Development of a Molecular Aptamer Beacon Applied to Magnetic-Assisted RNA Extraction for Detection of Dengue and Zika Viruses Using Clinical Samples
Abstract
1. Introduction
2. Results
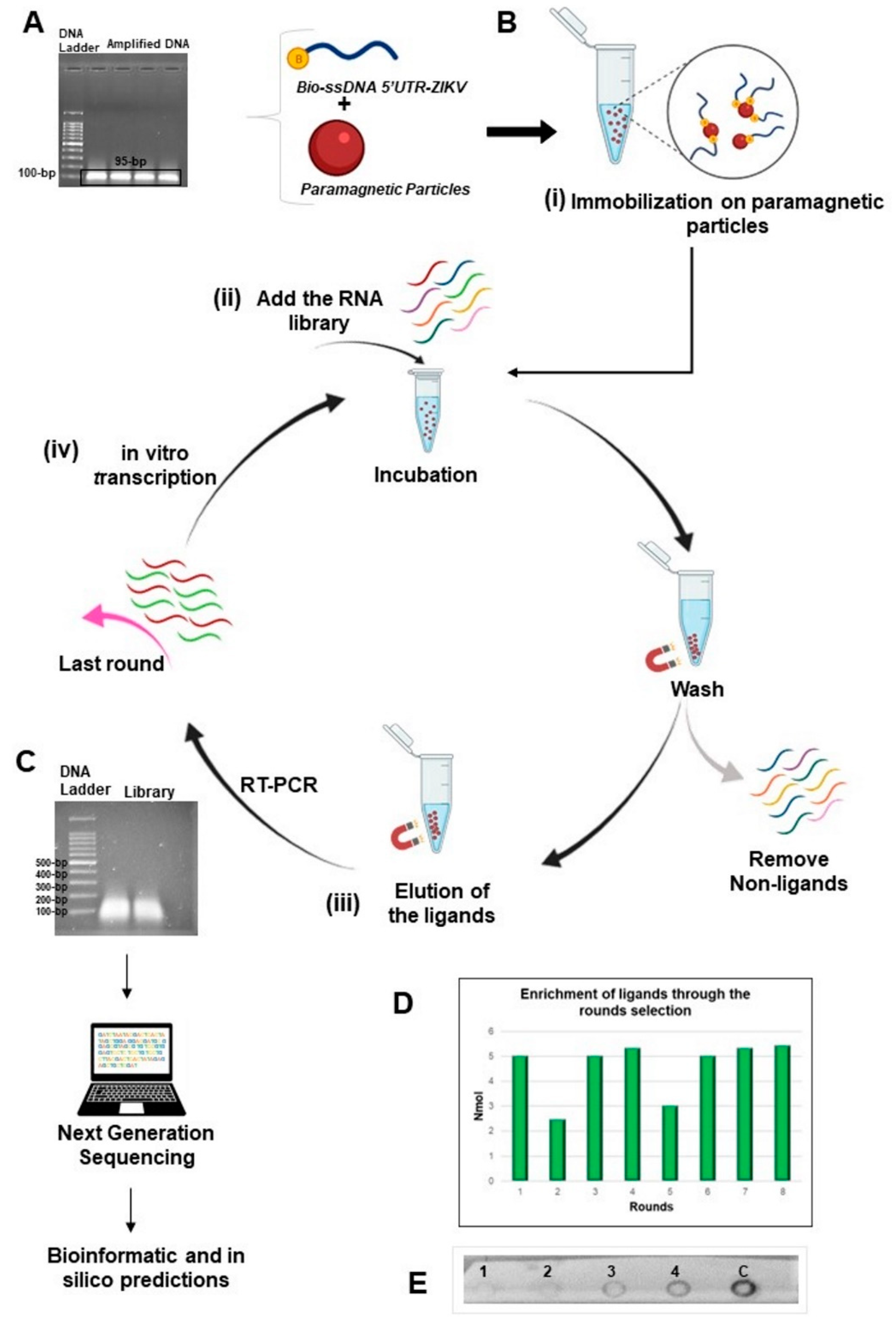
2.1. Target Production and SELEX
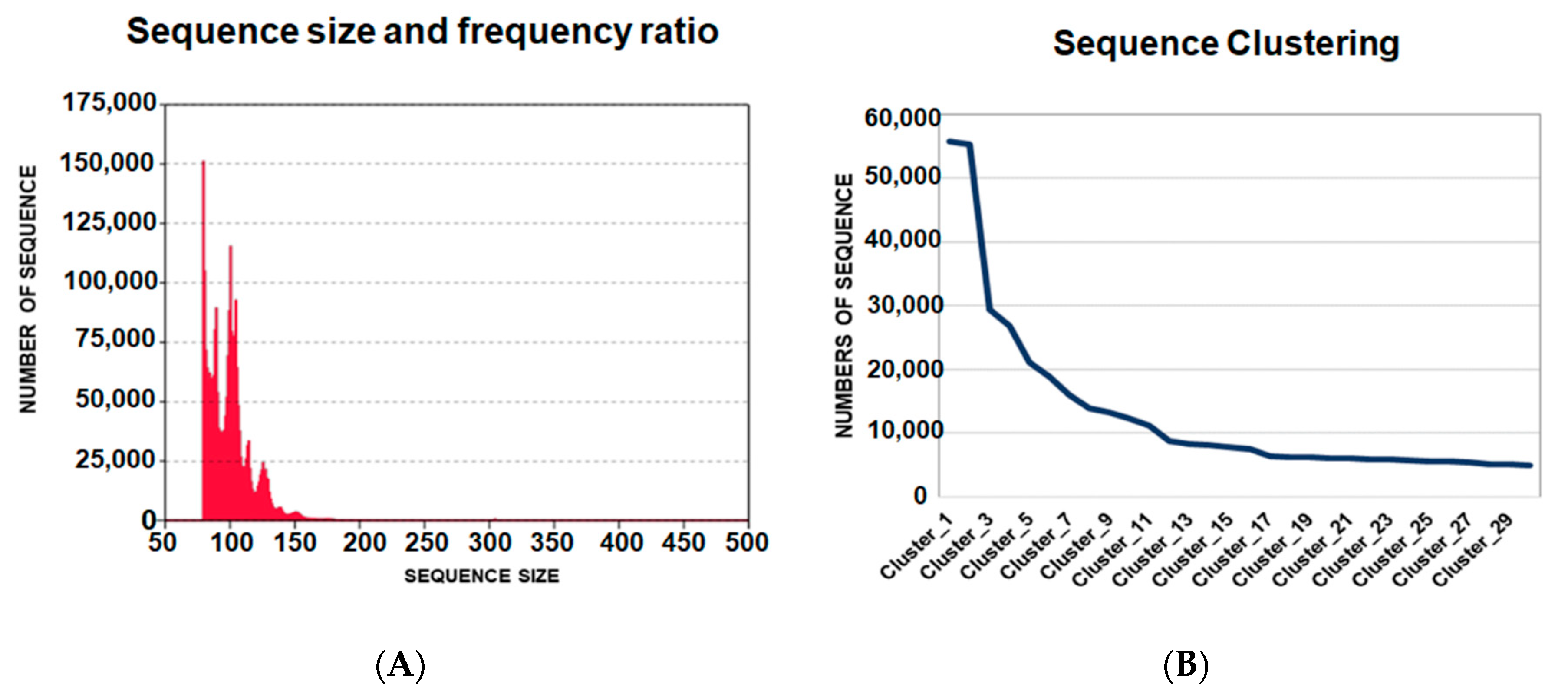
2.2. Analysis of the Sequences from Next-Generation Sequencing
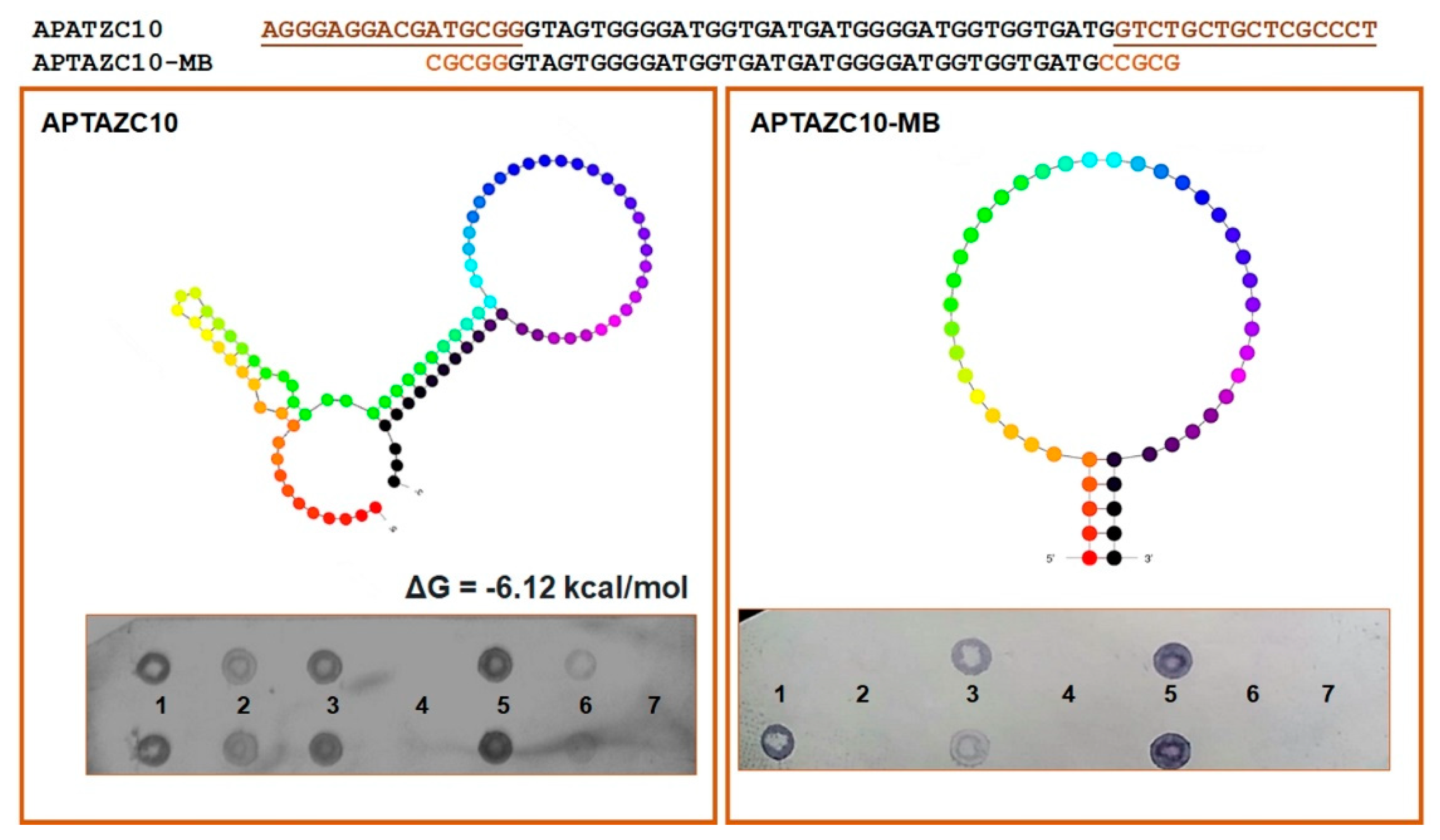
2.3. The Characterization of APTAZC10-MB
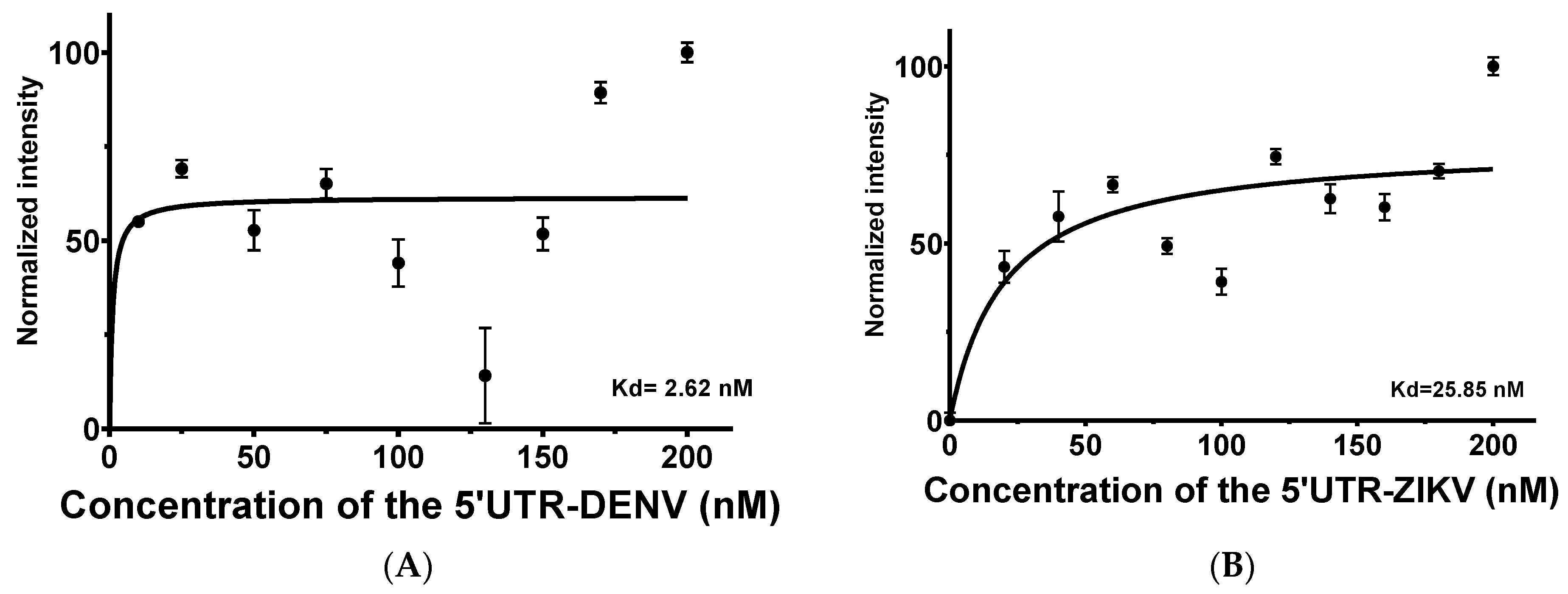
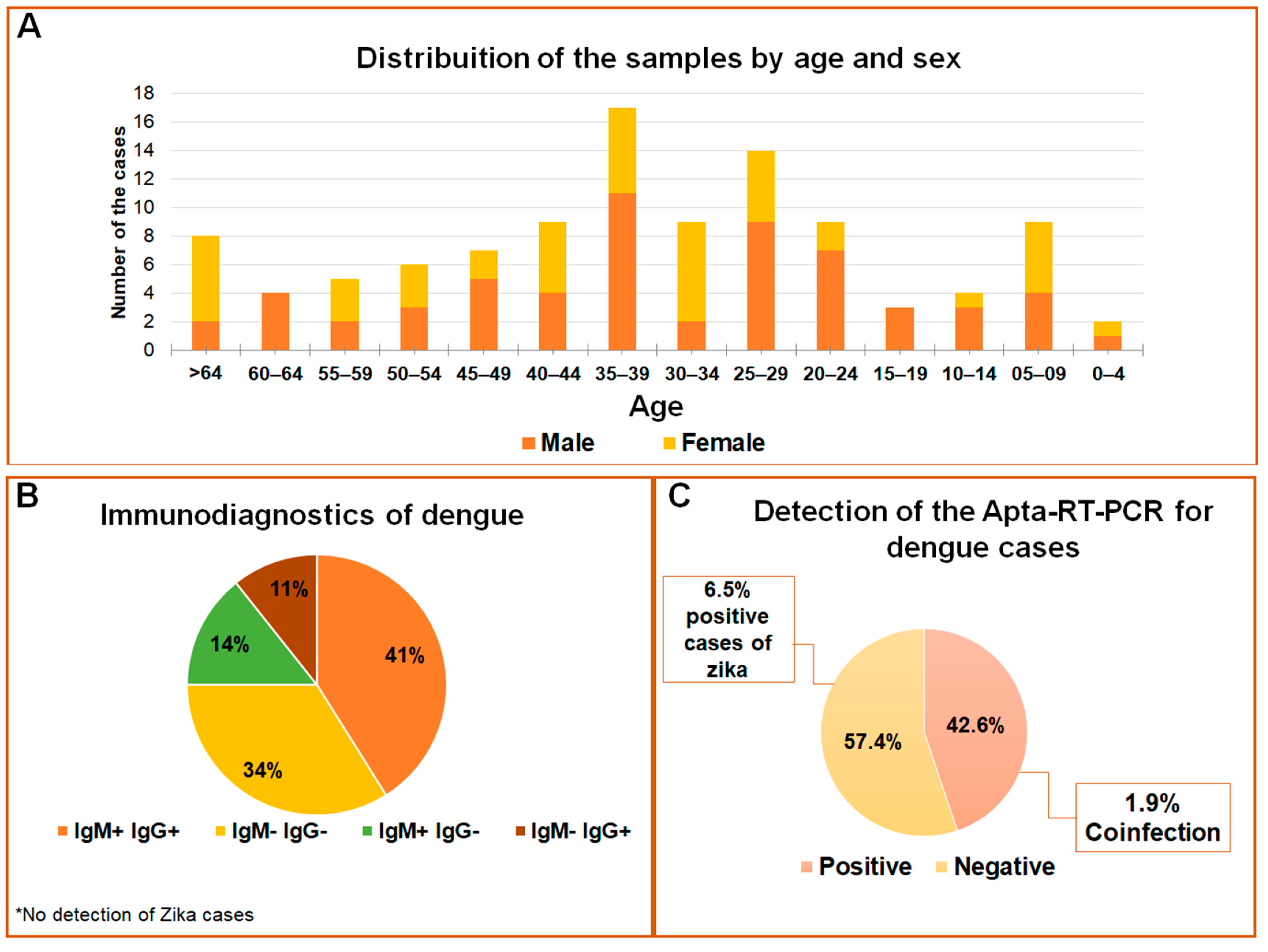
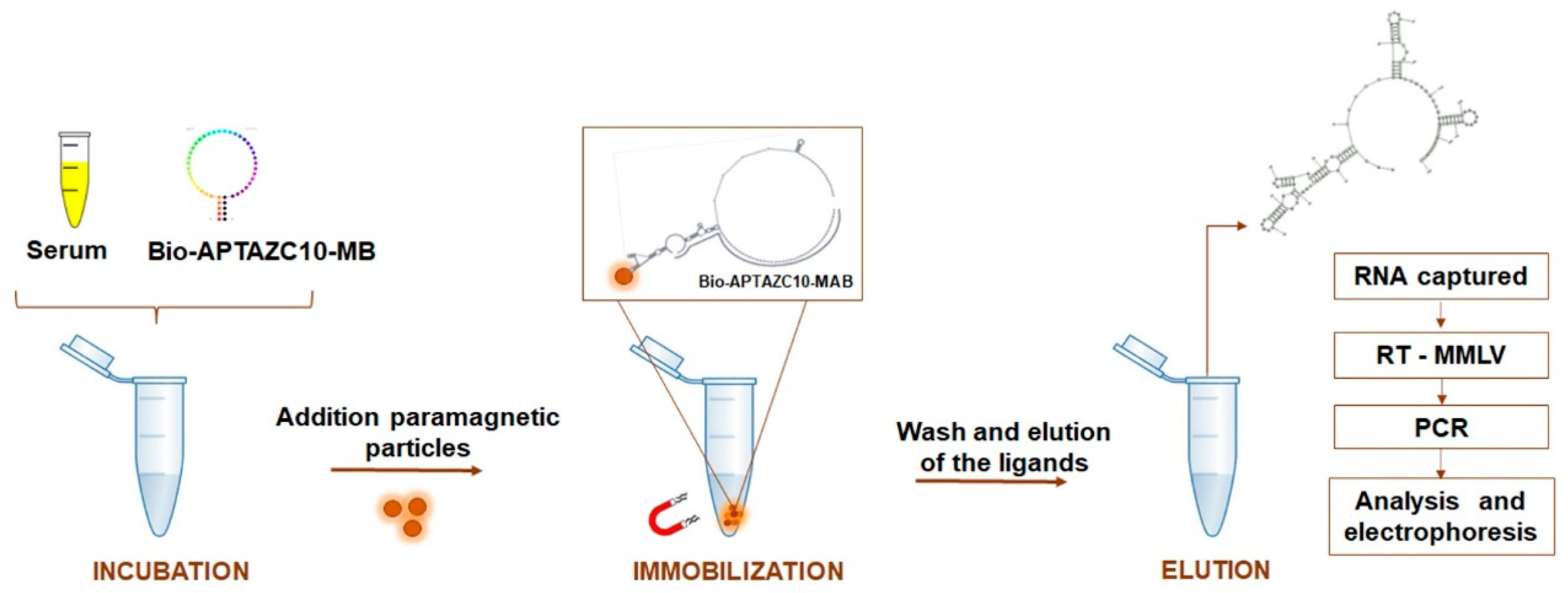
2.4. APTA-RT-PCR Development for DENV and ZIKV Detections
3. Discussion
4. Materials and Methods
4.1. Chemicals
4.2. 5′UTR-ZIKV as a Target for SELEX
4.3. Library Construction and Ligands Selection
4.4. Enrichment of the RNA Aptamers
4.5. Next-Generation Sequencing and Data Analysis
4.6. Chemical Modifications to Produce a Molecular Aptamer Beacon
4.7. APTA-RT-PCR for DENV and ZIKV Detections in Serum Samples
4.8. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ioos, S.; Mallet, H.P.; Leparc Goffart, I.; Gauthier, V.; Cardoso, T.; Herida, M. Current Zika virus epidemiology and recent epidemics. Méd. Mal. Infect. 2014, 44, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Faye, O.; Freire, C.C.M.; Iamarino, A.; Faye, O.; de Oliveira, J.V.C.; Diallo, M.; Zanotto, P.M.A.; Sall, A.A. Molecular Evolution of Zika Virus during Its Emergence in the 20th Century. PLoS Negl. Trop. Dis. 2014, 8, e2636. [Google Scholar] [CrossRef] [PubMed]
- Weaver, S.C.; Costa, F.; Garcia-Blanco, M.A.; Ko, A.I.; Ribeiro, G.S.; Saade, G.; Shi, P.Y.; Vasilakis, N. Zika virus: History, emergence, biology, and prospects for control. Antivir. Res. 2016, 130, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Oehler, E.; Watrin, L.; Larre, P.; Leparc-Goffart, I.; Lastere, S.; Valour, F.; Baudouin, L.; Mallet, H.P.; Musso, D.; Ghawche, F. Zika virus infection complicated by Guillain-barré syndrome—Case report, French Polynesia, December 2013. Eurosurveillance 2014, 19, 20720. [Google Scholar] [CrossRef] [PubMed]
- Zanluca, C.; De Melo, V.C.A.; Mosimann, A.L.P.; Dos Santos, G.I.V.; dos Santos, C.N.D.; Luz, K. First report of autochthonous transmission of Zika virus in Brazil. Mem. Inst. Oswaldo Cruz 2015, 110, 569–572. [Google Scholar] [CrossRef] [PubMed]
- Musso, D.; Roche, C.; Robin, E.; Nhan, T.; Teissier, A.; Cao-Lormeau, V.M. Potential sexual transmission of Zika virus. Emerg. Infect. Dis. 2015, 21, 359–361. [Google Scholar] [CrossRef]
- Gerdts, C.; Fuentes, L.; Wahlin, B.; Blanchard, K. Zika Virus and Pregnancy: What Obstetric Health Care Providers Need to Know. Obstet. Gynecol. 2016, 127, 642–648. [Google Scholar] [CrossRef]
- Calvet, G.; Aguiar, R.S.; Melo, A.S.O.; Sampaio, S.A.; de Filippis, I.; Fabri, A.; Araujo, E.S.M.; de Sequeira, P.C.; de Mendonça, M.C.L.; de Oliveira, L.; et al. Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: A case study. Lancet Infect. Dis. 2016, 16, 653–660. [Google Scholar] [CrossRef]
- Martines, R.B.; Bhatnagar, J.; Keating, M.K.; Silva-Flannery, L.; Muehlenbachs, A.; Gary, J.; Goldsmith, C.; Hale, G.; Ritter, J.; Rollin, D.; et al. Notes from the Field: Evidence of Zika Virus Infection in Brain and Placental Tissues from Two Congenitally Infected Newborns and Two Fetal Losses—Brazil, 2015. MMWR. Morb. Mortal. Wkly. Rep. 2016, 65, 159–160. [Google Scholar] [CrossRef]
- Barzon, L.; Percivalle, E.; Pacenti, M.; Rovida, F.; Zavattoni, M.; Del Bravo, P.; Cattelan, A.M.; Palù, G.; Baldanti, F. Virus and Antibody Dynamics in Travelers With Acute Zika Virus Infection. Clin. Infect. Dis. 2018, 66, 1173–1180. [Google Scholar] [CrossRef]
- Dejnirattisai, W.; Supasa, P.; Wongwiwat, W.; Rouvinski, A.; Barba-spaeth, G.; Duangchinda, T.; Sakuntabhai, A.; Malasit, P.; Rey, F.A.; Mongkolsapaya, J.; et al. Dengue virus sero-cross-reactivity drives antibody- dependent enhancement of infection with Zika virus. Nat. Immunol. 2016, 17, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Kikuti, M.; Tauro, L.B.; Moreira, P.S.S.; Campos, G.S.; Paploski, I.A.D.; Weaver, S.C.; Reis, M.G.; Kitron, U.; Ribeiro, G.S. Diagnostic performance of commercial IgM and IgG enzyme-linked immunoassays (ELISAs) for diagnosis of Zika virus infection. Virol. J. 2018, 15, 108. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Han, H.; Liu, F.; Lv, Z.; Wu, K.; Liu, Y.; Feng, Y.; Zhu, C. Positive rate of RT-PCR detection of SARS-CoV-2 infection in 4880 cases from one hospital in Wuhan, China, from Jan to Feb 2020. Clin. Chim. Acta 2020, 505, 172–175. [Google Scholar] [CrossRef] [PubMed]
- Judice, C.C.; Tan, J.J.L.; Parise, P.L.; Kam, Y.; Milanez, P.; Leite, J.A.; Caserta, L.C.; Arns, C.W.; Resende, M.R.; Angerami, R.; et al. Efficient detection of Zika virus RNA in patients’ blood from the 2016 outbreak in Campinas, Brazil. Sci. Rep. 2018, 8, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Ministério da Saúde. Dengue: Diagnóstico e Manejo Clínico, 5th ed.; Ministério da Saúde: Brasília, Brazil, 2016; ISBN 9788533417700.
- Brasil. Ministério da Saúde. Procedimentos a Serem Adotados Para a Vigilância da Febre do Vírus Zika no Brasil; 2016; pp. 1–7. Available online: https://www.conasems.org.br/wp-content/uploads/2016/03/portalsaude.saude.gov.br_images_pdf_2016_marco_07_Nota-Informativa-zika.pdf (accessed on 30 September 2020).
- Zou, X.; Wu, J.; Gu, J.; Shen, L.; Mao, L. Application of Aptamers in Virus Detection and Antiviral Therapy. Front. Microbiol. 2019, 10, 1462. [Google Scholar] [CrossRef] [PubMed]
- González, V.M.; Elena Martín, M.; Fernández, G.; García-Sacristán, A. Use of aptamers as diagnostics tools and antiviral agents for human viruses. Pharmaceuticals 2016, 9, 78. [Google Scholar] [CrossRef]
- World Health Organization, Regional Office for South-East Asia. Dengue Bulletin, Volume 41; World Health Organization, Regional Office for South-East Asia: New Delhi, India, 2020; ISSN 0250-8362. [Google Scholar]
- Jung, J.I.; Han, S.R.; Lee, S.W. Development of RNA aptamer that inhibits methyltransferase activity of dengue virus. Biotechnol. Lett. 2018, 40, 315–324. [Google Scholar] [CrossRef]
- Cnossen, E.J.; Silva, A.G.; Marangoni, K.; Arruda, R.A.; Souza, E.G.; Santos, F.A.; Fujimura, P.T.; Yokosawa, J.; Goulart, L.R.; Neves, A.F. Characterization of oligonucleotide aptamers targeting the 5′-UTR from dengue virus. Future Med. Chem. 2017, 9, 541–552. [Google Scholar] [CrossRef]
- Chen, H.-L.; Hsiao, W.-H.; Lee, H.-C.; Wu, S.-C.; Cheng, J.-W. Selection and Characterization of DNA Aptamers Targeting All Four Serotypes of Dengue Viruses. PLoS ONE 2015, 10, e131240. [Google Scholar] [CrossRef]
- Balinsky, C.A.; Schmeisser, H.; Ganesan, S.; Singh, K.; Pierson, T.C.; Zoon, K.C. Nucleolin Interacts with the Dengue Virus Capsid Protein and Plays a Role in Formation of Infectious Virus Particles. J. Virol. 2013, 87, 13094–13106. [Google Scholar] [CrossRef]
- Saito, S. SELEX-based DNA Aptamer Selection: A Perspective from the Advancement of Separation Techniques. Anal. Sci. 2021, 37, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Jiang, L.; Zeng, G. Non-coding RNA: A key regulator of the pathogenicity and immunity of Flaviviridae viruses infection. Cell. Mol. Immunol. 2018, 15, 185–186. [Google Scholar] [CrossRef] [PubMed]
- Gebhard, L.G.; Filomatori, C.V.; Gamarnik, A.V. Functional RNA elements in the dengue virus genome. Viruses 2011, 3, 1739–1756. [Google Scholar] [CrossRef]
- Shurtleff, A.C.; Beasley, D.W.C.; Chen, J.J.Y.; Ni, H.; Suderman, M.T.; Wang, H.; Xu, R.; Wang, E.; Weaver, S.C.; Watts, D.M.; et al. Genetic Variation in the 3′ Non-Coding Region of Dengue Viruses. Virology 2001, 281, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Chan, J.F.W.; Tee, K.M.; Choi, G.K.Y.; Lau, S.K.P.; Woo, P.C.Y.; Tse, H.; Yuen, K.Y. Comparative genomic analysis of pre-epidemic and epidemic Zika virus strains for virological factors potentially associated with the rapidly expanding epidemic. Emerg. Microbes Infect. 2016, 5, e22. [Google Scholar] [CrossRef]
- Gouel-Cheron, A.; Lumbard, K.; Hunsberger, S.; Arteaga-Cabello, F.J.; Beigel, J.; Belaunzarán-Zamudio, P.F.; Caballero-Sosa, S.; Escobedo-López, K.; Ibarra-González, V.; Nájera-Cancino, J.G.; et al. Serial real-time RT-PCR and serology measurements substantially improve Zika and Dengue virus infection classification in a co-circulation area. Antivir. Res. 2019, 172, 104638. [Google Scholar] [CrossRef]
- Darmostuk, M.; Rimpelova, S.; Gbelcova, H.; Ruml, T. Current approaches in SELEX: An update to aptamer selection technology. Biotechnol. Adv. 2014, 33, 1141–1161. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.H.; Zeng, H. Aptamer-Based ELISA Assay for Highly Specific and Sensitive Detection of Zika NS1 Protein. Anal. Chem. 2017, 89, 12743–12748. [Google Scholar] [CrossRef]
- Saraf, N.; Villegas, M.; Willenberg, B.J.; Seal, S. Multiplex Viral Detection Platform Based on a Aptamers-Integrated Microfluidic Channel. ACS Omega 2019, 4, 2234–2240. [Google Scholar] [CrossRef]
- Kim, D.T.H.; Bao, D.T.; Park, H.; Ngoc, N.M.; Yeo, S.J. Development of a novel peptide aptamer-based immunoassay to detect Zika virus in serum and urine. Theranostics 2018, 8, 3629–3642. [Google Scholar] [CrossRef]
- Oteng, E.K.; Gu, W.; McKeague, M. High-efficiency enrichment enables identification of aptamers to circulating Plasmodium falciparum-infected erythrocytes. Sci. Rep. 2020, 10, 9706. [Google Scholar] [CrossRef] [PubMed]
- Dorraj, G.S.; Rassaee, M.J.; Latifi, A.M.; Pishgoo, B.; Tavallaei, M. Selection of DNA aptamers against Human Cardiac Troponin I for colorimetric sensor based dot blot application. J. Biotechnol. 2015, 208, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhang, J.; Pei, X.; Zhang, Q.; Lu, B.; Zhang, X.; Liu, J. An aptamer targets HBV core protein and suppresses HBV replication in HepG2.2.15 cells. Int. J. Mol. Med. 2014, 34, 1423–1429. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Zhao, J.; Jiang, T.; Kwon, Y.M.; Lu, H.; Jiao, P.; Liao, M.; Li, Y. Selection and characterization of DNA aptamers for use in detection of avian influenza virus H5N1. J. Virol. Methods 2013, 189, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Marangoni, K.; Neves, A.F.; Rocha, R.M.; Faria, P.R.; Alves, P.T.; Souza, A.G.; Fujimura, P.T.; Santos, F.A.A.; Araújo, T.G.; Ward, L.S.; et al. Prostate-specific RNA aptamer: Promising nucleic acid antibody-like cancer detection. Sci. Rep. 2015, 5, 12090. [Google Scholar] [CrossRef]
- Nguyen Quang, N.; Bouvier, C.; Henriques, A.; Lelandais, B.; Ducongé, F. Time-lapse imaging of molecular evolution by high-throughput sequencing. Nucleic Acids Res. 2018, 46, 7480–7494. [Google Scholar] [CrossRef]
- Schütze, T.; Wilhelm, B.; Greiner, N.; Braun, H.; Peter, F.; Mörl, M.; Erdmann, V.A.; Lehrach, H.; Konthur, Z.; Menger, M.; et al. Probing the SELEX process with next-generation sequencing. PLoS ONE 2011, 6, e29604. [Google Scholar] [CrossRef]
- Cho, M.; Xiao, Y.; Nie, J.; Stewart, R.; Csordas, A.T.; Oh, S.S.; Thomson, J.A.; Soh, H.T. Quantitative selection of DNA aptamers through microfluidic selection and high-throughput sequencing. Proc. Natl. Acad. Sci. USA 2010, 107, 15373–15378. [Google Scholar] [CrossRef]
- Zuker, M. Mfold web server for nucleic acid folding and hybridization prediction. Nucleic Acids Res. 2003, 31, 3406–3415. [Google Scholar] [CrossRef]
- Zadeh, J.N.; Steenberg, C.D.; Bois, J.S.; Wolfe, B.R.; Pierce, M.B.; Khan, A.R.; Dirks, R.M.; Pierce, N.A. NUPACK: Analysis and design of nucleic acid systems. J. Comput. Chem. 2011, 32, 170–173. [Google Scholar] [CrossRef]
- Bellaousov, S.; Reuter, J.S.; Seetin, M.G.; Mathews, D.H. RNAstructure: Web servers for RNA secondary structure prediction and analysis. Nucleic Acids Res. 2013, 41, W471–W474. [Google Scholar] [CrossRef] [PubMed]
- Santini, B.L.; Zúñiga-Bustos, M.; Vidal-Limon, A.; Alderete, J.B.; Águila, S.A.; Jiménez, V.A. In Silico Design of Novel Mutant Anti-MUC1 Aptamers for Targeted Cancer Therapy. J. Chem. Inf. Model. 2020, 60, 786–793. [Google Scholar] [CrossRef] [PubMed]
- Soon, S.; Aina Nordin, N. In silico predictions and optimization of aptamers against Streptococcus agalactiae surface protein using computational docking. Mater. Today Proc. 2019, 16, 2096–2100. [Google Scholar] [CrossRef]
- Rockey, W.M.; Hernandez, F.J.; Huang, S.-Y.; Cao, S.; Howell, C.A.; Thomas, G.S.; Liu, X.Y.; Lapteva, N.; Spencer, D.M.; McNamara, J.O.; et al. Rational truncation of an RNA aptamer to prostate-specific membrane antigen using computational structural modeling. Nucleic Acid Ther. 2011, 21, 299–314. [Google Scholar] [CrossRef] [PubMed]
- Bhadra, S.; Ellington, A.D. Design, synthesis, and application of spinach molecular beacons triggered by strand displacement. Methods Enzymol. 2015, 550, 215–249. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Yang, R.; Shi, M.; Wu, C.; Fang, X.; Li, Y.; Li, J.; Tan, W. Rationally designed molecular beacons for bioanalytical and biomedical applications. Chem. Soc. Rev. 2015, 44, 3036–3055. [Google Scholar] [CrossRef]
- Beltrán-Silva, S.L.; Chacón-Hernández, S.S.; Moreno-Palacios, E.; Pereyra-Molina, J.Á. Clinical and differential diagnosis: Dengue, chikungunya and Zika. Rev. Médica Hosp. Gen. México 2018, 81, 146–153. [Google Scholar] [CrossRef]
- Zainah, S.; Wahab, A.H.A.; Mariam, M.; Fauziah, M.K.; Khairul, A.H.; Roslina, I.; Sairulakhma, A.; Kadimon, S.S.; Jais, M.S.M.; Chua, K.B. Performance of a commercial rapid dengue NS1 antigen immunochromatography test with reference to dengue NS1 antigen-capture ELISA. J. Virol. Methods 2009, 155, 157–160. [Google Scholar] [CrossRef]
- De Cavalcanti, L.P.G.; de Braga, D.N.M.; da Silva, L.M.A.; Aguiar, M.G.; Castiglioni, M.; Silva-Junior, J.U.; da Araújo, F.M.C.; da Pereira, R.A.C.; Malta, D.L.; de Pompeu, M.M.L. Postmortem Diagnosis of Dengue as an Epidemiological Surveillance Tool. Am. J. Trop. Med. Hyg. 2016, 94, 187–192. [Google Scholar] [CrossRef]
- Nogueira, R.M.; Miagostovich, M.P.; Schatzmayr, H.G. Molecular epidemiology of dengue viruses in Brazil. Cad. Saude Publica 2000, 16, 205–211. [Google Scholar] [CrossRef][Green Version]
- Peeling, R.W.; Artsob, H.; Pelegrino, J.L.; Buchy, P.; Cardosa, M.J.; Devi, S.; Enria, D.A.; Farrar, J.; Gubler, D.J.; Guzman, M.G.; et al. Evaluation of diagnostic tests: Dengue. Nat. Rev. Microbiol. 2010, 8, S30–S37. [Google Scholar] [CrossRef] [PubMed]
- Guzmán, M.G.; Kourí, G. Advances in dengue diagnosis. Clin. Diagn. Lab. Immunol. 1996, 3, 621–627. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Dengue: Guidelines for Diagnosis, Treatment, Prevention, and Control; World Health Organization: Geneva, Switzerland, 2009; ISBN 9789241547871. [Google Scholar]
- De Oliveira Poersch, C.; Pavoni, D.P.; Queiroz, M.H.; de Borba, L.; Goldenberg, S.; dos Santos, C.N.D.; Krieger, M.A. Dengue virus infections: Comparison of methods for diagnosing the acute disease. J. Clin. Virol. Off. Publ. Pan Am. Soc. Clin. Virol. 2005, 32, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Niesters, H.G.M. Clinical virology in real time. J. Clin. Virol. Off. Publ. Pan Am. Soc. Clin. Virol. 2002, 25 (Suppl. S3), S3–S12. [Google Scholar] [CrossRef]
- Zannoli, S.; Morotti, M.; Denicolò, A.; Tassinari, M.; Chiesa, C.; Pierro, A.; Sambri, V. Chapter 9—Diagnostics and laboratory techniques. In Chikungunya and Zika Viruses; Higgs, S., Vanlandingham, D.L., Powers, A.M., Eds.; Academic Press: New York, NY, USA, 2018; pp. 293–315. ISBN 978-0-12-811865-8. [Google Scholar]
- Castro-Jorge, L.A.; Machado, P.R.L.; Fávero, C.A.; Borges, M.C.; Passos, L.M.R.; de Oliveira, R.M.; Fonseca, B.A.L. Clinical evaluation of the NS1 antigen-capture ELISA for early diagnosis of dengue virus infection in Brazil. J. Med. Virol. 2010, 82, 1400–1405. [Google Scholar] [CrossRef]
- Innis, B.L.; Nisalak, A.; Nimmannitya, S.; Kusalerdchariya, S.; Chongswasdi, V.; Suntayakorn, S.; Puttisri, P.; Hoke, C.H. An Enzyme-Linked Immunosorbent Assay to Characterize Dengue Infections Where Dengue and Japanese Encephalitis Co-Circulate. Am. J. Trop. Med. Hyg. 1989, 40, 418–427. [Google Scholar] [CrossRef]
- Mora-Cárdenas, E.; Aloise, C.; Faoro, V.; Knap Gašper, N.; Korva, M.; Caracciolo, I.; D’Agaro, P.; Avšič-Županc, T.; Marcello, A. Comparative specificity and sensitivity of NS1-based serological assays for the detection of flavivirus immune response. PLoS Negl. Trop. Dis. 2020, 14, e0008039. [Google Scholar] [CrossRef]
- Zhang, B.; Salieb-Beugelaar, G.B.; Nigo, M.M.; Weidmann, M.; Hunziker, P. Diagnosing dengue virus infection: Rapid tests and the role of micro/nanotechnologies. Nanomedicine 2015, 11, 1745–1761. [Google Scholar] [CrossRef]
- Muller, D.A.; Depelsenaire, A.C.I.; Young, P.R. Clinical and laboratory diagnosis of dengue virus infection. J. Infect. Dis. 2017, 215, S89–S95. [Google Scholar] [CrossRef]
- Mata, V.E.; Passos, S.R.L.; Hökerberg, Y.H.M.; Berardinelli, G.M.; Dos Santos, M.A.B.; Fukuoka, L.V.B.; Maciel, A.C.F.S.R.; Dos Santos Rodrigues, C.D.; da Silva Santos, A.; de Vasconcellos Carvalhaes de Oliveira, R. Precisão e confiabilidade de um teste imuno-cromatográfico rápido NS1 para diagnóstico DENV-1 no ponto de atendimento e no laboratório. BMC Infect. Dis. 2017, 17, 594. [Google Scholar] [CrossRef]
- Van Meer, M.P.A.; Mögling, R.; Klaasse, J.; Chandler, F.D.; Pas, S.D.; van der Eijk, A.A.; Koopmans, M.P.G.; Reusken, C.B.E.M.; GeurtsvanKessel, C.H. Re-evaluation of routine dengue virus serology in travelers in the era of Zika virus emergence. J. Clin. Virol. 2017, 92, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Da Lima, M.R.Q.; Chouin-Carneiro, T.; Azeredo, E.; Barbosa, L.S.; Souza, T.M.A.; da Silva, J.B.C.; Nunes, P.C.G.; Dal Fabbro, M.; Facco, I.H.R.; Venâncio-da-Cunha, R.; et al. The inability of a dengue NS1 ELISA to detect Zika infections. Sci. Rep. 2019, 9, 18596. [Google Scholar] [CrossRef] [PubMed]
- Tsai, W.-Y.; Youn, H.H.; Brites, C.; Tsai, J.-J.; Tyson, J.; Pedroso, C.; Drexler, J.F.; Stone, M.; Simmons, G.; Busch, M.P.; et al. Distinguishing Secondary Dengue Virus Infection From Zika Virus Infection With Previous Dengue by a Combination of 3 Simple Serological Tests. Clin. Infect. Dis. 2017, 65, 1829–1836. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, M.B.; Cedillo-Barron, L.; González y Almeida, M.E.; Garcia-Cordero, J.; Campos, F.D.; Namorado-Tonix, K.; Perez, F. Serological tests reveal significant cross-reactive human antibody responses to Zika and Dengue viruses in the Mexican population. Acta Trop. 2020, 201, 105201. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.; Bermudo Redondo, M.C.; Ozalp, V.C.; O’Sullivan, C.K. Real-time apta-PCR for 20000-fold improvement in detection limit. Mol. Biosyst. 2009, 5, 548–553. [Google Scholar] [CrossRef] [PubMed]
- Guzman, M.G.; Gubler, D.J.; Izquierdo, A.; Martinez, E.; Halstead, S.B. Dengue infection. Nat. Rev. Dis. Prim. 2016, 2, 16055. [Google Scholar] [CrossRef]
- De La Cruz Hernández, S.I.; Flores-Aguilar, H.; González-Mateos, S.; López-Martínez, I.; Ortiz-Navarrete, V.; Ludert, J.E.; Del Angel, R.M. Viral load in patients infected with dengue is modulated by the presence of anti-dengue IgM antibodies. J. Clin. Virol. 2013, 58, 258–261. [Google Scholar] [CrossRef]
- Laue, T.; Emmerich, P.; Schmitz, H. Detection of dengue virus RNA in patients after primary or secondary dengue infection by using the TaqMan automated amplification system. J. Clin. Microbiol. 1999, 37, 2543–2547. [Google Scholar] [CrossRef]
- CDC—Centers for Disease Control and Prevention Diagnosis. Available online: https://www.cdc.gov/dengue/healthcare-providers/diagnosis.html (accessed on 10 October 2022).
- Sukla, S.; Mondal, P.; Biswas, S.; Ghosh, S. A Rapid and Easy-to-Perform Method of Nucleic-Acid Based Dengue Virus Diagnosis Using Fluorescence-Based Molecular Beacons. Biosensors 2021, 11, 479. [Google Scholar] [CrossRef]
- Hasegawa, H.; Savory, N.; Abe, K.; Ikebukuro, K. Methods for Improving Aptamer Binding Affinity. Molecules 2016, 21, 421. [Google Scholar] [CrossRef]
- Nomura, Y.; Yamazaki, K.; Amano, R.; Takada, K.; Nagata, T.; Kobayashi, N.; Tanaka, Y.; Fukunaga, J.; Katahira, M.; Kozu, T.; et al. Conjugation of two RNA aptamers improves binding affinity to AML1 Runt domain. J. Biochem. 2017, 162, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Songjaeng, A.; Thiemmeca, S.; Mairiang, D.; Punyadee, N.; Kongmanas, K.; Hansuealueang, P.; Tangthawornchaikul, N.; Duangchinda, T.; Mongkolsapaya, J.; Sriruksa, K.; et al. Development of a Singleplex Real-Time Reverse Transcriptase PCR Assay for Pan-Dengue Virus Detection and Quantification. Viruses 2022, 14, 1271. [Google Scholar] [CrossRef] [PubMed]
- Sievers, F.; Wilm, A.; Dineen, D.; Gibson, T.J.; Karplus, K.; Li, W.; Lopez, R.; McWilliam, H.; Remmert, M.; Söding, J.; et al. Fast, scalable generation of high-quality protein multiple sequence alignments using Clustal Omega. Mol. Syst. Biol. 2011, 7, 539. [Google Scholar] [CrossRef] [PubMed]
- Ali, E.O.M.; Babalghith, A.O.; Bahathig, A.O.S.; Dafalla, O.M.; Al-Maghamsi, I.W.; Mustafa, N.E.A.G.; Al-Zahrani, A.A.A.; Al-Mahmoudi, S.M.Y.; Abdel-Latif, M.E. Detection of Dengue Virus From Aedes aegypti (Diptera, Culicidae) in Field-Caught Samples From Makkah Al-Mokarramah, Kingdom of Saudi Arabia, Using RT-PCR. Front. Public Heal. 2022, 10, 850851. [Google Scholar] [CrossRef] [PubMed]
- Valiant, W.G.; Mattapallil, M.J.; Higgs, S.; Huang, Y.-J.S.; Vanlandingham, D.L.; Lewis, M.G.; Mattapallil, J.J. Simultaneous Coinfection of Macaques with Zika and Dengue Viruses Does not Enhance Acute Plasma Viremia but Leads to Activation of Monocyte Subsets and Biphasic Release of Pro-inflammatory Cytokines. Sci. Rep. 2019, 9, 7877. [Google Scholar] [CrossRef] [PubMed]
- Estofolete, C.F.; Terzian, A.C.B.; Colombo, T.E.; de Freitas Guimarães, G.; Ferraz, H.C.J.; da Silva, R.A.; Greque, G.V.; Nogueira, M.L. Co-infection between Zika and different Dengue serotypes during DENV outbreak in Brazil. J. Infect. Public Health 2019, 12, 178–181. [Google Scholar] [CrossRef]
- Maradani, B.S.; Parameswaran, S.; Subramanian, K. Development and characterization of DNA aptamer against Retinoblastoma by Cell-SELEX. Sci. Rep. 2022, 12, 16178. [Google Scholar] [CrossRef]
- Siddiqui, S.; Yuan, J. Binding Characteristics Study of DNA based Aptamers for E. coli O157:H7. Molecules 2021, 26, 204. [Google Scholar] [CrossRef]
| Diagnostic Methods | Advantages | Disadvantages |
|---|---|---|
| VIRAL ISOLATION |
|
|
| RT-PCR |
|
|
| REAL TIME RT-PCR |
| |
| PRNT |
|
|
| SEROLOGICAL TESTS |
|
|
| RAPID DIAGNOSTIC TEST |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Silva, A.G.; Goulart, L.R.; Löffler, P.; Code, C.; Neves, A.F. Development of a Molecular Aptamer Beacon Applied to Magnetic-Assisted RNA Extraction for Detection of Dengue and Zika Viruses Using Clinical Samples. Int. J. Mol. Sci. 2022, 23, 13866. https://doi.org/10.3390/ijms232213866
da Silva AG, Goulart LR, Löffler P, Code C, Neves AF. Development of a Molecular Aptamer Beacon Applied to Magnetic-Assisted RNA Extraction for Detection of Dengue and Zika Viruses Using Clinical Samples. International Journal of Molecular Sciences. 2022; 23(22):13866. https://doi.org/10.3390/ijms232213866
Chicago/Turabian Styleda Silva, Amanda Gabrielle, Luiz Ricardo Goulart, Philipp Löffler, Christian Code, and Adriana Freitas Neves. 2022. "Development of a Molecular Aptamer Beacon Applied to Magnetic-Assisted RNA Extraction for Detection of Dengue and Zika Viruses Using Clinical Samples" International Journal of Molecular Sciences 23, no. 22: 13866. https://doi.org/10.3390/ijms232213866
APA Styleda Silva, A. G., Goulart, L. R., Löffler, P., Code, C., & Neves, A. F. (2022). Development of a Molecular Aptamer Beacon Applied to Magnetic-Assisted RNA Extraction for Detection of Dengue and Zika Viruses Using Clinical Samples. International Journal of Molecular Sciences, 23(22), 13866. https://doi.org/10.3390/ijms232213866







