Serum Immunoglobulin G Is a Marker of Hidradenitis Suppurativa Disease Severity
Abstract
:1. Introduction
2. Results
2.1. Population Characteristics
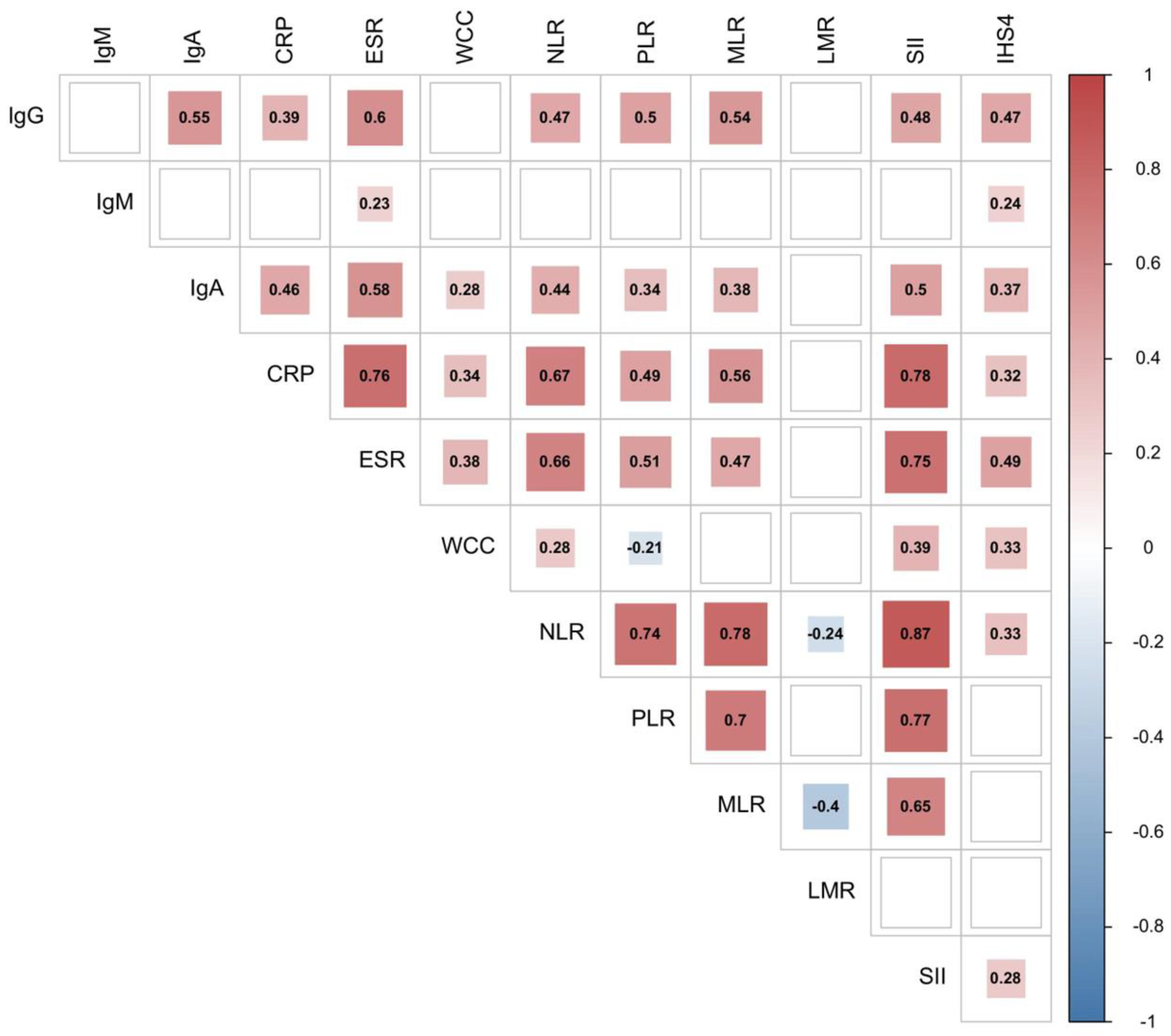
2.2. Serum Inflammatory Markers Correlate with IHS4 Disease Severity
2.3. Serum Immunoglobulin Levels Differ across HS Disease Severity
2.4. Serum IgG Level Identifies Patients with Severe HS
3. Discussion
4. Materials and Methods
4.1. Study Cohort
- Patients diagnosed with or suspected to have an active solid organ or haematological malignancy or terminal illness;
- Pregnancy;
- Patients found to have a monoclonal gammopathy;
- Patients diagnosed or suspected to have other active, systemic infective or inflammatory processes;
- Patients diagnosed or suspected to have a primary immunodeficiency disorder;
- Patients with suspected or confirmed seropositive coagulopathy;
- Patients treated with a systemic antibiotic, non-biologic immunomodulatory/immunosuppressant therapy and/or intralesional and/or oral corticosteroid in the last six weeks;
- Patients who underwent surgical intervention in the last three months;
- Patients who were unable to provide their own voluntary informed consent;
- Patients who could not attend timely follow-up appointments.
4.2. HS Severity Staging
- Stage I (mild): single or multiple nodules or abscesses in a typical site without the presence of sinus tracts;
- Stage II (moderate): single or multiple, recurrent, widely separated nodules and/or abscesses and tunnels with scarring;
- Stage III (severe): diffuse nodules, abscesses and draining tunnels involving the majority of an affected area.
- Mild HS: for scores ≤ 3;
- Moderate HS: for scores ranging from 4 to 10;
- Severe HS: for scores ≥ 11.
4.3. Assessment of Serum Immunoglobulin Levels
4.4. Calculation of Inflammatory Parameters
- Neutrophil–lymphocyte ratio (NLR) (neutrophil count divided by lymphocyte count);
- Platelet–lymphocyte ratio (PLR) (platelet count divided by lymphocyte count);
- Monocyte-lymphocyte ratio (MLR) (monocyte count divided by lymphocyte count);
- Lymphocyte–monocyte ratio (LMR) (lymphocyte count divided by monocyte count);
- Systemic immune-inflammation index (SII) (platelet x neutrophil/lymphocyte count [47]).
4.5. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jfri, A.; Nassim, D.; O’Brien, E.; Gulliver, W.; Nikolakis, G.; Zouboulis, C.C. Prevalence of Hidradenitis Suppurativa: A Systematic Review and Meta-regression Analysis. JAMA Dermatol. 2021, 157, 924. [Google Scholar] [CrossRef] [PubMed]
- Pace, N.P.; Mintoff, D.; Borg, I. The Genomic Architecture of Hidradenitis Suppurativa—A Systematic Review. Front. Genet. 2022, 13, 861241. [Google Scholar] [CrossRef] [PubMed]
- Vossen, A.R.J.V.; Van Der Zee, H.H.; Prens, E.P. Hidradenitis Suppurativa: A Systematic Review Integrating Inflammatory Pathways Into a Cohesive Pathogenic Model. Front. Immunol. 2018, 9, 2965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zouboulis, C.C.; Benhadou, F.; Byrd, A.S.; Chandran, N.S.; Giamarellos-Bourboulis, E.J.; Fabbrocini, G.; Frew, J.W.; Fujita, H.; González-López, M.A.; Guillem, P.; et al. What causes hidradenitis suppurativa?—15 years after. Exp. Dermatol. 2020, 29, 1154–1170. [Google Scholar] [CrossRef]
- Mintoff, D.; Pace, N.P.; Borg, I. Interpreting the spectrum of gamma-secretase complex missense variation in the context of hidradenitis suppurativa—An in-silico study. Front. Genet. 2022, 13, 962449. [Google Scholar] [CrossRef]
- König, A.; Lehmann, C.; Rompel, R.; Happle, R. Cigarette smoking as a triggering factor of hidradenitis suppurativa. Dermatology 1999, 198, 261–264. [Google Scholar] [CrossRef]
- Kromann, C.; Ibler, K.; Kristiansen, V.; Jemec, G. The Influence of Body Weight on the Prevalence and Severity of Hidradenitis Suppurativa. Acta Derm. Venereol. 2014, 94, 553–557. [Google Scholar] [CrossRef]
- Zouboulis, C.C.; del Marmol, V.; Mrowietz, U.; Prens, E.P.; Tzellos, T.; Jemec, G.B. Hidradenitis Suppurativa/Acne Inversa: Criteria for Diagnosis, Severity Assessment, Classification and Disease Evaluation. Dermatology 2015, 231, 184–190. [Google Scholar] [CrossRef]
- Chernyshov, P.; Finlay, A.; Tomas-Aragones, L.; Poot, F.; Sampogna, F.; Marron, S.; Zemskov, S.; Abeni, D.; Tzellos, T.; Szepietowski, J.; et al. Quality of Life in Hidradenitis Suppurativa: An Update. Int. J. Environ. Res. Public Health 2021, 18, 6131. [Google Scholar] [CrossRef]
- Der Sarkissian, S.; Hessam, S.; Kirby, J.S.; Lowes, M.A.; Mintoff, D.; Naik, H.B.; Ring, H.C.; Chandran, N.S.; Frew, J.W. Identification of Biomarkers and Critical Evaluation of Biomarker Validation in Hidradenitis Suppurativa. JAMA Dermatol. 2022, 158, 300–313. [Google Scholar] [CrossRef]
- Saunte, D.M.; Boer, J.; Stratigos, A.; Szepietowski, J.; Hamzavi, I.; Kim, K.; Zarchi, K.; Antoniou, C.; Matusiak, L.; Lim, H.; et al. Diagnostic delay in hidradenitis suppurativa is a global problem. Br. J. Dermatol. 2015, 173, 1546–1549. [Google Scholar] [CrossRef] [PubMed]
- Zouboulis, C.C.; Tzellos, T.; Kyrgidis, A.; Jemec, G.B.E.; Bechara, F.G.; Giamarellos-Bourboulis, E.J.; Ingram, J.R.; Kanni, T.; Karagiannidis, I.; Martorell, A.; et al. Development and validation of the International Hidradenitis Suppurativa Severity Score System (IHS 4), a novel dynamic scoring system to assess HS severity. Br. J. Dermatol. 2017, 177, 1401–1409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hurley, H. Axillary hyperhidrosis, apocrine bromhidrosis, hidradenitis suppurativa, and familial benign pemphigus: Surgical approach. Dermatol. Surg. Princ. Pract. 1989, 729, 39. [Google Scholar]
- Zouboulis, C.; Jemec, G.B.E.; Szepietowski, J.; Álvarez-Chinchilla, P.; Asoskova, A.; Bonnekoh, H.; Brattoli, G.; Cetinarslan, T.; Dawicka, J.; Dente, V.; et al. Inter-rater and intrarater agreement and reliability in clinical staging of hidradenitis suppurativa/acne inversa. Br. J. Dermatol. 2019, 181, 852–854. [Google Scholar] [CrossRef] [PubMed]
- Thorlacius, L.; Garg, A.; Riis, P.; Nielsen, S.M.; Bettoli, V.; Ingram, J.; Del Marmol, V.; Matusiak, L.; Pascual, J.; Revuz, J.; et al. Inter-rater agreement and reliability of outcome measurement instruments and staging systems used in hidradenitis suppurativa. Br. J. Dermatol. 2019, 181, 483–491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azarsiz, E.; Ertam, I.; Karaca, N.; Aksu, G.; Alper, S.; Kutukculer, N. IgG-anti-IgA antibodies: An autoimmune finding in patients with psoriasis vulgaris. Minerva Med. 2012, 103, 183–187. [Google Scholar] [PubMed]
- A Howell, F.; A Chamberlain, M.; A Perry, R.; Torrigiani, G.; Roitt, I.M. IgG antiglobulin levels in patients with psoriatic arthropathy, ankylosing spondylitis, and gout. Ann. Rheum. Dis. 1972, 31, 129–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varelzidis, A.; Wilson, A.B.; Meara, R.H.; Turk, J.L. Immunoglobulin levels in atopic eczema. Br. Med. J. 1966, 2, 925–927. [Google Scholar] [CrossRef] [Green Version]
- Ercan, H.; Ispir, T.; Kirac, D.; Baris, S.; Ozen, A.; Oztezcan, S.; Cengizlier, M. Predictors of atopic dermatitis phenotypes and severity: Roles of serum immunoglobulins and filaggrin gene mutation R501X. Allergol. Immunopathol. 2013, 41, 86–93. [Google Scholar] [CrossRef]
- Andriano, T.M.; Benesh, G.; Babbush, K.M.; Hosgood, H.D.; Lin, J.; Cohen, S.R. Serum inflammatory markers and leukocyte profiles accurately describe hidradenitis suppurativa disease severity. Int. J. Dermatol. 2022, 61, 1270–1275. [Google Scholar] [CrossRef]
- Ballova, A.; Vorcakova, K.; Pec, J. Correlation of Increased Total Serum Immunoglobulin E Levels and Hidradenitis Suppurativa. Acta Med. Martiniana 2021, 21, 9–12. [Google Scholar] [CrossRef]
- Kanni, T.; Tzanetakou, V.; Savva, A.; Kersten, B.; Pistiki, A.; van de Veerdonk, F.L.; Netea, M.G.; van der Meer, J.W.; Giamarellos-Bourboulis, E.J. Compartmentalized Cytokine Responses in Hidradenitis Suppurativa. PLoS ONE 2015, 10, e0130522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffman, L.K.; Tomalin, L.E.; Schultz, G.; Howell, M.D.; Anandasabapathy, N.; Alavi, A.; Suárez-Fariñas, M.; Lowes, M.A. Integrating the skin and blood transcriptomes and serum proteome in hidradenitis suppurativa reveals complement dysregulation and a plasma cell signature. PLoS ONE 2018, 13, e0203672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gudjonsson, J.E.; Tsoi, L.C.; Ma, F.; Billi, A.C.; van Straalen, K.; Vossen, A.; Van Der Zee, H.; Harms, P.W.; Wasikowski, R.; Yee, C.M.; et al. Contribution of plasma cells and B cells to hidradenitis suppurativa pathogenesis. JCI Insight 2020, 5, e139930. [Google Scholar] [CrossRef] [PubMed]
- Mintoff, D.; Camilleri, L.; Aquilina, S.; Boffa, M.J.; Clark, E.; Scerri, L. Prevalence of hidradenitis suppurativa in Malta: Comparison with established epidemiological data. Clin. Exp. Dermatol. 2020, 45, 758–759. [Google Scholar] [CrossRef]
- Lowe, M.M.; Naik, H.B.; Clancy, S.; Pauli, M.; Smith, K.M.; Bi, Y.; Dunstan, R.; Gudjonsson, J.; Paul, M.; Harris, H.; et al. Immunopathogenesis of hidradenitis suppurativa and response to anti–TNF-α therapy. JCI Insight 2020, 5, e139932. [Google Scholar] [CrossRef]
- Altman, S.R.; Criswell, S.L. Dynamic Leukocyte Populations Are Associated With Early- and Late-stage Lesions in Hidradenitis Suppurativa. J. Histochem. Cytochem. 2020, 69, 191–201. [Google Scholar] [CrossRef]
- Swamy, M.; Jamora, C.; Havran, W.; Hayday, A. Epithelial decision makers: In search of the ‘epimmunome’. Nat. Immunol. 2010, 11, 656–665. [Google Scholar] [CrossRef] [Green Version]
- Hintner, H.; Lawley, T.J. Keratin Intermediate Filaments Bear Antigenic Determinants for Stratum Corneum Antibodies. J. Investig. Dermatol. 1984, 82, 491–495. [Google Scholar] [CrossRef] [Green Version]
- Hotz, C.; Boniotto, M.; Guguin, A.; Surenaud, M.; Jean-Louis, F.; Tisserand, P.; Ortonne, N.; Hersant, B.; Bosc, R.; Poli, F.; et al. Intrinsic Defect in Keratinocyte Function Leads to Inflammation in Hidradenitis Suppurativa. J. Investig. Dermatol. 2016, 136, 1768–1780. [Google Scholar] [CrossRef] [Green Version]
- Bodkin, A.J.; Criswell, S.L. Hidradenitis suppurativa lesions are associated with decreased collagen, decreased elastin, and increased neovascularization. J. Histotechnol. 2021, 44, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Thélu, J.; Rossio, P.; Favier, B. Notch signalling is linked to epidermal cell differentiation level in basal cell carcinoma, psoriasis and wound healing. BMC Dermatol. 2002, 2, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kashyap, M.P.; Khan, J.; Sinha, R.; Jin, L.; Atigadda, V.; Deshane, J.S.; Ahmed, A.R.; Kilic, A.; Raman, C.; Mukhtar, M.S.; et al. Advances in molecular pathogenesis of hidradenitis suppurativa: Dysregulated keratins and ECM signaling. Semin. Cell Dev. Biol. 2022, 128, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Ghias, M.H.; Hyde, M.J.; Tomalin, L.E.; Morgan, B.P.; Alavi, A.; Lowes, M.A.; Piguet, V. Role of the Complement Pathway in Inflammatory Skin Diseases: A Focus on Hidradenitis Suppurativa. J. Investig. Dermatol. 2020, 140, 531–536.e1. [Google Scholar] [CrossRef] [PubMed]
- Diebolder, C.A.; Beurskens, F.J.; de Jong, R.N.; Koning, R.I.; Strumane, K.; Lindorfer, M.A.; Voorhorst, M.; Ugurlar, D.; Rosati, S.; Heck, A.J.R.; et al. Complement Is Activated by IgG Hexamers Assembled at the Cell Surface. Science 2014, 343, 1260–1263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mariottoni, P.; Jiang, S.W.; Prestwood, C.A.; Jain, V.; Suwanpradid, J.; Whitley, M.J.; Coates, M.; Brown, D.A.; Erdmann, D.; Corcoran, D.L.; et al. Single-Cell RNA Sequencing Reveals Cellular and Transcriptional Changes Associated With M1 Macrophage Polarization in Hidradenitis Suppurativa. Front. Med. 2021, 8, 665873. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Quintela, A.; Alende, R.; Gude, F.; Campos-Franco, J.; Rey, J.; Meijide, L.M.; Fernandez-Merino, C.; Vidal, C. Serum levels of immunoglobulins (IgG, IgA, IgM) in a general adult population and their relationship with alcohol consumption, smoking and common metabolic abnormalities. Clin. Exp. Immunol. 2008, 151, 42–50. [Google Scholar] [CrossRef]
- Mintoff, D.; Benhadou, F.; Pace, N.P.; Frew, J.W. Metabolic syndrome and hidradenitis suppurativa: Epidemiological, molecular, and therapeutic aspects. Int. J. Dermatol. 2021, 61, 1175–1186. [Google Scholar] [CrossRef]
- Macchiarella, G.; Cornacchione, V.; Cojean, C.; Riker, J.; Wang, Y.; Te, H.; Ceci, M.; Gudjonsson, J.E.; Gaulis, S.; Goetschy, J.F.; et al. Disease association of anti-CEL autoantibodies in hidradenitis suppurativa. J. Investig. Dermatol. 2022. [Google Scholar] [CrossRef]
- Assan, F.; Gottlieb, J.; Tubach, F.; Lebbah, S.; Guigue, N.; Hickman, G.; Pape, E.; Madrange, M.; Delaporte, E.; Sendid, B.; et al. Anti-Saccharomyces cerevisiae IgG and IgA antibodies are associated with systemic inflammation and advanced disease in hidradenitis suppurativa. J. Allergy Clin. Immunol. 2020, 146, 452–455.e5. [Google Scholar] [CrossRef] [Green Version]
- van Straalen, K.R. Anti–Saccharomyces cerevisiae antibodies could reflect distinct phenotypes in hidradenitis suppurativa. J. Allergy Clin. Immunol. 2020, 146, 461. [Google Scholar] [CrossRef] [PubMed]
- Gambichler, T.; Hessam, S.; Cramer, P.; Abu Rached, N.; Bechara, F. Complete blood collection-based systemic inflammation biomarkers for patients with hidradenitis suppurativa. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 1593–1596. [Google Scholar] [CrossRef] [PubMed]
- Kearney, N.; McCourt, C.; Hughes, R.; Alsharqi, A.; O’Kane, D.; Kirby, B. Systemic immune inflammation index is a marker of cardiovascular risk and not just disease severity in hidradenitis suppurativa. J. Eur. Acad. Dermatol. Venereol. 2022, 36, e928–e929. [Google Scholar] [CrossRef] [PubMed]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- Dati, F.; Schumann, G.; Thomas, L.; Aguzzi, F.; Baudner, S.; Bienvenu, J.; Blaabjerg, O.; Blirup-Jensen, S.; Carlström, A.; Hyltoft-Petersen, P. Consensus of a group of professional societies and diagnostic companies on guidelines for interim reference ranges for 14 proteins in serum based on the standardization against the IFCC/BCR/CAP Reference Material (CRM 470). International Federation of Clinical Chemistry. Community Bureau of Reference of the Commission of the European Communities. College of American Pathologists. Eur. J. Clin. Chem. Clin. Biochem. 1996, 34, 517–520. [Google Scholar]
- Velthuis, H.T.; Knop, I.; Stam, P.; Broek, M.V.D.; Bos, H.K.; Hol, S.; Teunissen, E.; Fischedick, K.S.; Althaus, H.; Schmidt, B.; et al. N Latex FLC—New monoclonal high-performance assays for the determination of free light chain kappa and lambda. Clin. Chem. Lab. Med. 2011, 49, 1323–1332. [Google Scholar] [CrossRef]
- Hu, B.; Yang, X.-R.; Xu, Y.; Sun, Y.-F.; Sun, C.; Guo, W.; Zhang, X.; Wang, W.-M.; Qiu, S.-J.; Zhou, J.; et al. Systemic Immune-Inflammation Index Predicts Prognosis of Patients after Curative Resection for Hepatocellular Carcinoma. Clin. Cancer Res. 2014, 20, 6212–6222. [Google Scholar] [CrossRef] [Green Version]
- Goksuluk, D.; Korkmaz, S.; Zararsiz, G.; Karaagaoglu, E.A. easyROC: An Interactive Web-tool for ROC Curve Analysis Using R Language Environment. R J. 2016, 8, 213–230. [Google Scholar] [CrossRef] [Green Version]
- López-Ratón, M.; Rodríguez-Álvarez, M.X.; Cadarso Suárez, C.M.; Gude Sampedro, F. OptimalCutpoints: An R Package for Selecting Optimal Cutpoints in Diagnostic Tests. J. Stat. Softw. 2014, 61, 1–36. [Google Scholar] [CrossRef]



| Hurley Stage | IHS4 Stage | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall (n = 95) | Mild (n = 45) | Moderate (n = 35) | Severe (n = 15) | p Value | Mild (n = 43) | Moderate (n = 33) | Severe (n = 19) | p Value | |
| % Females | 50.5 | 48.9 | 48.6 | 60 | 0.759 | 53.5 | 42.4 | 57.9 | 0.489 |
| % Current and Ex-smokers | 63.1 | 51.1 | 77.1 | 46.7 | 0.029 | 55.9 | 72.7 | 43.2 | 0.209 |
| % Rx adalimumab | 14.7 | 6.7 | 11.4 | 46.7 | 0.003 | 9.3 | 12.1 | 31.6 | 0.04 |
| % MetS | 34 | 34.1 | 34.3 | 33.3 | 1 | 30.2 | 46.9 | 21.1 | 0.14 |
| Age years | 34 (24) | 29 (16) | 37 (21) | 45 (31) | 0.087 | 30 (22) | 35 (14) | 36 (31) | 0.433 |
| BMI kg/m2 | 31.3 (11) | 33.6 (12.3) | 29.4 (11.4) | 33.9 (12.6) | 0.188 | 28.9 (11.9) | 34.1 (12.6) | 31.5 (9) | 0.207 |
| WBC × 109/L | 7.97 (2.86) | 7.34 (3.07) | 7.98 (2.87) | 9.14 (2.67) | 0.014 | 7.3 (3.54) | 7.92 (2.21) | 8.78 (2.89) | 0.05 |
| NLR | 2.32 (1.04) | 2.11 (1.05) | 2.36 (0.94) | 2.66 (3.01) | 0.05 | 2.15 (1.07) | 2.38 (0.97) | 2.66 (2.05) | 0.046 |
| PLR | 136.42 (73.59) | 135.40 (67.34) | 140.10 (59.50) | 167.89 (133.08) | 0.768 | 136.52 (72.41) | 138.57 (73.59) | 132.17 (97.56) | 0.919 |
| MLR | 0.27 (0.12) | 0.27 (0.10) | 0.29 (0.12) | 0.28 (0.27) | 0.746 | 0.26 (0.1) | 0.29 (0.13) | 0.28 (0.13) | 0.445 |
| LMR | 3.66 (1.69) | 3.73 (1.53) | 3.43 (1.70) | 3.62 (3.13) | 0.746 | 3.87 (1.65) | 3.44 (1.87) | 3.54 (1.8) | 0.445 |
| ESR mm 1st Hr | 14 (26) | 9 (15) | 17 (28) | 46 (45) | <0.001 | 9 (12) | 14 (21) | 36 (38) | <0.001 |
| CRP mg/L | 3.9 (7) | 2.1 (3.2) | 5 (7.6) | 12 (21.5) | <0.001 | 2 (4.2) | 4.7 (6.6) | 9.8 (21.3) | 0.001 |
| Ferritin ng/mL | 61 (90) | 62 (81) | 60 (98) | 56 (143) | 0.847 | 55 (76) | 52 (130) | 70 (60) | 0.625 |
| IgG g/L | 12.2 (2.8) | 11.35 (2.7) | 12 (1.8) | 16.6 (6.7) | <0.001 | 11.6 (3.1) | 11.7 (2.4) | 14.1 (5.5) | <0.001 |
| IgM g/L | 0.9 (0.73) | 0.86 (0.7) | 0.75 (0.61) | 1.27 (0.51) | 0.05 | 0.8 (0.62) | 0.92 (0.77) | 1.19 (1.11) | 0.1 |
| IgA g/L | 2.195 (1) | 2.055 (0.65) | 2.253 (1.25) | 3.65 (2.39) | 0.002 | 2.07 (0.83) | 2.09 (1.08) | 3.25 (1.97) | 0.036 |
| IHS4 | 4 (8) | 2 (3) | 6 (8) | 24 (15) | <0.001 | 1 (2) | 5 (3) | 18 (15) | <0.001 |
| % Hurley Stage | 47.4 | 36.8 | 15.8 | ||||||
| IHS4 | HSS | ||||
|---|---|---|---|---|---|
| β (95% CI) | p Value | β (95% CI) | p Value | ||
| Model 1 | IgG | 0.14 (0.041–0.22) | 0.001 | 0.31 (0.146–0.475) | <0.001 |
| IgA | 0.109 (−0.09–0.307) | 0.284 | 0.354 (−0.042–0.749) | 0.08 | |
| IgM | 0.237 (−0.049–0.542) | 0.104 | 0.303 (−0.089–0.7649) | 0.13 | |
| Model 2 | IgG | 0.14 (0.058–0.223) | 0.001 | 0.3847 (0.192–0.581) | <0.001 |
| IgA | 0.081 (−0.124–0.285) | 0.438 | 0.291 (−0.107–0.689) | 0.151 | |
| IgM | 0.281 (−0.02–0.583) | 0.06 | 0.422 (−0.004–0.847) | 0.052 | |
| Model 3 | IgG | 0.125 (0.038–0.213) | 0.005 | 0.373 (0.173–0.574) | <0.001 |
| IgA | 0.034 (−0.186–0.255) | 0.76 | 0.248 (0.170–0.667) | 0.245 | |
| IgM | 0.274 (−0.022–0.571) | 0.07 | 0.398 (−0.037–0.833) | 0.073 | |
| Hurley Severe vs. Hurley Moderate/Mild | IHS4 Severe vs. IHS4 Moderate/Mild | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Marker | AUC | SE AUC | 95%CI L | 95%CI U | p | AUC | SE AUC | 95%CI L | 95%CI U | p |
| IgG | 0.90 | 0.04 | 0.86 | 0.97 | <0.001 | 0.79 | 0.05 | 0.69 | 0.89 | <0.001 |
| IgM | 0.69 | 0.07 | 0.56 | 0.82 | <0.001 | 0.65 | 0.08 | 0.51 | 0.80 | 0.409 |
| IgA | 0.78 | 0.08 | 0.62 | 0.95 | <0.001 | 0.69 | 0.08 | 0.54 | 0.84 | 0.011 |
| SII | 0.71 | 0.09 | 0.53 | 0.88 | 0.020 | 0.69 | 0.08 | 0.53 | 0.85 | 0.017 |
| NLR | 0.67 | 0.09 | 0.49 | 0.84 | 0.058 | 0.66 | 0.08 | 0.51 | 0.81 | 0.041 |
| Hurley Severe vs. Hurley Mild | IHS4 Severe vs. IHS4 Mild | |||||||||
| IgG | 0.92 | 0.04 | 0.86 | 0.99 | <0.001 | 0.81 | 0.06 | 0.70 | 0.92 | <0.001 |
| IgM | 0.69 | 0.08 | 0.54 | 0.84 | 0.030 | 0.68 | 0.08 | 0.52 | 0.83 | 0.026 |
| IgA | 0.80 | 0.08 | 0.64 | 0.97 | <0.001 | 0.71 | 0.08 | 0.54 | 0.87 | 0.010 |
| SII | 0.74 | 0.09 | 0.56 | 0.94 | 0.007 | 0.69 | 0.08 | 0.54 | 0.84 | 0.018 |
| NLR | 0.70 | 0.09 | 0.53 | 0.87 | 0.024 | 0.69 | 0.08 | 0.54 | 0.84 | 0.019 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mintoff, D.; Borg, I.; Pace, N.P. Serum Immunoglobulin G Is a Marker of Hidradenitis Suppurativa Disease Severity. Int. J. Mol. Sci. 2022, 23, 13800. https://doi.org/10.3390/ijms232213800
Mintoff D, Borg I, Pace NP. Serum Immunoglobulin G Is a Marker of Hidradenitis Suppurativa Disease Severity. International Journal of Molecular Sciences. 2022; 23(22):13800. https://doi.org/10.3390/ijms232213800
Chicago/Turabian StyleMintoff, Dillon, Isabella Borg, and Nikolai P. Pace. 2022. "Serum Immunoglobulin G Is a Marker of Hidradenitis Suppurativa Disease Severity" International Journal of Molecular Sciences 23, no. 22: 13800. https://doi.org/10.3390/ijms232213800
APA StyleMintoff, D., Borg, I., & Pace, N. P. (2022). Serum Immunoglobulin G Is a Marker of Hidradenitis Suppurativa Disease Severity. International Journal of Molecular Sciences, 23(22), 13800. https://doi.org/10.3390/ijms232213800






