi, S. The Role of Matrix Metalloproteinases (MMPs) in Human Caries. J. Dent. Res. 2006, 85, 22–32. [Google Scholar] [CrossRef]
- Deo, P.N.; Deshmukh, R. Oral microbiome: Unveiling the fundamentals. J. Oral Maxillofac. Pathol. JOMFP 2019, 23, 122–128. [Google Scholar] [CrossRef]
- Featherstone, J.D. Dental caries: A dynamic disease process. Aust. Dent. J. 2008, 53, 286–291. [Google Scholar] [CrossRef]
- Takahashi, N.; Nyvad, B. Ecological Hypothesis of Dentin and Root Caries. Caries Res. 2016, 50, 422–431. [Google Scholar] [CrossRef]
- Besinis, A.; van Noort, R.; Martin, N. Remineralization potential of fully demineralized dentin infiltrated with silica and hydroxyapatite nanoparticles. Dent. Mater. 2014, 30, 249–262. [Google Scholar] [CrossRef]
- Allam, E.; Feitosa, S.; Palasuk, J.; Bottino, M.C.; Windsor, L.J. Roles of Matrix Metalloproteinases in Periodontal Diseases and Dental Caries. In Matrix Metalloproteinases (MMPs): Classification, Molecular Mechanisms and Roles in Diseases; Sullivan, J., Ed.; Nova Science Publishers, Inc.: Hauppage, NY, USA, 2015; pp. 33–57. [Google Scholar]
- Ballal, V.; Rao, S.; Bagheri, A.; Bhat, V.; Attin, T.; Zehnder, M. MMP-9 in Dentinal Fluid Correlates with Caries Lesion Depth. Caries Res. 2017, 51, 460–465. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.; Miao, C.; Tian, Z.; Li, J.; Zhang, C.; Yang, D. The Effect of Chemically Modified Tetracycline-3 on the Progression of Dental Caries in Rats. Caries Res. 2018, 52, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Brodzikowska, A.; Gondek, A.; Rak, B.; Paskal, W.; Pełka, K.; Cudnoch-Jędrzejewska, A.; Włodarski, P. Metalloproteinase 14 (MMP-14) and hsa-miR-410-3p expression in human inflamed dental pulp and odontoblasts. Histochem. Cell Biol. 2019, 152, 345–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Femiano, F.; Femiano, R.; Femiano, L.; Jamilian, A.; Rullo, R.; Perillo, L. Dentin caries progression and the role of metalloproteinases: An update. Eur. J. Paediatr. Dent. 2016, 17, 243–247. [Google Scholar] [PubMed]
- Borilova Linhartova, P.; Deissova, T.; Kukletova, M.; Izakovicova Holla, L. Matrix metalloproteinases gene variants and dental caries in Czech children. BMC Oral Health 2020, 20, 138. [Google Scholar] [CrossRef] [PubMed]
- Lewis, D.D.; Shaffer, J.R.; Feingold, E.; Cooper, M.; Vanyukov, M.M.; Maher, B.S.; Slayton, R.L.; Willing, M.C.; Reis, S.E.; McNeil, D.W.; et al. Genetic Association of MMP10, MMP14, and MMP16 with Dental Caries. Int. J. Dent. 2017, 2017, 8465125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hannas, A.R.; Kato, M.T.; Cardoso, C.D.A.B.; Magalhães, A.C.; Pereira, J.C.; Tjäderhane, L.; Buzalaf, M.A.R. Preventive effect of toothpastes with MMP inhibitors on human dentine erosion and abrasion in vitro. J. Appl. Oral Sci. 2016, 24, 61–66. [Google Scholar] [CrossRef]
- Gonçalves, R.S.; Scaffa, P.M.C.; Giacomini, M.C.; Vidal, C.M.P.; Honório, H.M.; Wang, L. Sodium Trimetaphosphate as a Novel Strategy for Matrix Metalloproteinase Inhibition and Dentin Remineralization. Caries Res. 2018, 52, 189–198. [Google Scholar] [CrossRef]
- Kato, M.T.; Bolanho, A.; Zarella, B.L.; Salo, T.; Tjäderhane, L.; Buzalaf, M.A.R. Sodium Fluoride Inhibits MMP-2 and MMP-9. J. Dent. Res. 2014, 93, 74–77. [Google Scholar] [CrossRef] [Green Version]
- Zhao, I.S.; Gao, S.S.; Hiraishi, N.; Burrow, M.F.; Duangthip, D.; Mei, M.L.; Lo, E.C.-M.; Chu, C.-H. Mechanisms of silver diamine fluoride on arresting caries: A literature review. Int. Dent. J. 2018, 68, 67–76. [Google Scholar] [CrossRef] [Green Version]
- Mei, M.L.; Lo, E.C.M.; Chu, C.H. Arresting Dentine Caries with Silver Diamine Fluoride: What’s Behind It? J. Dent. Res. 2018, 97, 751–758. [Google Scholar] [CrossRef]
- Wahlgren, J.; Salo, T.; Teronen, O.; Luoto, H.; Sorsa, T.; Tjäderhane, L. Matrix metalloproteinase-8 (MMP-8) in pulpal and periapical inflammation and periapical root-canal exudates. Int. Endodont. J. 2002, 35, 897–904. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.F.C.; Antunes, L.S.; Oliveira, N.F.; Küchler, E.C.; Gomes, C.C.; Antunes, L.A.A. Genetic Polymorphism and Expression of Matrix Metalloproteinases and Tissue Inhibitors of Metalloproteinases in Periapical Lesions: Systematic Review. J. Endodont. 2020, 46, 3–11.e1. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, M.; Takahashi, Y.; Komichi, S.; Cooper, P.R.; Hayashi, M. Dentinogenic effects of extracted dentin matrix components digested with matrix metalloproteinases. Sci. Rep. 2018, 8, 10690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pattamapun, K.; Handagoon, S.; Sastraruji, T.; Gutmann, J.L.; Pavasant, P.; Krisanaprakornkit, S. Decreased levels of matrix metalloproteinase-2 in root-canal exudates during root canal treatment. Arch. Oral Biol. 2017, 82, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Aguirre-López, E.C.; Patiño-Marín, N.; Martínez-Castañón, G.A.; Medina-Solís, C.E.; Castillo-Silva, B.E.; Cepeda-Argüelles, O.; Aguilera-Galaviz, L.A.; Rosales-García, P. Levels of matrix metalloproteinase-8 and cold test in reversible and irreversible pulpitis. Medicine 2020, 99, e23782. [Google Scholar] [CrossRef] [PubMed]
- Akbal Dincer, G.; Erdemir, A.; Kisa, U. Comparison of Neurokinin A, Substance P, Interleukin 8, and Matrix Metalloproteinase-8 Changes in Pulp tissue and Gingival Crevicular Fluid Samples of Healthy and Symptomatic Irreversible Pulpitis Teeth. J. Endodont. 2020, 46, 1428–1437. [Google Scholar] [CrossRef]
- Cunha, N.N.D.O.; Junqueira, M.A.; Cosme-Silva, L.; Santos, L.D.S.T.; Oliveira, G.A.V.D.; Moretti Neto, R.T.; Nogueira, D.A.; Brigagão, M.R.P.L.; Moretti, A.B.D.S. Expression of Matrix Metalloproteinases-8 and Myeloperoxidase in Pulp Tissue after Pulpotomy with Calcium Silicate Cements. Pesq. Bras. Odontopediatr. Clín. Integr. 2021, 21, 38. [Google Scholar] [CrossRef]
- Tsai, C.H.; Chen, Y.J.; Huang, F.M.; Su, Y.F.; Chang, Y.C. The upregulation of matrix metalloproteinase-9 in inflamed human dental pulps. J. Endodont. 2005, 31, 860–862. [Google Scholar] [CrossRef]
- Sharma, R.; Kumar, V.; Logani, A.; Chawla, A.; Mir, R.A.; Sharma, S.; Kalaivani, M. Association between concentration of active MMP-9 in pulpal blood and pulpotomy outcome in permanent mature teeth with irreversible pulpitis-a preliminary study. Int. Endodont. J. 2021, 54, 479–489. [Google Scholar] [CrossRef]
- Schmidt, J.; Hübler, C.; Krohn, S.; Schmalz, G.; Schneider, H.; Berg, T.; Haak, R.; Ziebolz, D. Detection of Inflammatory and Homeostasis Biomarkers after Selective Removal of Carious Dentin—An In Vivo Feasibility Study. J. Clin. Med. 2021, 10, 1003. [Google Scholar] [CrossRef]
- Barreiros, D.; Nelson, P.; Paula-Silva, F.W.G.; Oliveira, K.M.H.; Lucisano, M.P.; Rossi, A.; Silva, L.A.B.; Küchler, E.C.; Silva, R.A.B. MMP2 and MMP9 are Associated with Apical Periodontitis Progression and Might be Modulated by TLR2 and MyD88. Braz. Dent. J. 2018, 29, 43–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kermeoğlu, F.; Aksoy, U.; Sebai, A.; Savtekin, G.; Özkayalar, H.; Sayıner, S.; Şehirli, A.Ö. Anti-Inflammatory Effects of Melatonin and 5-Methoxytryptophol on Lipopolysaccharide-Induced Acute Pulpitis in Rats. BioMed Res. Int. 2021, 2021, 8884041. [Google Scholar] [CrossRef]
- Sarmento, E.B.; Gomes, C.C.; Pires, F.R.; Pinto, L.C.; Antunes, L.A.A.; Armada, L. Immunoexpression of bone resorption biomarkers in apical periodontitis in diabetics and normoglycaemics. Int. Endodont. J. 2020, 53, 1025–1032. [Google Scholar] [CrossRef]
- Carvalho, C.A.T.; Hasna, A.A.; Carvalho, A.S.; Vilela, P.D.G.F.; Ramos, L.P.; Valera, M.C.; Oliveira, L.D. Clinical Study of Sodium Hypochlorite, Polymyxin B And Limewater Effect on MMP-3,-8,-9 In Apical Periodontitis. Braz. Dent. J. 2020, 31, 116–121. [Google Scholar] [CrossRef] [PubMed]
- El-Gezawi, M.F.; Al-Harbi, F.A. Reliability of Bonded MOD Restorations in Maxillary Premolars: Microleakage and Cusp Fracture Resistance. Acta stomatol. Croat. 2012, 46, 31–42. [Google Scholar]
- El Gezawi, M.; Haridy, R.; Abo Elazm, E.; Al-Harbi, F.; Zouch, M.; Kaisarly, D. Microtensile bond strength, 4-point bending and nanoleakage of resin-dentin interfaces: Effects of two matrix metalloproteinase inhibitors. J. Mech. Behav. Biomed. Mater. 2018, 78, 206–213. [Google Scholar] [CrossRef]
- Longhi, M.; Cerroni, L.; Condò, S.G.; Ariano, V.; Pasquantonio, G. The effects of host derived metalloproteinases on dentin bond and the role of MMPs inhibitors on dentin matrix degradation. Oral Implantol. 2014, 7, 71–79. [Google Scholar]
- Münchow, E.A.; Bottino, M.C. Recent Advances in Adhesive Bonding-The Role of Biomolecules, Nanocompounds, and Bonding Strategies in Enhancing Resin Bonding to Dental Substrates. Curr. Oral Health Rep. 2017, 4, 215–227. [Google Scholar] [CrossRef]
- Pashley, D.H.; Tay, F.R.; Imazato, S. How to increase the durability of resin-dentin bonds. Compend. Cont. Educ. Dent. 2011, 32, 60–64. [Google Scholar]
- Franco, C.; Patricia, H.R.; Timo, S.; Claudia, B.; Marcela, H. Matrix Metalloproteinases as Regulators of Periodontal Inflammation. Int. J. Mol. Sci. 2017, 18, 440. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.; Zhang, H.; Wang, J.; Zhang, Z.; Li, C. Puerarin decreases bone loss and collagen destruction in rats with ligature-induced periodontitis. J. Periodont. Res. 2015, 50, 748–757. [Google Scholar] [CrossRef] [PubMed]
- Branco-de-Almeida, L.S.; Franco, G.C.; Castro, M.L.; Dos Santos, J.G.; Anbinder, A.L.; Cortelli, S.C.; Kajiya, M.; Kawai, T.; Rosalen, P.L. Fluoxetine inhibits inflammatory response and bone loss in a rat model of ligature-induced periodontitis. J. Periodontol. 2012, 83, 664–671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, D.; Wang, J.; Ni, J.; Shang, S.; Liu, L.; Xiang, J.; Li, C. Temporal expression of metalloproteinase-8 and -13 and their relationships with extracellular matrix metalloproteinase inducer in the development of ligature-induced periodontitis in rats. J. Periodont. Res. 2013, 48, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Sakagami, G.; Sato, E.; Sugita, Y.; Kosaka, T.; Kubo, K.; Maeda, H.; Kameyama, Y. Effects of nifedipine and interleukin-1alpha on the expression of collagen, matrix metalloproteinase-1, and tissue inhibitor of metalloproteinase-1 in human gingival fibroblasts. J. Periodont. Res. 2006, 41, 266–272. [Google Scholar] [CrossRef]
- Türkoğlu, O.; Becerik, S.; Tervahartiala, T.; Sorsa, T.; Atilla, G.; Emingil, G. The effect of adjunctive chlorhexidine mouthrinse on GCF MMP-8 and TIMP-1 levels in gingivitis: A randomized placebo-controlled study. BMC Oral Health 2014, 14, 55. [Google Scholar] [CrossRef] [Green Version]
- Azmak, N.; Atilla, G.; Luoto, H.; Sorsa, T. The effect of subgingival controlled-release delivery of chlorhexidine chip on clinical parameters and matrix metalloproteinase-8 levels in gingival crevicular fluid. J. Periodontol. 2002, 73, 608–615. [Google Scholar] [CrossRef]
- De Colli, M.; Tortorella, P.; Agamennone, M.; Campestre, C.; Loiodice, F.; Cataldi, A.; Zara, S. Bisphosfonate matrix metalloproteinase inhibitors for the treatment of periodontitis: An in vitro study. Int. J. Mol. Med. 2018, 42, 651–657. [Google Scholar] [CrossRef] [Green Version]
- Nakaya, H.; Osawa, G.; Iwasaki, N.; Cochran, D.L.; Kamoi, K.; Oates, T.W. Effects of bisphosphonate on matrix metalloproteinase enzymes in human periodontal ligament cells. J. Periodontol. 2000, 71, 1158–1166. [Google Scholar] [CrossRef]
- Björnsson, M.J.; Havemose-Poulsen, A.; Stoltze, K.; Holmstrup, P. Influence of the matrix metalloproteinase inhibitor batimastat (BB-94) on periodontal bone destruction in Sprague-Dawley rats. J. Periodontal. Res. 2004, 39, 269–274. [Google Scholar] [CrossRef]
- Gupta, N.; Gupta, N.D.; Gupta, A.; Khan, S.; Bansal, N. Role of salivary matrix metalloproteinase-8 (MMP-8) in chronic periodontitis diagnosis. Front. Med. 2015, 9, 72–76. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Duarte, C.; Moriyama, K. Hormone Relaxin as Biomarker for Bone Health and Disease. In Biomarkers in Bone Disease; Preedy, V.R., Ed.; Springer Netherlands: Dordrecht, The Netherlands, 2016; pp. 1–25. [Google Scholar]
- Tay, C.X.; Quah, S.Y.; Lui, J.N.; Yu, V.S.; Tan, K.S. Matrix Metalloproteinase Inhibitor as an Antimicrobial Agent to Eradicate Enterococcus faecalis Biofilm. J. Endodont. 2015, 41, 858–863. [Google Scholar] [CrossRef] [PubMed]
- Lütfioğlu, M.; Sakallıoğlu, E.E.; Sakallıoğlu, U.; Gülbahar, M.Y.; Muğlalı, M.; Baş, B.; Aksoy, A. Excessıve fluorıde ıntake alters the MMP-2, TIMP-1 and TGF-β levels of perıodontal soft tıssues: An experımental study ın rabbıts. Clin. Oral Investig. 2012, 16, 1563–1570. [Google Scholar] [CrossRef] [PubMed]
- Luchian, I.; Goriuc, A.; Sandu, D.; Covasa, M. The Role of Matrix Metalloproteinases (MMP-8, MMP-9, MMP-13) in Periodontal and Peri-Implant Pathological Processes. Int. J. Mol. Sci. 2022, 23, 1806. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, I.; Onodera, K.; Nishimura, M.; Mitnai, H.; Sasano, Y.; Mitani, H. Expression of genes for gelatinases and tissue inhibitors of metalloproteinases in periodontal tissues during orthodontic tooth movement. J. Mol. Histol. 2006, 37, 333–342. [Google Scholar] [CrossRef]
- Cantarella, G.; Cantarella, R.; Caltabiano, M.; Risuglia, N.; Bernardini, R.; Leonardi, R. Levels of matrix metalloproteinases 1 and 2 in human gingival crevicular fluid during initial tooth movement. Am. J. Orthodont. Dentofac. Orthop. 2006, 130, 568.e11–568.e16. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.J.; Jeng, J.H.; Chang, H.H.; Huang, M.Y.; Tsai, F.F.; Yao, C.C. Differential regulation of collagen, lysyl oxidase and MMP-2 in human periodontal ligament cells by low- and high-level mechanical stretching. J. Periodont. Res. 2013, 48, 466–474. [Google Scholar] [CrossRef]
- He, Y.; Macarak, E.J.; Korostoff, J.M.; Howard, P.S. Compression and tension: Differential effects on matrix accumulation by periodontal ligament fibroblasts in vitro. Connect. Tissue Res. 2004, 45, 28–39. [Google Scholar] [CrossRef] [PubMed]
- Canavarro, C.; Teles, R.P.; Capelli Júnior, J. Matrix metalloproteinases -1, -2, -3, -7, -8, -12, and -13 in gingival crevicular fluid during orthodontic tooth movement: A longitudinal randomized split-mouth study. Eur. J. Orthodont. 2013, 35, 652–658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garlet, T.P.; Coelho, U.; Silva, J.S.; Garlet, G.P. Cytokine expression pattern in compression and tension sides of the periodontal ligament during orthodontic tooth movement in humans. Eur. J. Oral Sci. 2007, 115, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Alikhani, M.; Chou, M.Y.; Khoo, E.; Alansari, S.; Kwal, R.; Elfersi, T.; Almansour, A.; Sangsuwon, C.; Al Jearah, M.; Nervina, J.M.; et al. Age-dependent biologic response to orthodontic forces. Am. J. Orthodont. Dentofac. Orthop. 2018, 153, 632–644. [Google Scholar] [CrossRef]
- Shirozaki, M.U.; da Silva, R.A.B.; Romano, F.L.; da Silva, L.A.B.; de Rossi, A.; Lucisano, M.P.; Messora, M.R.; Feres, M.; Novaes Júnior, A.B. Clinical, microbiological, and immunological evaluation of patients in corrective orthodontic treatment. Prog. Orthod. 2020, 21, 307. [Google Scholar] [CrossRef] [PubMed]
- Behm, C.; Nemec, M.; Weissinger, F.; Rausch, M.A.; Andrukhov, O.; Jonke, E. MMPs and TIMPs Expression Levels in the Periodontal Ligament during Orthodontic Tooth Movement: A Systematic Review of In Vitro and In Vivo Studies. Int. J. Mol. Sci. 2021, 22, 6967. [Google Scholar] [CrossRef] [PubMed]
- Tantilertanant, Y.; Niyompanich, J.; Everts, V.; Supaphol, P.; Pavasant, P.; Sanchavanakit, N. Cyclic tensile force-upregulated IL6 increases MMP3 expression by human periodontal ligament cells. Arch. Oral Biol. 2019, 107, 104495. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, I.; Nishimura, M.; Onodera, K.; Bae, J.W.; Mitani, H.; Okazaki, M.; Sasano, Y. Expression of MMP-8 and MMP-13 genes in the periodontal ligament during tooth movement in rats. J. Dent. Res. 2003, 82, 646–651. [Google Scholar] [CrossRef]
- Holliday, L.S.; Vakani, A.; Archer, L.; Dolce, C. Effects of matrix metalloproteinase inhibitors on bone resorption and orthodontic tooth movement. J. Dent. Res. 2003, 82, 687–691. [Google Scholar] [CrossRef]
- Sulkala, M. Matrix Metalloproteinases (MMPs) in the Dentin-Pulp Complex of Healthy and Carious Teeth. Ph.D.Thesis, University of Oulu, Oulu, Finnland, 2004. [Google Scholar]
- Benjamin, M.M.; Khalil, R.A. Matrix metalloproteinase inhibitors as investigative tools in the pathogenesis and management of vascular disease. Exp. Suppl. 2012, 103, 209–279. [Google Scholar] [CrossRef] [Green Version]
- Cabral-Pacheco, G.A.; Garza-Veloz, I.; Castruita-De la Rosa, C.; Ramirez-Acuña, J.M.; Perez-Romero, B.A.; Guerrero-Rodriguez, J.F.; Martinez-Avila, N.; Martinez-Fierro, M.L. The Roles of Matrix Metalloproteinases and Their Inhibitors in Human Diseases. Int. J. Mol. Sci. 2020, 21, 9739. [Google Scholar] [CrossRef]
- Akcalı, A.; Bostanci, N.; Özçaka, Ö.; Öztürk-Ceyhan, B.; Gümüş, P.; Tervahartiala, T.; Husu, H.; Buduneli, N.; Sorsa, T.; Belibasakis, G.N. Elevated matrix metalloproteinase-8 in saliva and serum in polycystic ovary syndrome and association with gingival inflammation. Innate Immun. 2015, 21, 619–625. [Google Scholar] [CrossRef]
- Golbasi, F.; Erdemir, A.; Kisa, U. Comparison of ADAMTS Levels in Pulp Tissue Samples of Healthy and Symptomatic Irreversible Pulpitis Teeth. J. Endodont. 2022, 48, 496–501. [Google Scholar] [CrossRef]
- Letra, A.; Ghaneh, G.; Zhao, M.; Ray, H.; Francisconi, C.F.; Garlet, G.P.; Silva, R.M. MMP-7 and TIMP-1, new targets in predicting poor wound healing in apical periodontitis. J. Endodont. 2013, 39, 1141–1146. [Google Scholar] [CrossRef]
- Wan, C.Y.; Li, L.; Liu, L.S.; Jiang, C.M.; Zhang, H.Z.; Wang, J.X. Expression of Matrix Metalloproteinases and Tissue Inhibitor of Matrix Metalloproteinases during Apical Periodontitis Development. J. Endodont. 2021, 47, 1118–1125. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Li, M.; Wang, W.; Wu, Z.; Wang, C.; Jin, X.; Zhang, L.; Jiang, W.; Fu, B. A novel prime-&-rinse mode using MDP and MMPs inhibitors improves the dentin bond durability of self-etch adhesive. J. Mech. Behav. Biomed. Mater. 2020, 104, 103698. [Google Scholar] [CrossRef] [PubMed]
- Scaffa, P.M.; Vidal, C.M.; Barros, N.; Gesteira, T.F.; Carmona, A.K.; Breschi, L.; Pashley, D.H.; Tjäderhane, L.; Tersariol, I.L.; Nascimento, F.D.; et al. Chlorhexidine inhibits the activity of dental cysteine cathepsins. J. Dent. Res. 2012, 91, 420–425. [Google Scholar] [CrossRef]
- Akram, Z.; Daood, U.; Aati, S.; Ngo, H.; Fawzy, A.S. Formulation of pH-sensitive chlorhexidine-loaded/mesoporous silica nanoparticles modified experimental dentin adhesive. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 122, 111894. [Google Scholar] [CrossRef]
- De Menezes, L.R.; da Silva, E.O.; Maurat da Rocha, L.V.; Ferreira Barbosa, I.; Rodrigues Tavares, M. The use of clays for chlorhexidine controlled release as a new perspective for longer durability of dentin adhesion. J. Mater. Sci. Mater. Med. 2019, 30, 132. [Google Scholar] [CrossRef]
- Montagner, A.F.; Sarkis-Onofre, R.; Pereira-Cenci, T.; Cenci, M.S. MMP Inhibitors on Dentin Stability: A Systematic Review and Meta-analysis. J. Dent. Res. 2014, 93, 733–743. [Google Scholar] [CrossRef] [Green Version]
- Osorio, R.; Yamauti, M.; Osorio, E.; Ruiz-Requena, M.E.; Pashley, D.; Tay, F.; Toledano, M. Effect of dentin etching and chlorhexidine application on metalloproteinase-mediated collagen degradation. Eur. J. Oral Sci. 2011, 119, 79–85. [Google Scholar] [CrossRef] [Green Version]
- Zhou, J.; Tan, J.; Yang, X.; Xu, X.; Li, D.; Chen, L. MMP-inhibitory effect of chlorhexidine applied in a self-etching adhesive. J. Adhes. Dent. 2011, 13, 111–115. [Google Scholar] [CrossRef]
- Brackett, M.G.; Agee, K.A.; Brackett, W.W.; Key, W.O.; Sabatini, C.; Kato, M.T.; Buzalaf, M.A.; Tjäderhane, L.; Pashley, D.H. Effect of Sodium Fluoride on the endogenous MMP Activity of Dentin Matrices. J. Nat. Sci. 2015, 1, e118. [Google Scholar]
- Altinci, P.; Mutluay, M.; Tjäderhane, L.; Tezvergil-Mutluay, A. Inhibition of dentin matrix-bound cysteine cathepsins by potassium fluoride. Eur. J. Oral Sci. 2019, 127, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Gonçalves, R.S.; Candia Scaffa, P.M.; Giacomini, M.C.; Rabelo Buzalaf, M.A.; Honório, H.M.; Wang, L. Use of sodium trimetaphosphate in the inhibition of dentin matrix metalloproteinases and as a remineralizing agent. J. Dent. 2018, 68, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Cvikl, B.; Lussi, A.; Carvalho, T.S.; Moritz, A.; Gruber, R. Stannous chloride and stannous fluoride are inhibitors of matrix metalloproteinases. J. Dent. 2018, 78, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, R.E.; Libert, C. Is there new hope for therapeutic matrix metalloproteinase inhibition? Nat. Rev. Drug Discov. 2014, 13, 904–927. [Google Scholar] [CrossRef] [PubMed]
- Oliveira Hde, L.; Tedesco, T.K.; Rodrigues-Filho, L.E.; Soares, F.Z.; Rocha Rde, O. Doxycycline as a matrix metalloproteinase inhibitor to prevent bond degradation: The effect of acid and neutral solutions on dentin bond strength. Gen. Dent. 2016, 64, 14–17. [Google Scholar]
- Feitosa, S.A.; Palasuk, J.; Kamocki, K.; Geraldeli, S.; Gregory, R.L.; Platt, J.A.; Windsor, L.J.; Bottino, M.C. Doxycycline-encapsulated nanotube-modified dentin adhesives. J. Dent. Res. 2014, 93, 1270–1276. [Google Scholar] [CrossRef] [Green Version]
- Ramamurthy, N.S.; Rifkin, B.R.; Greenwald, R.A.; Xu, J.W.; Liu, Y.; Turner, G.; Golub, L.M.; Vernillo, A.T. Inhibition of matrix metalloproteinase-mediated periodontal bone loss in rats: A comparison of 6 chemically modified tetracyclines. J. Periodontol. 2002, 73, 726–734. [Google Scholar] [CrossRef]
- Breschi, L.; Martin, P.; Mazzoni, A.; Nato, F.; Carrilho, M.; Tjäderhane, L.; Visintini, E.; Cadenaro, M.; Tay, F.R.; Dorigo, E.D.S.; et al. Use of a specific MMP-inhibitor (galardin) for preservation of hybrid layer. Dent. Mater. 2010, 26, 571–578. [Google Scholar] [CrossRef] [Green Version]
- Shailendra, M.; Bhandari, S.; Kulkarni, S.; Janavathi, K.; Ghatole, K. Evaluation of indomethacin as matrix metalloproteases inhibitor in human dentin. J. Conserv. Dent. 2019, 22, 598–601. [Google Scholar] [CrossRef]
| Type of MMP | Name | Substrate | Production | Physiological Function | Associated Diseases |
|---|---|---|---|---|---|
| MMP-1 | Collagenase 1/Interstitial Collagenase/Fibroblast Collagenase | Collagen I, II, III, VII, VIII, X, XI, Gelatin, Fibronectin, Aggrecan, Entactin, Tenascin, Ovostatin, Casein | Fibroblast, Keratinocytes, Endothelial cells, Macrophages, Osteoblast, Chondrocytes, Platelet | Wound healing, re-epithelialization, cell proliferation, keratinocyte migration | Periodontitis, rheumatoid arthritis, atherosclerosis, fibrosis, autoimmune disease, cancer |
| MMP-2 | Gelatinase A/72-kDa type IV collagenase | Collagen, Elastin, Endothelin, Fibroblast growth factor, MMP-9, MMP-13, Plasminogen, and TGF-β, | Cardiomyocytes, Fibroblasts, and Myofibroblasts. | Neovascularization, Angiogenesis, Promoting and inhibiting Inflammation, | Cancer, asthma, lung diseases, |
| MMP-8 | Collagenase 2/Neutrophil Collagenase | Collagen I, II, III, Fibronectin, Aggrecan, Ovostatin | Chondrocytes, Endothelial cell, Macrophages, Smooth muscle cell | Periodontal tissue turnover, Anti-inflammatory activity, Wound healing | Periodontitis, rheumatoid arthritis, asthma, cancer |
| MMP-9 | Gelatinase B/92-kDa type IV collagenase | Gelatin, Type V collagen, Laminin, Fibronectin | Neutrophils, Eosinophils, Epithelial cells | Wound healing, embryo implantation, neovascularization, immune cells function, tissue remodeling | Arthritis, metastasis, pulmonary disease, infections, cardiovascular disease, periodontal disease |
| MMP-12 | Macrophage elastase | Elastin, Laminin, Fibronectin, Vitronectin, Type IV collagen | Endothelial cells, Neutrophils, Fibroblasts, T-cells, Myocytes, Macrophages, | degrade extracellular matrix component | Emphysema, arthritis, cancer, periodontal disease |
| MMP-13 | Collagenase 3 | Collagen I, II, III, IV, IX, X, XIV, Fibronectin, Laminin, Gelatin, Aggrecan, Plasminogen, Osteonectin | Epithelial cell, Neuronal cell, Connective tissue (Cartilage and Bone) | Osteoclastic activation, anti-inflammatory activity | Periodontitis, osteoarthritis, liver fibrosis, cancer |
| MMPs Groups | Enamel | Dentine | Pulp and Periapical Lesions | Periodontal Ligament | Dental Caries | Orthodontic Tooth Movement |
|---|---|---|---|---|---|---|
| 1. Collagenases MMP-1 MMP-8 MMP-13 | MMP-13 mucosal penetration during tooth eruption | MMP-8 and MMP-13 Dentinogenesis MMP-8 reparative dentine formation | MMP-1, -8, -13 reparative dentine formation MMP-1 acute pulpitis | MMP-1 periodontitis MMP-8 gingivitis MMP-13 periodontitis | MMP-1, 8 pathogenesis of caries | MMP-1, -8, -13 expressed in crevicular fluid during orthodontic treatment |
| 2. Gelatinases MMP-2 MMP-9 | MMP-2, MMP-9 mucosal penetration during tooth eruption | MMP-2, 9 dentinogenesis | MMP-9 reparative dentine formation MMP-2 acute pulpitis MMP-2, -9 progression of apical periodontitis MMP-9 alveolar bone resorption | MMP-9 gingivitis | MMP-2, 9 pathogenesis of caries | MMP-2 expressed in crevicular fluid during orthodontic treatment |
| 3. Stromelysins MMP-3 MMP-10 MMP-11 MMP-12 | MMP-3 dentine mineralization | MMP-3 reparative dentine formation | MMP-3 pathogenesis of caries | MMP-3, -12 expressed in crevicular fluid during orthodontic treatment | ||
| 4. Matrilysins MMP-7 MMP-26 | MMP-7 expressed in crevicular fluid during orthodontic treatment | |||||
| 5. MT-MMPs (Membrane type) MMPs-14(MT1-MMP) MMPs-15(MT2-MMP) MMPs-16(MT3-MMP) MMPs-17(MT4-MMP) MMPs-24(MT5-MMP) MMPs-25(MT6-MMP) | MMPs-14 dentinogenesis MT1-MMPs and TIMP-2 correlate to the rate of tooth eruption | MMP-16 pathogenesis of caries | ||||
| 6. Other MMPs MMPs-18 MMP-19 MMPs20(enamelysin) MMPs21 MMPs-23 MMPs-27 MMPs-28 | MMPs-19 dentinogenesis MMPs-20 (amelogenesis and dentinogenesis) | MMP-20 reparative dentine formation | MMP-20 pathogenesis of caries |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elgezawi, M.; Haridy, R.; Almas, K.; Abdalla, M.A.; Omar, O.; Abuohashish, H.; Elembaby, A.; Christine Wölfle, U.; Siddiqui, Y.; Kaisarly, D. Matrix Metalloproteinases in Dental and Periodontal Tissues and Their Current Inhibitors: Developmental, Degradational and Pathological Aspects. Int. J. Mol. Sci. 2022, 23, 8929. https://doi.org/10.3390/ijms23168929
Elgezawi M, Haridy R, Almas K, Abdalla MA, Omar O, Abuohashish H, Elembaby A, Christine Wölfle U, Siddiqui Y, Kaisarly D. Matrix Metalloproteinases in Dental and Periodontal Tissues and Their Current Inhibitors: Developmental, Degradational and Pathological Aspects. International Journal of Molecular Sciences. 2022; 23(16):8929. https://doi.org/10.3390/ijms23168929
Chicago/Turabian StyleElgezawi, Moataz, Rasha Haridy, Khalid Almas, Moamen A. Abdalla, Omar Omar, Hatem Abuohashish, Abeer Elembaby, Uta Christine Wölfle, Yasir Siddiqui, and Dalia Kaisarly. 2022. "Matrix Metalloproteinases in Dental and Periodontal Tissues and Their Current Inhibitors: Developmental, Degradational and Pathological Aspects" International Journal of Molecular Sciences 23, no. 16: 8929. https://doi.org/10.3390/ijms23168929








