Progress of Nanomaterials-Based Photothermal Therapy for Oral Squamous Cell Carcinoma
Abstract
:1. Introduction
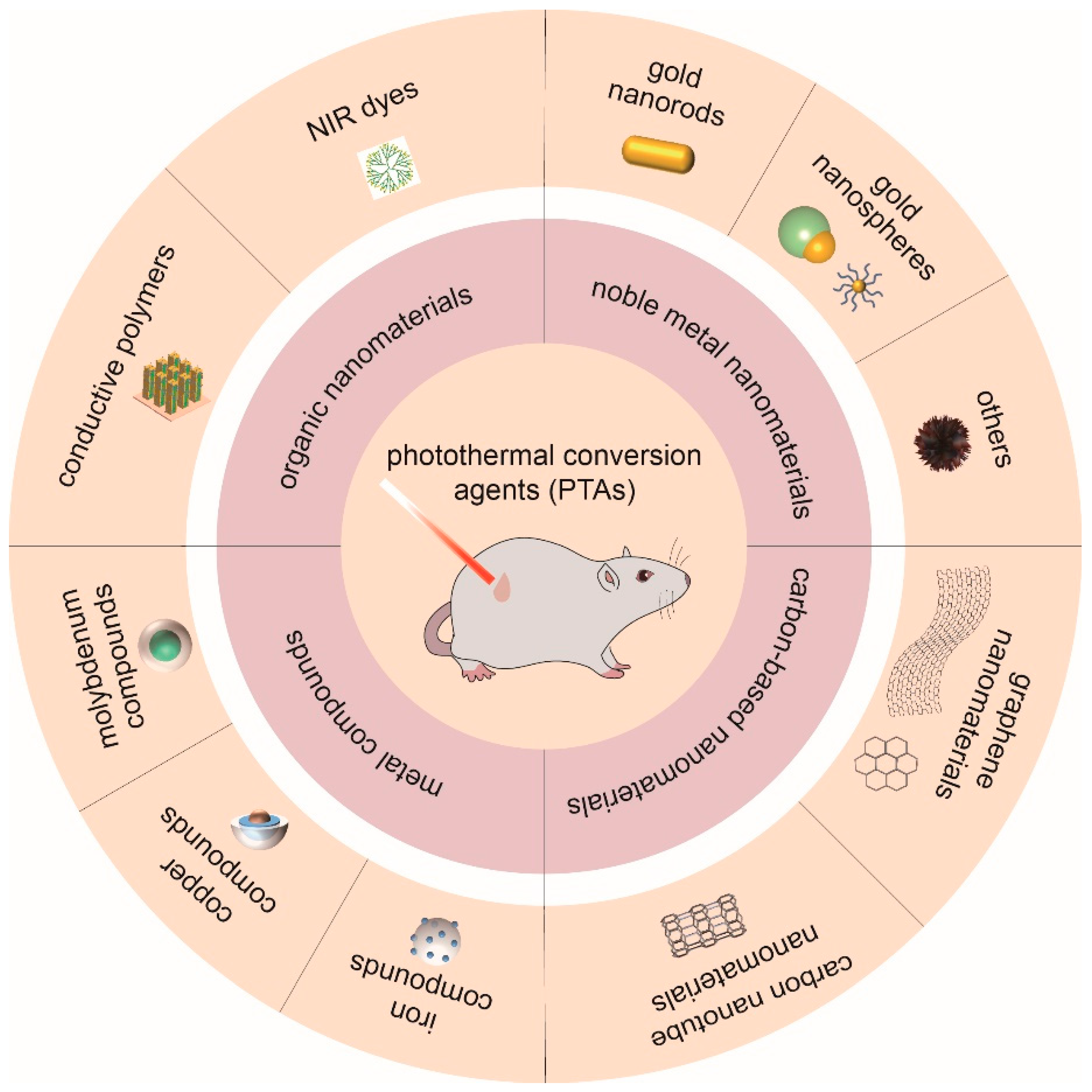
2. Noble Metal Nanomaterials
2.1. Gold Nanorods
2.2. Gold Nanospheres
2.3. Others
3. Carbon-Based Nanomaterials
3.1. Graphene Nanomaterials
3.2. Carbon Nanotubes
4. Metal Compounds
4.1. Iron
4.2. Copper
4.3. Molybdenum
5. Organic Nanoparticles
5.1. NIR Dyes
5.2. Conductive Polymers
6. Drug Delivery System
6.1. In Situ Hydrogels
6.2. Liposomes
6.3. Micelles
7. Conclusions and Outlooks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Butchart, A.; Mikton, C.; Dahlberg, L.L.; Krug, E.G. Global status report on violence prevention 2014. Inj. Prev. 2015, 21, 213. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Gu, M.Q.; Jiang, L.; Hao, L.Y.; Lu, J.Z.; Liu, Z.Q.; Lei, Z.X.; Li, Y.J.; Hua, C.G.; Li, W.; Li, X.Y. A novel theranostic nanoplatform for imaging-guided chemo-photothermal therapy in oral squamous cell carcinoma. J. Mater. Chem. B 2021, 9, 6006–6016. [Google Scholar] [CrossRef]
- Mannelli, G.; Arcuri, F.; Agostini, T.; Innocenti, M.; Raffaini, M.; Spinelli, G. Classification of tongue cancer resection and treatment algorithm. J. Surg. Oncol. 2018, 117, 1092–1099. [Google Scholar] [CrossRef]
- Shah, A.K. Postoperative pathologic assessment of surgical margins in oral cancer: A contemporary review. J. Oral Maxillofac. Pathol. 2018, 22, 78–85. [Google Scholar] [CrossRef]
- Benson, A.B., 3rd; Ajani, J.A.; Catalano, R.B.; Engelking, C.; Kornblau, S.M.; Martenson, J.A., Jr.; McCallum, R.; Mitchell, E.P.; O’Dorisio, T.M.; Vokes, E.E.; et al. Recommended guidelines for the treatment of cancer treatment-induced diarrhea. J. Clin. Oncol. 2004, 22, 2918–2926. [Google Scholar] [CrossRef]
- Jordan, K.; Gralla, R.; Jahn, F.; Molassiotis, A. International antiemetic guidelines on chemotherapy induced nausea and vomiting (CINV): Content and implementation in daily routine practice. Eur. J. Pharmacol. 2014, 722, 197–202. [Google Scholar] [CrossRef]
- Metri, K.; Bhargav, H.; Chowdhury, P.; Koka, P.S. Ayurveda for chemo-radiotherapy induced side effects in cancer patients. J. Stem Cells 2013, 8, 115–129. [Google Scholar] [CrossRef]
- Hare, J.I.; Lammers, T.; Ashford, M.B.; Puri, S.; Storm, G.; Barry, S.T. Challenges and strategies in anti-cancer nanomedicine development: An industry perspective. Adv. Drug Deliv. Rev. 2017, 108, 25–38. [Google Scholar] [CrossRef]
- Rawat, P.S.; Jaiswal, A.; Khurana, A.; Bhatti, J.S.; Navik, U. Doxorubicin-induced cardiotoxicity: An update on the molecular mechanism and novel therapeutic strategies for effective management. Biomed. Pharmacother. 2021, 139, 111708. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhou, C.; He, Q. Radiation therapy’s efficacy on tongue cancer: A population-based survival analysis. OncoTargets Ther. 2018, 11, 7271–7276. [Google Scholar] [CrossRef]
- Song, X.J.; Chen, Q.; Liu, Z. Recent advances in the development of organic photothermal nano-agents. Nano Res. 2015, 8, 340–354. [Google Scholar] [CrossRef]
- Xia, Y.N.; Li, W.Y.; Cobley, C.M.; Chen, J.Y.; Xia, X.H.; Zhang, Q.; Yang, M.X.; Cho, E.C.; Brown, P.K. Gold Nanocages: From Synthesis to Theranostic Applications. Acc. Chem. Res. 2011, 44, 914–924. [Google Scholar] [CrossRef]
- Hornback, N.B. Historical aspects of hyperthermia in cancer therapy. Radiol. Clin. N. Am. 1989, 27, 481–488. [Google Scholar] [CrossRef]
- Toraya-Brown, S.; Fiering, S. Local tumour hyperthermia as immunotherapy for metastatic cancer. Int. J. Hyperth. 2014, 30, 531–539. [Google Scholar] [CrossRef]
- Kong, G.; Braun, R.D.; Dewhirst, M.W. Characterization of the effect of hyperthermia on nanoparticle extravasation from tumor vasculature. Cancer Res. 2001, 61, 3027–3032. [Google Scholar]
- Li, X.S.; Lovell, J.F.; Yoon, J.; Chen, X.Y. Clinical development and potential of photothermal and photodynamic therapies for cancer. Nat. Rev. Clin. Oncol. 2020, 17, 657–674. [Google Scholar] [CrossRef]
- Xia, B.; Wang, B.; Shi, J.S.; Zhang, Y.; Zhang, Q.; Chen, Z.Y.; Li, J.C. Photothermal and biodegradable polyaniline/porous silicon hybrid nanocomposites as drug carriers for combined chemo-photothermal therapy of cancer. Acta Biomater. 2017, 51, 197–208. [Google Scholar] [CrossRef]
- Wei, W.F.; Zhang, X.Y.; Zhang, S.; Wei, G.; Su, Z.Q. Biomedical and bioactive engineered nanomaterials for targeted tumor photothermal therapy: A review. Mater. Sci. Eng. C-Mater. Biol. Appl. 2019, 104, 109891. [Google Scholar] [CrossRef]
- Brace, C. Thermal Tumor Ablation in Clinical Use. IEEE Pulse 2011, 2, 28–38. [Google Scholar] [CrossRef]
- Nikfarjam, M.; Muralidharan, V.; Christophi, C. Mechanisms of focal heat destruction of liver tumors. J. Surg. Res. 2005, 127, 208–223. [Google Scholar] [CrossRef]
- Liu, T.M.; Conde, J.; Lipinski, T.; Bednarkiewicz, A.; Huang, C.C. Smart NIR linear and nonlinear optical nanomaterials for cancer theranostics: Prospects in photomedicine. Prog. Mater. Sci. 2017, 88, 89–135. [Google Scholar] [CrossRef]
- Tomatsu, I.; Peng, K.; Kros, A. Photoresponsive hydrogels for biomedical applications. Adv. Drug Deliv. Rev. 2011, 63, 1257–1266. [Google Scholar] [CrossRef]
- Zou, L.; Wang, H.; He, B.; Zeng, L.; Tan, T.; Cao, H.; He, X.; Zhang, Z.; Guo, S.; Li, Y. Current Approaches of Photothermal Therapy in Treating Cancer Metastasis with Nanotherapeutics. Theranostics 2016, 6, 762–772. [Google Scholar] [CrossRef]
- Lv, Z.Q.; He, S.J.; Wang, Y.F.; Zhu, X.Y. Noble Metal Nanomaterials for NIR-Triggered Photothermal Therapy in Cancer. Adv. Healthc. Mater. 2021, 10, 2001806. [Google Scholar] [CrossRef]
- Niemeyer, C.M. Nanoparticles, Proteins, and Nucleic Acids: Biotechnology Meets Materials Science. Angew. Chem. Int. Ed. Engl. 2001, 40, 4128–4158. [Google Scholar] [CrossRef]
- West, J.L.; Halas, N.J. Engineered nanomaterials for biophotonics applications: Improving sensing, imaging, and therapeutics. Annu. Rev. Biomed. Eng. 2003, 5, 285–292. [Google Scholar] [CrossRef]
- Hobbs, S.K.; Monsky, W.L.; Yuan, F.; Roberts, W.G.; Griffith, L.; Torchilin, V.P.; Jain, R.K. Regulation of transport pathways in tumor vessels: Role of tumor type and microenvironment. Proc. Natl. Acad. Sci. USA 1998, 95, 4607–4612. [Google Scholar] [CrossRef]
- Albanese, A.; Tang, P.S.; Chan, W.C.W. The Effect of Nanoparticle Size, Shape, and Surface Chemistry on Biological Systems. Annu. Rev. Biomed. Eng. 2012, 14, 1–16. [Google Scholar] [CrossRef]
- Liu, S.; Pan, X.; Liu, H. Two-Dimensional Nanomaterials for Photothermal Therapy. Angew. Chem. Int. Ed. Engl. 2020, 59, 5890–5900. [Google Scholar] [CrossRef]
- Willets, K.A.; Van Duyne, R.P. Localized surface plasmon resonance spectroscopy and sensing. Annu. Rev. Phys. Chem. 2007, 58, 267–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, X.M.; Wan, H.Y.; Jia, H.; Liu, L.; Wang, J. Porous Pt Nanoparticles with High Near-Infrared Photothermal Conversion Efficiencies for Photothermal Therapy. Adv. Healthc. Mater. 2016, 5, 3165–3172. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Li, X.; Wang, J.; Zhang, P.; Huang, X.; Zhang, Z.; Guo, D.S.; Yang, X. Ag@S-nitrosothiol core-shell nanoparticles for chemo and photothermal synergistic tumor targeted therapy. J. Mater. Chem. B 2020, 8, 5483–5490. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Chen, M.; Zheng, N. Sub-10-nm Pd nanosheets with renal clearance for efficient near-infrared photothermal cancer therapy. Small 2014, 10, 3139–3144. [Google Scholar] [CrossRef] [PubMed]
- Jia, J.; Liu, G.Y.; Xu, W.J.; Tian, X.L.; Li, S.B.; Han, F.; Feng, Y.H.; Dong, X.C.; Chen, H.Y. Fine-Tuning the Homometallic Interface of Au-on-Au Nanorods and Their Photothermal Therapy in the NIR-II Window. Angew. Chem. Int. Ed. 2020, 59, 14443–14448. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.L.; Shipton, M.K.; Ryan, J.; Kaufman, E.D.; Franzen, S.; Feldheim, D.L. Synthesis, stability, and cellular internalization of gold nanoparticles containing mixed peptide-poly(ethylene glycol) monolayers. Anal. Chem. 2007, 79, 2221–2229. [Google Scholar] [CrossRef]
- Sperling, R.A.; Parak, W.J. Surface modification, functionalization and bioconjugation of colloidal inorganic nanoparticles. Philos. Trans. Royal Soc. A 2010, 368, 1333–1383. [Google Scholar] [CrossRef]
- Klebowski, B.; Depciuch, J.; Parlinska-Wojtan, M.; Baran, J. Applications of Noble Metal-Based Nanoparticles in Medicine. Int. J. Mol. Sci. 2018, 19, 4031. [Google Scholar] [CrossRef]
- Wang, B.K.; Yu, X.F.; Wang, J.H.; Li, Z.B.; Li, P.H.; Wang, H.; Song, L.; Chu, P.K.; Li, C. Gold-nanorods-siRNA nanoplex for improved photothermal therapy by gene silencing. Biomaterials 2016, 78, 27–39. [Google Scholar] [CrossRef]
- Melancon, M.P.; Lu, W.; Zhong, M.; Zhou, M.; Liang, G.; Elliott, A.M.; Hazle, J.D.; Myers, J.N.; Li, C.; Stafford, R.J. Targeted multifunctional gold-based nanoshells for magnetic resonance-guided laser ablation of head and neck cancer. Biomaterials 2011, 32, 7600–7608. [Google Scholar] [CrossRef]
- Lin, M.Y.; Hsieh, H.H.; Chen, J.C.; Chen, C.L.; Sheu, N.C.; Huang, W.S.; Ho, S.Y.; Chen, T.W.; Lee, Y.J.; Wu, C.Y. Brachytherapy Approach Using Lu-177 Conjugated Gold Nanostars and Evaluation of Biodistribution, Tumor Retention, Dosimetry and Therapeutic Efficacy in Head and Neck Tumor Model. Pharmaceutics 2021, 13, 1903. [Google Scholar] [CrossRef]
- Wang, D.; Guo, Z.; Zhou, J.; Chen, J.; Zhao, G.; Chen, R.; He, M.; Liu, Z.; Wang, H.; Chen, Q. Novel Mn3[Co(CN)6]2@SiO2@Ag Core–Shell Nanocube: Enhanced Two-Photon Fluorescence and Magnetic Resonance Dual-Modal Imaging-Guided Photothermal and Chemo-therapy. Small 2015, 11, 5956–5967. [Google Scholar] [CrossRef]
- Huang, Z.; Gao, L.; Kong, L.; Zhang, H.H.; Yang, J.X.; Li, L. In vivo two-photon imaging/excited photothermal therapy strategy of a silver-nanohybrid. J. Mater. Chem. B 2019, 7, 7377–7386. [Google Scholar] [CrossRef]
- Fang, W.J.; Tang, S.H.; Liu, P.X.; Fang, X.L.; Gong, J.W.; Zheng, N.F. Pd Nanosheet-Covered Hollow Mesoporous Silica Nanoparticles as a Platform for the Chemo-Photothermal Treatment of Cancer Cells. Small 2012, 8, 3816–3822. [Google Scholar] [CrossRef]
- Bharathiraja, S.; Bui, N.Q.; Manivasagan, P.; Moorthy, M.S.; Mondal, S.; Seo, H.; Phuoc, N.T.; Phan, T.T.V.; Kim, H.; Lee, K.D.; et al. Multimodal tumor-homing chitosan oligosaccharide-coated biocompatible palladium nanoparticles for photo-based imaging and therapy. Sci. Rep. 2018, 8, 500. [Google Scholar] [CrossRef]
- Ma, Q.X.; Cheng, L.; Gong, F.; Dong, Z.L.; Liang, C.; Wang, M.Y.; Feng, L.Z.; Li, Y.G.; Liu, Z.; Li, C.; et al. Platinum nanoworms for imaging-guided combined cancer therapy in the second near-infrared window. J. Mater. Chem. B 2018, 6, 5069–5079. [Google Scholar] [CrossRef]
- Shrivastava, R.; Dube, A. Effect of the polyelectrolyte coating on the photothermal efficiency of gold nanorods and the photothermal induced cancer cell damage. IET Nanobiotechnol. 2017, 11, 909–916. [Google Scholar] [CrossRef]
- Huang, X.H.; El-Sayed, I.H.; Qian, W.; El-Sayed, M.A. Cancer cell imaging and photothermal therapy in the near-infrared region by using gold nanorods. J. Am. Chem. Soc. 2006, 128, 2115–2120. [Google Scholar] [CrossRef]
- Lee, J.; Chatterjee, D.K.; Lee, M.H.; Krishnan, S. Gold nanoparticles in breast cancer treatment: Promise and potential pitfalls. Cancer Lett. 2014, 347, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Hussein, E.A.; Zagho, M.M.; Nasrallah, G.K.; Elzatahry, A.A. Recent advances in functional nanostructures as cancer photothermal therapy. Int. J. Nanomed. 2018, 13, 2897–2906. [Google Scholar] [CrossRef]
- Liao, Y.T.; Liu, C.H.; Chin, Y.; Chen, S.Y.; Liu, S.H.; Hsu, Y.C.; Wu, K.C.W. Biocompatible and multifunctional gold nanorods for effective photothermal therapy of oral squamous cell carcinoma. J. Mater. Chem. B 2019, 7, 4451–4460. [Google Scholar] [CrossRef]
- Ali, M.R.K.; Wu, Y.; Tang, Y.; Xiao, H.P.; Chen, K.C.; Han, T.G.; Fang, N.; Wu, R.H.; El-Sayed, M.A. Targeting cancer cell integrins using gold nanorods in photothermal therapy inhibits migration through affecting cytoskeletal proteins. Proc. Natl. Acad. Sci. USA 2017, 114, E5655–E5663. [Google Scholar] [CrossRef] [PubMed]
- Webb, J.A.; Bardhan, R. Emerging advances in nanomedicine with engineered gold nanostructures. Nanoscale 2014, 6, 2502–2530. [Google Scholar] [CrossRef]
- Chen, C.W.; Lee, P.H.; Chan, Y.C.; Hsiao, M.; Chen, C.H.; Wu, P.C.; Wu, P.R.; Tsai, D.P.; Tu, D.; Chen, X.; et al. Plasmon-induced hyperthermia: Hybrid upconversion NaYF4:Yb/Er and gold nanomaterials for oral cancer photothermal therapy. J. Mater. Chem. B 2015, 3, 8293–8302. [Google Scholar] [CrossRef]
- Charan, S.; Sanjiv, K.; Singh, N.; Chien, F.C.; Chen, Y.F.; Nergui, N.N.; Huang, S.H.; Kuo, C.W.; Lee, T.C.; Chen, P. Development of chitosan oligosaccharide-modified gold nanorods for in vivo targeted delivery and noninvasive imaging by NIR irradiation. Bioconjug. Chem. 2012, 23, 2173–2182. [Google Scholar] [CrossRef]
- Sun, Q.; Wu, J.; Jin, L.; Hong, L.; Wang, F.; Mao, Z.; Wu, M. Cancer cell membrane-coated gold nanorods for photothermal therapy and radiotherapy on oral squamous cancer. J. Mater. Chem. B 2020, 8, 7253–7263. [Google Scholar] [CrossRef]
- Wang, B.; Wang, J.H.; Liu, Q.; Huang, H.; Chen, M.; Li, K.; Li, C.; Yu, X.F.; Chu, P.K. Rose-bengal-conjugated gold nanorods for in vivo photodynamic and photothermal oral cancer therapies. Biomaterials 2014, 35, 1954–1966. [Google Scholar] [CrossRef]
- Yeo, E.L.L.; Cheah, J.U.J.; Lim, B.Y.; Thong, P.S.P.; Soo, K.C.; Kah, J.C.Y. Protein Corona around Gold Nanorods as a Drug Carrier for Multimodal Cancer Therapy. ACS Biomater. Sci. Eng. 2017, 3, 1039–1050. [Google Scholar] [CrossRef] [PubMed]
- Yeo, E.L.L.; Cheah, J.U.J.; Neo, D.J.H.; Goh, W.I.; Kanchanawong, P.; Soo, K.C.; Thong, P.S.P.; Kah, J.C.Y. Exploiting the protein corona around gold nanorods for low-dose combined photothermal and photodynamic therapy. J. Mater. Chem. B 2017, 5, 254–268. [Google Scholar] [CrossRef] [PubMed]
- Zeng, S.; Liu, S.; Lan, Y.; Qiu, T.; Zhou, M.; Gao, W.; Huang, W.; Ge, L.; Zhang, J. Combined Photothermotherapy and Chemotherapy of Oral Squamous Cell Carcinoma Guided by Multifunctional Nanomaterials Enhanced Photoacoustic Tomography. Int. J. Nanomed. 2021, 16, 7373–7390. [Google Scholar] [CrossRef] [PubMed]
- Melancon, M.P.; Zhou, M.; Zhang, R.; Xiong, C.Y.; Allen, P.; Wen, X.X.; Huang, Q.; Wallace, M.; Myers, J.N.; Stafford, R.J.; et al. Selective Uptake and Imaging of Aptamer- and Antibody-Conjugated Hollow Nanospheres Targeted to Epidermal Growth Factor Receptors Overexpressed in Head and Neck Cancer. ACS Nano 2014, 8, 4530–4538. [Google Scholar] [CrossRef] [PubMed]
- Wenzhi, S.; Dezhou, W.; Ming, R.; Yingzi, L.; Zhenzhen, H.; Chen, W.; Wanzhong, Y.; Qiwei, Y.; Wensheng, Y. Growth Inhibition Effect and Validation of Stable Expressed Reference Genes for Near-Infrared Photothermal Therapy Mediated by Gold Nanoflower Particles on Human Tongue Carcinoma Tca-8113 Cells. J. Biomed. Nanotechnol. 2017, 13, 1158–1167. [Google Scholar] [CrossRef] [PubMed]
- Song, W.Z.; Li, H.; Zhang, Y.; He, D.; Li, Y.Z.; Huang, Z.Z.; Liu, X.; Yin, W.Z. Preparation of Gold Nanoflower-double Layer Silica Core-shell Nanoparticles and Their Photothermal Properties and Metabolism in vivo. Chem. J. Chin. U 2018, 39, 2644–2650. [Google Scholar] [CrossRef]
- Sasidharan, S.; Poojari, R.; Bahadur, D.; Srivastava, R. Embelin-Mediated Green Synthesis of Quasi-Spherical and Star-Shaped Plasmonic Nanostructures for Antibacterial Activity, Photothermal Therapy, and Computed Tomographic Imaging. ACS Sustain. Chem. Eng. 2018, 6, 10562–10577. [Google Scholar] [CrossRef]
- Mapanao, A.K.; Santi, M.; Voliani, V. Combined chemo-photothermal treatment of three-dimensional head and neck squamous cell carcinomas by gold nano-architectures. J. Colloid Interface Sci. 2021, 582, 1003–1011. [Google Scholar] [CrossRef]
- Sasidharan, S.; Bahadur, D.; Srivastava, R. Protein-Poly(amino acid) Nanocore-Shell Mediated Synthesis of Branched Gold Nanostructures for Computed Tomographic Imaging and Photothermal Therapy of Cancer. ACS Appl. Mater. Interfaces 2016, 8, 15889–15903. [Google Scholar] [CrossRef]
- Su, J.; Lu, S.; Jiang, S.; Li, B.; Liu, B.; Sun, Q.; Li, J.; Wang, F.; Wei, Y. Engineered Protein Photo-Thermal Hydrogels for Outstanding In Situ Tongue Cancer Therapy. Adv. Mater. 2021, 33, e2100619. [Google Scholar] [CrossRef]
- Sonnichsen, C.; Franzl, T.; Wilk, T.; von Plessen, G.; Feldmann, J.; Wilson, O.; Mulvaney, P. Drastic reduction of plasmon damping in gold nanorods. Phys. Rev. Lett. 2002, 88, 077402. [Google Scholar] [CrossRef]
- Pan, L.; Liu, J.; Shi, J. Nuclear-Targeting Gold Nanorods for Extremely Low NIR Activated Photothermal Therapy. ACS Appl. Mater. Interfaces 2017, 9, 15952–15961. [Google Scholar] [CrossRef]
- Chauhan, V.P.; Popović, Z.; Chen, O.; Cui, J.; Fukumura, D.; Bawendi, M.G.; Jain, R.K. Fluorescent Nanorods and Nanospheres for Real-Time In Vivo Probing of Nanoparticle Shape-Dependent Tumor Penetration. Angew. Chem. Int. Ed. 2011, 50, 11417–11420. [Google Scholar] [CrossRef]
- Link, S.; El-Sayed, M.A. Spectral properties and relaxation dynamics of surface plasmon electronic oscillations in gold and silver nanodots and nanorods. J. Phys. Chem. B 1999, 103, 8410–8426. [Google Scholar] [CrossRef]
- Fernandes, N.; Rodrigues, C.F.; Moreira, A.F.; Correia, I.J. Overview of the application of inorganic nanomaterials in cancer photothermal therapy. Biomater. Sci. 2020, 8, 2990–3020. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.G.; Xia, Y.N. Gold and silver nanoparticles: A class of chromophores with colors tunable in the range from 400 to 750 nm. Analyst 2003, 128, 686–691. [Google Scholar] [CrossRef]
- Huang, X.; Qian, W.; El-Sayed, I.H.; El-Sayed, M.A. The potential use of the enhanced nonlinear properties of gold nanospheres in photothermal cancer therapy. Lasers Surg. Med. 2007, 39, 747–753. [Google Scholar] [CrossRef]
- Mousavi, S.M.; Zarei, M.; Hashemi, S.A.; Ramakrishna, S.; Chiang, W.H.; Lai, C.W.; Gholami, A. Gold nanostars-diagnosis, bioimaging and biomedical applications. Drug Metab. Rev. 2020, 52, 299–318. [Google Scholar] [CrossRef]
- Ye, S.J.; Wheeler, M.C.; McLaughlan, J.R.; Tamang, A.; Diggle, C.P.; Cespedes, O.; Markham, A.F.; Coletta, P.L.; Evans, S.D. Developing Hollow-Channel Gold Nanoflowers as Trimodal Intracellular Nanoprobes. Int. J. Mol. Sci. 2018, 19, 2327. [Google Scholar] [CrossRef]
- Xie, J.; Zhang, Q.; Lee, J.Y.; Wang, D.I. The synthesis of SERS-active gold nanoflower tags for in vivo applications. ACS Nano 2008, 2, 2473–2480. [Google Scholar] [CrossRef]
- Lagos, K.J.; Buzza, H.H.; Bagnato, V.S.; Romero, M.P. Carbon-Based Materials in Photodynamic and Photothermal Therapies Applied to Tumor Destruction. Int. J. Mol. Sci. 2022, 23, 22. [Google Scholar] [CrossRef]
- Xu, Y.H.; Shan, Y.L.; Cong, H.L.; Shen, Y.Q.; Yu, B. Advanced Carbon-based Nanoplatforms Combining Drug Delivery and Thermal Therapy for Cancer Treatment. Curr. Pharm. Des. 2018, 24, 4060–4076. [Google Scholar] [CrossRef]
- Chen, Y.W.; Su, Y.L.; Hu, S.H.; Chen, S.Y. Functionalized graphene nanocomposites for enhancing photothermal therapy in tumor treatment. Adv. Drug Deliv. Rev. 2016, 105, 190–204. [Google Scholar] [CrossRef]
- Ardakani, T.S.; Meidanchi, A.; Shokri, A.; Shakeri-Zadeh, A. Fe3O4@Au/reduced graphene oxide nanostructures: Combinatorial effects of radiotherapy and photothermal therapy on oral squamous carcinoma KB cell line. Ceram. Int. 2020, 46, 28676–28685. [Google Scholar] [CrossRef]
- Wang, G.H.; Zhang, F.; Tian, R.; Zhang, L.W.; Fu, G.F.; Yang, L.L.; Zhu, L. Nanotubes-Embedded Indocyanine Green-Hyaluronic Acid Nanoparticles for Photoacoustic-Imaging-Guided Phototherapy. ACS Appl. Mater. Interfaces 2016, 8, 5608–5617. [Google Scholar] [CrossRef]
- Gao, S.; Zhang, L.W.; Wang, G.H.; Yang, K.; Chen, M.L.; Tian, R.; Ma, Q.J.; Zhu, L. Hybrid graphene/Au activatable theranostic agent for multimodalities imaging guided enhanced photothermal therapy. Biomaterials 2016, 79, 36–45. [Google Scholar] [CrossRef]
- Das, R.K.; Panda, S.; Bhol, C.S.; Bhutia, S.K.; Mohapatra, S. N-Doped Carbon Quantum Dot (NCQD)-Deposited Carbon Capsules for Synergistic Fluorescence Imaging and Photothermal Therapy of Oral Cancer. Langmuir 2019, 35, 15320–15329. [Google Scholar] [CrossRef]
- Shen, S.; Kong, F.F.; Guo, X.M.; Wu, L.; Shen, H.J.; Xie, M.; Wang, X.S.; Jin, Y.; Ge, Y.R. CMCTS stabilized Fe3O4 particles with extremely low toxicity as highly efficient near-infrared photothermal agents for in vivo tumor ablation. Nanoscale 2013, 5, 8056–8066. [Google Scholar] [CrossRef]
- Bhana, S.; Lin, G.; Wang, L.J.; Starring, H.; Mishra, S.R.; Liu, G.; Huang, X.H. Near-Infrared-Absorbing Gold Nanopopcorns with Iron Oxide Cluster Core for Magnetically Amplified Photothermal and Photodynamic Cancer Therapy. ACS Appl. Mater. Interfaces 2015, 7, 11637–11647. [Google Scholar] [CrossRef] [PubMed]
- Zuo, J.X.; Huo, M.F.; Wang, L.Y.; Li, J.; Chen, Y.; Xiong, P. Photonic hyperthermal and sonodynamic nanotherapy targeting oral squamous cell carcinoma. J. Mater. Chem. B 2020, 8, 9084–9093. [Google Scholar] [CrossRef]
- Huang, X.J.; Deng, G.Y.; Han, Y.; Yang, G.Z.; Zou, R.J.; Zhang, Z.Y.; Sun, S.Y.; Hu, J.Q. Right Cu2-xS@MnS Core-Shell Nanoparticles as a Photo/H2O2-Responsive Platform for Effective Cancer Theranostics. Adv. Sci. 2019, 6, 1901461. [Google Scholar] [CrossRef]
- Maor, I.; Asadi, S.; Korganbayev, S.; Dahis, D.; Shamay, Y.; Schena, E.; Azhari, H.; Saccomandi, P.; Weitz, I.S. Laser-induced thermal response and controlled release of copper oxide nanoparticles from multifunctional polymeric nanocarriers. Sci. Technol. Adv. Mater. 2021, 22, 218–233. [Google Scholar] [CrossRef]
- Qian, M.; Cheng, Z.; Luo, G.; Galluzzi, M.; Shen, Y.; Li, Z.; Yang, H.; Yu, X.F. Molybdenum Diphosphide Nanorods with Laser-Potentiated Peroxidase Catalytic/Mild-Photothermal Therapy of Oral Cancer. Adv. Sci. (Weinh.) 2022, 9, 2101527. [Google Scholar] [CrossRef]
- Chen, J.; Li, Q.; Wang, F.; Yang, M.; Xie, L.; Zeng, X. Biosafety, Nontoxic Nanoparticles for VL-NIR Photothermal Therapy Against Oral Squamous Cell Carcinoma. ACS Omega 2021, 6, 11240–11247. [Google Scholar] [CrossRef]
- Thakare, V.S.; Das, M.; Jain, A.K.; Patil, S.; Jain, S. Carbon nanotubes in cancer theragnosis. Nanomedicine 2010, 5, 1277–1301. [Google Scholar] [CrossRef]
- Nagai, Y.; Nakamura, K.; Ohno, J.; Kawaguchi, M.; Fujigaya, T. Antibody-Conjugated Gel-Coated Single-Walled Carbon Nanotubes as Photothermal Agents. ACS Appl. Bio Mater. 2021, 4, 5049–5056. [Google Scholar] [CrossRef]
- Wu, J.J.; Zhang, S.M.; Mei, X.; Liu, N.; Hu, T.T.; Liang, R.Z.; Yan, D.; Wei, M. Ultrathin Transition Metal Chalcogenide Nanosheets Synthesized via Topotactic Transformation for Effective Cancer Theranostics. ACS Appl. Mater. Interfaces 2020, 12, 48310–48320. [Google Scholar] [CrossRef]
- Wu, M.Z.; He, S.Q.; Hu, X.; Chen, J.Q.; Ha, E.N.; Ai, F.J.; Ji, T.; Hu, J.Q.; Ruan, S.C. A Near-Infrared Light Triggered Composite Nanoplatform for Synergetic Therapy and Multimodal Tumor Imaging. Front. Chem. 2021, 9, 695511. [Google Scholar] [CrossRef]
- Saeed, M.; Ren, W.Z.; Wu, A.G. Therapeutic applications of iron oxide based nanoparticles in cancer: Basic concepts and recent advances. Biomater. Sci. 2018, 6, 708–725. [Google Scholar] [CrossRef]
- Chu, M.; Shao, Y.; Peng, J.; Dai, X.; Li, H.; Wu, Q.; Shi, D. Near-infrared laser light mediated cancer therapy by photothermal effect of Fe3O4 magnetic nanoparticles. Biomaterials 2013, 34, 4078–4088. [Google Scholar] [CrossRef]
- Liu, K.; Liu, K.; Liu, J.C.; Ren, Q.L.; Zhao, Z.; Wu, X.Y.; Li, D.L.; Yuan, F.K.; Ye, K.C.; Li, B. Copper chalcogenide materials as photothermal agents for cancer treatment. Nanoscale 2020, 12, 2902–2913. [Google Scholar] [CrossRef]
- Li, Y.B.; Lu, W.; Huang, Q.A.; Huang, M.A.; Li, C.; Chen, W. Copper sulfide nanoparticles for photothermal ablation of tumor cells. Nanomedecine 2010, 5, 1161–1171. [Google Scholar] [CrossRef]
- Zhou, M.; Tian, M.; Li, C. Copper-Based Nanomaterials for Cancer Imaging and Therapy. Bioconjug. Chem. 2016, 27, 1188–1199. [Google Scholar] [CrossRef]
- Feng, W.; Nie, W.; Cheng, Y.H.; Zhou, X.J.; Chen, L.; Qiu, K.X.; Chen, Z.G.; Zhu, M.F.; He, C.L. In vitro and in vivo toxicity studies of copper sulfide nanoplates for potential photothermal applications. Nanomedicine 2015, 11, 901–912. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Meng, F.; Lu, T.; Wei, L.; Pan, X.; Nong, Z.; Wei, M.; Liao, C.; Li, X. Functionalised molybdenum disulfide nanosheets for co-delivery of doxorubicin and siRNA for combined chemo/gene/photothermal therapy on multidrug-resistant cancer. J. Pharm. Pharmacol. 2021, 73, 1128–1135. [Google Scholar] [CrossRef] [PubMed]
- Gai, S.L.; Yang, G.X.; Yang, P.P.; He, F.; Lin, J.; Jin, D.Y.; Xing, B.G. Recent advances in functional nanomaterials for light-triggered cancer therapy. Nano Today 2018, 19, 146–187. [Google Scholar] [CrossRef]
- Zhang, L.; Jing, D.; Wang, L.; Sun, Y.; Li, J.J.; Hill, B.; Yang, F.; Li, Y.; Lam, K.S. Unique Photochemo-Immuno-Nanoplatform against Orthotopic Xenograft Oral Cancer and Metastatic Syngeneic Breast Cancer. Nano Lett. 2018, 18, 7092–7103. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Hong, W.; Jeon, S.; Choi, Y.; Cho, Y. Electroactive Polypyrrole Nanowire Arrays: Synergistic Effect of Cancer Treatment by On-Demand Drug Release and Photothermal Therapy. Langmuir 2015, 31, 4264–4269. [Google Scholar] [CrossRef]
- Ren, S.S.; Cheng, X.; Chen, M.K.; Liu, C.; Zhao, P.C.; Huang, W.; He, J.; Zhou, Z.Y.; Miao, L.Y. Hypotoxic and Rapidly Metabolic PEG-PCL-C3-ICG Nanoparticles for Fluorescence-Guided Photothermal/Photodynamic Therapy against OSCC. ACS Appl. Mater. Interfaces 2017, 9, 31509–31518. [Google Scholar] [CrossRef]
- Song, W.Z.; Li, Y.Z.; Wang, Y.Q.; Wang, D.Z.; He, D.; Chen, W.; Yin, W.Z.; Yang, W.S. Indocyanine Green-Loaded Gold Nanoflowers@Two Layers of Silica Nanocomposites for Photothermal and Photodynamic Therapy of Oral Carcinoma. J. Biomed. Nanotechnol. 2017, 13, 1115–1123. [Google Scholar] [CrossRef]
- Ren, W.; Qiu, L.H.; Gao, Z.; Li, P.; Zhao, X.; Hu, C.C. Preparation of multifunctional nanoparticles targeting tongue cancer and in vitro study. Hua Xi Kou Qiang Yi Xue Za Zhi 2018, 36, 240–246. [Google Scholar] [CrossRef]
- Xiong, J.; Feng, J.L.; Qiu, L.H.; Gao, Z.; Li, P.; Pang, L.; Zhang, Z.W. SDF-1-loaded PLGA nanoparticles for the targeted photoacoustic imaging and photothermal therapy of metastatic lymph nodes in tongue squamous cell carcinoma. Int. J. Pharm. 2019, 554, 93–104. [Google Scholar] [CrossRef]
- Sun, X.S.; Guo, H.Y.; Fu, Y.H.; Wang, S.; Feng, W.J.; Zheng, Y. Preparation of Multifunctional Nanocomposites and Local Hyperthermia for Oral Squamous Cell Carcinoma. Sci. Adv. Mater. 2021, 13, 829–838. [Google Scholar] [CrossRef]
- Wang, Y.X.; Xie, D.Y.; Pan, J.R.; Xia, C.W.; Fan, L.; Pu, Y.M.; Zhang, Q.; Ni, Y.H.; Wang, J.Q.; Hu, Q.G. A near infrared light-triggered human serum albumin drug delivery system with coordination bonding of indocyanine green and cisplatin for targeting photochemistry therapy against oral squamous cell cancer. Biomater. Sci. 2019, 7, 5270–5282. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.R.; Wang, Y.; Wang, B.B.; Chen, Q.; Wan, G.Y.; Yang, X.Y.; Zhang, J.; Zhang, L.Y.; Li, C.Y.; Wang, Y.S. Homologous -targeting biomimetic nanoparticles for photothermal therapy and Nrf2-siRNA amplified photodynamic therapy against oral tongue squamous cell carcinoma. Chem. Eng. J. 2020, 388, 124268. [Google Scholar] [CrossRef]
- Bu, L.L.; Wang, H.Q.; Pan, Y.W.; Chen, L.; Wu, H.; Wu, X.J.; Zhao, C.C.; Rao, L.; Liu, B.; Sun, Z.J. Gelatinase-sensitive nanoparticles loaded with photosensitizer and STAT3 inhibitor for cancer photothermal therapy and immunotherapy. J. Nanobiotechnology 2021, 19, 379. [Google Scholar] [CrossRef]
- Wu, Y.Z.; Chen, F.M.; Huang, N.W.; Li, J.J.; Wu, C.Z.; Tan, B.W.; Liu, Y.K.; Li, L.J.; Yang, C.; Shao, D.; et al. Near-infrared light-responsive hybrid hydrogels for the synergistic chemo-photothermal therapy of oral cancer. Nanoscale 2021, 13, 17168–17182. [Google Scholar] [CrossRef]
- Muhanna, N.; Jin, C.S.; Huynh, E.; Chan, H.; Qiu, Y.; Jiang, W.L.; Cui, L.Y.; Burgess, L.; Akens, M.K.; Chen, J.; et al. Phototheranostic Porphyrin Nanoparticles Enable Visualization and Targeted Treatment of Head and Neck Cancer in Clinically Relevant Models. Theranostics 2015, 5, 1428–1443. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.T.; Hao, Y.; Li, W.; Xiao, Y.; Zhou, T.L.; Hu, D.R.; Liu, Q.Y.; Zhou, X.L.; Qian, Z.Y. Near-Infrared Responsive Doxorubicin Loaded Hollow Mesoporous Prussian Blue Nanoparticles Combined with Dissolvable Hyaluronic Acid Microneedle System for Human Oral Cell Carcinoma. J. Biomed. Nanotechnol. 2020, 16, 721–738. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.J.; Ruan, C.P.; Shi, R.; Jiang, B.P.; Ji, S.C.; Shen, X.C. A near infrared-modulated thermosensitive hydrogel for stabilization of indocyanine green and combinatorial anticancer phototherapy. Biomater. Sci. 2019, 7, 1705–1715. [Google Scholar] [CrossRef]
- Maarek, J.M.I.; Holschneider, D.P.; Harimoto, J. Fluorescence of indocyanine green in blood: Intensity dependence on concentration and stabilization with sodium polyaspartate. J. Photochem. Photobiol. B Biol. 2001, 65, 157–164. [Google Scholar] [CrossRef]
- Liu, X.; Liu, Y.; Guo, Y.J.; Shi, W.; Sun, Y.A.; He, Z.; Shen, Y.Q.; Zhang, X.M.; Xiao, H.H.; Ge, D.T. Metabolizable pH/H2O2 dual-responsive conductive polymer nanoparticles for safe and precise chemo-photothermal therapy. Biomaterials 2021, 277, 121115. [Google Scholar] [CrossRef]
- Unsoy, G.; Gunduz, U. Smart Drug Delivery Systems in Cancer Therapy. Curr. Drug Targets 2018, 19, 202–212. [Google Scholar] [CrossRef]
- Kumari, P.; Ghosh, B.; Biswas, S. Nanocarriers for cancer-targeted drug delivery. J. Drug Target. 2016, 24, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Gong, X.; Liao, W.; Lv, N.; Yan, R. Molecular targeted treatment and drug delivery system for gastric cancer. J. Cancer Res. Clin. Oncol. 2021, 147, 973–986. [Google Scholar] [CrossRef] [PubMed]
- Tila, D.; Ghasemi, S.; Yazdani-Arazi, S.N.; Ghanbarzadeh, S. Functional liposomes in the cancer-targeted drug delivery. J. Biomater. Appl. 2015, 30, 3–16. [Google Scholar] [CrossRef]
- Tan, B.; Huang, L.; Wu, Y.; Liao, J. Advances and trends of hydrogel therapy platform in localized tumor treatment: A review. J. Biomed. Mater. Res. A 2021, 109, 404–425. [Google Scholar] [CrossRef]
- Wei, W.; Li, H.; Yin, C.; Tang, F. Research progress in the application of in situ hydrogel system in tumor treatment. Drug Deliv. 2020, 27, 460–468. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Song, C.; Wang, C.; Hu, Y.; Wu, J. Hydrogel-Based Controlled Drug Delivery for Cancer Treatment: A Review. Mol. Pharm. 2020, 17, 373–391. [Google Scholar] [CrossRef]
- Chen, M.; Wang, Z.; Suo, W.; Bao, Z.; Quan, H. Injectable Hydrogel for Synergetic Low Dose Radiotherapy, Chemodynamic Therapy and Photothermal Therapy. Front. Bioeng. Biotechnol. 2021, 9, 757428. [Google Scholar] [CrossRef]
- Dimatteo, R.; Darling, N.J.; Segura, T. In situ forming injectable hydrogels for drug delivery and wound repair. Adv. Drug Deliv. Rev. 2018, 127, 167–184. [Google Scholar] [CrossRef]
- Norouzi, M.; Nazari, B.; Miller, D.W. Injectable hydrogel-based drug delivery systems for local cancer therapy. Drug Discov. Today 2016, 21, 1835–1849. [Google Scholar] [CrossRef]
- Allen, T.M.; Cullis, P.R. Liposomal drug delivery systems: From concept to clinical applications. Adv. Drug Deliv. Rev. 2013, 65, 36–48. [Google Scholar] [CrossRef]
- Forouhari, S.; Beygi, Z.; Mansoori, Z.; Hajsharifi, S.; Heshmatnia, F.; Gheibihayat, S.M. Liposomes: Ideal drug delivery systems in breast cancer. Biotechnol. Appl. Biochem. 2021; Online ahead of print. [Google Scholar] [CrossRef]
- Chaurasiya, A.; Gorajiya, A.; Panchal, K.; Katke, S.; Singh, A.K. A review on multivesicular liposomes for pharmaceutical applications: Preparation, characterization, and translational challenges. Drug Deliv. Transl. Res. 2022, 12, 1569–1587. [Google Scholar] [CrossRef]
- Anilkumar, T.S.; Lu, Y.J.; Chen, J.P. Optimization of the Preparation of Magnetic Liposomes for the Combined Use of Magnetic Hyperthermia and Photothermia in Dual Magneto-Photothermal Cancer Therapy. Int. J. Mol. Sci. 2020, 21, 5187. [Google Scholar] [CrossRef]
- Xu, L.; Zhang, W.; Park, H.B.; Kwak, M.; Oh, J.; Lee, P.C.W.; Jin, J.O. Indocyanine green and poly I:C containing thermo-responsive liposomes used in immune-photothermal therapy prevent cancer growth and metastasis. J. Immunother. Cancer 2019, 7, 220. [Google Scholar] [CrossRef] [PubMed]
- Gong, J.; Chen, M.; Zheng, Y.; Wang, S.; Wang, Y. Polymeric micelles drug delivery system in oncology. J. Control Release 2012, 159, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Keskin, D.; Tezcaner, A. Micelles as Delivery System for Cancer Treatment. Curr. Pharm. Des. 2017, 23, 5230–5241. [Google Scholar] [CrossRef]
- Bose, A.; Burman, D.R.; Sikdar, B.; Patra, P. Nanomicelles: Types, properties and applications in drug delivery. IET Nanobiotechnol. 2021, 15, 19–27. [Google Scholar] [CrossRef]
- Ji, Y.; Sun, Y.; Hei, M.; Cheng, D.; Wang, B.; Tang, Y.; Fu, Y.; Zhu, W.; Xu, Y.; Qian, X. NIR Activated Upper Critical Solution Temperature Polymeric Micelles for Trimodal Combinational Cancer Therapy. Biomacromolecules 2022, 23, 937–947. [Google Scholar] [CrossRef]
- Huang, X.; Li, Y.; Li, D.; Zhou, X.; Qiao, H.; Yang, L.; Ji, Y.; Zhang, X.; Huang, D.; Chen, W. Black phosphorus assisted polyionic micelles with efficient PTX loading for remotely controlled release and synergistic treatment of drug-resistant tumors. Biomater. Sci. 2021, 9, 6108–6115. [Google Scholar] [CrossRef]
- Zhang, Y.G.; Zhang, S.Y.; Zhang, Z.H.; Ji, L.L.; Zhang, J.M.; Wang, Q.H.; Guo, T.; Ni, S.M.; Cai, R.; Mu, X.Y.; et al. Recent Progress on NIR-II Photothermal Therapy. Front. Chem. 2021, 9, 728066. [Google Scholar] [CrossRef]





| Classification | Photothermal Nanomaterial | Exposure Conditions | Tumor Type | Therapy Model | Ref. |
|---|---|---|---|---|---|
| Gold nanorods | UCP@SiO2-NR-FA | 980 nm | OECM-1 cells | PTT | [54] |
| GNRs-siRNA | 810 nm | Cal-27 cells | PTT | [39] | |
| PDDAC-GNRs | 780 nm | NT8e cells | PTT | [47] | |
| EGFR antibody Conjugated gold nanoparticles | 514 nm | HSC 313, HOC 3 Clone 8 and HaCaT cells | PTT | [48] | |
| CO-GNRs | 780 nm | Cal-27 cells | PTT | [55] | |
| GNR@Mem | X-rays, 4 Gy; 980 nm | KB cells | PTT; RT | [56] | |
| RB-GNRs | PTT: 810 nm; PDT: 532 nm | Cal-27 cells | PTT; PDT | [57] | |
| NR-HS-Ce6-DOX | 665 nm | Cal-27 cells | PTT; PDT; chemotherapy | [58,59] | |
| DOX-AuNRs@mSiO2-HA | 808 nm | Cal-27 cells | PTT; chemotherapy | [60] | |
| Gold nanospheres | Apt-HAuNS | - | OSC-19 cells | PTT | [61] |
| C225-SPIO@Au NS | 808 nm | A431, FaDu, OSC-19 and HN5 cells | PTT | [40] | |
| Others | gold nanoflower | TCA-8113 cells | PTT | [62] | |
| AuNF@SiO2@mSiO2 | 808 nm | Cal-27 cells | PTT | [63] | |
| 177Lu-DTPA-pAuNS | 793 nm | SAS-3R cells | Brachytherapy; PTT | [41] | |
| E-GNS | 808 nm | KB cells; | PTT | [64] | |
| tNAs-cisPt | 808 nm | SCC-25 cells; UPCI:SCC-154 cells | PTT; chemotherapy | [65] | |
| Branched gold nanostructures | 808 nm | KB cells | PTT | [66] | |
| E72-Chitosan-Ag3AuS2 | 808 nm | Cal-27 cells | PTT | [67] |
| Classification | Photothermal Nanomaterial | Exposure Conditions | Tumor Type | Therapy Model | Ref. | |
|---|---|---|---|---|---|---|
| Carbon-based nanomaterials | Graphene nanomaterials | Fe3O4@Au/rGO NSs | X-rays, 2 and 4 Gy; 808 nm | KB cells | RT; PTT | [81] |
| CPGA | 808 nm | SCC7 cells | PTT | [83] | ||
| Carbon nanotubes | ICG-HANP/SWCNT | 808 nm | SCC7 cells | PTT; PDT | [82] | |
| Others | NCOD-HCS | 980 nm | FaDu and HaCaT cells | PTT | [84] | |
| Metal compounds | Iron | Fe3O4@CMCTS | 808 nm | KB cells, MCF-7 and S180 cells | PTT | [85] |
| MUA-PEG/SiNC/IOC-Au NCPs | NIR light | KB-3-1 and SK-BR-3 cells | PTT; PDT | [86] | ||
| Copper | Cu2−xS-RB@DMSN-AE105 | laser: 1064 nm; US: 1.0 MHz | OCS-19 | PTT; SDT | [87] | |
| Cu2−xS@MnS | 808 nm | HeLa cells and HNSCC patient derived xenograft models | PTT; PDT | [88] | ||
| CuO-NPs@L-PLGA/PDA/PEG | 808 nm | Cal-33 cells | PTT | [89] | ||
| Molybdenum | MoP2 NRs | 808 nm | Cal-27, HOK and SCC9 cells | PTT; Chemodynamic therapy | [90] | |
| Cys-MoO3−x NPs | 808 nm | OSCC cells | PTT | [91] | ||
| Classification | Photothermal Nanomaterial | Exposure Conditions | Tumor Type | Therapy Model | Ref. |
|---|---|---|---|---|---|
| NIR dyes | PEG-PCL-C3-ICG NPs | 808 nm | HSC cells | PTT; PDT | [106] |
| AuNFs@SiO2@mSiO2-ICG | - | Cal-27 | PTT; PDT | [107] | |
| DOC-SINPs | 808 nm | SCC-15 | PTT; chemotherapy | [108] | |
| CPCI/DOX-NP | 808 nm | OSC-3 | PTT; chemotherapy | [104] | |
| SDF-1/ICG/PFH/DOX/PLGA NPs | 808 nm | SCC-15 | PTT; chemotherapy | [109] | |
| SDF-a/ICG/PNE/ADRPLGA NPs | - | SCC-15 | PTT; chemotherapy | [110] | |
| HSA-ICG-DDP NPs | 808 nm | HSC and CAF cells | PTT; PDT; chemotherapy | [111] | |
| M@PPI-siRNA | 808 nm | SCC-25 | PTT; PDT | [112] | |
| Gel-N-ICG | 808 nm | Cal-27 and HIOEC cells | PTT; immunotherapy | [113] | |
| IR820-loaded gel-MSNs | 808 nm | Cal-27 | PTT; chemotherapy | [114] | |
| Porphysomes | 808 nm | buccal cancer model | PTT | [115] | |
| Conductive polymers | DOX/Ppy NW | 810 nm | KB cells and MCF7 cells | PTT; chemotherapy | [105] |
| HATb–PDA–DOX | 808 nm | Cal-27, HSC-3 and HGF cells | PTT; chemotherapy | [3] | |
| HMPBs&DOX@HAMNs | - | OSCC cells | PTT; chemotherapy | [116] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niu, Q.; Sun, Q.; Bai, R.; Zhang, Y.; Zhuang, Z.; Zhang, X.; Xin, T.; Chen, S.; Han, B. Progress of Nanomaterials-Based Photothermal Therapy for Oral Squamous Cell Carcinoma. Int. J. Mol. Sci. 2022, 23, 10428. https://doi.org/10.3390/ijms231810428
Niu Q, Sun Q, Bai R, Zhang Y, Zhuang Z, Zhang X, Xin T, Chen S, Han B. Progress of Nanomaterials-Based Photothermal Therapy for Oral Squamous Cell Carcinoma. International Journal of Molecular Sciences. 2022; 23(18):10428. https://doi.org/10.3390/ijms231810428
Chicago/Turabian StyleNiu, Qin, Qiannan Sun, Rushui Bai, Yunfan Zhang, Zimeng Zhuang, Xin Zhang, Tianyi Xin, Si Chen, and Bing Han. 2022. "Progress of Nanomaterials-Based Photothermal Therapy for Oral Squamous Cell Carcinoma" International Journal of Molecular Sciences 23, no. 18: 10428. https://doi.org/10.3390/ijms231810428
APA StyleNiu, Q., Sun, Q., Bai, R., Zhang, Y., Zhuang, Z., Zhang, X., Xin, T., Chen, S., & Han, B. (2022). Progress of Nanomaterials-Based Photothermal Therapy for Oral Squamous Cell Carcinoma. International Journal of Molecular Sciences, 23(18), 10428. https://doi.org/10.3390/ijms231810428






