Antithrombin Activity and Association with Risk of Thrombosis and Mortality in Patients with Cancer
Abstract
:1. Introduction
2. Results
2.1. Patient Characteristics
2.2. Distribution of Antithrombin Levels
2.3. Antithrombin Activity and Risk of VTE and ATE
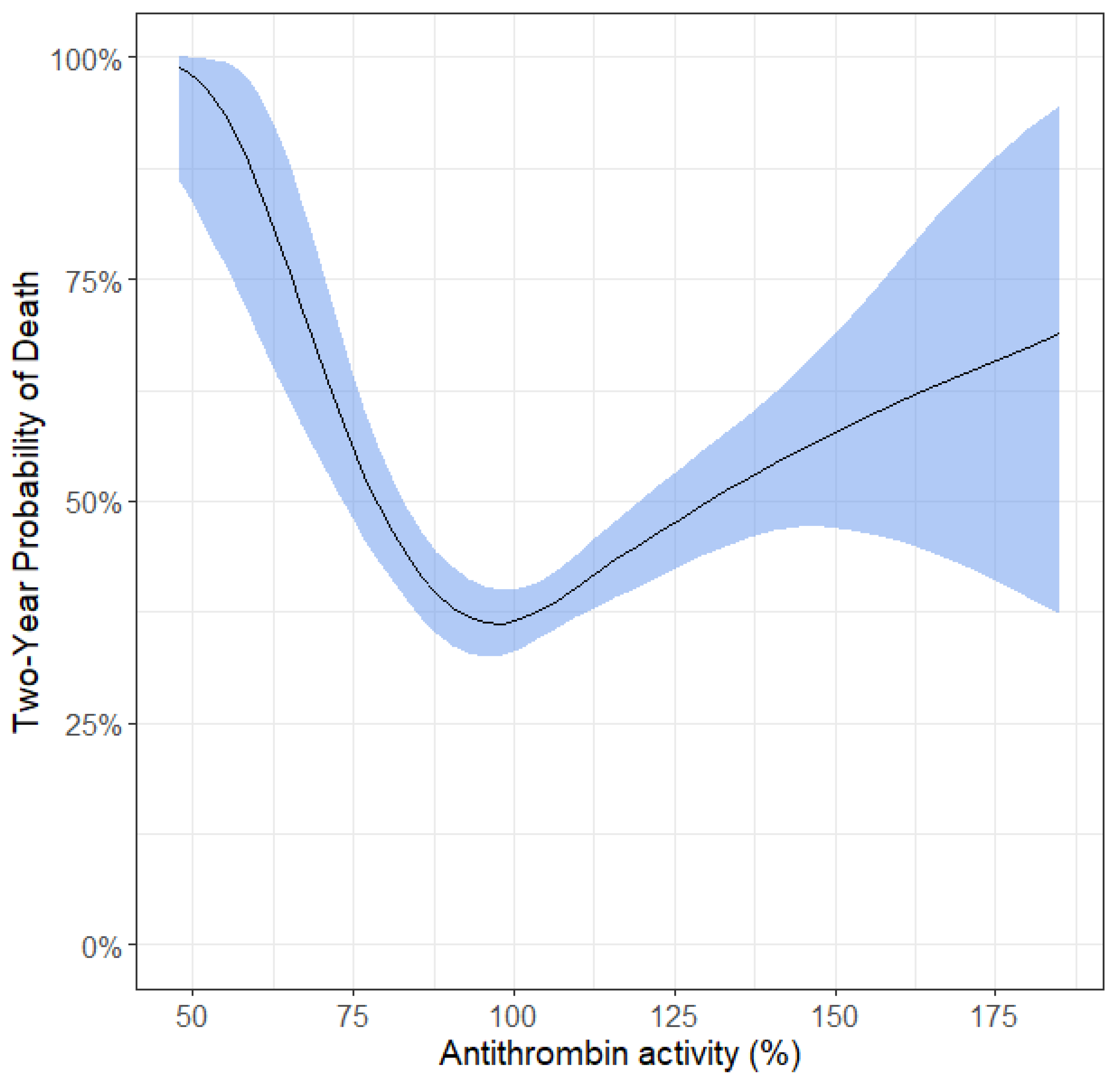
2.4. Antithrombin Activity and All-Cause Mortality
3. Discussion
4. Materials and Methods
4.1. Study Cohort
4.2. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ay, C.; Pabinger, I.; Cohen, A.T. Cancer-associated venous thromboembolism: Burden, mechanisms, and management. Thromb. Haemost. 2017, 117, 219–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grilz, E.; Posch, F.; Nopp, S.; Königsbrügge, O.; Lang, I.M.; Klimek, P.; Thurner, S.; Pabinger, I.; Ay, C. Relative risk of arterial and venous thromboembolism in persons with cancer vs. persons without cancer-a nationwide analysis. Eur. Hear. J. 2021, 42, 2299–2307. [Google Scholar] [CrossRef] [PubMed]
- Mulder, F.I.; Horváth-Puhó, E.; van Es, N.; van Laarhoven, H.W.M.; Pedersen, L.; Moik, F.; Ay, C.; Büller, H.R.; Sørensen, H.T. Venous thromboembolism in cancer patients: A population-based cohort study. Blood 2021, 137, 1959–1969. [Google Scholar] [CrossRef] [PubMed]
- Chew, H.K.; Wun, T.; Harvey, D.; Zhou, H.; White, R.H. Incidence of venous thromboembolism and its effect on survival among patients with common cancers. Arch. Intern. Med. 2006, 166, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Moik, F.; Zochbauer-Muller, S.; Posch, F.; Pabinger, I.; Ay, C. Systemic Inflammation and Activation of Haemostasis Predict Poor Prognosis and Response to Chemotherapy in Patients with Advanced Lung Cancer. Cancers 2020, 12, 1619. [Google Scholar] [CrossRef]
- Moik, F.; Posch, F.; Grilz, E.; Scheithauer, W.; Pabinger, I.; Prager, G.; Ay, C. Haemostatic biomarkers for prognosis and prediction of therapy response in patients with metastatic colorectal cancer. Thromb. Res. 2020, 187, 9–17. [Google Scholar] [CrossRef] [Green Version]
- Moik, F.; Prager, G.; Thaler, J.; Posch, F.; Wiedemann, S.; Schramm, T.; Englisch, C.; Mackman, N.; Pabinger, I.; Ay, C. Hemostatic Biomarkers and Venous Thromboembolism Are Associated with Mortality and Response to Chemotherapy in Patients with Pancreatic Cancer. Arterioscler. Thromb. Vasc. Biol. 2021, 41, 2837–2847. [Google Scholar] [CrossRef]
- Ay, C.; Vormittag, R.; Dunkler, D.; Simanek, R.; Chiriac, A.-L.; Drach, J.; Quehenberger, P.; Wagner, O.; Zielinski, C.; Pabinger, I. D-dimer and prothrombin fragment 1 + 2 predict venous thromboembolism in patients with cancer: Results from the Vienna Cancer and Thrombosis Study. J. Clin. Oncol. 2009, 27, 4124–4129. [Google Scholar] [CrossRef]
- Ay, C.; Dunkler, D.; Simanek, R.; Thaler, J.; Koder, S.; Marosi, C.; Zielinski, C.; Pabinger, I. Prediction of venous thromboembolism in patients with cancer by measuring thrombin generation: Results from the Vienna Cancer and Thrombosis Study. J. Clin. Oncol. 2011, 29, 2099–2103. [Google Scholar] [CrossRef]
- Pabinger, I.; Ay, C.; Dunkler, D.; Thaler, J.; Reitter, E.-M.; Marosi, C.; Zielinski, C.; Mannhalter, C. Factor V Leiden mutation increases the risk for venous thromboembolism in cancer patients—Results from the Vienna Cancer and Thrombosis Study (CATS). J. Thromb. Haemost. 2015, 13, 17–22. [Google Scholar] [CrossRef]
- Kottke-Marchant, K.; Duncan, A. Antithrombin deficiency: Issues in laboratory diagnosis. Arch. Pathol. Lab Med. 2002, 126, 1326–1336. [Google Scholar] [CrossRef] [PubMed]
- Khor, B.; Van Cott, E.M. Laboratory tests for antithrombin deficiency. Am. J. Hematol. 2010, 85, 947–950. [Google Scholar] [CrossRef] [PubMed]
- Croles, F.N.; Borjas-Howard, J.; Nasserinejad, K.; Leebeek, F.W.G.; Meijer, K. Risk of Venous Thrombosis in Antithrombin Deficiency: A Systematic Review and Bayesian Meta-analysis. Semin. Thromb. Hemost. 2018, 44, 315–326. [Google Scholar] [PubMed]
- Lijfering, W.M.; Brouwer, J.-L.P.; Veeger, N.J.G.M.; Bank, I.; Coppens, M.; Middeldorp, S.; Hamulyák, K.; Prins, M.H.; Büller, H.R.; van der Meer, J. Selective testing for thrombophilia in patients with first venous thrombosis: Results from a retrospective family cohort study on absolute thrombotic risk for currently known thrombophilic defects in 2479 relatives. Blood 2009, 113, 5314–5322. [Google Scholar] [CrossRef] [Green Version]
- Pabinger, I.; Schneider, B. Thrombotic risk of women with hereditary antithrombin III-, protein C- and protein S-deficiency taking oral contraceptive medication. The GTH Study Group on Natural Inhibitors. Thromb. Haemost. 1994, 71, 548–552. [Google Scholar]
- Pabinger, I.; Thaler, J. How I treat patients with hereditary antithrombin deficiency. Blood 2019, 134, 2346–2353. [Google Scholar] [CrossRef]
- Croles, F.N.; Van Loon, J.E.; Dippel, D.W.J.; De Maat, M.P.M.; Leebeek, F.W.G. Antithrombin levels are associated with the risk of first and recurrent arterial thromboembolism at a young age. Atherosclerosis 2018, 269, 144–150. [Google Scholar] [CrossRef]
- Mahmoodi, B.K.; Veeger, N.J.; Middeldorp, S.; Lijfering, W.M.; Brouwer, J.L.P.; Ten Berg, J.; Hamulyák, K.; Meijer, K. Interaction of Hereditary Thrombophilia and Traditional Cardiovascular Risk Factors on the Risk of Arterial Thromboembolism: Pooled Analysis of Four Family Cohort Studies. Circ. Cardiovasc. Genet. 2016, 9, 79–85. [Google Scholar] [CrossRef] [Green Version]
- Kuhle, S.; Lane, D.A.; Jochmanns, K.; Male, C.; Quehenberger, P.; Lechner, K.; Pabinger, I. Homozygous antithrombin deficiency type II (99 Leu to Phe mutation) and childhood thromboembolism. Thromb. Haemost. 2001, 86, 1007–1011. [Google Scholar] [CrossRef]
- Tait, R.C.; Walker, I.D.; Perry, D.J.; Islam, S.I.A.M.; Daly, M.E.; McCall, F.; Conkie, J.A.; Carrell, R.W. Prevalence of antithrombin deficiency in the healthy population. Br. J. Haematol. 1994, 87, 106–112. [Google Scholar] [CrossRef]
- Wells, P.S.; Blajchman, M.A.; Henderson, P.; Wells, M.J.; Demers, C.; Bourque, R.; McAvoy, A. Prevalence of antithrombin deficiency in healthy blood donors: A cross-sectional study. Am. J. Hematol. 1994, 45, 321–324. [Google Scholar] [CrossRef] [PubMed]
- Semrad, T.J.; O’Donnell, R.; Wun, T.; Chew, H.; Harvey, D.; Zhou, H.; White, R.H. Epidemiology of venous thromboembolism in 9489 patients with malignant glioma. J. Neurosurg. 2007, 106, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Riedl, J.; Preusser, M.; Nazari, P.M.S.; Posch, F.; Panzer, S.; Marosi, C.; Birner, P.; Thaler, J.; Brostjan, C.; Lötsch, D.; et al. Podoplanin expression in primary brain tumors induces platelet aggregation and increases risk of venous thromboembolism. Blood 2017, 129, 1831–1839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nazari, P.M.S.; Berghoff, A.S.; Preusser, M.; Moik, F.; Posch, F.; Ricken, G.; Riedl, J.; Hell, L.; Marosi, C.; Hainfellner, J.A.; et al. Association of programmed cell death ligand 1 and circulating lymphocytes with risk of venous thromboembolism in patients with glioma. ESMO Open 2020, 5, e000647. [Google Scholar] [CrossRef]
- Riedl, J.; Ay, C. Venous Thromboembolism in Brain Tumors: Risk Factors, Molecular Mechanisms, and Clinical Challenges. Semin. Thromb. Hemost. 2019, 45, 334–341. [Google Scholar] [CrossRef]
- Thaler, J.; Ay, C.; Kaider, A.; Reitter, E.-M.; Haselböck, J.; Mannhalter, C.; Zielinski, C.; Marosi, C.; Pabinger, I. Biomarkers predictive of venous thromboembolism in patients with newly diagnosed high-grade gliomas. Neuro. Oncol. 2014, 16, 1645–1651. [Google Scholar] [CrossRef] [Green Version]
- Koudriavtseva, T.; Villani, V.; Lorenzano, S.; Giannarelli, D.; Di Domenico, E.G.; Stefanile, A.; Maschio, M.; D’Agosto, G.; Pimpinelli, F.; Tanzilli, A.; et al. Neutrophil-to-lymphocyte ratio, Factor VIII and Antithrombin III: Inflammatory-clotting biomarkers in glioma. Excli. J. 2021, 20, 1152–1169. [Google Scholar] [CrossRef]
- Rehman, S.U.; Ashraf, S.; Ahamad, S.; Sarwar, T.; Husain, M.A.; Ahmad, P.; Tabish, M.; Jairajpuri, M.A. Identification of a novel alternatively spliced isoform of antithrombin containing an additional RCL-like loop. Biochem. Biophys Res. Commun. 2019, 517, 421–426. [Google Scholar] [CrossRef]
- Niessen, R.W.L.M.; Lamping, R.J.; Jansen, P.M.; Prins, M.H.; Peters, M.; Taylor, F.B.; de Vijlder, J.J.M.; Cate, J.W.T.; Hack, C.E.; Sturk, A. Antithrombin acts as a negative acute phase protein as established with studies on HepG2 cells and in baboons. Thromb. Haemost. 1997, 78, 1088–1092. [Google Scholar] [CrossRef]
- Owens, M.R.; Miller, L.L. Net biosynthesis of antithrombin III by the isolated rat liver perfused for 12–24 hours. Compared with rat fibrinogen and alpha-2 (acute-phase) globulin, antithrombin III is not an acute phase protein. Biochim. Biophys Acta. 1980, 627, 30–39. [Google Scholar] [CrossRef]
- Moik, F.; Ay, C. Hemostasis and cancer: Impact of haemostatic biomarkers for the prediction of clinical outcomes in patients with cancer. J. Thromb. Haemost. 2022, 20, 2733–2745. [Google Scholar] [CrossRef] [PubMed]
- Grilz, E.; Königsbrügge, O.; Posch, F.; Schmidinger, M.; Pirker, R.; Lang, I.M.; Pabinger, I.; Ay, C. Frequency, risk factors, and impact on mortality of arterial thromboembolism in patients with cancer. Haematologica 2018, 103, 1549–1556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ay, C.; Simanek, R.; Vormittag, R.; Dunkler, D.; Alguel, G.; Koder, S.; Kornek, G.; Marosi, C.; Wagner, O.; Zielinski, C.; et al. High plasma levels of soluble P-selectin are predictive of venous thromboembolism in cancer patients: Results from the Vienna Cancer and Thrombosis Study (CATS). Blood 2008, 112, 2703–2708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lane, D.; Bayston, T.; Olds, R.J.; Fitches, A.C.; Cooper, D.N.; Millar, D.S.; Jochmans, K.; Perry, D.J.; Okajima, K.; Thein, S.L.; et al. Antithrombin mutation database: 2nd (1997) update. For the Plasma Coagulation Inhibitors Subcommittee of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Thromb. Haemost. 1997, 77, 197–211. [Google Scholar] [CrossRef]
- Mammen, E.F. Antithrombin: Its physiological importance and role in DIC. Semin. Thromb. Hemost. 1998, 24, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Monagle, P.; Barnes, C.; Ignjatovic, V.; Furmedge, J.; Newall, F.; Chan, A.; De Rosa, L.; Hamilton, S.; Ragg, P.; Robinson, S.; et al. Developmental haemostasis. Impact for clinical haemostasis laboratories. Thromb. Haemost. 2006, 95, 362–372. [Google Scholar] [PubMed]


| Patient Characteristics | ||||
|---|---|---|---|---|
| n (% Missing Value) | n (%) | Median (IQR) | Mean (+/− SD) | |
| Age | 1127 (0%) | 62 (52–68) | ||
| Female | 1127 (0%) | 509 (45%) | ||
| VTE | 1127 (0%) | 110 (9.8%) | ||
| ATE | 1127 (0%) | 32 (2.8%) | ||
| Died | 1127 (0%) | 563 (50%) | ||
| Metastatic disease (solid tumor patients) | 892 (0%) | 548 (61%) | ||
| Non-classifiable (brain, hematological) | 235 (0%) | |||
| Median follow-up period (months) | 1127 (0%) | 18 (6–24) | ||
| Antithrombin activity level (%) | 1127 (0%) | |||
| 1127 (0%) | 104.9 (88.3–121.5) | ||
| 194 (0%) | 121.2 (102.4–140) | ||
| 943 (0%) | 101.7 (87.6–115.8) | ||
| Outcomes within 2 years follow-up | 1127 (0%) | |||
| 110 (9.8%) | |||
| 32 (2.8%) | |||
| 563 (50%) | |||
| Univariable (95% CI) | p | Multivariable (95% CI) | p | |
|---|---|---|---|---|
| Full cohort (n = 1127) | ||||
| Risk of VTE | 1.01 (0.99–1.02) | 0.343 | 1.00 (0.99–1.01) | 0.903 |
| Risk of ATE | 1.00 (0.97–1.02) | 0.743 | 1.00 (0.98–1.03) | 0.952 |
| Risk of mortality | 1.00 (1.00–1.01) | 0.608 | 1.00 (0.99–1.00) | 0.102 |
| Only brain tumors (n = 194) | ||||
| Risk of VTE | 0.99 (0.96–1.03) | 0.680 | 0.99 (0.96–1.03) | 0.690 |
| Risk of ATE | 1.02 (1.00–1.04) | 0.017 | 1.02 (1.00–1.04) | 0.055 |
| Risk of mortality | 1.01 (1.00–1.02) | 0.030 | 1.01 (1.00–1.02) | 0.083 |
| Non-brain cancer (n = 977) | ||||
| Risk of VTE | 1.00 (0.99–1.02) | 0.460 | 1.01 (1.00–1.02) | 0.246 |
| Risk of ATE | 0.98 (0.95–1.01) | 0.217 | 0.99 (0.96–1.02) | 0.527 |
| Risk of mortality | 1.00 (0.99–1.00) | 0.546 | 1.00 (0.99–1.00) | 0.449 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Englisch, C.; Königsbrügge, O.; Nopp, S.; Moik, F.; Quehenberger, P.; Preusser, M.; Pabinger, I.; Ay, C. Antithrombin Activity and Association with Risk of Thrombosis and Mortality in Patients with Cancer. Int. J. Mol. Sci. 2022, 23, 15770. https://doi.org/10.3390/ijms232415770
Englisch C, Königsbrügge O, Nopp S, Moik F, Quehenberger P, Preusser M, Pabinger I, Ay C. Antithrombin Activity and Association with Risk of Thrombosis and Mortality in Patients with Cancer. International Journal of Molecular Sciences. 2022; 23(24):15770. https://doi.org/10.3390/ijms232415770
Chicago/Turabian StyleEnglisch, Cornelia, Oliver Königsbrügge, Stephan Nopp, Florian Moik, Peter Quehenberger, Matthias Preusser, Ingrid Pabinger, and Cihan Ay. 2022. "Antithrombin Activity and Association with Risk of Thrombosis and Mortality in Patients with Cancer" International Journal of Molecular Sciences 23, no. 24: 15770. https://doi.org/10.3390/ijms232415770
APA StyleEnglisch, C., Königsbrügge, O., Nopp, S., Moik, F., Quehenberger, P., Preusser, M., Pabinger, I., & Ay, C. (2022). Antithrombin Activity and Association with Risk of Thrombosis and Mortality in Patients with Cancer. International Journal of Molecular Sciences, 23(24), 15770. https://doi.org/10.3390/ijms232415770







